Back to Journals » Patient Preference and Adherence » Volume 17
EUFOREA Comment on a Misleading Allergic Rhinitis Report [Letter]
Authors Scadding GK , Smith PK , Hellings PW
Received 24 July 2023
Accepted for publication 25 July 2023
Published 29 July 2023 Volume 2023:17 Pages 1881—1883
DOI https://doi.org/10.2147/PPA.S431247
Checked for plagiarism Yes
Editor who approved publication: Dr Johnny Chen
Glenis K Scadding,1,* Peter K Smith,2,* Peter W Hellings3,4,*
1Department of Allergy & Rhinology, Royal National ENT Hospital; Division of Immunity and Infection, University College, London, UK; 2Griffith University, School of Medicine, Southport, Queensland, 4215, Australia; 3Department of Otorhinolaryngology-Head and Neck Surgery, University Hospitals, Leuven, Belgium; 4Upper Airways Research Laboratory, Department of Head and Skin, Ghent University, Ghent, Belgium
*These authors contributed equally to this work
Correspondence: Glenis K Scadding, Royal National ENT Hospital, 6 Huntley Street, London, W1E 6DG, UK, Tel +442087236045, Email [email protected]
View the original paper by Dr Fifer and colleagues
A Response to Letter has been published for this article.
Dear editor
As members of the EUFOREA Allergic Rhinitis Expert Panel we look for new evidence of effectiveness and acceptability of rhinitis treatments, reflecting EUFOREA’s ambition to optimize chronic respiratory disease therapy.1 Having read “Patient Satisfaction and Sensory Attributes of Nasal Spray Treatments of Olopatadine Hydrochloride/Mometasone Furoate Monohydrate and Azelastine Hydrochloride/Fluticasone Propionate for Allergic Rhinitis in Australia – An Observational Real-World Clinical Study”, published in Patient Preference and Adherence 2023:17,141–1512 we wish to comment on its concept, conduct and conclusions.
The title “REAL-WORLD” is inappropriate for a skewed, paid, unbalanced patient population, collected via a commercial online portal. The patients studied do not correspond to real world practice in Australia.3
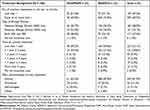
There is marked disparity between patient populations: that of Olopatadine Hydrochloride/Mometasone Furoate Monohydrate (OLO/MOM) was 44% female, versus 76% of the Azelastine Hydrochloride/Fluticasone Propionate (AZE/FLU) population. 77% of OLO/MOM were under 40 years of age versus 63% for AZE/FLU. There was no differentiation of non-allergic rhinitis (NAR) which is a co-factor in approximately 30% of allergic rhinitis (AR) patients, nor for any concomitant nasal structural abnormalities. NAR is associated with nasal hyper-reactivity and is more common in females. AZE/FLU nasal formulation is currently the only treatment with proven efficacy on nasal hyperreactivity (NHR).4
Nearly two thirds of those receiving OLO/MOM had a short disease duration of under 12 months vs 50% in the AZE/FLU group. Longer duration of disease involves priming: increased reactivity towards both allergic and non-allergic stimuli following allergen exposure.
There was also a significant difference in treatment background with more OLO-MOM subjects being treatment naive: 51% patients in the OLO/MOM group used less than 1 previous treatment (meaning zero) whereas 75.9% patients in the AZE/FLU group used 1 or more in the last 12 months (Table 1). To be prescribed AZE/FLU patients had to be dissatisfied with their previous treatment and were thus more likely to suffer from severe AR.
Self-determination of treatment, a positive influencer of health outcomes and satisfaction, occurred in 29.2% of the OLO-MOM group but in only 2.1% for AZE/FLU.
Thus there was significant bias in favour of OLO-MOM on several counts. Despite this the outcome which matters to patients, namely efficacy, was superior in the AZE/FLU users (p< 0.01**) and the duration of action was also significantly superior when re-scaled for importance. These results were not discussed in the Conclusions.
Another important omission was that of nasal irritation. OLO/MOM formulation has a pH of 3.7 with sucralose as a taste-masking agent. AZE/FLU has a pH of 5.9, without any taste-masking excipients. It is likely that a more acidic pH will cause more nasal irritation.5 However, the authors did not discuss the results in this respect.
Thus the paper which states that patient satisfaction is greater with OLO/MOM than with AZE/FLU is unrepresentative, biased and inaccurate since the most important outcomes: efficacy and duration of action were actually superior in the AZE/FLU treated patients.
Disclosure
GKS: Honoraria for articles, speaker and advisory boards: ALK, Bayer, GlaxoSmithKline, Haleon, Noucor, Sanofi- Regeneron, and Viatris. Chair of BSACI rhinitis guidelines, Scientific Chief Editor, Rhinology Section of Frontiers in Allergy, Board member and AR lead for EUFOREA, and Chair/ member Data Monitoring Committees on SLIT for ALK.
PKS: grants for investigator-initiated research from Hyloris, GSK and Sanofi. He has received honorarium for participating in GA2LEN and Viatris activities and advisory boards for the Nestle Nutrition institute and speaker activities for the latter and GSK. Grants from the Stafford Fox Foundation and the Australian Nation Health and Medical Research Foundation. He has shares in Valneva, a vaccine company. He has patents in detection and modification of TRP receptor dysfunction. He is a member of the EUFOREA rhinitis expert panel.
PWH: Is recipient of consultancy/lecture fees or unrestricted research grants from Sanofi/Regeneron, Novartis, GSK, Medtronic, Stallergenes, Nocour and Viatris.
EUFOREA has received funding from Sanofi/Regeneron, Novartis, Astra-Zeneca, GSK, Stallergenes, ALK, Noucor, Viatris, Johnson and Johnson, EAACI, Covis Pharma Europe BV, Nestlé, Thermo Fisher Scientific and Chiesi for educational and/or research initiatives.
References
1. Hellings PW, Scadding G, Bachert C, et al. EUFOREA treatment algorithm for allergic rhinitis. Rhinology. 2020;58(6):618–622. PMID: 329916582. doi:10.4193/Rhin20.376
2. Fifer S, Toh L, Barkate H, et al. Patient satisfaction and sensory attributes of nasal spray treatments of olopatadine hydrochloride/mometasone furoate monohydrate and azelastine hydrochloride/fluticasone propionate for allergic rhinitis in Australia – an observational real-world clinical study. Patient Prefer Adherence. 2023;17:141–151. doi:10.2147/PPA.S389875
3. Price DB, Smith PK, Harvey RJ, et al. Real-life treatment of rhinitis in Australia: a historical cohort study of prescription and over-The-counter therapies for patients with and without additional respiratory disease. Pragmat Obs Res. 2018;9:43–54. doi:10.2147/POR.S153266
4. Kortekaas Krohn I, Callebaut I, Alpizar YA, et al. MP29-02 reduces nasal hyperreactivity and nasal mediators in patients with house dust mite-allergic rhinitis. Allergy. 2018;73:1084–1093. doi:10.1111/all.13349
5. Bustamante-Marin XM, Ostrowski LE. Cilia and Mucociliary Clearance. Cold Spring Harb Perspect Biol. 2017;9(4):a028241. PMID: 27864314; PMCID: PMC5378048. doi:10.1101/cshperspect.a028241
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.