Back to Journals » International Journal of General Medicine » Volume 16
Establishment and Validation of the Risk Nomogram of Poor Prognosis in Patients with Severe Pulmonary Infection Complicated with Respiratory Failure
Received 20 March 2023
Accepted for publication 2 June 2023
Published 21 June 2023 Volume 2023:16 Pages 2623—2632
DOI https://doi.org/10.2147/IJGM.S413350
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Beizhan Liu, Qiang Zhang
Department of Respiratory and Critical Care Medicine, The Third Xiangya Hospital, Changsha City, Hunan Province, People’s Republic of China
Correspondence: Qiang Zhang, The Third Xiangya Hospital, No. 108 Tongzipo Road, Yuelu District, Changsha City, Hunan Province, 410013, People’s Republic of China, Email [email protected]
Objective: To investigate the prognosis of patients with severe pulmonary infection combined with respiratory failure and analyze the influencing factors of prognosis.
Methods: The clinical data of 218 patients with severe pneumonia complicated with respiratory failure were retrospectively analyzed. The risk factors were analyzed by univariate and multivariate logistic regression analyses. The risk nomogram and Bootstrap self-sampling method were used for internal inspection. Calibration curves and receiver operating characteristic (ROC) curve were drawn to assess the predictive ability of the model.
Results: Among 218 patients, 118 (54.13%) cases had a good prognosis and 100 (45.87%) cases had a poor prognosis. Multivariate logistic regression analysis showed that the number of complicated basic diseases ≥ 5, APACHE II score > 20, MODS score > 10, PSI score > 90, and multi-drug resistant bacterial infection were independent risk factors affecting the prognosis (P< 0.05), and the level of Alb was an independent protective factor (P< 0.05). The consistency index (C-index) was 0.775, and the Hosmer Lemeshow goodness-of-fit test showed that the model was not significant (P> 0.05). The area under the curve (AUC) was 0.813 (95% CI: 0.778~0.895), with the sensitivity of 83.20%, and the specificity of 77.00%.
Conclusion: The risk nomograph model had good discrimination and accuracy in predicting the prognosis of patients with severe pulmonary infection combined with respiratory failure, which may provide a basis for early identification and intervention of patients at clinical risk and improve the prognosis.
Keywords: severe pulmonary infection, respiratory failure, prognosis, influencing factors
A Letter to the Editor has been published for this article.
Introduction
Lung infection refers to the inflammation of the lung parenchyma caused by infection, which has a high incidence rate and mortality. Severe pulmonary infection accounts for about 1/3 of the major causes of death worldwide.1 The occurrence factors of lung infection are relatively complex, which may be caused by the interaction of multiple organisms. Age, malnutrition, immunosuppression, tobacco smoke, air pollution, etc. may be the risk factors of inducing pneumonia.2,3 Patients with lung infection have abnormal changes in normal lung cells, and lung function cannot be carried out effectively, so lung ventilation is significantly reduced, eventually causing hypoxia and carbon dioxide retention. Respiratory failure caused by lung infection is generally more likely to occur in the later stages of the lesion, and the onset rate is slower than other diseases. Respiratory failure is a serious complication in patients with severe pneumonia. Due to the high mortality rate and complications of respiratory failure, it is the key to the treatment of respiratory critical illness. Data show that patients with severe lung infections will have acidosis, hypoxia, bacterial toxins and other syndromes, which result in pulmonary arteriolar spasm, metabolic disorders, thus causing multi-organ damage and respiratory failure.4 Respiratory failure progresses rapidly with a poor prognosis, which seriously threatens the life safety of patients.
In the past, severe pneumonia was mainly treated by tracheal intubation and ventilator. However, this therapy may induce severe invasive stress reaction and inflammatory reaction, leading to inflammatory reaction, secondary infection and other complications, and increase the pain of patients.5 With the progress of medical diagnosis and treatment technology, the treatment effect of severe pulmonary infection combined with respiratory failure has been greatly improved, but the mortality of patients is still high. Therefore, finding effective methods for early diagnosis and timely intervention to improve the survival rate and prognosis has become the focus of medical workers. However, at present, there is little information about the risk factors related to the death and development of patients with severe pulmonary infection.
In this study, 218 patients with severe pneumonia complicated with respiratory failure were picked as the objects, aiming to analyze the risk factors affecting the prognosis of patients and provide reference for their future preventive diagnosis and treatment, so that clinicians can assess the prognosis of patients in advance, formulate standardized and effective treatment plans, and reasonably allocate medical resources.
Materials and Methods
General Materials
The sample size was determined by retrospective analysis using random sampling in proportion to probability and size from the hospital otolaryngology database. The time range was March 2019~August 2021, and a total of 218 patients with severe pneumonia and respiratory failure were obtained. The prognosis was divided into cure, improvement and death. Patients with cure and improvement in prognosis were defined as the good prognosis group (118 cases) and patients with death were defined as the poor prognosis group (100 cases). Seventy-eight males and 40 females were included in the good prognosis group, with an average age of (63.78 ± 5.35) years. The poor prognosis group included 62 males and 38 females, with an average age of (68.91 ± 6.24) years. The selection process of general data is shown in Figure 1. Inclusion criteria: All subjects met the diagnosis and treatment criteria for severe pneumonia and respiratory failure.6,7 Exclusion criteria: (1) Patients with obvious cardiac function. (2) Glucocorticoids were used within 8 weeks before the study. (3) Pregnant or lactating patients. (4) Patients with mental disease or other infectious diseases. This study was approved by the hospital Ethics Committee, met the requirements of the Declaration of Helsinki, and followed the principles of medical ethics.
 |
Figure 1 The general data selection process. |
Collection of Clinical Pathological Data
Clinical data of the picked subjects were collected, including the gender (female, male), age, body mass index (BMI), cause of pneumonia (bacterial, viral), type of pneumonia (hospital-acquired, community-acquired), type of respiratory failure (type I, type II), hypertension history (yes, no), diabetes history (yes, no), smoking history (yes, no), mechanical ventilation history (yes, no), number of combined basic diseases (<5, ≥5), Acute Physiology and Chronic Health Evaluation (APACHE II) score (≤20, >20), multiple organ dysfunction syndrome (MODS) score (≤10, >10), pneumonia severity index (PSI) score (≤90, >90), multi-drug resistant bacterial infection (yes, no), oxygenation index, platelet (PLT), white blood cell (WBC), albumin (Albumin), neutrophil/lymphocyte ratio (NLR), aspartate aminotransferase (AST) and alanine aminotransferase (ALT), etc. Among them, APACHE II score is composed of acute physiological score, age score and chronic health score with a total score of 0~71 points.8 The higher the score, the more serious the disease, the worse the prognosis, and the higher the case fatality rate. The MODS score is a scoring system consisting of six functional assessments of organ systems, which is commonly used to assess the severity of organ damage.9 The scoring system has a total score of 24 points with a total of 6 indicators. Each index score is 0~4 points, in which 0 points represent basically normal function, and 4 points represent organ failure. PSI score includes 0~130 points. The higher the patient’s PSI score, the more serious the patient’s condition. The worse the prognosis of the patient, the higher the case fatality rate. A fully automatic biochemical analyzer (purchased in Shanghai Yuyan Scientific Instrument Co., Ltd., Fengxian District, Shanghai, China) was used to detect the levels of PLT, WBC, Alb, NLR, AST, and ALT.
Establishment and Verification of Risk Prediction Model
Logistic regression equation was established according to the multifactor regression model, and independent risk factors were screened by R software. Each independent risk factor was applied to the equation to calculate the regression coefficient. According to the value of the regression coefficient on the integral line of the nomogram, the corresponding specific integral value was obtained. The total score was obtained through adding the scores to evaluate the prognosis of patients.
The accuracy of risk model was evaluated by establishing ROC curve and drawing calibration chart for verification.
Statistical Analysis
The enumeration data in this study was expressed in [cases (%)] and was compared using χ2 test. The measurement data were all tested by normal distribution, which were consistent with normal distribution, and were expressed in the form of (x ± s). The measurement data between two groups were compared by independent sample t-test. Univariate analysis and multivariate logistic regression analysis were used to analyze the influencing factors of the prognosis of severe pulmonary infection complicated with respiratory failure, and the risk prediction model of nomogram was established according to the risk factors. The bootstrap self-sampling method was adopted for internal test. The prediction ability of the model was verified by ROC curve, C-index and calibration curve. SPSS 23.0 software was used for statistical data analysis in this study, and P<0.05 was regarded as the difference with statistical significance.
Results
Univariate Analysis on Prognosis of Patients
Univariate analysis showed that there existed no significant difference in gender, BMI, causes of pneumonia, type of pneumonia, respiratory failure type, hypertension history, diabetes history, smoking history, PLT, WBC, NLR, AST and ALT between the good prognosis group and the poor prognosis group (P>0.05). Significant differences existed in age, history of mechanical ventilation, number of combined basic diseases, APACHE II score, MODS score, PSI score, multi-drug resistant bacterial infections, oxygenation index and Alb between the groups with good prognosis and those with poor prognosis (P<0.05, Table 1).
 |
Table 1 Univariate Analysis on Prognosis of Patients [Cases (%), ( |
Multivariate Logistic Regression Analysis of Prognostic Factors of Severe Pulmonary Infection Complicated with Respiratory Failure
The indexes with statistical significance (see Table 2 for the assignment of variables) in Table 1 were used as independent variables, and the adverse prognosis of patients with severe pulmonary infection and respiratory failure was used as dependent variables for multivariate logistic regression analysis. The number of complicated basic diseases ≥5, APACHE II score >20, MODS score >10, PSI score >90, and multi-drug resistant bacterial infection were independent risk factors affecting the prognosis (P<0.05), and the level of Alb was an independent protective factor (P<0.05, Table 3).
 |
Table 2 The Assignment of Variables |
 |
Table 3 Multivariate Logistic Regression Analysis of Prognostic Factors of Severe Pulmonary Infection Complicated with Respiratory Failure |
Construction of Prognostic Nomogram for Patients with Severe Pulmonary Infection and Respiratory Failure
A risk nomograph model was established based on independent risk factors to predict the prognosis of patients with severe pulmonary infection and respiratory failure. The results showed that the number of complicated basic diseases, APACHE II score, MODS score, PSI score, multi-drug resistant bacterial infection, and Alb had certain predictive value for the prognosis risk of patients with severe pulmonary infection and respiratory failure (Figure 2).
 |
Figure 2 Construction of risk prediction model. |
Verification of Predictive Value of Risk Prediction Model
The accuracy of the nomograph model was tested by bootstrap self-sampling method. The result showed that the consistency index (C-index) was 0.775, and the Hosmer Lemeshow goodness-of-fit test showed that the model was not significant (P>0.05), indicating that the nomograph model was well fitted with the actual observation results (Figure 3). ROC curve analysis showed that AUC of the nomograph model to predict the adverse prognosis was 0.813 (95% CI: 0.778~0.895), with the sensitivity of 83.20% and the specificity of 77.00%, indicating that the constructed nomogram had good discrimination (Figure 4).
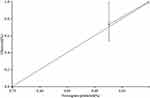 |
Figure 3 Calibration curve for external validation of nomograph model. |
 |
Figure 4 ROC curve for the validation of predictive value of risk prediction model. |
Discussion
Pulmonary infection is one of the common disease complications in respiratory and intensive care departments, and easily affects the respiratory system and other organs. Although the relevant treatment has made great progress in the past ten years, severe pulmonary infection is still the main cause of infection and death of patients worldwide, and its mortality has increased from about 20% to more than 50%.10 The severe pulmonary infection is more serious. Without timely treatment, it may rapidly develop into respiratory failure, shock, multiple organ dysfunction, and even life-threatening, with a high disability rate and mortality.11 Therefore, early prediction of patients’ prognosis and timely intervention play an important role in improving patients’ prognosis. In this study, the clinical data of patients were collected to analyze the relevant factors affecting the prognosis. The results showed that the number of complicated basic diseases, APACHE II score, MODS score, PSI score, multi-drug resistant bacterial infection, and low Alb disease were independent risk factors for the prognosis of severe pulmonary infection complicated with respiratory failure. Patients are often complicated with hypertension, diabetes, dyslipidemia, kidney and cardiovascular diseases and other complications with increased age. The correlation between basic diseases aggravates the existing chronic inflammation and leads to a strong immune response, thus increasing the susceptibility to lung infection and aggravating the severity of the disease.12,13 Some studies have found that diabetes and hyperglycemia may be the main complications that lead to poor prognosis of patients with COVID-19. In addition, patients with diabetes have an obviously increased risk of developing acute respiratory distress syndrome, multiple organ failure, and even death. It is reported14 that chronic obstructive pulmonary disease and malignant tumor are closely associated with a higher risk of death due to pneumonia infection. APACHE II score is one of the most famous disease severity scores and is also a common way to evaluate the prognosis of patients. APACHE II score has the advantages of simple and reliable operation and has been more and more widely used in various departments. In the study of severe pneumonia in children,15 the patients were grouped as the effective group and ineffective group according to the outcome of the disease. Compared with the ineffective group, the APACHE II score of patients in the effective group was sharply lower. APACHE II score could be used as an effective indicator to evaluate the severity of severe pneumonia in children and to indicate the prognosis of the disease. MODS score is a common index to judge the severity and prognosis of the disease, with high accuracy and specificity, and has no significant relationship with treatment. Some scholars found in the study of severe pneumonia with respiratory failure in the elderly16 that APACHE II score and MODS score were markedly higher in patients with poor prognosis, which can effectively predict the prognosis of severe pneumonia with respiratory failure in the elderly. PSI score is an important scoring system, which can evaluate the severity of pneumonia and determine the admission status. Some scholars found in the study of severe pneumonia with respiratory failure in the elderly that APACHE II score and MODS score were much higher in patients with poor prognosis, which could effectively predict the prognosis of severe pneumonia with respiratory failure in the elderly. PSI score is an important scoring system, which could be used to evaluate the severity of pneumonia and determine the admission status. Previous study found17 that the AUC of PSI was the highest (0.717, 95% CI 0.673~0.761) among all indexes to evaluate the severity of pneumonia. The PSI score may be the most useful pneumonia severity score for predicting the mortality of medical-related pneumonia.
Pneumonia is a respiratory infectious disease induced by different pathogens such as bacteria and viruses. Due to the lack of typical clinical manifestations in the early stage of pneumonia, patients are prone to gradually worsen the disease due to inappropriate empirical antibiotic treatment and other reasons, and even lead to severe pneumonia.18 With the abuse of antibacterial drugs, the normal balance of bacteria in the body is destroyed. Multiple drug-resistant bacterial infections often occur in patients, complicating the infection and increasing the mortality of patients. This study found that the level of Alb was closely related to the prognosis of patients, suggesting that Alb might be an important protective factor for the prognosis of patients with failure and death. It is reported19 that the complications and severity of infection of patients at the time of diagnosis have been regarded as important factors affecting prognosis. Alb level is a sign of nutrition and weakness. Some studies have found20 that the admission serum alb lower than 3.5 g/dL is associated with a higher risk of acute respiratory failure requiring mechanical ventilation, while a high serum albumin level of at least 4.5 g/dL is associated with a lower risk of acute respiratory failure. Therefore, the albumin level at admission may be helpful to predict the acute respiratory failure during hospitalization. The above influencing factors can help clinicians identify the poor prognosis in the early stage and give timely intervention to improve the effective rate of treatment and the prognosis of patients. In addition, early identification and provision of fast and active care are of great significance for patients in need of intensive care to reduce mortality and optimize the use of medical resources. A retrospective study was conducted on hospitalized patients with pneumonia confirmed by laboratory data.21 The results showed that the nomograph model had good prediction ability for serious diseases requiring follow-up. Clinicians can easily predict the patient’s course of disease and determine further follow-up procedures and facilities based on the patient’s admission clinical data and laboratory values. In the present study, the results of the nomogram showed that the nomogram model fitted well with the actual observation results, and the ROC curve results showed that the area under the curve of the nomogram model predicting the adverse prognosis of patients with severe lung infection and respiratory failure was 0.813 (95% CI: 0.778~0.895), the sensitivity was 83.20%, and the specificity was 77.00%, indicating that the constructed nomogram had a good degree of discrimination. The results indicated that in patients with severe pulmonary infection and respiratory failure, targeted treatment measures could be formulated according to relevant risk factors, which was of great significance to improve the safety of treatment and the prognosis of patients. This study used retrospective, case–control studies to collect clinical data of patients with severe lung infection and respiratory failure, analyze the prognostic risk factors, clinical features, diagnosis and treatment status and etiological types of patients, use logistic regression analysis to screen and analyze the relevant factors affecting the prognosis of patients, and establish a classification model to evaluate the prognosis of patients, which will help to understand the development trend and prognosis of the disease, and can provide reference for clinicians to judge the condition and prognosis of patients and formulate reasonable treatment plans. This improves the rescue success rate of patients with severe pulmonary infection and respiratory failure.
Conclusion
Taken together, in patients with severe pulmonary infection combined with respiratory failure, the risk nomograph model based on independent risk factors to predict the prognosis had good discrimination and accuracy, which provided a basis for early identification and intervention of patients at clinical risk and improved the prognosis. However, the study area was relatively limited and the sample size was small. Prospective research methods will be adopted in the follow-up study, and the sample size will be expanded to further evaluate the accuracy of the results.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by The Ethics Committee of the third Xiangya Hospital (Approval number: 22128). Informed consent was obtained from participants and/or their legal guardian for the participation in the study, and all methods were carried out in accordance with relevant guidelines and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Fang X, Yang H. The significance of implementing bilevel positive airway pressure under cluster nursing in improving the survival possibility of patients with severe pulmonary infection complicated by respiratory failure. Comput Math Methods Med. 2022;2022(1):2324797. doi:10.1155/2022/2324797
2. Marangu D, Zar HJ. Childhood pneumonia in low-and-middle-income countries: an update. Paediatr Respir Rev. 2019;32(1):3–9. doi:10.1016/j.prrv.2019.06.001
3. Goyal JP, Kumar P, Mukherjee A, et al.; Acute Respiratory Infection Treatment Unit Study Group. Risk factors for the development of pneumonia and severe pneumonia in children. Indian Pediatr. 2021;58(11):1036–1039. doi:10.1007/s13312-021-2369-1
4. Lin WV, Kruse RL, Yang K, Musher DM. Diagnosis and management of pulmonary infection due to Rhodococcus equi. Clin Microbiol Infect. 2019;25(3):310–315. doi:10.1016/j.cmi.2018.04.033
5. Perkins GD, Ji C, Connolly BA, et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the RECOVERY-RS randomized clinical trial. JAMA. 2022;327(6):546–558. doi:10.1001/jama.2022.0028
6. Grief SN, Loza JK. Guidelines for the evaluation and treatment of pneumonia. Prim Care. 2018;45(3):485–503. doi:10.1016/j.pop.2018.04.001
7. Villgran VD, Lyons C, Nasrullah A, Clarisse Abalos C, Bihler E, Alhajhusain A. Acute respiratory failure. Crit Care Nurs Q. 2022;45(3):233–247. doi:10.1097/CNQ.0000000000000408
8. Tian Y, Yao Y, Zhou J, et al. Dynamic APACHE II score to predict the outcome of intensive care unit patients. Front Med. 2022;8:744907. doi:10.3389/fmed.2021.744907
9. Sharif AF, Fayed MM. Evaluation of Multiple Organ Dysfunction Score (MODS) and the Sequential Organ Failure Assessment (SOFA) score as in-hospital outcome predictors among cases of hydrogen cyanamide exposure: a cross-sectional study. Environ Sci Pollut Res Int. 2021;28(31):42161–42176. doi:10.1007/s11356-021-13655-6
10. Chen J, Li Y, Zeng Y, Tian Y, Wen Y, Wang Z. High mean platelet volume associates with in-hospital mortality in severe pneumonia patients. Mediators Inflamm. 2020;2020(1):8720535. doi:10.1155/2020/8720535
11. Meyerholz DK, Beck AP. Histopathologic evaluation and scoring of viral lung infection. Methods Mol Biol. 2020;2099(1):205–220.
12. Salazar M, Barochiner J, Espeche W, Ennis I. COVID-19, hipertensión y enfermedad cardiovascular [COVID-19 and its relationship with hypertension and cardiovascular disease]. Hipertens Riesgo Vasc. 2020;37(4):176–180. doi:10.1016/j.hipert.2020.06.003
13. Lanks CW, Musani AI, Hsia DW. Community-acquired pneumonia and hospital-acquired pneumonia. Med Clin North Am. 2019;103(3):487–501. doi:10.1016/j.mcna.2018.12.008
14. Rajpal A, Rahimi L, Ismail-Beigi F. Factors leading to high morbidity and mortality of COVID-19 in patients with type 2 diabetes. J Diabetes. 2020;12(12):895–908. doi:10.1111/1753-0407.13085
15. Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. 2020;23(5):1416–1424. doi:10.1080/13685538.2020.1774748
16. Zhang HF, Zhang X, Sha YX, et al. Value of sTREM-1 in serum and bronchoalveolar lavage fluid, APACHE II score, and SOFA score in evaluating the conditions and prognosis of children with severe pneumonia. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(6):626–631. doi:10.7499/j.issn.1008-8830.1912134
17. Pittman J, Beeson T, Dillon J, et al. Hospital-acquired pressure injuries and acute skin failure in critical care: a case-control study. J Wound Ostomy Continence Nurs. 2021;48(1):20–30. doi:10.1097/WON.0000000000000734
18. Ito A, Ishida T, Tokumasu H, Yamazaki A, Washio Y. Evaluation of pneumonia severity scoring systems in nursing and healthcare-associated pneumonia for predicting prognosis: a prospective, cohort study. J Infect Chemother. 2020;26(4):372–378. doi:10.1016/j.jiac.2019.11.001
19. Kim MA, Park JS, Lee CW, Choi WI. Pneumonia severity index in viral community acquired pneumonia in adults. PLoS One. 2019;14(3):e0210102. doi:10.1371/journal.pone.0210102
20. Thongprayoon C, Cheungpasitporn W, Chewcharat A, Mao MA, Thirunavukkarasu S, Kashani KB. Risk of acute respiratory failure among hospitalized patients with various admission serum albumin levels: a cohort study. Medicine. 2020;99(9):e19352. doi:10.1097/MD.0000000000019352
21. Guner R, Kayaaslan B, Hasanoglu I, et al. Development and validation of nomogram to predict severe illness requiring intensive care follow up in hospitalized COVID-19 cases. BMC Infect Dis. 2021;21(1):1004. doi:10.1186/s12879-021-06656-w
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

