Back to Journals » Journal of Inflammation Research » Volume 15
Establishment and Effectiveness Evaluation of a Scoring System-RAAS (RDW, AGE, APACHE II, SOFA) for Sepsis by a Retrospective Analysis
Authors Huang Y, Jiang S, Li W, Fan Y , Leng Y , Gao C
Received 9 November 2021
Accepted for publication 25 December 2021
Published 20 January 2022 Volume 2022:15 Pages 465—474
DOI https://doi.org/10.2147/JIR.S348490
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Yingying Huang,1,* Shaowei Jiang,1,* Wenjie Li,1 Yiwen Fan,2 Yuxin Leng,3 Chengjin Gao1
1Emergency Department, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Department of Pathology Medicine Biology, The University Medical Center Groningen, Groningen, the Netherlands; 3Critical Care Medicine Department, Peking University Third Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chengjin Gao; Yuxin Leng Email [email protected]; [email protected]
Background: A modified scoring system based on the RDW, AGE, SOFA, and APACHE II score (RAAS score) was composed to investigated the short-, medium-, and long-term high risk of mortality in patients with sepsis identified early in the emergency department (ED).
Methods: Data were collected from a total of 1066 sepsis patients in emergency department, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine from March 2013 to April 2021, including 529 patients in the primary cohort and 537 patients in the validation cohort. By comparing each parameter and the area under ROC (AUC) and K-M (Kaplan–Meier) survival curve in different periods, valuable parameters were screened out to form a new scoring system, and finally the prediction model of the nomogram was built.
Results: The RAAS scoring system, consisting of RDW, AGE, SOFA and APACHE II, is a 0– 6 scale to reflect the severity of sepsis. AUC at 30, 60, and 90 days was 0.816, 0.815, and 0.820, respectively. K-M curves across six prognostic time periods in both databases showed survival probabilities with different RDW segments and RAAS scores. In the calibration curve, the results of the internal validation of the primary cohort and the results of the external validation cohort showed the prognostic accuracy of RAAS.
Conclusion: The RAAS score system is a novel and reliable indicator to predict the short-term and medium-term mortality of patients with sepsis. With the increase of the RAAS score, the mortality of patients with sepsis gradually increases.
Keywords: sepsis, risk factors, prognosis, mortality, nomograms
A Letter to the Editor has been published for this article.
Background
Sepsis is a serious, life-threatening syndrome that is one of the leading causes of death in hospitals.1,2 Sepsis was also among the leading causes of the death associated with COVID-19.3 Despite significant advances in critical care, sepsis still has a relatively high short-term mortality rate due to organ failure due to a dysregulated response to infection.4 Often as the first place where sepsis patients are initially treated, it is significant for the emergency department (ED) to identify patients with a high mortality rate among sepsis patients in the early stages of sepsis, in order to provide more timely and adequate interventions for these patients and to help patients be properly classified.5 Up to now, there is still no effective treatment and means for sepsis.6
Early prediction of progressive septic shock plays an important role in its clinical course and prognosis.7 Although several biomarkers have been studied to predict mortality in patients with sepsis, none of these biomarkers have been shown to reliably identify patients at high risk for sepsis, and tests for these biomarkers are often not widely used in clinical practice.8 Moreover, due to the complexity of sepsis, the diagnostic accuracy of each parameter is limited in clinical practice. As a standard to evaluate the severity of disease in intensive care unit (ICU), scoring system has become an important tool to help clinicians make decisions.9
A scoring system with higher prognostic accuracy has been developed that combines four clinical indicators to predict the mortality of patients with sepsis using a score of 0 to 6, with one point awarded for each value that meets the scoring requirement (Supplementary Table 1). The main objective of this study was to evaluate the effect of RAAS on short-term (30 days), medium-term (60 days, 90 days) and long-term (180 days, 365 days, 730 days) mortality in patients with sepsis using a large clinical database, and then to establish nomograms of the effective prediction period to visually predict the 30-day,60-day and 90-day mortality probability in patients with sepsis. The RAAS score has a great predictive function for the evaluation of the prognosis of death in sepsis.
Methods
Patients and Study Design
We conducted a retrospective observational study on 1066 patients with sepsis between March 2013 and April 2021. According to the time point, 529 patients were selected as the primary cohort. The remaining 537 patients were selected as validation cohort study subjects to verify the effectiveness of RAAS. As can be seen from Supplementary Table 2, this database has a high degree of fit and is suitable for the verification of the scoring system. The authors used a structured collection format to collect data from electronic medical records. The other author reviewed all the data, and any disagreements were resolved through discussion among the authors.
All hospitalized patients diagnosed with sepsis or septic shock were eligible for inclusion in the study. In order to unify the standards, we reevaluated the situation and information of all patients according to the latest sepsis standards, and eliminated the information of patients that did not meet the latest sepsis standards. Exclusion criteria included: (1) Patients younger than 18 years; (2) Patients with ICU stay less than 24 h; (3) Patients with abnormal values (values 3 times higher than the mean standard deviation (SD)). For patients admitted more than once, only the first hospitalization was included in the analysis. In the case of multiple infections, the main source of infection was dominant (the infection that been spotted first and related organ diseases).
Ethics
The research was carried out in accordance with the ethical standards of the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (No. XHEC-D-2021-131) and the National Research Council and in accordance with the Declaration of Helsinki and its subsequent amendments or similar ethical standards. We confirm the patients were informed about the purpose of the study and we read informed consents from the participants to participate the study and to report or publish the retrospective study data.
Establishment of RAAS Scoring System for Sepsis and Investigate the Correlation Between Different RAAS Scores and Prognosis of Patients with Sepsis
Assign values for parameters according to different variable ranges and CUTOFF values of different parameters. The parameter assignment is based on the assignment method of the APACHE II scoring system and the MODS scoring system.10 To verify the prognosis evaluation effect of RAAS in patients with sepsis, The APACHE II score, SOFA score and corresponding RAAS score within 24h after admission were calculated for patients in the primary cohort and validation cohort. The AUC area of the three scoring systems and the AUC area of the single RDW were calculated, and the predictive effect of RAAS on sepsis patients was judged by comparing the AUC area of the three scoring systems.
The scores were divided into four intervals (GROUP-1:0–1, GROUP-2:2–3, GROUP-3:4–5, GROUP-4:6), and the total mortality of sepsis patients corresponding to four different RAAS scoring intervals and the mortality of patients with different RAAS scores were calculated. The survival curves at 30, 60, 90, 180, 365 and 730 days in the primary cohort and the validation cohort were used to demonstrate and verify their prognostic value.
Statistical Analysis
The normal-distributed measurement data set is represented by mean plus or minus standard deviation (mean±SD or x±S), while the mis-distributed measurement data set is represented by median (quaternary range). Counting data is expressed as a percentage. For the comparison of data between two groups, univariate statistical method is used to measure the data, two-independent-samples t-test is used for the normal distribution of the two groups of data, and the rank sum test of two independent samples is used for the normal distribution of the data.
For parameters with statistically significant differences in univariate analysis, receiver operating characteristic (ROC) curve analysis was used to determine the optimal truncation value of each independent parameter. The corresponding value of the highest Youden index calculated by specificity + sensitivity −1 was used to calculate the AUC screening RAAS parameters, and the 95% confidence interval was calculated. Log rank test was used to compare the survival curves in different intervals of RDW and the survival curves in different time periods of each rating group of RAAS. The significant 30-day, 60-day and 90-day RAAS calibration curves were plotted respectively to verify the performance of the RAAS scoring system model trained by the primary cohort in the validation cohort. Meanwhile, the overall and 30-day, 60-day and 90-day nomogram were plotted. The results of logistic regression analysis were used to construct the nomogram. The performance of the nomogram was evaluated for calibration, identification and clinical applications.
The statistical analyses were performed using SPSS software version 26.0 (SPSS Inc, Chicago, IL) and the R statistical software, version 3.2.4 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline Clinical Data and Demographic Characteristics and Results of Screening the Scoring System Parameters for RAAS
There were no significant differences between the alive and dead groups for cardiovascular, kidney disease, or other comorbidities. In terms of the sources of sepsis infection, the distribution of each source of infection is roughly the same. Since it is not the key research parameter in this study, no more details will be given here (Table 1). The determined single-factor statistical analysis of RAAS parameters actually included in the statistical analysis is shown in Table 2. A total of four significantly different parameters were included in RAAS between the two groups. Through the above series of screening, this study finally determined that RDW, AGE, SOFA and APACHE II can be used as the parameters of RAAS.
 |
Table 1 The Demographics and Baseline Clinical Data of the Sepsis Patients for RAAS Establishment |
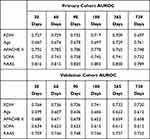 |
Table 2 The AUC of Each Parameter for RAAS in Different Survival Length at Two Cohorts |
Establishment of the Scoring System for Sepsis and Evaluation Effectiveness of RAAS on the Prognosis of Sepsis Patients
The RAAS scoring system is a better predictor of mortality than the old scoring system. Had the highest value (Table 2), indicating that the improved scoring system was the best predictor of the three scoring methods (Figure 1). AUC of all parameters of RAAS were calculated using the database to evaluate the effectiveness of RAAS (Table 2). The prognosis of survival was different between the primary cohort and the validation cohort with different lengths of the RAAS scoring system, but was greater than 0.7 overall. In the primary cohort, AUC-30 days were 0.816, AUC-60 days were 0.815, AUC-90 days were 0.820, AUC-180 days were 0.805, AUC-365 days were 0.800, and AUC-730 days were 0.789. In the validation cohort, the values of AUC-30 days, AUC-60 days, AUC-90 days, AUC-180 days, AUC-365 days and AUC-730 days were 0.759, 0.746, 0.748, 0.746, 0.737 and 0.732. When the RAAS score was no less than 6, sepsis patients have a mortality rate of up to 80%.
In the Kaplan–Meier analysis, higher RAAS scores were associated with higher mortality on days 30, 60, and 90 (Figure 2). As can be seen from the statistical results (Figure 3), correction curves were drawn in the primary cohort and the validation cohort in this study on days 30, 60 and 90, and the data of the two groups of sepsis patients were highly fitted. With the improvement of RAAS score, sepsis’s mortality rate also increased and the number of patients also increased (Supplementary Figure 1, Supplementary Table 3). However, there was no significant difference between the death rates at 180 days, 365 days, and 730 days. When the RAAS≤1, the mortality rate of sepsis patients was less than 10%; when the RAAS=6, the mortality rate of sepsis patients was more than 80% (Supplementary Table 3). Line plots were made based on the overall prognosis and 30-day, 60-day, 90-day data. Four elements of the multivariate analysis were used to construct the nomogram (Figure 4).
Discussion
Critical patient scoring system is an important method to quantitatively evaluate the severity of disease.11 APACHE II scoring system is the most widely used and authoritative critical disease evaluation system. The system, designed by Professor Knaus’s team at the University of Washington in 1985, consists of three components: age, acute physiological score (APS) and chronic health score. In general, disease assessment and prognosis prediction are often quite accurate for common critical diseases, especially when the pathophysiological characteristics of the disease are similar to the included indicators in the APACHE II scoring system.12,13 However, continuous studies have confirmed that for some diseases with strong specialty characteristics or some special populations, diseases with special organ damage or abnormal physiological indicators, the above scoring system has certain defects.14 There is study found that the APACHE II score tended to overestimate mortality in this population.15
Previous study established and evaluated of a scoring system for exertional heat stroke by retrospective analysis. As EHSS score increases, the mortality rate of EHS patients gradually increases.16 Our study refers to this study, and adopts a similar method to screen out four parameters that constitute RAAS. Through statistical analysis, four parameters were included in RAAS, which included SOFA and APACHE II, simplified the lengthy details in the scoring system, and at the same time covered most of the clinical evaluation indicators. A review of the development of previous critical illness scoring systems (APACHE II, SAPS II, and MODS) shows that they were established on a large sample size.17,18 However, for the diseases with strong characteristics of specialization, the sample size of the scoring system based on the larger sample size cannot be obtained due to the limitation of the characteristics of primary disease and the source of cases. For example, the Ranson Scale.19,20
The number of indicators and scoring systems that enhance sepsis prognosis has been increasing researched in previous studies, sepsis (severe infection) on hematopoietic system has a great influence, one of the directions is the diagnostic and prognostic value of red blood cell distribution width in sepsis.21,22 In previous study, our group found the RDW fluctuation can help predict sepsis-related DIC morbidity and prognosis in patients with sepsis.23,24 More importantly, is it the RDW or the cause of increased RDW that is associated with increase mortality, in particular, malignancy, active chemoRT, vitamin B12 deficiency and chronic liver disease.25–28 The new research also found new biomarkers such as monocyte distribution width improve early detection of ED sepsis.29 Age is also a default prognostic factor for critical illness, with sepsis severely affecting the elderly.30
To our knowledge, this is the first study to assess independent risk factors associated with RAAS (RDW, AGE, APACHE II and SOFA) and establish a prediction graph for 30-day, 60-day, 90-day, 180-day, 365-day, and 730-day mortality. The overall study covered from short, to medium to long term outcomes (Figure 2). In addition, with the increase of RAAS score, the mortality rate of sepsis patients gradually increased from 20% to 80%, which has a great predictive function for the evaluation of the prognosis of death (Supplementary Table 3). The RAAS scoring system does not only apply the initial assessment of sepsis patients in ED, but also can intensively evaluate sepsis patients in the ICU, and also can do second evaluate to the latest condition of septic patients.
The difference between our RAAS score and SOFA score and APACHE II score is that, first, we obtained the score from a large number of patients with heterogeneous suspected sepsis, and we selected patients with confirmed sepsis who were admitted to the ICU of the emergency department for treatment. Second, we used only four independent predictors. In addition to pragmatic considerations, these rules may also suffer from overfitting,31 the performance of classifier is usually evaluated by increasing the amount of data and testing the sample set, we also calculate variance inflation factor (VIF) (variance inflation factor value) (Supplementary Table 4). The larger the VIF is, the smaller the tolerance of the independent variable is, and the more collinearity there is. This can result in poor subsequent performance of the validation queue. However, the performance of the fitting degree in the correction curve is still relatively fit. The RAAS score is simple and practical, but it also has a good sensitivity and negative predictive value, allowing us to exclude patients with an elevated risk of death.
In the medical literature, a nomogram is a graphical tool commonly used as a statistical prognostic model to assign a relative risk score for each risk factor based on its contribution to prognosis. The nomogram is primarily used for cancer prognosis and is primarily used to estimate the likelihood of an event.32 In this study, we applied the nomograms of RAAS to assess sepsis patients and explored the accuracy of its prediction in order to identify sepsis patients at high risk of death in the emergency department early in order to make the prediction model visualized and easy to use. Combined with the four RAAS parameters, a nomogram was made to predict the overall and 30-day, 60-day, and 90-day mortality of sepsis patients (Figure 4). It is essential that clinicians comprehensively assess the true risk of death and objectively assess the risks/benefits of medical interventions for patients with sepsis, enabling clinicians, patients and their families to carefully evaluate the impact of potential treatment options. Help them make medical decisions together and prevent medical disputes.
Reinforcement learning has been successfully applied to medical problems in the past, such as diabetes and mechanical ventilation in the ICU.33,34 As the number of cases participating in the RAAS scoring system increases, the weights of the four parameters constituting RAAS can be modified or adjusted continuously through machine reinforcement learning to make the scoring system more perfect and practical. We take RAAS as the base to jointly look forward to the emergence of a more accurate prognosis system for sepsis.
Our study had several limitations. First, as retrospective observational studies are by nature, information obtained from hospital electronic medical record systems may be biased or inaccurate. Second, as others have discussed,35,36 the total in-hospital mortality rate was used because the primary outcome of the performance evaluation may not match, because the in-hospital mortality rate may not have been caused by the initial sepsis in the ED. Finally, this was a retrospective study from a single medical center with a limited sample size. Therefore, Follow-up prospective studies are necessary to validate our findings and further confirmation of RAAS in a large sample is needed. In the following study, we plan to validate the RAAS scoring system in the MMIC III database.
Conclusions
RAAS (RDW, AGE, APACHE II, SOFA) is a scoring system for the prognosis of patients with sepsis. The establishment of this scoring system quantifies the severity of sepsis, which is of great significance to effectively determine the severity of sepsis patients in the future, improve the success rate of treatment, judge the prognosis of patients, and guide the treatment of doctors.
Abbreviations
RDW, Red cell distribution width; ED, emergency department; RAAS score, RDW, AGE, APACHE II and SOFA; AUC, the area under ROC; K-M, Kaplan–Meier survival curve; ICU, intensive care unit; MPV, Mean Platelet Volume; PC, platelet count; DNI, Delta neutrophil index; SD, standard deviation; mean±SD or x± S, mean plus or minus standard deviation; APS, acute physiological score; VIF, variance inflation factor value.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Review Committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, and all methods were in accordance with the Committee’s guidelines.
Acknowledgments
The authors thank all research participants throughout the included ICUs for their assistance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (82172138 and 81873947), Special Medical Innovation Project of Shanghai Science and Technology Committee (No.21Y11902400), Excellent Academic Leader Program of Shanghai Science and Technology Committee (21XD1402200), and the Key Laboratory of Emergency and Trauma (Hainan Medical University), Ministry of Education (Grant. KLET-202016).
Disclosure
The authors declare that they have no competing interests.
References
1. Goswami DG, Walker WE. Aged IRF3-KO mice are protected from sepsis. J Inflamm Res. 2021;14:5757–5767. doi:10.2147/JIR.S335203
2. Skirecki T, Drechsler S, Jeznach A, et al. An early myelosuppression in the acute mouse sepsis is partly outcome-dependent. Front Immunol. 2021;12:708670. doi:10.3389/fimmu.2021.708670
3. Sherwani S, Khan MWA. Cytokine response in SARS-CoV-2 infection in the elderly. J Inflamm Res. 2020;13:737–747. doi:10.2147/JIR.S276091
4. Crouser ED, Parrillo JE, Seymour C, et al. Improved early detection of sepsis in the ED with a novel monocyte distribution width biomarker. Chest. 2017;152(3):518–526. doi:10.1016/j.chest.2017.05.039
5. Rowe TA, McKoy JM. Sepsis in older adults. Infect Dis Clin North Am. 2017;31(4):731–742. doi:10.1016/j.idc.2017.07.010
6. Hu ZD, Lippi G, Montagnana M. Diagnostic and prognostic value of red blood cell distribution width in sepsis: a narrative review. Clin Biochem. 2020;77:1–6. doi:10.1016/j.clinbiochem.2020.01.001
7. Investigators P, Rowan KM, Angus DC, et al. Early, goal-directed therapy for septic shock - a patient-level meta-analysis. N Engl J Med. 2017;376(23):2223–2234.
8. Kim JH, Lee Y, Cho YS, et al. A modified simple scoring system using the red blood cell distribution width, delta neutrophil index, and mean platelet volume-to-platelet count to predict 28-day mortality in patients with sepsis. J Intensive Care Med. 2021;36(8):873–878. doi:10.1177/0885066620933245
9. Keegan MT, Gajic O, Afessa B. Severity of illness scoring systems in the intensive care unit. Crit Care Med. 2011;39(1):163–169. doi:10.1097/CCM.0b013e3181f96f81
10. Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638–1652. doi:10.1097/00003246-199510000-00007
11. Sekulic AD, Trpkovic SV, Pavlovic AP, Marinkovic OM, Ilic AN. Scoring systems in assessing survival of critically ill ICU patients. Med Sci Monit. 2015;21:2621–2629. doi:10.12659/MSM.894153
12. Fortis S, Amy M.J. O, Beck BF, et al. An automated computerized critical illness severity scoring system derived from APACHE III: modified APACHE. J Crit Care. 2018;48:237–242. doi:10.1016/j.jcrc.2018.09.005
13. Naqvi IH, Mahmood K, Ziaullaha S, Kashif SM, Sharif A. Better prognostic marker in ICU - APACHE II, SOFA or SAP II! Pak J Med Sci. 2016;32(5):1146–1151. doi:10.12669/pjms.325.10080
14. Stevens TA, Carroll MA, Promecene PA, Seibel M, Monga M. Utility of acute physiology, age, and chronic health evaluation (APACHE III) score in maternal admissions to the intensive care unit. Am J Obstet Gynecol. 2006;194(5):e13–e15. doi:10.1016/j.ajog.2006.01.073
15. Ryan HM, Sharma S, Magee LA, et al. The usefulness of the APACHE II score in obstetric critical care: a structured review. J Obstet Gynaecol Can. 2016;38(10):909–918. doi:10.1016/j.jogc.2016.06.013
16. Yang MM, Wang L, Zhang Y, et al. Establishment and effectiveness evaluation of a scoring system for exertional heat stroke by retrospective analysis. Mil Med Res. 2020;7(1):40. doi:10.1186/s40779-020-00269-1
17. Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014;20(5):557–565. doi:10.1097/MCC.0000000000000135
18. Lambden S, Laterre PF, Levy MM, Francois FB. The SOFA score—development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1):374. doi:10.1186/s13054-019-2663-7
19. Bartlett PL, Long PM, Lugosi G, Tsigler A. Benign overfitting in linear regression. Proc Natl Acad Sci U S A. 2020;117(48):30063–30070. doi:10.1073/pnas.1907378117
20. Takeda T, Nakai Y, Mizuno S, et al. Fluid sequestration is a useful parameter in the early identification of severe disease of acute pancreatitis. J Gastroenterol. 2019;54(4):359–366. doi:10.1007/s00535-018-1531-6
21. Han YQ, Zhang L, Yan L, et al. Red blood cell distribution width predicts long-term outcomes in sepsis patients admitted to the intensive care unit. Clin Chim Acta. 2018;487:112–116. doi:10.1016/j.cca.2018.09.019
22. Jiang Y, Jiang FQ, Kong F, et al. Inflammatory anemia-associated parameters are related to 28-day mortality in patients with sepsis admitted to the ICU: a preliminary observational study. Ann Intensive Care. 2019;9(1):67. doi:10.1186/s13613-019-0542-7
23. Fan YW, Liu D, Chen JM, Li WJ, Gao CJ. Fluctuation in red cell distribution width predicts disseminated intravascular coagulation morbidity and mortality in sepsis: a retrospective single-center study. Minerva Anestesiol. 2021;87(1):52–64. doi:10.23736/S0375-9393.20.14420-1
24. Tang L, Chen JR. The predictive value of hemocytometry based on peripheral platelet-related parameters in identifying the causes of febrile seizures. J Inflamm Res. 2021;14:5381–5392. doi:10.2147/JIR.S334165
25. Ai L, Mu S, Hu Y. Prognostic role of RDW in hematological malignancies: a systematic review and meta-analysis. Cancer Cell Int. 2018;18:61. doi:10.1186/s12935-018-0558-3
26. Pedrazzani C, Tripepi M, Turri G, et al. Prognostic value of red cell distribution width (RDW) in colorectal cancer. Results from a single-center cohort on 591 patients. Sci Rep. 2020;10(1):1072. doi:10.1038/s41598-020-57721-4
27. Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52(2):86–105. doi:10.3109/10408363.2014.992064
28. Fava C, Cattazzo F, Hu ZD, Lippi G, Montagnana M. The role of red blood cell distribution width (RDW) in cardiovascular risk assessment: useful or hype? Ann Transl Med. 2019;7(20):581. doi:10.21037/atm.2019.09.58
29. Crouser ED, Parrillo JE, Seymour CW, et al. Monocyte distribution width: a novel indicator of sepsis-2 and sepsis-3 in high-risk emergency department patients. Crit Care Med. 2019;47(8):1018–1025. doi:10.1097/CCM.0000000000003799
30. Wang AY, Ma HP, Kao WF, Tsai SH, Chang CK. Red blood cell distribution width is associated with mortality in elderly patients with sepsis. Am J Emerg Med. 2018;36(6):949–953. doi:10.1016/j.ajem.2017.10.056
31. Cook JA, Ranstam J. Overfitting. Br J Surg. 2016;103(13):1814. doi:10.1002/bjs.10244
32. Kim JH, Kim HS, Seo WY, et al. External validation of nomogram for the prediction of recurrence after curative resection in early gastric cancer. Ann Oncol. 2012;23(2):361–367. doi:10.1093/annonc/mdr118
33. Komorowski M, Celi LA, Badawi O, Gordon AC, Faisal AA. The Artificial Intelligence Clinician learns optimal treatment strategies for sepsis in intensive care. Nat Med. 2018;24(11):1716–1720. doi:10.1038/s41591-018-0213-5
34. Schinkel M, Paranjape K, Nannan Panday RS, Skyttberg N, Nanayakkara PWB. Clinical applications of artificial intelligence in sepsis: a narrative review. Comput Biol Med. 2019;115:103488. doi:10.1016/j.compbiomed.2019.103488
35. Osborn TM, Phillips G, Lemeshow S, et al. Sepsis severity score. Crit Care Med. 2014;42(9):1969–1976. doi:10.1097/CCM.0000000000000416
36. Cardoso T, Teixeira-Pinto A, Rodrigues PP, Aragao I, Costa-Pereira A, Sarmento AE. Predisposition, insult/ infection, response and organ dysfunction (PIRO): a pilot clinical staging system for hospital mortality in patients with infection. PLoS One. 2013;8(7):e70806. doi:10.1371/journal.pone.0070806
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




