Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Erdosteine reduces inflammation and time to first exacerbation postdischarge in hospitalized patients with AECOPD
Received 21 April 2015
Accepted for publication 6 July 2015
Published 28 October 2015 Volume 2015:10(1) Pages 2319—2325
DOI https://doi.org/10.2147/COPD.S87091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Maurizio Moretti,1 Stefano Fagnani2
1Respiratory Unit, Massa-Carrara Hospital and University of Pisa, Pisa, Italy; 2Medical Department, Edmond Pharma Srl, Paderno Dugnano, Milan, Italy
Purpose: Mucolytics can improve disease outcome in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). The objectives of this study were to investigate the effects of erdosteine (ER), a mucolytic agent with antioxidant activity, on systemic inflammation, symptoms, recurrence of exacerbation, and time to first exacerbation postdischarge in hospitalized patients with AECOPD.
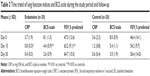
Patients and methods: Patients admitted to hospital with AECOPD were randomized to receive either ER 900 mg daily (n=20) or a matching control (n=20). Treatment was continued for 10 days until discharge. Patients also received standard treatment with steroids, nebulized bronchodilators, and antibiotics as appropriate. Serum C-reactive protein levels, lung function, and breathlessness–cough–sputum scale were measured on hospital admission and thereafter at days 10 and 30 posttreatment. Recurrence of AECOPD-requiring antibiotics and/or oral steroids and time to first exacerbation in the 2 months (days 30 and 60) postdischarge were also assessed.
Results: Mean serum C-reactive protein levels were lower in both groups at days 10 and 30, compared with those on admission, with significantly lower levels in the ER group at day 10. Improvements in symptom score and forced expiratory volume in 1 second were greater in the ER than the control group, which reached statistical significance on day 10. ER was associated with a 39% lower risk of exacerbations and a significant delay in time to first exacerbation (log-rank test P=0.009 and 0.075 at days 30 and 60, respectively) compared with controls.
Conclusion: Results confirm that the addition of ER (900 mg/d) to standard treatment improves outcomes in patients with AECOPD. ER significantly reduced airway inflammation, improved the symptoms of AECOPD, and prolonged time to first exacerbation. The authors suggest ER could be most beneficial in patients with recurring, prolonged, and/or severe exacerbations of COPD.
Keywords: C-reactive protein, mucolytics, time to exacerbation, inflammation, COPD
Introduction
Exacerbations are a significant cause of morbidity in chronic obstructive pulmonary disease (COPD). The course of the disease is characterized by episodes of exacerbation with seasonal variation, defined as events during the natural progress of the disease featuring aggravation of the symptoms that often require a change in the patient’s regular treatment.1 The most frequent causes of acute exacerbations of COPD (AECOPD) are respiratory infections and atmospheric pollution; however, in around one-third of cases the causes are not identified.1 AECOPD can have significant health implications for the patient, such as acceleration of the decline of lung function, deterioration in the quality of life, and increased mortality.2–4 It has been shown that patients with frequent exacerbations have significant airway and systemic inflammation even during the stable phase of the disease.5,6 Exacerbations in more severe disease frequently require hospitalization, with more than 30% of patients experiencing frequent relapses, requiring repeated readmissions to hospital. Indeed, much of the morbidity and mortality in COPD relates to exacerbations.7 Patients who present with frequent relapses in the 2 months following an initial exacerbation after 14 days of treatment have been shown to have significantly higher levels of biomarkers for systemic inflammation, such as C-reactive protein (CRP).8 Exacerbations in more severe disease requiring hospitalization cause considerably distress to the patient and also account for a large proportion of the health care expenditure on the treatment of COPD.9 This has led to a search for strategies to prevent exacerbations and to hasten their resolution when they do occur.
Mucolytics, as adjunctive treatment for both stable and exacerbated COPD, have been used to improve disease outcome, but their precise place in therapy is still under debate.10 Erdosteine (ER) has been approved for the treatment of acute and chronic pulmonary diseases for over 10 years and has been shown to be effective in the treatment of stable and exacerbated chronic bronchitis (CB) and COPD. ER is a prothiol agent with a multifactorial mechanism of action via the presence of free SH groups following metabolization. In experimental studies, it has shown mucolytic activity and inhibition of bacterial adhesiveness to respiratory mucosa; antioxidant activity both in vitro and in vivo; and antioxidant/anti-inflammatory activity in stable COPD.11–15
The objective of this study was to evaluate the effects of ER on systemic inflammation in patients with AECOPD, assessed by changes in levels of serum CRP (a marker of systemic inflammation). In addition, the study evaluated whether the anti-inflammatory effects of ER were associated with clinical efficacy in terms of resolution of symptoms, improvements in pulmonary function, and reduced risk of and time to recurrence of exacerbations.
Materials and methods
Study design
This was a prospective, randomized, controlled, single-blind study conducted from October 2012 at the Respiratory Unit of Massa-Carrara General Hospital, Massa-Carrara, Italy. The study was carried out in accordance with Good Clinical Practice guidelines and conformed with the Declaration of Helsinki 1964, as currently amended. The protocol was approved by the local ethics committee, and all patients gave written informed consent to participate in the study.
Patients
From October 2012 to May 2013, male and female patients (aged between 38 and 75 years) admitted to the Respiratory Unit of Massa-Carrara General Hospital, Massa-Carrara, Italy with an acute exacerbation of COPD, fever, cough, and purulent sputum in the previous 24 hours were eligible for enrollment in the study. Patients were excluded if they had any of the following: pneumonia, acute heart failure, bronchiectasis, asthma (as the primary diagnosis), acute respiratory acidosis needing noninvasive ventilation, AECOPD treated with antibiotics or systemic corticosteroids in the previous 4 weeks, or any other medical or personal problems that in the opinion of the investigator would interfere with the conduct of the study. All patients were vaccinated against seasonal influenza.
Treatment
Patients were randomized to receive either oral ER 300 mg tid for 10 days (kindly provided by Edmond Pharma Srl, Paderno Dugnano, Italy) in combination with standard therapy for AECOPD according to our hospital’s current guidelines or standard therapy alone.
Standard treatment for AECOPD at our hospital was Methylprednisolone 80 mg for 3 days, gradually tapered on day 10, and nebulized salbutamol 5 mg plus ipratropium 0.5 mg four times daily. Intravenous cephalosporin was initially prescribed as all patients had increased sputum volume and purulence, but it was later changed according to the results of the sputum antibiograms. Treatment was continued for 10 days until discharge from hospital. On discharge, patients continued to receive standard treatment with inhaled corticosteroids, long-acting β2-agonists, and anticholinergics.
Outcome measures
The primary endpoint was serum CRP levels as a measure of systemic inflammation during AECOPD and was measured on admission and at days 10 and 30. CRP was measured using a high-sensitivity CRP assay (Beckman Coulter Diagnostics, Brea, CA, USA).
Secondary clinical endpoints included lung function and respiratory symptoms (measured on admission and at days 10 and 30 at the same time each day in the morning and at least 2 hours after inhaled bronchodilators). Spirometry was performed according to European Respiratory Society criteria, while intensity of respiratory symptoms was assessed using the breathlessness–sputum–cough scale (BCS).16,17 Relapse of AECOPD and time to first exacerbation in the first 2 months after discharge were assessed by telephone follow-up. Exacerbations, defined according to Anthonisen criteria, were assessed if changes in therapy with antibiotics and/or oral steroids were required.18
Power calculation
The number of subjects required was estimated using changes in CRP levels. Using differences in CRP levels, it is possible to differentiate between patients “with frequent relapses” and “nonrelapsing” patients.8 The percentage difference between these two groups, in terms of variations of CRP during an exacerbation was approximately 35% (day 10), which can therefore be considered a clinically significant value. Based on these data, it was estimated that 20 patients per group were required to demonstrate a 35% difference (standard deviation 38%), with α=0.05 (two digits) and a power of 80%.
Statistical analysis
All clinical variables were analyzed as changes from baseline values using paired samples t-test. Analysis of variance was used to compare the two treatment groups, while χ2 test was used to compare the difference in percentages between groups. We constructed Kaplan–Meier curves of the probability of exacerbation-free status. Time-to-event analyses were performed with the use of the log-rank test. Cox regression analysis was used to estimate hazard ratios with 95% confidence interval (CI) for the predictors of reexacerbations (such as smoking status, age, sex, CRP, and concomitant treatment) adjusted for each other. All hypothesis tests were two sided, and P<0.05 was defined as significant. The analyses were carried out using IBM SPSS Statistics for Windows Version 20.0 (IBM Corporation, Armonk, NY, USA).
Results
A total of 40 hospitalized patients were eligible for inclusion in the study. Overall, 20 patients received ER 900 mg/d in addition to standard therapy for AECOPD, and 20 patients received standard therapy alone. Demographic and clinical characteristics of patients in the two groups (age, smoking history, lung function, arterial blood gases, BCS scale, duration and severity of COPD, and self-reported exacerbations during the 12 months before screening, comorbidities) were similar at baseline (Table 1). Few patients reported two or more exacerbations annually (six patients in ER group and five patients in control group). Among patients reporting two or more exacerbations in the year before enrollment, only five had relapse of exacerbations in the 2-month study period.
All patients had fever and the major symptoms of AECOPD, requiring hospitalization as evidenced by high BCS scale. All patients completed the study protocol.
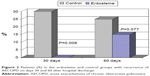
Mean serum CRP concentrations were significantly and progressively lower in both groups on days 10 and 30 when compared with levels on hospital admission. CRP levels in the ER and control group were significantly different on day 10, with patients receiving ER having lower levels of this inflammatory marker (P=0.003) (Figure 1). Mean changes in lung function and BCS score from the beginning to the end of the study were greater in patients treated with ER compared with control group, with statistically significant differences occurring at day 10 (Table 2). All patients were discharged on day 10 of hospitalization after a significant reduction in serum CRP concentrations and a complete recovery from AECOPD. There were no differences between groups in the bronchodilator treatment continued at home.
  | Figure 1 Changes in mean serum CRP levels during the study and at follow-up. |
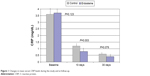
A significantly greater percentage of patients in the control group had exacerbations at day 30 (P=0.008) and day 60 (P=0.077) after hospital discharge, compared with those in the ER group (Figure 2). The percentage of patients with reexacerbation on day 60 was 40.0 and 15.0 in the control and ER groups, respectively. ER was associated with a 39.1% reduction of risk of exacerbation and a significant delay in time to first exacerbation. Kaplan–Meier analysis showed a different time course of exacerbations in the follow-up 2 months after discharge for the ER and control groups (log-rank test P=0.009 at day 30 and log-rank test P=0.075 at day 60) (Figure 3). ER was well tolerated, and no adverse events due to treatment were reported.
  | Figure 3 Probability of being exacerbation free in the erdosteine and control groups at days 30 and 60 after hospital discharge. |
Discussion
The study shows that 10 days of treatment with ER (900 mg daily) in hospitalized patients with AECOPD was associated with a significant decrease in serum CRP concentrations, faster improvement in lung function and symptom scores, and a decrease in early relapses of AECOPD compared to the control group. Our results are in line with those of previous studies investigating the effects of ER in acute exacerbations of CB and COPD, which showed a faster clinical response in patients receiving active treatment compared to those receiving placebo.19,20 Clinical symptoms such as breathlessness, cough, and sputum viscosity improved more quickly in patients treated with the combination of amoxicillin and ER (600 mg/d) compared with those receiving antibiotics alone.20 In addition, in the study reported by Ricevuti et al19 7 days of treatment with ER (900 mg/d) together with amoxicillin significantly increased sputum antibiotic concentration and improved symptoms when compared with the group receiving antibiotic alone. There have been a number of studies investigating the effects of different mucolytics in acute exacerbations of CB/COPD. All of these studies have certain limitations concerning fully validated endpoints; further none of the products studied had consistent effects on resolution of CB/COPD exacerbations, although these drugs had proven in vitro antioxidant activity.21,22,31,32 In this study, we decided to administer high dose ER (900 mg/d) as preliminary data indicated increased clinical effects with higher dose ER. In fact, serum CRP concentrations significantly decreased in the ER and control group at days 10 and 30 compared to baseline levels, with the difference between groups significantly in favor of ER at day 10 (Figure 1).
In general, AECOPD is accompanied with a significant increase in systemic and airway inflammation, of which CRP is a reliable marker. More specifically, CRP significantly increases at the onset of an exacerbation, and the absence of renormalization after treatment is associated with a greater frequency of relapses.23 We contend that the significant decrease in CRP following treatment with ER is due to its antioxidant/anti-inflammatory properties, previously shown in patients with stable COPD.15 Results of the present study demonstrate the positive effects of ER treatment in significantly reducing serum CRP – a biomarker for systemic inflammation. This is the first clinical trial to provide direct evidence of the anti-inflammatory activity of ER in AECOPD.
The study by Dal Negro et al15 in stable COPD patients showed that 10 days of treatment with ER (900 mg/d) rapidly reduced reactive oxygen species (ROS) in peripheral blood, with a maximal effect measured after 4 days of treatment, while the effect of placebo was negligible over the entire treatment period. Furthermore, the reduction in ROS levels observed in ER-treated patients was maintained over the entire treatment period, with significant differences recorded up to day 10 of treatment. Proinflammatory cytokines specifically involved in oxidative stress in mild COPD were also altered following treatment with ER.15 In the 30 days after hospital admission, mean CRP concentrations were significantly reduced in both groups according to the recovery from acute exacerbation, with a lower (not statistically significant) mean value in the ER group. This finding is in line with the progressive recovery from exacerbation and the discontinuation of ER after 10 days. BCS scale and lung function showed a similar trend with the rate of improvement of BCS scale and forced expiratory volume in 1 second% predicted greater in patients treated with ER compared to control, with statistically significant differences at day 10.
We consider that these clinical results are related to the multifactorial mechanism of action of ER (mucolytic, antibacterial, and antioxidant activity) via the free SH group.12,14,15,24 Relapse of AECOPD occurred in 25% of the study population in the 2 months after hospital discharge. A significantly higher percentage of patients in the control group had exacerbations, requiring antibiotics and/or steroids in the control group compared with ER group after 30 (P=0.008) and 60 days (P=0.077), respectively. These results are not related to the clinical phenotype of enrolled COPD patients since there was no difference between groups in mean number of self-reported exacerbations during the 12 months before screening. Furthermore, ER was associated with a 39.1% reduction of risk of exacerbation and a significant delay in time to first exacerbation (Figure 3). Active treatment with ER had a significant impact on 60 days exacerbation rate (hazard ratio 0.169, 95% CI =0.033–0.875, P=0.034). Observational data have suggested that the risk of a second exacerbation is higher in the period immediately after an initial exacerbation, with a UK national audit showing that 34% of 1,221 patients hospitalized for exacerbations were readmitted in the subsequent 3 months.25 Exacerbations are not, as previously thought, random events, but tend to cluster together.26 The persistence of elevated systemic inflammation, a probable indicator of a nonoptimal response to therapy, seems to be a predictor of such negative development. COPD patients with relapses in the 2 months following exacerbation had significantly higher levels of biomarker indicators of systemic inflammation, such as CRP, after 14 days of treatment.8
In the present study, the risk of relapses was lower with ER, while time to first exacerbation was shorter in the control group. These data were associated with a faster decline of serum CRP concentrations with ER, significant after 10 days prior to stopping active treatment. The lower concentrations of serum CRP in the ER group compared with the control group on day 30 had a significant impact on the 60 days exacerbation rate (hazard ratio 27.5, 95% CI =4.27–176.8, P<0.001).
Conclusion
The results of our study confirm that 10 days of treatment with ER (900 mg/d) is effective in hospitalized patients with AECOPD receiving standard treatment with corticosteroids and antibiotics. ER significantly reduced serum CRP concentrations and hastened recovery of acute respiratory symptoms and lung function compared to controls. Our results demonstrate the benefits of adding ER, due to its anti-inflammatory action and the potential to reduce ROS released from inflammatory cell, into the standard therapeutic regimen for AECOPD.27,28 These data also confirm previous positive outcomes with ER plus antibiotic in AECOPD compared with antibiotic treatment alone.19
Importantly, the results also confirm a reduction of risk of relapse of AECOPD and prolonged time to the first exacerbation with ER compared to control group. Once again, our data are similar to those obtained with long-term ER in patients with stable COPD. ER reduced significantly the rate of exacerbation and hospitalization and improved patients’ quality of life when administered for 8 months during the winter season in patients with moderate and/or severe COPD.29 We conclude that there is good clinical evidence of the anti-inflammatory activity of ER in both acute and chronic COPD. The present study indicates that a higher dose of ER (900 mg/d) can be safely prescribed as add-on therapy in AECOPD to accelerate the clinical response.
Further, appropriately sized studies with longer follow-up should be undertaken to reinforce the present results and better define the longer term benefits of ER in patients with AECOPD.
Acknowledgment
Medical writing assistance was provided by Editamed srl (Torino, Italy) and was funded by Edmond Pharma Srl (Milan, Italy).
Author contributions
Both authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
MM participated in multicenter clinical trials on erdosteine sponsored by Edmond Pharma Srl; he has received financial reimbursement from Edmond Pharma Srl for providing lecture services. SF is full-time employee of Edmond Pharma Srl. The authors report no other conflicts of interest in this work.
References
Donaldson GC, Wedzicha JA. The causes and consequences of seasonal variation in COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2014;9:1101–1110. | ||
Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852. | ||
Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:1418–1422. | ||
Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60:925–931. | ||
Bhowmik A, Seemungal TA, Sapsford RJ, Wedzicha JA. Relation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbations. Thorax. 2000;55:114–120. | ||
Gan WQ, Man SF, Senthilselvan A. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–580. | ||
Garcia-Aymerich J, Farrero E, Félez MA, Izquierdo J, Marrades RM, Antó JM. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax. 2003;58:100–105. | ||
Perera WR, Hurst JR, Wilkinson TM, et al. Inflammatory changes, recovery and recurrence at COPD exacerbation. Eur Respir J. 2007;29:527–534. | ||
Wouters EF. Economic analysis of the confronting COPD survey: an overview of results. Respir Med. 2003;97(Suppl C):S3–S14. | ||
Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. | ||
Marchioni CF, Moretti M, Muratori M, et al. Effects of erdosteine on sputum biochemical and rheologic properties: pharmacokinetics in chronic obstructive lung disease. Lung. 1990;68:285–293. | ||
Braga PC, Dal Sasso M, Sala MT, Gianelle V. Effects of erdosteine and its metabolites on bacterial adhesiveness. Arzneimittelforschung. 1999;49(4):344–350. | ||
Braga PC, Dal Sasso M, Zuccotti T. Assessment of the antioxidant activity of the SH Metabolite I of erdosteine on human neutrophils respiratory bursts. Arzneimittelforschung. 2000;50(8):739–746. | ||
Moretti M, Marchioni CF. An overview of erdosteine antioxidant activity in experimental research. Pharmacol Res. 2007;55(4):249–254. | ||
Dal Negro RW, Visconti M, Micheletto C, Tognella S. Changes in blood ROS, e-NO, and some pro-inflammatory mediators in bronchial secretions following erdosteine or placebo: a controlled study in current smokers with mild COPD. Pulm Pharmacol Ther. 2008;21(2):304–308. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | ||
Leidy NK, Rennard SI, Schmier J, Jones MK, Goldman M. The breathlessness, cough and sputum scale: the development of empirically based guidelines for interpretation. Chest. 2003;124(6):2182–2191. | ||
Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbation of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106(2):196–204. | ||
Ricevuti G, Mazzone A, Uccelli E, Gazzani G, Fregnan GB. Influence of erdosteine, a mucolytic agent, on amoxicillin penetration into sputum in patients with an infective exacerbation of chronic bronchitis. Thorax. 1988;43(8):585–590. | ||
Marchioni CF, Polu JM, Taytard A, Hanard T, Noseda G, Mancini C. Evaluation of efficacy and safety of erdosteine in patients affected by chronic bronchitis during an infective exacerbation phase and receiving amoxicillin as basic treatment (ECOBES, European Chronic Obstructive Bronchitis Erdosteine Study). Int J Clin Pharm Ther. 1995;33(11):612–618. | ||
Langlands JH. Double-blind clinical trial of bromhexine as a mucolytic drug in chronic bronchitis. Lancet. 1970;1(7644):448–450. | ||
Black PN, Morgan-Day A, McMillan TE, Poole PJ, Young RP. Randomised, controlled trial of N-acetylcysteine for treatment of acute exacerbations of chronic obstructive pulmonary disease [ISRCTN21676344]. BMC Pulm Med. 2004;4:13. | ||
Hurst JR, Donaldson GC, Perera WR, et al. Use of plasma biomarkers at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174(8):867–874. | ||
Moretti M. Pharmacology and clinical efficacy of erdosteine in chronic obstructive pulmonary disease. Expert Rev Respir Med. 2007;1:307–316. | ||
Roberts CM, Lowe D, Bucknall CE, Ryland I, Kelly Y, Pearson MG. Clinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2002;57(2):137–141. | ||
Hurst JR, Donaldson GC, Quint JK, Goldring JJ, Baghai-Ravary R, Wedzicha JA. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179(5):369–374. | ||
Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet. 1999;354(9177):456–460. | ||
Wood-Baker R, Walters EH, Gibson P. Oral corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2001;2:CD001288. | ||
Moretti M, Bottrighi P, Dallari R, et al. The effect of long-term treatment with erdosteine on chronic obstructive pulmonary disease: the EQUALIFE Study. Drugs Exp Clin Res. 2004;30(4):143–152. | ||
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. | ||
Maesen FP, Davies BI, Brouwers J, Rubingh G. Erythromycin and bromhexine in acute exacerbations of chronic bronchitis. A study on sputum penetration and clinical effectiveness. Eur J Respir Dis. 1982;63(4):325–329. | ||
Finiguerra M, Conti P, Figura I, Legnani W, Morandini GC. Clinical study on the effects of an antibiotic and mucolytic association (amoxicillin and domiodol) in hypersecretory chronic bronchopulmonary diseases. Curr Ther Res.1982;31:895–905. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.