Back to Journals » Clinical Epidemiology » Volume 13
Epidemiology of Vitiligo – A Dual Population-Based Approach
Authors Mohr N , Petersen J, Kirsten N , Augustin M
Received 28 January 2021
Accepted for publication 15 April 2021
Published 26 May 2021 Volume 2021:13 Pages 373—382
DOI https://doi.org/10.2147/CLEP.S304155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Irene Petersen
Nicole Mohr, Jana Petersen, Natalia Kirsten, Matthias Augustin
Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany
Correspondence: Nicole Mohr
Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Martinistraße 52, Hamburg, D-20246, Germany
Tel +49-40-7410-55428
Fax +49-40-7410-5348
Email [email protected]
Background: Most epidemiological data on vitiligo refer to selected environments or focus on the prevalence of comorbidity unrelated to the population.
Objective: Aim of the study was to gain robust representative prevalence data on vitiligo and on associated dermatologic comorbidity in the German adult population.
Methods: A dual population-based approach was applied with 1) primary data obtained between 2004 and 2014 from dermatological exams in the general working population; 2) claims data from a large German statutory health insurance, reference year 2010.
Results: In the working cohort (N = 121,783; 57% male; mean age 43 years), the prevalence of vitiligo was 0.77% (0.84% in men; 0.67% in women). In the claims data (N = 1,619,678; 38% male; mean age 46 years), prevalence was 0.17% (0.14% in men; 0.18% in women). In the working cohort, vitiligo was significantly more common in people with fair skin type, ephelides and port-wine stains and less common in people with acne and solar lentigines. In the claims data, vitiligo was associated with a variety of skin conditions, eg, atopic dermatitis, psoriasis and alopecia areata.
Conclusion: The resulting discrepancy of claims vs primary data between 0.17% and 0.77% indicates the most probable spectrum of vitiligo prevalence in Germany. It is more frequently observed in clinical exams than recorded in claims data, indicating a marked proportion of people seeking no medical help. Such nonattendance may result from the fact that many treatment options do not provide satisfying benefits to the patients.
Keywords: pigmentation, health services research, public health research, prevalence, comorbidity
Introduction
Vitiligo is a chronic skin condition associated with a loss of pigmentation in the epidermis.1 To many people affected, the visibility of the lesions is perceived as disfiguring and burdensome.2–4 Accordingly, there is a high level of psychological strain2,5 as well as of patient needs for treatment.6 In spite of this there has been little attention to the disease from the perspective of population-based epidemiology. Most of the epidemiological data on vitiligo either refer to strongly selected environments like hospital populations7 or focus on the prevalence of comorbidity of people affected from vitiligo8–10 without associating the general public. Studies commenting on dermatologic comorbidity mostly suggest association of vitiligo with atopic dermatitis, alopecia areata and psoriasis.11–15
A study from South Korea revealed a prevalence of 0.12% to 0.13% over a three year period in a population of people admitted to hospitals.15 In a population-based cohort study from China the overall prevalence of vitiligo was 0.56% (0.71% in men vs 0.45% in women) and increased with age.12 In a literature review, Krüger and Schallreuter16 identified more than fifty studies describing the prevalence of vitiligo in a range between 0.06% and 2.28%. The population-based study conducted in France by Richard et al, in which a prevalence of 0.46% was reported, also lies in this range.17
In total, the data on the population-based epidemiology of vitiligo show large variations which may depend on different populations and ethnicities observed but also on different evaluation methods used. In addition to these cross-national specificities, there are also potential selection mechanisms at the national level that influence the observed prevalence. In Germany, claims data resulting from physician consultations are a widely used population-based data source. In case of vitiligo, however, many patients after years of frustrating treatment attempts do not seek medical attention,18 which might lead to an underestimation of the true prevalence. For this reason, it may be useful to supplement the claims data with further data sources.
In order to obtain representative population-based data on the prevalence of vitiligo and to get control on selection bias of the claims data, the current study investigated two large data sources which represent significant proportions of the German general population. The research questions were as follows:
- What is the prevalence of vitiligo in the adult population in the data sources?
- Is there any particular dermatologic comorbidity associated with vitiligo?
- How can differences in the observed results be explained by selective effects?
- Do these differences provide information about the healthcare situation and possible healthcare needs?
Materials and Methods
Large-Scale Dermatological Examinations in Employees
Primary data from the general working population were gained from large scale skin screenings in >300 German companies as described previously.19–23 All employees between 16 and 70 years were voluntarily invited to participate in skin examinations free of charge in their companies. The screenings were conducted between 2004 and 2014 nationwide in companies from different branches. All employees, regardless of gender or social status, were invited to participate. Examinations took place within the working hours. Whole body examinations were performed by trained dermatologists and all findings were recorded by assistants in an electronic data system. For a series of dermatological conditions, it was documented whether they are prevalent and whether there is a need for treatment. In the latter case, employees were referred to a dermatologist. Moreover, a structured questionnaire for history of skin diseases and medication was used.
Secondary Claims Data from a Nationwide Sick Fund
For the present analysis, data of the DAK-Gesundheit (DAK-G), a nationwide operating health insurance company, were used. The statutory health insurance (SHI) is essential within the German healthcare system: about 90% of the German population (approx. 72 million) is insured with one of the 110 SHI companies (in 2018). The remaining 10% are privately insured.24,25 The routine data are available for a 40% representative sample of all insured people of the DAK-G on December 31, 2010. This is around 2.4 million insured persons. The data contains all billing-relevant information from the outpatient and inpatient sector, including work incapacity data and all outpatient-prescribed drugs. These also comprise all outpatient contacts with physicians, coded diagnoses, billed services and the time specification of the doctor visit at quarterly level. All information on prescribed and delivered drugs as well as information on the prescribing specialist group are available, too. The insured person’s master data contain socio-demographic information on age and gender, start and end of time of insurance. All service areas are to be linked with each other via a pseudonym.
On the basis of the DAK-G population, a cohort of prevalent patients with vitiligo was selected. The subsequent inclusion criteria provide the basis for sampling prevalent vitiligo patients in 2010:
- Insurees who were insured on December 31, 2010 at the DAK-G
- Aged 16–70 years in 2010
- One assured diagnosis of vitiligo (ICD-Code: L80) in the outpatient sector or one main or secondary hospital diagnosis in 2010
For analysing dermatological comorbidities, we examined insured people who show at least one assured diagnosis in the outpatient sector or one main or secondary diagnosis in the hospital sector. Diagnoses of frequent or typical skin conditions from a predefined list were identified by ICD-10 codes.
Statistics
Statistical analysis of primary data gathered from the occupational screenings was performed using SPSS (IBM, Armonk, New York, US) version 23 for Windows. The screenings were conducted between 2004 and 2014, only once a person. Thus, point-prevalence rates and their 95% confidence intervals were calculated. Group differences were tested by means of chi-squared tests. To explore the association of vitiligo with further dermatological conditions controlling for age, gender and skin type a logistic regression analysis was conducted. Missing data on skin disease were rated as not prevalent. In some cases, skin type was not explicitly specified, these cases were excluded from the respective subgroup analyses.
For secondary sick fund data, we performed all statistical analyses using SAS (SAS Institute Inc, Cary, North Carolina, US) version 9.4 for Windows. The prevalence data of the DAK-G were standardised according to age and gender to the indicators of the German population in 2012.26 One-year prevalence rates (reference year 2010) and their 95% confidence intervals (CI) were calculated. Furthermore, a multivariate logistic regression was conducted for secondary data. Our dependent variable was defined as at least one diagnosis of L80 in 2010. Our independent variables were age (continuous) and sex (female or male) and defined comorbidities (yes/no).
Results
Prevalence of Vitiligo
Working Cohort
In the primary cohort a total of 121,783 persons (43.5% female, mean age 43.1 ± 10.8 years) was clinically examined by a dermatologist (Table 1). Fair skin (skin type I and II on the Fitzpatrick scale) was present in 74.9% of the total sample (71.6% in men, 79.1% in women).
 |
Table 1 Cohort of People with (n = 933) and without (n = 120,850) Vitiligo Examined in the Companies by Dermatologists |
The prevalence of vitiligo in this primary cohort was 0.77% including 0.84% for men and 0.67% for women. Prevalence was significantly higher in older people, men (Figure 1) and fair skin (type I and II on the Fitzpatrick scale).
 |
Figure 1 Point-prevalence of vitiligo in the working cohort (N = 121,783) and one-year prevalence in the claims data (N = 1,619,678), stratified by age and gender. |
Claims Data Cohort
A total of 1,619,678 persons aged 16–70 years (61.8% female, mean age 45.8 ± 15.6 years) were insured on December 31, 2010 at the DAK-G. Of them, 2689 had at least one relevant vitiligo-diagnosis in 2010 indicating an overall nonstandardised prevalence of 0.17% (0.14% in men and 0.18% in women). People with vitiligo were on average older and more often female (Table 2, Figure 1). Age- and gender-adjusted prevalence rates standardised to the German population in 2012 were 0.15% in total, 0.13% in men and 0.18% in women. Figure 1 demonstrates that the one-year prevalence identified in the claims data cohort was lower than the point-prevalence from the working cohort. This was the case in all age groups and for both men and women.
 |
Table 2 Cohort of People with (n = 2689) and without (n = 1,616,989) Vitiligo in the Claims Data |
Dermatologic Comorbidity of Vitiligo
Working Cohort
In the primary cohort investigated by dermatologists there was a significant positive association of vitiligo with port-wine stains and negative associations with acne and solar lentigines (Table 3).
In the logistic regression analysis, controlling for age, gender and skin type, the significant negative association of vitiligo with acne and solar lentigines as well as the association with port-wine stains were confirmed. Additionally, ephelides were found to be associated with vitiligo (Table 4). Apart from that, higher age led to a higher frequency of vitiligo as well as being male and fair skin type (type I and II on the Fitzpatrick scale).
 |
Table 4 Predictors and Their ORs of the Logistic Regression Model, Dependent Variable: Presence of Vitiligo Among Working People in German Companies (n = 120,833) |
Claims Data Cohort
The prevalence rates of selected comorbidities were compared between insured people with and without vitiligo. As one can see in Table 5, the sick fund cohort vitiligo was significantly associated with higher levels of atopic dermatitis, psoriasis, lichen planus, alopecia areata, androgenic alopecia, other nonscarring hair loss, malignant melanoma, other and unspecified malignant neoplasm of skin, other disorders of pigmentation, acne vulgaris, congenital nonneoplastic nevus, other melanin hyperpigmentation and xerosis cutis.
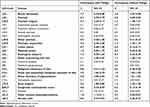 |
Table 5 Prevalence of Dermatologic Comorbidity in People with (n = 2689; Mean Age 50.0 Years) vs without Vitiligo (n = 1,616,989; Mean Age 45.8 Years), Non-adjusted Claims Data |
In the logistic regression model (Table 6), age and gender were associated with vitiligo-diagnosis when controlling for all other variables. The significant positive association with atopic dermatitis, psoriasis, lichen planus, alopecia areata, other nonscarring hair loss, other and unspecified malignant neoplasm of skin, other disorders of pigmentation, acne vulgaris and congenital nonneoplastic nevus could be confirmed also. Only other melanin hyperpigmentation was negatively associated with vitiligo.
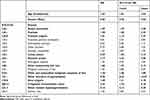 |
Table 6 Logistic Regression Model (Odds Ratios) for Factors Associated with Vitiligo-Diagnosis, Dependent Variable: Assured ICD-Diagnosis of Vitiligo (L80) in the Claims Data |
Discussion
Prevalence
The objective of the current study was to assess the prevalence and dermatologic comorbidity of vitiligo in the adult general population. To do so, two different data sources were used. They revealed remarkable differences between the cohorts, possibly reflecting the general difference between claims data and findings based directly on dermatological examinations. Even though one-year prevalence rates were calculated in the claims data, the resulting prevalence was lower than the point-prevalence in the screening data. In this context, a potential selection bias of claims data, eg, due to nonattendance to medical care, needs to be discussed. Such nonattendance may result from the fact that many treatment options do not provide satisfying response to the patients.18,27 An unfulfilled treatment need due to dissatisfaction with care and a high emotional burden was just recently identified by Narayan et al.28 Moreover, in the general population vitiligo is significantly more frequent in men whereas in the claims data women were significantly more frequently presented. This discrepancy that was found in both the group comparisons and in the logistic regression analyses may result from the fact that women are more concerned with vitiligo as shown in previous publications.4,6 Thus, disease burden and resulting motivation for medical attendance could be higher in women. All in all, both reported prevalence rates in this paper (0.2% in the claims data and 0.8% in the working cohort) correspond to the rates provided by the most relevant and comparable studies16,17,29 and thus suggest a certain validity of the data sources.
Comorbidity
The data sources also provided differing results with regard to dermatological comorbidity. Since regression analyses were applied to control for age and gender effects, it can be assumed that these differences are more likely to be justified by the described selection effects. Generally, it needs to be noted that we analysed cross-sectional data and therefore are not able to make statements on causality but rather on associations. Relevant findings related to dermatological comorbidity in the claims data were the higher prevalence of chronic inflammatory skin conditions (eg, atopic dermatitis, psoriasis, lichen planus), autoimmune disease (alopecia areata), nonscarring hair loss and other disorders of pigmentation and unspecified malignant neoplasm of the skin. These findings as well as the inverse association with other melanin hyperpigmentations (ICD-10 code) fit into previous single publications.11–15 Remarkably, these associations probably reflect the common autoinflammatory character of these diseases, which, though different in immunopathological mechanisms, show common features of autoimmunity as has been described as multiple autoimmune syndrome (MAS).30,31 Also the observed associations of vitiligo and congenital nevi are consistent with primary research. Eg, in accordance with our findings in the claims data, a study by van Geel et al using a cohort of 1004 patients with vitiligo described a triple higher prevalence (3%) of congenital nonneoplastic naevi compared to the control group (1%),32 suggesting a common pathogenic link, which, however, is not fully understood.33 These results were only partially verified in the primary data of the working cohort. Here, the regression analysis controlling for age and gender revealed a few disorders as positively associated with vitiligo (ephelides, port-wine stains) whereas a few others were inversely correlated (solar lentigines, acne). The interpretation of these statistically significant findings is still open for further investigations.
Strengths and Limitations
In the claims data diagnoses derived from physicians in routine care, a large proportion of whom were dermatologists. Due to the secondary nature of this data source, there is no chance of verifying these diagnoses. In the large-scale company-based examinations, it has been assured that trained dermatologists performed the skin examinations. They used dermatoscopy but no wood lights in the investigations. Thus, in single cases an under- or even overestimation may have occurred.
Another potential source of uncertainty could be the clinical differentiation between vitiligo and vitiligo-like leukoderma which can hardly be based on morphological features only.34 It is conceivable that single patients have developed a vitiligo-like leukoderma within the framework of an immunological reaction and that this has been misdiagnosed in our cohort as classical vitiligo. With a cumulative indication of 3.4% in patients with stage III and stage IV melanoma, vitiligo-like leukoderma is a rare immunological response. In our cohort, there were only 22 (0.8%) patients with melanoma in total so the risk of a relevant misdiagnosis of vitiligo-like eruption seems rather unlikely.
Further limitations derive from the fact that the primary data are solely based on patients volunteering for the participation. However, the cohort of more than 120,000 persons is sufficient to reflect a substantial proportion of the population. A limitation of the secondary data is the reduction of documented cases to people attending medical services. For this reason the claims data were related to the primary data. Overall, these data reflect the situation in Mid-European countries like Germany. Results in countries with a higher proportion of people having dark skin may be different since people with darker skin show more visible vitiligo and thus potentially higher burden.
Conclusions
In total, these large-scale data from two independent cohorts and settings confirm that Vitiligo is a relatively frequent disease associated with relevant comorbidity. The resulting discrepancy of claims vs primary data between 0.17% and 0.77% indicates the most probable spectrum of vitiligo prevalence in Germany. It is more frequently observed in clinical exams than recorded in claims data, indicating a marked proportion of people seeking no medical help. Such nonattendance may result from the fact that many treatment options do not provide satisfying benefits to the patients, which underlines the need for treatment among patients with vitiligo. Further studies should additionally differentiate the phenotype and the patient burden of vitiligo.
Data Sharing Statement
Primary data from the occupational screenings are available upon reasonable request. The datasets generated for the claims data cohort are not available as the use of claims data is restricted to defined persons.
Ethics Approval
The study was conducted according to the principles expressed in the Declaration of Helsinki. We took the criteria of a National Good Practice Guideline into consideration. According to the Good Practice of Secondary Data Analysis, no approval of an ethical committee is required.
Acknowledgments
We gratefully thank Katharina Müller for her valuable assistance and contribution to the current paper and the Scientific Communication Team of the IVDP, in particular Merle Twesten and Mario Gehoff, for copy editing. We thank the DAK-G and Heigel GmbH for providing the data analysed in this study.
Disclosure
Prof Matthias Augustin has served as consultant and/or paid speaker for and/or has received research grants and/or honoraries for consulting and/or scientific lectures for and/or got travel expenses reimbursed and/or participated in clinical trials sponsored by companies that manufacture drugs including Abbott/AbbVie, ALK Scherax, Almirall, Amgen, Beiersdorf, Biogen Idec, BMS, Boehringer Ingelheim, Celgene, Centocor, Dermira, Eli Lilly, Forward Pharma, Fresenius, Galderma, GSK, Hexal, Incyte, Janssen-Cilag, LEO Pharma, Lilly, Medac, Menlo, Merck, MSD, Mylon, Novartis, Pfizer, Regeneron, Sandoz, Sanofi-Aventis, Stallergenes, Stiefel, Teva, TK, Trevi, UCB and Xenoport outside the submitted work. Dr Natalia Kirsten reports personal fees from AbbVie, personal fees, non-financial support from Novartis, personal fees, non-financial support from Leo, Eli Lilly, UCB, Pfizer, and Celgene, outside the submitted work. The authors declare that they have no other conflicts of interest in this work.
References
1. Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE; Vitiligo Working Group. New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77(1):1–13. doi:10.1016/j.jaad.2016.10.048
2. Elbuluk N, Ezzedine K. Quality of life, burden of disease, co-morbidities, and systemic effects in vitiligo patients. Dermatol Clin. 2017;35(2):117–128. doi:10.1016/j.det.2016.11.002
3. Morrison B, Burden-Teh E, Batchelor JM, Mead E, Grindlay D, Ratib S. Quality of life in people with vitiligo: a systematic review and meta-analysis. Br J Dermatol. 2017;177(6):e338–e339. doi:10.1111/bjd.15933
4. Radtke MA, Schäfer I, Gajur A, Langenbruch A, Augustin M. Willingness-to-pay and quality of life in patients with vitiligo. Br J Dermatol. 2009;161(1):134–139. doi:10.1111/j.1365-2133.2009.09091.x
5. Osinubi O, Grainge MJ, Hong L, et al. The prevalence of psychological co-morbidity in people with vitiligo: a systematic review and meta-analysis. Br J Dermatol. 2018;178(4):863–878. doi:10.1111/bjd.16049
6. Augustin M, Gajur AI, Reich C, Rustenbach SJ, Schaefer I. Benefit evaluation in vitiligo treatment: development and validation of a patient-defined outcome questionnaire. Dermatology. 2008;217(2):101–106. doi:10.1159/000128992
7. Marinho Fde S, Cirino PV, Fernandes NC. Clinical epidemiological profile of vitiligo in children and adolescents. An Bras Dermatol. 2013;88(6):1026–1028. doi:10.1590/abd1806-4841.20132219
8. Afkhami-Ardekani M, Ghadiri-Anari A, Ebrahimzadeh-Ardakani M, Zaji N. Prevalence of vitiligo among type 2 diabetic patients in an Iranian population. Int J Dermatol. 2014;53(8):956–958. doi:10.1111/ijd.12148
9. Al-Harbi M. Prevalence of depression in vitiligo patients. Skinmed. 2013;11(6):327–330.
10. Paradisi A, Tabolli S, Didona B, Sobrino L, Russo N, Abeni D. Markedly reduced incidence of melanoma and nonmelanoma skin cancer in a nonconcurrent cohort of 10.040 patients with vitiligo. J Am Acad Dermatol. 2014;71(6):1110–1116. doi:10.1016/j.jaad.2014.07.050
11. Chen YT, Chen YJ, Hwang CY, et al. Comorbidity profiles in association with vitiligo: a nationwide population-based study in Taiwan. J Eur Acad Dermatol Venereol. 2015;29(7):1362–1369. doi:10.1111/jdv.12870
12. Dahir AM, Thomsen SF. Comorbidities in vitiligo: comprehensive review. Int J Dermatol. 2018;57(10):1157–1164. doi:10.1111/ijd.14055
13. Mohan GC, Silverberg JI. Association of vitiligo and alopecia areata with atopic dermatitis: a systematic review and meta-analysis. JAMA Dermatol. 2015;151(5):522–528. doi:10.1001/jamadermatol.2014.3324
14. Silverberg JI, Silverberg NB. Association between vitiligo and atopic disorders: a pilot study. JAMA Dermatol. 2013;149(8):983–986. doi:10.1001/jamadermatol.2013.4228
15. Lee H, Lee MH, Lee DY, et al. Prevalence of vitiligo and associated comorbidities in Korea. Yonsei Med J. 2015;56(3):719–725. doi:10.3349/ymj.2015.56.3.719
16. Krüger C, Schallreuter KU. A review of the worldwide prevalence of vitiligo in children/adolescents and adults. Int J Dermatol. 2012;51(10):1206–1212. doi:10.1111/j.1365-4632.2011.05377.x
17. Richard MA, Corgibet F, Beylot-Barry M, et al. Sex- and age-adjusted prevalence estimates of five chronic inflammatory skin diseases in France: results of the « OBJECTIFS PEAU » study. J Eur Acad Dermatol Venereol. 2018;32(11):1967–1971. doi:10.1111/jdv.14959
18. Radtke MA, Schäfer I, Gajur AI, Augustin M. Clinical features and treatment outcomes of vitiligo from the patients’ perspective. results of a national survey in Germany. Dermatology. 2010;220(3):194–200. doi:10.1159/000275657
19. Augustin M, Herberger K, Hintzen S, Heigel H, Franzke N, Schäfer I. Prevalence of skin lesions and need for treatment in a cohort of 90 880 workers. Br J Dermatol. 2011;165(4):865–873. doi:10.1111/j.1365-2133.2011.10436.x
20. Augustin M, Radtke MA, Herberger K, Kornek T, Heigel H, Schaefer I. Prevalence and disease burden of hyperhidrosis in the adult population. Dermatology. 2013;227(1):10–13. doi:10.1159/000351292
21. Schäfer I, Rustenbach SJ, Zimmer L, Augustin M. Prevalence of skin diseases in a cohort of 48.665 employees in Germany. Dermatology. 2008;217(2):169–172. doi:10.1159/000136656
22. Ständer S, Schäfer I, Phan NQ, et al. Prevalence of chronic pruritus in Germany: results of a Cross-Sectional Study in a sample working population of 11.730. Dermatology. 2010;221(3):229–235. doi:10.1159/000319862
23. Zander N, Schäfer I, Radtke MA, Jacobi A, Heigel H, Augustin M. Dermatological comorbidity in psoriasis: results from a large-scale cohort of employees. Arch Dermatol Res. 2017;309(5):349–356. doi:10.1007/s00403-017-1741-4
24. Busse R, Blümel M. Germany: health system review. Health Syst Transit. 2014;16(2):224.
25. The National Association of Statutory Health Insurance Funds (GKV-Spitzenverband). Together we are 90 percent. annual report 2016. Available from: https://www.gkv-spitzenverband.de/media/dokumente/service_1/publikationen/geschaeftsberichte/GKV_GB2016_Englisch_barrierefrei_02.pdf.
26. Destatis - Federal Statistical Office. Population: Federal states, cut-off date, gender, age years. Available from: https://www-genesis.destatis.de/genesis/online/data;sid=AE5DC519704B990BC2FF46B3810229EA.GO_1_2?operation=abruftabelleBearbeiten&levelindex=1&levelid=1536226140277&auswahloperation=abruftabelleAuspraegungAuswaehlen&auswahlverzeichnis=ordnungsstruktur&auswahlziel=werteabruf&selectionname=12411-0013&auswahltext=%23SGES-GESW%2CGESM&werteabruf=Werteabruf.
27. Migayron L, Boniface K, Seneschal J. Vitiligo, from physiopathology to emerging treatments: a review. Dermatol Ther (Heidelb). 2020;10(6):1185–1198. doi:10.1007/s13555-020-00447-y
28. Narayan VS, Uitentuis SE, Luiten RM, Bekkenk MW, Wolkerstorfer A. Patients’ perspective on current treatments and demand for novel treatments in vitiligo. J Eur Acad Dermatol Venereol. 2021;35(3):744–748. doi:10.1111/jdv.16927
29. Wang X, Du J, Wang T, et al. Prevalence and clinical profile of vitiligo in China: a community-based study in six cities. Acta Derm Venereol. 2013;93(1):62–65. doi:10.2340/00015555-1397
30. Rork JF, Rashighi M, Harris JE. Understanding autoimmunity of vitiligo and alopecia areata. Curr Opin Pediatr. 2016;28(4):463–469. doi:10.1097/MOP.0000000000000375
31. Tatu AL, Ionescu MA. Multiple autoimmune syndrome type 3-thyroiditis, vitiligo and alopecia areata. Acta Endocrinol. 2017;13(1):124–125. doi:10.4183/aeb.2017.124
32. van Geel N, Van Poucke L, Van de Maele B, Speeckaert R. Relevance of congenital melanocytic naevi in vitiligo. Br J Dermatol. 2015;172(4):1052–1057. doi:10.1111/bjd.13444
33. Speeckaert R, Lambert J, Bulat V, Belpaire A, Speeckaert M, van Geel N. Autoimmunity in segmental vitiligo. Front Immunol. 2020;11:568447. doi:10.3389/fimmu.2020.568447
34. Hartmann A, Bedenk C, Keikavoussi P, et al. Vitiligo and melanoma-associated hypopigmentation (MAH): shared and discriminative features. J Dtsch Dermatol Ges. 2008;6(12):1053–1059. doi:10.1111/j.1610-0387.2008.06755.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

