Back to Journals » Infection and Drug Resistance » Volume 16
Epidemiology and Factors Associated with Treatment Success of Invasive Fungal Infections Among Newly Hematologic Malignancy Patients Receiving Chemotherapy or Hematopoietic Stem Cell Transplant in Thailand
Authors Weeraphon B, Nakaranurack C, Jutivorakool K, Puttilerpong C
Received 26 January 2023
Accepted for publication 28 March 2023
Published 5 April 2023 Volume 2023:16 Pages 2029—2042
DOI https://doi.org/10.2147/IDR.S405810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Benjabhorn Weeraphon,1,2 Chotirat Nakaranurack,3 Kamonwan Jutivorakool,4 Chankit Puttilerpong3,5
1College of Pharmacotherapy of Thailand, Nonthaburi, Thailand; 2Department of Pharmacy Practice and Pharmaceutical Care, Faculty of Pharmaceutical Science, Burapha University, Chonburi, Thailand; 3Department of Pharmacy Practice, Faculty of Pharmaceutical Sciences, Chulalongkorn University, Bangkok, Thailand; 4Division of Infectious Diseases, Department of Medicine, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand; 5Center of Excellence in Bioactive Resources for Innovative Clinical Applications, Chulalongkorn University, Bangkok, Thailand
Correspondence: Chankit Puttilerpong, Department of Pharmacy Practice, Faculty of Pharmaceutical Sciences, Chulalongkorn University, Bangkok, Thailand, Email [email protected]
Purpose: Invasive fungal infection (IFI) causes disability/death in patients with hematologic malignancy (HM) receiving chemotherapy or hematopoietic stem cell transplant (HSCT). There is limited epidemiological data, treatment outcomes, and factors associated with IFI treatment success in Thailand. This study aimed to identify factors associated with IFI treatment success among new HM patients receiving chemotherapy or HSCT, determine IFI incidence among HM patients receiving chemotherapy or HSCT, and the IFI incidence of a breakthrough in patients receiving primary antifungal prophylaxis, and identify antifungal drugs susceptibility.
Patients and Methods: This study reviewed the charts of patients aged ≥ 15 years with newly HM who received chemotherapy or HSCT between January 2016 and June 2021 at King Chulalongkorn Memorial Hospital, Bangkok, Thailand. The 2020 EORTC/MSG criteria were used to diagnose IFI. IFI treatment success factors were evaluated using logistic regression.
Results: Ninety-two patients with 107 episodes of IFI met the inclusion criteria. IFI incidence on proven and probable cases among newly HM patients receiving chemotherapy or HSCT was 7%. Most infections (38.3%) occurred during the induction-phase chemotherapy. Aspergillosis (35.5%) was the commonest IFI, followed by candidiasis (11.2%), Pneumocystis jirovecii pneumonia (8.4%), mucormycosis (3.7%), and others, respectively. The 12-week IFI treatment success rate was 67.3%. It was associated with age < 60 years, absence of coinfection, and the receipt of appropriate empirical therapy on the first day of IFI diagnosis. The incidence of breakthrough IFI from proven and probable cases in patients receiving primary antifungal prophylaxis was 6.1%. Most fungal pathogen isolates were still highly susceptible to antifungal drugs.
Conclusion: The IFI treatment success in patients with HM or HSCT in our study was high. Close monitoring of coinfected patients aged ≥ 60 is recommended. Appropriate antifungal drugs are essential for clinical outcomes.
Keywords: epidemiology, hematologic malignancy, invasive fungal infections, Thailand, treatment outcomes
Introduction
Invasive fungal infection (IFI) remains a significant cause of morbidity and mortality in high-risk patients, especially patients with hematologic malignancy (HM) or hematopoietic stem cell transplant (HSCT) recipients.1 Patients with HM have the highest risk of IFI because of receiving intensive cytotoxic chemotherapy, and IFI is the leading mortality cause in this group of patients (39%).2 The epidemiology trends of IFI in patients with HM have also changed in recent decades. Aspergillosis is the most common type of IFI, and its incidence, as well as that of mucormycosis, continues to increase, especially in Asia.3 Conversely, the incidence of candidiasis has declined.4 The risk factors for developing IFI in patients with HM have been well studied, but the factors associated with treatment success have been limited. The data on IFI in Thailand are limited,5 and most studies focused on patients with acute myeloid leukemia (AML).6,7 The treatment of IFI is challenging. Accordingly, this study aimed to identify treatment outcomes, factors associated with IFI treatment success, epidemiology, and IFI characteristics in new patients with HM receiving chemotherapy or HSCT in Thailand. We also evaluated the incidence of breakthrough IFI in patients indicated to receive antifungal drugs as primary prophylaxis during chemotherapy or HSCT.
Materials and Methods
Patients and Methods
A retrospective cohort study reviewing the electronic medical records was conducted at King Chulalongkorn Memorial Hospital, a 1993-bed tertiary referral center and teaching hospital in Bangkok, Thailand. The inclusion criteria were as follows: (1) Patients with newly diagnosed HM receiving chemotherapy or HSCT recipients aged ≥ 15 years and hospitalized between January 1st, 2016, and June 30th, 2021, and (2) Patients who were diagnosed with IFI and received IFI treatment. All patients were followed from IFI diagnosis until the 12th week of IFI treatment or to death or loss to follow-up. Patients were excluded if they met the following criteria: (1) Those who refused IFI treatment or received palliative care only, (2) Patients with incomplete data in the electronic medical record, or (3) Patients who were diagnosed with IFI before receiving chemotherapy.
The following data were collected: demographics, patient’s HM underlying information, diagnosis of IFI, antifungal regimen, treatment outcome at the 12th week, and overall survival within 12 weeks after an IFI treatment. The fungal species identification, if requested, was performed by VITEK® 2 AST-YS09 for yeast and by fungal culture or the amplification of fungal DNA by PCR combined with DNA sequencing using biopsy tissue for mold. Antifungal susceptibility testing was performed by Sensititre™ YeastOne™ or E-test® in accordance with the Clinical and Laboratory Standards Institute (CLSI).8,9
Diagnosis, Definition, Primary Prophylaxis, and Management of IFI
This study was limited to patients with newly diagnosed malignancy who were receiving either chemotherapy or autologous or allogeneic stem cell transplant for AML, acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), chronic lymphoid leukemia (CLL), lymphoma, or multiple myeloma (MM).
The 2020 European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria10 were used to diagnose IFI. This revision and updated guideline include Pneumocystis jirovecii pneumonia (PJP) as one type of IFI, differing from the prior guideline.11 The 2008 MSG/EORTC criteria12 were used to define responding to IFI therapy in this study. Our study evaluates the treatment outcomes at the 12th week since the patient received IFI treatment, which has two results: treatment success and treatment failure. If patients cannot be evaluated for treatment outcomes at the 12th week, we evaluate them at the time closest to the 12th week.
The overall incidence of IFI and breakthrough IFI was calculated based on “proven” and “probable” IFI, which was not including “possible” IFI. The definition of breakthrough IFI followed the breakthrough IFI position paper of the Mycoses Study Group Education and Research Consortium and European Confederation of Medical Mycology.13 Disseminated fungal infection was defined as the presence of a fungal pathogen in the blood and any other sterile deep-seated structure or organ infected due to hematogenous seeding. Neutropenia was defined as an absolute neutrophil count of less than 500/ microliter. Active hematologic malignancy was defined as patients who did not respond completely to chemotherapy. Coinfection was defined as other infections (eg, bacterial, viral, Clostridium difficile) during IFI treatment. The appropriate empirical therapy was defined as appropriateness regarding the type of antifungal drugs, dose, administration, and effective spectrum during initial empirical therapy.
Primary antifungal prophylaxis (PAP) was defined as using antifungal drugs to prevent IFI before occurring IFI from mold and yeast. Our institute used the consecutive galactomannan follow-up strategy (before 2018) and then used PAP in induction-phase chemotherapy for AML in 2018 according to the ECIL guideline.14 Primary P. jirovecii prophylaxis was defined as patients receiving anti-pneumocystis drugs (two single-strength cotrimoxazole tablets two or three times per week) before they were diagnosed with PJP. The management of febrile neutropenia was as follows: broad-spectrum antimicrobial drugs (eg, ceftazidime, cefepime, piperacillin–tazobactam) were first administered, followed by escalation to carbapenems if indicated. When patients had suspected symptoms of IFI, all diagnostic workups were performed, including the collection of blood cultures, serology tests for IFI, and computed tomography of the suspected infection organ. Other examinations were performed as indicated. The use of antifungal drugs for empirical or preemptive therapy was based on the suspected pathogen. The environmental situation of the treatment unit at the hematology ward when the patients with HM underwent chemotherapy was facilitated as a portable HEPA filter provided in each room, whereas at the HSCT ward was facilitated as both a positive pressure room and a portable HEPA filter provided in each room.
Statistical Analysis
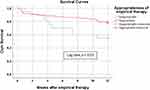
Descriptive statistics were used for all variables. Differences in continuous variables among the groups were compared using the Student’s t-test, whereas categorical variables were compared using the chi-squared test. The incidence of IFI was reported for patients with proven and probable IFI according to the 2020 EORTC/MSG criteria.10 All factors associated with treatment success at the 12th week were assessed using logistic regression analysis to identify factors associated with the treatment success for IFI among new patients with HM receiving chemotherapy or HSCT and patients with proven, probable, or possible IFI were included. Odds ratio (OR) and associated 95% confidence intervals (95% CI) were calculated. Variables associated with treatment success in patients with IFI on univariate analysis with a p-value of ≤ 0.1 were included in multivariate analysis. Both univariate and multivariate analyses used the enter method. The survival curves of patients who received appropriate or inappropriate empirical therapy were drawn by the Kaplan–Meier method and compared using the Log rank test. For all tests, a p-value of ≤ 0.05 was considered significant. Statistical analyses were performed using SPSS version 26.0 (IBM, Armonk, NY, USA).
Result
Baseline Characteristic
During the study period, 931 patients were newly diagnosed with HM. Ninety-two patients with 107 episodes of IFI met the inclusion criteria (Figure 1). The common type of HM was lymphoma (54.9%). Patients with AML had the highest rate of IFI (Table 1).
 |
Figure 1 Flow diagram for selection of patient cohort. |
The characteristics of patients with IFI of total 107 episodes are described in Table 2. Approximately half of the patients were male (52.3%), and their mean (SD) age was 46.78 (14.36) years. There was a higher age in the IFI treatment failure group than in the treatment success group (53.14 ± 12.34 versus 43.68 ± 14.32; p = 0.001). Hypertension was the common underlying disease (23.4%), followed by hepatitis B (18.7%) and diabetes mellitus (9.3%). The median (IQR) duration of neutropenia during fungal infection was 14 days (5, 33). Fifty-eight cases of IFI (54.2%) emerged in patients with active HM, and all patients with treatment failure had active HM. The leading cases of IFI occurred in patients with AML (48.6%), followed by lymphoma (24.3%) and ALL (23.4%). The common cases of IFI (38.3%) emerged during the induction chemotherapy phase, followed by the reinduction phase (12.1%) and consolidation phase (12.1%). For cases of IFI emerging during stem cell transplantation, IFI was more common in allogeneic HSCT recipients than in autologous HSCT recipients. The primary pathogen for coinfection was bacteria (78.6%), followed by viruses (23.2%). There was a significant difference between the treatment success group and treatment failure group (43.1% vs 71.4%, p = 0.006) in patients with coinfection. There was a higher rate of bacterial coinfection in the treatment failure group than in the treatment success group (84% vs 74.2%, p = 0.006).
Epidemiology of IFI
Among 107 episodes, most patients were possible IFI (39.3%), followed by probable (32.7%) and proven (28%) IFI. The overall incidence of IFI was 7%. We also reported the incidence in patients with different types of HM and the annual incidence in Tables S1 and S2, respectively.
By proven and probable IFI cases, aspergillosis was the leading diagnosis (35.5%), followed by candidiasis (11.2%), PJP (8.4%), and mucormycosis (3.7%). Two of 6 cases of mucormycosis (including a possible case) occurred in patients with diabetes mellitus. No HIV-positive patient was diagnosed with PJP. Fusariosis was found in two cases in our study (1.9%), including one case of sinusitis accompanied by Exserohilum rostratum and one case of cellulitis.
The common site of infection was the lungs (43.9%), followed by blood (9.3%) and ears, nose, and throat (ENT) (8.4%). The lungs were the primary site of infection in patients with aspergillosis (74.5%) and PJP (19.1%), blood was the primary site of infection in patients with candidiasis (90%), and ENT was the leading site of infection in patients with mucormycosis (22.2%).
The fungal pathogen identification via fungal culture or the amplification of fungal DNA by PCR combined with DNA sequencing using biopsy tissue was available for 26 isolates from 20 cases of proven IFI, as described in Table 3. Antifungal susceptibility tests were available for 12 cases of proven IFI, as in Table 4. We found that most fungal pathogen in our study still had high susceptibility to antifungal drugs. All Candida spp. isolates were susceptible to echinocandins, amphotericin B, posaconazole, itraconazole and flucytosine. Twenty percent of Candida spp. isolates were resistant to fluconazole.
 |
Table 3 The Identification of Fungal Species from 20 Proven Invasive Fungal Infection Cases |
 |
Table 4 The Data of Antifungal Susceptibility Testing (N = 12) |
Incidence of Breakthrough IFI
Among 931 HM patients, 198 HM patients were received PAP which 12 of them were diagnosed with proven and probable IFI cases, whereas 598 HM patients were received primary P. jirovecii prophylaxis which 1 of them was diagnosed with probable PJP. Thus, the incidence of breakthrough IFI from proven and probable cases in patients receiving PAP and in patients receiving primary P. jirovecii prophylaxis was 6.1% and 0.2%, respectively.
Aspergillosis was the most breakthrough IFI among proven and probable cases (69.2%). There was not statistically different in mold, candida, and PJP between the treatment success group and the treatment failure group.
The leading antifungal drugs used for IFI prophylaxis in breakthrough IFI cases were posaconazole (19.6%), followed by fluconazole (7.5%) and voriconazole (4.7%). We found one case that was a breakthrough PJP from cotrimoxazole.
Patterns of Antifungal Therapy
Conventional amphotericin B was the leading antifungal drug used as the monotherapy for empirical therapy (39.8%), followed by voriconazole (37.8%) and cotrimoxazole (9.2%). For combination therapy, we found five regimens, including liposomal amphotericin B plus voriconazole (44.4%), conventional amphotericin B plus voriconazole (22.2%), conventional amphotericin B plus posaconazole, anidulafungin plus voriconazole, and anidulafungin plus posaconazole (each 11.1%). Sixty-seven percent of combination empirical regimens were administered to patients with breakthrough IFI. Additional details of the antifungal drugs used in each regimen are reported in Table S3.
Treatment Outcome and Factors Associated with Treatment Success in Cases of IFI
The overall treatment success rate at the 12th week was 67.3%, including complete and partial response rates of 63.6% and 3.7%, respectively. Conversely, failure treatment outcomes included stable disease (2.8%), progression of fungal disease (3.7%), and death (26.2%).
The factors significantly associated with IFI treatment success in univariate analysis were age < 60 years (odds ratio [OR] = 4.16; 95% confidence interval [CI] = 1.64–10.52), duration of neutropenia (OR = 0.98; 95% CI = 0.97–1), absence of coinfection (OR = 3.31; 95% CI = 1.39–7.89), received appropriate empirical therapy on the first day of an IFI diagnosis (OR = 4.64; 95% CI = 1.42–15.15), and received appropriate empirical therapy within six days of an IFI diagnosis (OR = 4.17; 95% CI = 1.51–11.5). From multivariate analysis, age < 60 years (adjusted odds ratio [aOR] = 5.07; 95% CI = 1.78–14.42), absence of coinfection (aOR = 2.85; 95% CI = 1.09–7.49), and received appropriate empirical therapy on the first day of an IFI diagnosis (aOR = 3.40; 95% CI = 1.03–11.26) were significant factors associated with treatment success. The results of univariate and multivariate analysis are presented in Table 5.
Survival Outcome Within 12 Weeks
The overall mortality rate in patients with IFI within 12 weeks after antifungal therapy was 26.2%. The overall survival rate significantly differed between patients who received appropriate empirical therapy and those who received inappropriate empirical therapy on the first day of an IFI diagnosis (p = 0.03, Log rank test; Figure 2). The overall survival rate also differed according to the presence of candidiasis (p = 0.002, Log rank test; Figure S1).
Discussion
This retrospective cohort study found that the incidence of proven and probable IFI according to the recent EORTC/MSG consensus criteria10 was 7%. The epidemiology of IFI in patients with HM has also changed recently. Its incidence varies among different regions, ranging 4.6%–15% in Europe,2,15–19 9.6% to 16.2% in South Africa,20,21 and 1.3% to 12% in Asia.3,5,22–24 In our study, the incidence of IFI among patients with HM was lower than that reported in the past decade in Thailand (14%).5 This finding may reflect the efficacy of initial PAP use in recent years. Conversely, a 1-year retrospective study in 2006 in the same setting as our study25 revealed that the incidence of IFI in patients with HM was 4.8%, slightly lower than our result. The explanation might be the increased awareness and the accessibility of newer diagnostic techniques.26
Surprisingly, when stratifying patients by the underlying HM, although AML was the most common HM in this study, the frequency of IFI was highest in patients with ALL. Usually, chemotherapy intensity is lower in ALL than in AML. Hence, patients with ALL have a lower risk of IFI than those with AML.27 However, the incidence of IFI in patients with ALL has increased in recent years. In the past decade, one of the largest retrospective studies reported an incidence of IFI of approximately 6.5% in patients with ALL.2 Another retrospective study in Korea found that patients with ALL had a slightly higher rate of IFI than those with AML (7.5% vs 7.1%).27 This higher IFI incidence in ALL in our study may be related to the use of PAP has been mainly recommended in patients with AML in our institution since 2018, and there is no consensus on the routine use of antifungal prophylaxis in patients with ALL. Thus, the emergence of IFI should be closely monitored in patients with ALL. However, the use of PAP should be carefully considered in these patients because of drug–drug interactions between mold-active azoles and Vinca alkaloids, which are the main chemotherapies used in ALL.14 These azoles are potent inhibitors of the P450 3A4 enzyme system, which can enhance the neurotoxicity of vincristine.
When focusing on the annual incidence of IFI during the study period, a trend reduction of mold infections was observed between the era of the consecutive galactomannan follow-up strategy (2016–2017, 8.5%) and the era of PAP (since 2018, 6.2%) (Table S2). This result indicates that PAP represents an effective and reasonable approach for reducing the incidence of IFI in patients with HM, as previously reported.21,27–29
Aspergillosis was the leading IFI in our study, similar to other studies.20–23,30,31 It was the most frequent IFI and the most commonly found in patients with AML, which was similar to other studies conducted in Thailand.3,5 Almost all mycological samples of Aspergillus spp. which had the identification of fungal species in our study were A. flavus. This finding differed from Europe and the US, where the main fungal species of aspergillosis in patients with HM is A. fumigatus.17,32 The interesting or unique epidemiology in Asian countries was that A. flavus was more common than A. fumigatus.33,34 However, the newest 2020 EORTC/MSG criteria may affect the incidence of aspergillosis due to the changing of definitions compared to the 2008 version, such as adding the cut point of galactomannan antigen. This change may improve the specificity of diagnosis, but it could affect the type of IFI category diagnosis. Our study found 41.1% of probable IFI when using the 2008 EORTC/MSG criteria and reduced to 32.7% when using the 2020 EORTC/MSG criteria, which is similar to a retrospective in Turkey showed that the use of 2020 EORTC/MSG criteria resulted in a 27.3% reduction in probable invasive pulmonary aspergillosis.35 This result indicated that using the 2020 EORTC/MSG criteria could reduce the diagnosis of probable IFI cases.
In agreement with previous findings,24 we noted that candidiasis was more common in patients with ALL. Candida tropicalis was the most common Candida spp. in patients with HM,36 similar to our finding. All Candida spp. in our study were susceptible to echinocandins, posaconazole, and amphotericin B. Approximately 20% of the total Candida spp. isolates in our study were resistant to fluconazole, which was slightly more susceptible compared to the one retrospective study in Italy found that the available antifungal susceptibility of Candida spp. isolates from HM patients with IFI were resistant to fluconazole and voriconazole 40%.17
Five of the nine cases of PJP occurred in patients with lymphoma. However, the incidence of PJP in patients with lymphoma in our study was extremely low (1% from 5/511) compared to that in a single-center retrospective study conducted in the US (6.2%).37
The incidence of mucormycosis has slightly increased recently, especially among patients with acute leukemia.38 Still, it is likely underestimated because most cases were detected during autopsy.39,40 In our study, only two of six cases of mucormycosis (including a possible case) occurred in patients with diabetes mellitus. We could not clarify whether diabetes mellitus was a risk factor for mucormycosis because of the small number of cases. Lastly, fusariosis was found in only 1.9% of the other uncommon pathogens, in agreement with other studies in the same region of ours.5,41
The incidence of breakthrough IFI in our study was approximately 6%, which was slightly higher than the results from other previous studies in recent years.29,42–44 Aspergillosis was the leading cause of breakthrough IFI (53.8%), similar to other studies.45,46 Contrarily, our result differed from a 4-year retrospective study from France showed that mucormycosis and fusariosis were the leading cause of breakthrough IFI.42 Thus, the incidence and spectrum of breakthrough IFI significantly differ among countries depending on the antifungal prophylaxis, the local epidemiology, and individual patient characteristics.
Most other studies use the term “survival” and “death” for the treatment outcome. In contrast, our study uses “success” and “failure” according to the 2008 MSG/EORTC defining the response of IFI therapy criteria.12 The survival rate within 12 weeks was high in our study (73.8%) when compared to previous studies that reported a survival rate of about 60%.2,5,21,22 Our mortality rate was 26.2% which lower than that reported in prior retrospective cohort studies in Thailand.5 Our finding suggested that the accessibility of novel antifungal drugs and novel diagnostic tools in recent years may improve the survival outcome of patients. Meanwhile, our result revealed that the mortality rate associated with candidiasis in patients with HM is increasing, contradicting a large retrospective study conducted in Italy, where mucormycosis was the primary cause of death.2 This study also evaluated factors associated with treatment success in IFI. Our finding suggested closely monitoring treatment outcomes in patients aged ≥ 60 years and with coinfection. Since “age” was the non-modifiable risk factor, the strategy for primary prophylaxis of IFI among elderly patients would be considered but a delicate condition from polypharmacy would be a concern. Thus, the use of PAP in the elderly may be determined by physicians’ judgment for an individual patient. Lastly, the appropriate type of antifungal drug is significant for clinical outcomes.
The significant effect of receiving appropriate empirical therapy immediately after an IFI diagnosis was even more pronounced in multivariate analysis, which revealed a 2-fold reduction in the mortality rate on Kaplan–Meier analysis from 45% to 21.8%. Notably, this result reiterates the importance of appropriateness regarding the drug, dose, administration route, and effective spectrum during initial empirical therapy in HM patients with IFI. Since mold was the leading pathogen in our study, protocol implementation in the institution by initially using rapid novel diagnostic tools and using extended-spectrum azoles as empirical therapy strategies may provide more appropriate empirical therapy and lead patients to better clinical outcomes.
Our study had some strengths. To the best of our knowledge, this is the first study to determine the occurrence of IFI using the standard criteria recommended by the latest 2020 EORTC/MSG. This is the first study to evaluate the factors associated with the treatment success of IFI in patients with HM. Our study is the newest retrospective analysis of IFI, including PJP infection in patients with HM and evaluating the incidence of breakthrough IFI in Thailand reported to date. We also provided antifungal susceptibility data, including minimum inhibitory concentration and its interpretation from CLSI, to indicate a trend of antifungal resistance in such a group of patients.
Our study also had some limitations. Despite the retrospective study and its relatively short duration of data collection because the microbiological data before the year 2016 in the electronic medical records in our institution were unavailable, we have provided essential information. Because of resource limitations in our country, a substantial proportion of patients with IFI received conventional amphotericin B as opposed to liposomal amphotericin B, but this did not significantly affect outcomes. Some fungal isolates were performed by E-test®, which was not the standard test of antifungal susceptibility testing.
Conclusion
In conclusion, the epidemiology and mortality of IFI in Thailand slightly differed from findings in other countries. Most cases of IFI occurred during the induction phase of chemotherapy. Our data confirmed that PAP has significantly reduced the incidence of IFI. Further studies are needed to determine the risk–benefit profiles of PAP for certain hematological disorders, especially ALL. This finding could represent a first step toward standardizing such protocols (providing better antifungal guidance in treating invasive candidiasis) to improve patient outcomes.
Ethics Approval and Informed Consent
Ethics approval for the study was obtained from the Institutional Review Board of the Faculty of Medicine at Chulalongkorn University (IRB No. 910/64). Waiving of informed consent was given due to the retrospective, non-interventional study design. All patient data were collected anonymously and ensured about the confidentiality of their information. Therefore, the study was conducted following the Declaration of Helsinki.
Acknowledgments
The authors express their gratitude to all the study patients, physicians, pharmacists, nurses, microbiological laboratory technicians as well as the entire infectious disease medical teams at King Chulalongkorn Memorial Hospital for their voluntary participation, without their hard working, this study could not be successful.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bays DJ, Thompson GR
2. Pagano L, Caira M, Candoni A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006;91(8):1068–1075.
3. Rotjanapan P, Chen YC, Chakrabarti A, et al. Epidemiology and clinical characteristics of invasive mould infections: a multicenter, retrospective analysis in five Asian countries. Med Mycol. 2018;56(2):186–196.
4. Pagano L, Dragonetti G, Cattaneo C, et al. Changes in the incidence of candidemia and related mortality in patients with hematologic malignancies in the last ten years. A SEIFEM 2015-B report. Haematologica. 2017;102(10):e407–e410.
5. Phikulsod P, Suwannawiboon B, Chayakulkeeree M. Invasive Fungal Infection among Febrile Patients with Chemotherapy-Induced Neutropenia in Thailand. Se Asian J Trop Med. 2017;48(1):159–169.
6. Nganthavee V, Phutthasakda W, Atipas K, et al. High incidence of invasive fungal infection during acute myeloid leukemia treatment in a resource-limited country: clinical risk factors and treatment outcomes. Support Care Cancer. 2019;27(9):3613–3622.
7. Supatharawanich S, Narkbunnam N, Vathana N, et al. Invasive Fungal Diseases in Children with Acute Leukemia and Severe Aplastic Anemia. Mediterr J Hematol Infect Dis. 2021;13(1):e2021039.
8. CLSI. Performance Standards for Antifungal Susceptibility Testing of Yeasts (M60).
9. CLSI. Performance Standards for Antifungal Susceptibility Testing of Filamentous Fungi (M61).
10. Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2020;71(6):1367–1376.
11. De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–1821.
12. Segal BH, Herbrecht R, Stevens DA, et al. Defining responses to therapy and study outcomes in clinical trials of invasive fungal diseases: mycoses Study Group and European Organization for Research and Treatment of Cancer consensus criteria. Clin Infect Dis. 2008;47(5):674–683.
13. Cornely OA, Hoenigl M, Lass-Florl C, et al. Defining breakthrough invasive fungal infection-Position paper of the mycoses study group education and research consortium and the European Confederation of Medical Mycology. Mycoses. 2019;62(9):716–729.
14. Maertens JA, Girmenia C, Bruggemann RJ, et al. European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European Conference on Infections in Leukaemia. J Antimicrob Chemother. 2018;73(12):3221–3230.
15. Auberger J, Lass-Florl C, Ulmer H, et al. Significant alterations in the epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol. 2008;88(5):508–515.
16. Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infection in adult hematopoietic stem cell transplant recipients: analysis of Multicenter Prospective Antifungal Therapy (PATH) Alliance registry. Clin Infect Dis. 2009;48(3):265–273.
17. Fracchiolla NS, Sciume M, Orofino N, et al. Epidemiology and treatment approaches in management of invasive fungal infections in hematological malignancies: results from a single-centre study. PLoS One. 2019;14(5):e0216715.
18. Karthaus M, Cornely OA. Recent developments in the management of invasive fungal infections in patients with hematological malignancies. Ann Hematol. 2005;84(4):207–216.
19. Caira M, Girmenia C, Fadda RM, et al. Invasive fungal infections in patients with acute myeloid leukemia and in those submitted to allogeneic hemopoietic stem cell transplant: who is at highest risk? Eur J Haematol. 2008;81(3):242–243.
20. Camplesi MJ, Silva HM, Arantes AM, et al. Invasive fungal infection in patients with hematologic disorders in a Brazilian tertiary care hospital. Rev Soc Bras Med Trop. 2017;50(1):80–85.
21. Bergamasco MD, Pereira CAP, Arrais-Rodrigues C, et al. Epidemiology of Invasive Fungal Diseases in Patients with Hematologic Malignancies and Hematopoietic Cell Transplantation Recipients Managed with an Antifungal Diagnostic Driven Approach. J Fungi. 2021;7(8);56.
22. Kurosawa M, Yonezumi M, Hashino S, et al. Epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol. 2012;96(6):748–757.
23. Lee SY, Yeo CL, Lee WH, Kwa AL, Koh LP, Hsu LY. Prevalence of invasive fungal disease in hematological patients at a tertiary university hospital in Singapore. BMC Res Notes. 2011;4:42.
24. Chen CY, Huang SY, Tsay W, et al. Clinical characteristics of candidaemia in adults with haematological malignancy, and antimicrobial susceptibilities of the isolates at a medical centre in Taiwan, 2001-2010. Int J Antimicrob Agents. 2012;40(6):533–538.
25. Roongpoovapatr P. Causative Pathogens of Fever in Neutropenic Patients at King Chulalongkorn Memorial Hospital. J Med Assoc Thai. 2010;93(7):776–783.
26. Ruhnke M, Schwartz S. Recent developments in the management of invasive fungal infections in patients with oncohematological diseases. Ther Adv Hematol. 2016;7(6):345–359.
27. Oh SM, Byun JM, Chang E, et al. Incidence of invasive fungal infection in acute lymphoblastic and acute myelogenous leukemia in the era of antimold prophylaxis. Sci Rep. 2021;11(1):22160.
28. Wasylyshyn A, Linder KA, Castillo CG, Zhou S, Kauffman CA, Miceli MH. Breakthrough Invasive Fungal Infections in Patients with Acute Myeloid Leukemia. Mycopathologia. 2020;185(2):299–306.
29. Patel HP, Perissinotti AJ, Patel TS, Bixby DL, Marshall VD, Marini BL. Incidence and Risk Factors for Breakthrough Invasive Mold Infections in Acute Myeloid Leukemia Patients Receiving Remission Induction Chemotherapy. Open Forum Infect Dis. 2019;6(5):ofz176.
30. Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001-2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis. 2010;50(8):1091–1100.
31. Souza L, Nouer SA, Morales H, et al. Epidemiology of invasive fungal disease in haematologic patients. Mycoses. 2021;64(3):252–256.
32. Perea S, Patterson TF. Invasive Aspergillus infections in hematologic malignancy patients. Semin Respir Infect. 2002;17(2):99–105.
33. Chen CY, Sheng WH, Cheng A, et al. Invasive fungal sinusitis in patients with hematological malignancy: 15 years experience in a single university hospital in Taiwan. BMC Infect Dis. 2011;11:250.
34. Zarrinfar H, Mirhendi H, Fata A, Khodadadi H, Kordbacheh P. Detection of Aspergillus flavus and A. fumigatus in Bronchoalveolar Lavage Specimens of Hematopoietic Stem Cell Transplants and Hematological Malignancies Patients by Real-Time Polymerase Chain Reaction, Nested PCR and Mycological Assays. Jundishapur J Microbiol. 2015;8(1):e13744.
35. Acet-Ozturk NA, Omer-Topcu D, Vurat-Acar K, et al. Impact of revised EORTC/MSGERC 2020 criteria on diagnosis and prognosis of invasive pulmonary aspergillosis in patients with hematological malignancies undergoing bronchoscopy. J Mycol Med. 2022;32(4):101304.
36. Dewan E, Biswas D, Kakati B, Verma SK, Kotwal A, Oberoi A. Epidemiological and mycological characteristics of candidemia in patients with hematological malignancies attending a tertiary-care center in India. Hematol Oncol Stem Cell Ther. 2015;8(3):99–105.
37. Barreto JN, Thompson CA, Mara KC, et al. Incidence and Outcomes of Pneumocystis pneumonia When Utilizing PCR-Based Diagnosis in Patients with Hodgkin Lymphoma Receiving Intensive Chemotherapy. Blood. 2019;134(Supplement_1):4052.
38. Kontoyiannis DP, Lionakis MS, Lewis RE, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases. J Infect Dis. 2005;191(8):1350–1360.
39. Chamilos G, Luna M, Lewis RE, et al. Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989-2003). Haematologica. 2006;91(7):986–989.
40. Chayakulkeeree M, Denning DW. Serious fungal infections in Thailand. Eur J Clin Microbiol Infect Dis. 2017;36(6):931–935.
41. Hsu LY, Lee DG, Yeh SP, et al. Epidemiology of invasive fungal diseases among patients with haematological disorders in the Asia-Pacific: a prospective observational study. Clin Microbiol Infect. 2015;21(6):594 e597–511.
42. Lerolle N, Raffoux E, Socie G, et al. Breakthrough invasive fungal disease in patients receiving posaconazole primary prophylaxis: a 4-year study. Clin Microbiol Infect. 2014;20(11):O952–959.
43. Biehl LM, Vehreschild JJ, Liss B, et al. A cohort study on breakthrough invasive fungal infections in high-risk patients receiving antifungal prophylaxis. J Antimicrob Chemother. 2016;71(9):2634–2641.
44. Kuster S, Stampf S, Gerber B, et al. Incidence and outcome of invasive fungal diseases after allogeneic hematopoietic stem cell transplantation: a Swiss transplant cohort study. Transpl Infect Dis. 2018;20(6):e12981.
45. Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356(4):348–359.
46. Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356(4):335–347.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.