Back to Journals » Risk Management and Healthcare Policy » Volume 16
Epidemiology and Clinical Characteristics of Seasonal Human Coronaviruses in Children Hospitalized in Hebei Province, China Before and During the COVID-19 Pandemic
Authors Zhao MC, Wen C, Sun L, Duan SX, Zang KX, Wang L, Cui XW
Received 26 May 2023
Accepted for publication 19 August 2023
Published 8 September 2023 Volume 2023:16 Pages 1801—1807
DOI https://doi.org/10.2147/RMHP.S423077
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Gulsum Kubra Kaya
Meng-Chuan Zhao,1 Chan Wen,2 Ling Sun,2 Su-xia Duan,1 Ke-xin Zang,3 Le Wang,1 Xiao-Wei Cui4
1Department of Laborotory Medicine, Children’s Hospital of Hebei Province, Shijiazhuang, People’s Republic of China; 2Department of Medical, Children’s Hospital of Hebei Province, Shijiazhuang, People’s Republic of China; 3Hebei Medical University, Shijiazhuang, People’s Republic of China; 4Children’s Hospital of Hebei Province, Shijiazhuang, People’s Republic of China
Correspondence: Xiao-Wei Cui, Children’s Hospital of Hebei Province, No. 133 of JianHua Street, Shijiazhuang, 050031, People’s Republic of China, Tel +86 18503292016, Fax +86 031185911109, Email [email protected]
Background: This study aimed to assess the impact of the COVID-19 pandemic on the prevalence and clinical characteristics of seasonal human coronavirus (HCoV) infections among children hospitalized in Hebei, China.
Methods: We examined nasopharyngeal aspirate (NPA) specimens for seasonal HCoVs from January 2018 to December 2021, at the Children’s Hospital of Hebei Province. We used a GeXP-based multiplex reverse transcription PCR assay for the detection of 11 common respiratory viruses (including seasonal HCoVs), chlamydia, and Mycoplasma pneumoniae. The demographic and clinical characteristics of children who tested positive for seasonal HCoVs were recorded and analyzed.
Results: A total of 377 (1.96%) of the 19,248 specimens from 2018 to 2019 and 263 (1.96%) of the 13,426 specimens from 2020 to 2021 exhibited seasonal HCoVs. Compared to 2018 and 2019, the positive rate of seasonal HCoVs was lower from January to July of 2020 and increased beginning in August 2020, peaking in the autumn and winter. In 2020– 2021, nasal blockage and swollen adenoids were detected more frequently in children who tested positive for seasonal HCoVs. During 2018– 2019, however, the duration of fever was significantly longer, and cough and dyspnea were more prominent among children who had fallen ill. In addition, seasonal HCoV-positive patients in 2018– 2019 were more likely to experience complications, had a higher risk of severe community-acquired pneumonia (CAP), and had a tendency to require a longer hospital stay than patients in 2020– 2021.
Conclusion: According to our findings, there were significant changes in the epidemiology of seasonal HCoVs in Hebei, China during the COVID-19 pandemic, and children infected with seasonal HCoVs usually experienced milder clinical symptoms during the pandemic than before it.
Keywords: children, clinical characteristics, COVID-19 pandemic, epidemiology, Seasonal human coronavirus
Introduction
Human coronaviruses (HCoVs) are enclosed, single-stranded, positive-sense RNA viruses. There are currently seven HCoVs, including SARS-CoV-2, MERS-CoV, SARS-CoV, and four seasonal HCoV species—NL63, 229E, OC43, and HKU1. The four seasonal HCoVs are significant causes of respiratory illnesses and circulate worldwide. Approximately one-third of all “common colds” are typically linked with relatively mild upper respiratory tract illnesses.1–3 In some cases, however, acute respiratory failure might develop, particularly in immunosuppressed patients, children, and patients with preexisting pulmonary diseases.4
In December 2019, the COVID-19 epidemic caused by SARS-CoV-2 first emerged in Hubei Province, China, and subsequently swiftly spread throughout the world.5,6 To control the transmission of SARS-CoV-2, China implemented numerous public health preventative measures, including the prohibition of social gatherings, the wearing of masks, and vaccination. The public’s understanding of respiratory protection and health has also increased. Several studies conducted in Hangzhou and Shanghai have demonstrated that the COVID-19 outbreak and these diverse efforts have had varying effects on the incidence of common respiratory viruses.7,8 In Hebei, China, information regarding seasonal HCoVs among children hospitalized during the COVID-19 pandemic is limited. In this study, we evaluated the influence of the COVID-19 pandemic on the prevalence and clinical characteristics of seasonal HCoV infections among hospitalized children with acute respiratory tract infection (ARTI) in Hebei, Northern China, between January 2018 and December 2021.
Materials and Methods
Study Population
This retrospective analysis included children under the age of 14 years with suspected acute respiratory tract infections (ARTI) who underwent detection of respiratory pathogens at the Children’s Hospital of Hebei Province between January 2018 and December 2021. Children’s Hospital of Hebei Province is a tertiary, pediatric, specialist hospital, which only accepts children aged 14 years and under. Children were diagnosed with ARTI if they had one or more respiratory tract infection symptoms (fever, cough, nasal obstruction, sneezing) or lower respiratory infection symptoms (tachypnea, dyspnea, or wheezing/rales upon auscultation). Patients with ARTI with radiographic evidence (consolidation, other infiltrate, or pleural effusion) were diagnosed with community-acquired pneumonia (CAP). Patients with severe CAP had one of the following clinical signs: hypoxemia [oxygen saturation < 92%, cyanosis, respiratory rate > 70 (infants) or 50 (older children) breaths/min, intermittent apnoea, clinical manifestations of chest wall inspiratory depression or nasal flapping or moaning sounds]; central cyanosis; severe respiratory distress, anorexia or dehydration, and consciousness disorders (lethargy, coma, convulsion).
The Institutional Review Board of the Children’s Hospital of Hebei Province approved this study. As data records and clinical specimens were totally deidentified and anonymized, informed consent was waived.
Information Collection and Detection of Pathogens
Demographic and clinical data on seasonal HCoV-positive cases were collected from the database of the hospital. The nasopharyngeal aspirate (NPA) specimens of the children were routinely analyzed using a GeXP-based multiplex reverse transcription PCR assay for a range of targets, including influenza A (Flu A), influenza B (Flu B), influenza A H1N1 pdm09 (09H1), influenza H3N2 (H3), human parainfluenza virus (HPIV), respiratory syncytial virus (RSV), human adenovirus (HAdV), human metapneumovirus (HMPV), rhinovirus (HRV), human bocavirus (HBoV), seasonal HCoVs (including HKU1, NL63, 229E, and OC43), chlamydia (Ch) and Mycoplasma pneumoniae (MP).9 Bronchial alveolar lavage fluids or pleural effusions were employed to identify any bacteria or fungi in HCoV-positive children during their entire hospital admission.
Statistical Analysis
Statistical Product and Service Solutions (SPSS) 25.0 software was utilized for the data analysis. The median and interquartile range were used to characterize quantitative data. Categorical variables were defined using frequency and percentages before being tested using the chi-squared test and Fisher’s exact test, where appropriate. All tests were two-tailed, and a P< 0.05 was regarded as statistically significant.
Results
Study Population
During the study period, a total of 32,674 children who were hospitalized were enrolled, including 9442 in 2018, 9806 in 2019, 6226 in 2020, and 7200 in 2021. Among these children, there were 19,656 males (60.16%) and 13,018 females (39.84%). The ages ranged from 1 month to 14 years. Among them, 2562 (78.54%) were under the age of 3 years old.
Epidemiological Characteristics
Among the 32,674 children, 640 (1.96%) seasonal HCoV-positive cases were identified, with 377 (1.96%) cases from 2018 to 2019 and 263 (1.96%) cases from 2020 to 2021. The median age of children who were positive for seasonal HCoV was older in 2020–2021 than in 2018–2019 (16 months vs 11 months, Z = −5.07, P < 0.001, Table 1). There were no statistically significant differences in the gender in the years 2018–2019 and 2020–2021 (χ2 = 0.096, P = 0.757, Table 1).
 |
Table 1 Comparison of the Demographic and Clinical Characteristics of Children with Seasonal HCoV-Positive During the COVID-19 Pandemic (2020–2021) with the Previous Year (2018–2019) |
We analyzed the seasonal distribution of seasonal HCoVs from 2018 through 2021. Seasonal HCoV infections occurred throughout the year from 2018 to 2019, with a peak in the spring of 2018. (Figure 1). Seasonal HCoVs were identified throughout the year in 2020 and 2021. From January through July of 2020, the positive rate of seasonal HCoVs was lower than that in 2018 and 2019. Subsequently, in August 2020, the positive rate grew, reaching a peak in autumn and winter, which was higher than the same period in 2018 and 2019. The positive rates of seasonal HCoVs was lower in 2021 than in 2018 and 2019 throughout the entire year.
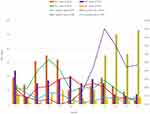 |
Figure 1 Monthly distribution of seasonal human coronaviruses compared before (Jan 2018–Dec 2019) and during (Jan 2020–Dec 2021) the COVID-19 pandemic. |
From 2018 to 2019, 205 (54.38%) of the 377 seasonal HCoV-positive cases were co-detected with other respiratory pathogens. Of the 263 seasonal HCoV-positive cases from 2020 to 2021, 157 (59.70%) were co-detected with other respiratory pathogens. There were no statistically significant differences in the co-detection rate between 2018–2019 and 202–2021 (χ2 = 1.893, P = 0.169, Table 1).
Clinical Characteristics
Table 1 provides a summary of the differences in clinical data, complications, underlying conditions and disease severity parameters between seasonal HCoV-positive cases in 2018–2019 and 2020–2020.
Fever, cough, and pharyngeal hyperemia were the most prevalent clinical manifestations of seasonal HCoV-positive children. Headache, abdominal pain, and rashes were rare extra-respiratory symptoms. The most prevalent complication in these children was anemia, followed by myocardial damage (myocardial enzymes increased in different degrees). Compared to seasonal HCoV-positive children in 2018–2019, the duration of fever in seasonal HCoV-positive children in 2020–2021 was considerably shorter (Z = −2.609, P = 0.009). Cough (χ2 = 5.796, P =0.016) and dyspnea (χ2 = 12.182, P < 0.001) were more prevalent in seasonal HCoV-positive children in 2018–2019; however, nasal obstruction (χ2 = 6.85, P = 0.01) and swollen adenoids (χ2 = 18.593, P < 0.001) were more prevalent in seasonal HCoV-positive children in 2020–2021. In terms of complications, seasonal HCoV-positive children in 2018–2019 were more likely to develop cardiac injury (χ2 = 4.527, P < 0.033) and respiratory failure (χ2 = 4.131, P = 0.042) than those in 2020–2021. When comparing these two research periods, no significant differences in underlying circumstances were detected.
Among the seasonal HCoV-positive children in 2020–2021, 4.56% (12/263) had a diagnosis of severe CAP, which was significantly lower than the 9.55% (36/377) in 2018–2019 (χ2 = 5.552, P = 0.018). Moreover, compared to seasonal HCoV-positive children in 2018–2019, seasonal HCoV-positive children in 2020–2021 had a shorter hospitalization stay (Z = −3.435, P = 0.001). However, seasonal HCoV-positive children in 2020–2021 who required pediatric intensive care unit (PICU) level treatment, noninvasive positive pressure ventilation, and invasive mechanical ventilation were comparable to those in 2018–2019 (χ2 = 0.211, 0.021 and 0, P = 0.646, 0.883 and 1).
Discussion
During the pandemic, a range of preventative and control actions against SARS-CoV-2 resulted in a drop in both the number of requests for respiratory virus testing and the proportion of positive results.7,8,10 In this study, respiratory virus testing requests decreased throughout the pandemic (2020–2021). However, no significant changes were observed in the positive rates of seasonal HCoVs before and during the pandemic, which contradicts the findings of our earlier research.7,8,10 We analyzed the monthly distribution of seasonal HCoVs during the COVID-19 pandemic to determine the reasons for the discrepancy. The positive rates of seasonal HCoVs remained relatively low from January to June 2020, when the most stringent epidemic prevention measures were implemented, indicating that wearing masks, closing schools, frequent handwashing, and home quarantine were also effective at preventing the spread of seasonal HCoVs. Upon the reopening of schools and kindergartens in Hebei in June 2020, subsequent to the efficient suppression of the pandemic, a rapid increase in seasonal HCoVs was seen. A recent study found a similar rapid increase in the prevalence of rhinoviruses following the reopening of schools.11 There are two possible explanations for the correlation between seasonal increases in HCoVs and the reopening of schools. Initially, seasonal HCoV-protective immunity was short-lasting.12 Antibody levels that neutralize seasonal HCoVs often decrease after six months, and reinfections may occur. After six months of home quarantine and social distancing during the epidemic, most of the protective immunity of the children would decline, resulting in an increase in vulnerability to seasonal HCoVs. Second, maintaining strict social distance at school and kindergarten was challenging for children. The positive rates of seasonal HCoVs declined again from January 2021 and remained lower than that in 2018 and 2019 throughout the year. This could be explained by the development of protective immunity in the second half of 2020 and the increase in public awareness of self-protection.
The major impact of the COVID-19 pandemic on the clinical characteristics of seasonal HCoV infection in hospitalized children in China was another significant finding of this study. First, we note that symptoms of upper respiratory tract infection, including nasal obstruction and swollen adenoids, were reported more frequently among seasonal HCoV-positive children in 2020–2021. During 2018–2019, however, the duration of fever was significantly longer, and signs of lower respiratory tract infection, such as cough and dyspnea, were also more common among these children. Second, in 2018–2019, seasonal HCoV-positive patients were more likely to have complications (myocardial damage and respiratory failure) than the patients in 2020–2021. Third, seasonal HCoV-positive patients in 2018–2019 exhibited a greater incidence of severe CAP and tended to require longer hospitalizations than those in 2020–2021. According to these findings, during the COVID-19 pandemic, seasonal HCoV-positive children typically had milder clinical symptoms than they did prior to the pandemic.
Seasonal HCoVs are considered to be common cold viruses; nevertheless, they can also cause a more severe respiratory disease in children, the elderly, and patients with underlying conditions.13 In this study, a comparable distribution of underlying conditions was seen across seasonal HCoV-positive children in 2018–2019 and 2020–2021; however, seasonal HCoV-positive children in 2020–2021 were older than those in 2018–2019. Consequently, we hypothesize that age differences may be one of the causes for the milder clinical signs during the COVID-19 pandemic. Immunity against one HCoV type may affect subsequent infection by another HCoV type.14 Recent studies found that SARS-CoV-2 vaccination considerably improved the neutralizing activity against seasonal HCoVs,15–17 suggesting that SARS-CoV-2 vaccination may give some cross-protection against seasonal HCoVs. China began administering SARS-CoV-2 vaccinations to children aged between 3 and 11 in June 2021, and the immunization rate for this age group reached 50% by the end of 2021. Perhaps this strategy also affected the clinical manifestations of seasonal HCoV infection.
There are several limitations to this study. First, this was a small-sample, single-center study that may not be representative of the total Chinese pediatric population. Further studies using multi-center and large samples are required to demonstrate the efficacy of our findings. Second, although we detected seasonal HCoVs from the respiratory samples of patients, it is questionable if their clinical symptoms were caused by these seasonal HCoVs, hence introducing an uncertainty bias to our results.
Conclusions
During the COVID-19 pandemic, significant changes in the epidemiology and clinical aspects of seasonal HCoV infection in hospitalized children occurred in Hebei, China. In comparison to before the pandemic, the positive rate of seasonal HCoVs rose sharply after August 2020, with peaks in autumn and winter, while the positive rate of seasonal HCoVs decreased significantly during the other periods of the pandemic. In addition, seasonal HCoV-positive children typically exhibited less severe clinical signs during the COVID-19 pandemic compared to before the outbreak.
Abbreviations
HCoVs, human coronaviruses; NPA, nasopharyngeal aspirate; CAP, community-acquired pneumonia; ARTI, acute respiratory tract infection; Flu A, influenza A; Flu B, influenza B; 09H1, influenza A H1N1 pdm09; H3, influenza H3N2; HPIV, human parainfluenza virus; RSV, respiratory syncytial virus; HAdV, human adenovirus; HMPV, human metapneumovirus; HRV, rhinovirus; HBoV, human bocavirus; Ch, Chlamydia; Mp, Mycoplasma pneumoniae; PICU, pediatric intensive Care Unit.
Ethical Approval
This study was conducted in accordance with the declaration of Helsinki. And all aspects were performed in accordance with national ethics regulations and approved by the Ethics Committee of Children’s Hospital of Hebei Province, China (YYLS No.204). Data records and collected clinical specimens were de-identified and completely anonymous so informed consent was waived.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was supported by a grant from Hebei medical science research project (No.20210211).
Disclosure
The authors declare that they have no competing interests.
References
1. Gaunt ER, Hardie A, Claas EC, Simmonds P, Templeton KE. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48:2940–2947. doi:10.1128/JCM.00636-10
2. Gadsby NJ, Russell CD, McHugh MP, et al. Comprehensive molecular testing for respiratory pathogens in community-acquired pneumonia. Clin Infect Dis. 2016;62:817–823. doi:10.1093/cid/civ1214
3. Trombetta H, Faggion HZ, Leotte J, Nogueira MB, Vidal LR, Raboni SM. Human coronavirus and severe acute respiratory infection in Southern Brazil. Pathog Glob Health. 2016;110:113–118. doi:10.1080/20477724.2016.1181294
4. Corman VM, Lienau J, Witzenrath M. Coronaviruses as the cause of respiratory infections. Internist. 2019;60:1136–1145. doi:10.1007/s00108-019-00671-5
5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi:10.1056/NEJMoa2001316
6. Gorbalenya AE, Baker SC, Baric RS; Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi:10.1038/s41564-020-0695-z
7. Du X, Wu G, Zhu Y, Zhang S. Exploring the epidemiological changes of common respiratory viruses since the COVID-19 pandemic: a hospital study in Hangzhou, China. Arch Virol. 2021;166(11):3085–3092. doi:10.1007/s00705-021-05214-8
8. Liu P, Xu M, Cao L, et al. Impact of COVID-19 pandemic on the prevalence of respiratory viruses in children with lower respiratory tract infections in China. Virol J. 2021;18(1):159. doi:10.1186/s12985-021-01627-8
9. Zhao MC, Li GX, Zhang D, et al. Clinical evaluation of a new single-tube multiplex reverse transcription PCR assay for simultaneous detection of 11 respiratory viruses, Mycoplasma pneumoniae and Chlamydia in hospitalized children with acute respiratory infections. Diagn Microbiol Infect Dis. 2017;88(2):115–119. doi:10.1016/j.diagmicrobio.2017.03.010
10. Agca H, Akalin H, Saglik I, Hacimustafaoglu M, Celebi S, Ener B. Changing epidemiology of influenza and other respiratory viruses in the first year of COVID-19 pandemic. J Infect Public Health. 2021;14(9):1186–1190. doi:10.1016/j.jiph.2021.08.004
11. Zhang RX, Chen DM, Qian Y, et al. Surges of hospital-based rhinovirus infection during the 2020 coronavirus disease-19 (COVID-19) pandemic in Beijing, China. World J Pediatr. 2021;17(6):590–596. doi:10.1007/s12519-021-00477-2
12. Edridge AWD, Kaczorowska J, Hoste ACR, et al. Seasonal coronavirus protective immunity is short-lasting. Nat Med. 2020;26(11):1691–1693. doi:10.1038/s41591-020-1083-1
13. van der Hoek L. Human coronaviruses: what do they cause? Antivir Ther. 2007;12(4 Pt B):651–658. doi:10.1177/135965350701200S01.1
14. Dijkman R, Jebbink MF, Gaunt E, et al. The dominance of human coronavirus OC43 and NL63 infections in infants. J Clin Virol. 2012;53:135–139. doi:10.1016/j.jcv.2011.11.011
15. Lawrenz J, Xie Q, Zech F, et al. Severe acute respiratory syndrome coronavirus 2 vaccination boosts neutralizing activity against seasonal human coronaviruses. Clin Infect Dis. 2022;75(1):e653–661. doi:10.1093/cid/ciac057
16. Kaplonek P, Wang C, Bartsch Y, et al. Early cross-coronavirus reactive signatures of humoral immunity against COVID-19. Sci Immunol. 2021;6:eabj2901. doi:10.1126/sciimmunol.abj2901
17. Dangi T, Palacio N, Sanchez S, et al. Cross-protective immunity following coronavirus vaccination and coronavirus infection. J Clin Invest. 2021;131(24):e151969. doi:10.1172/JCI151969
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
