Back to Journals » International Journal of General Medicine » Volume 15
Epidemiological Characteristics, Antimicrobial Susceptibility Profile, and Surgical Outcome of Complicated Intra-Abdominal Infection at a Tertiary Hospital in Somalia
Authors Yasin NA , Ali AM , Ahmed MA, Keleşoğlu Sİ
Received 6 July 2022
Accepted for publication 9 September 2022
Published 22 September 2022 Volume 2022:15 Pages 7427—7434
DOI https://doi.org/10.2147/IJGM.S379711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nor Abdi Yasin, Abdihamid Mohamed Ali, Mohamed Abdi Ahmed, Salim İdris Keleşoğlu
Department of General Surgery, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Nor Abdi Yasin, Tel +252 615732173, Email [email protected]
Background: Intra-abdominal infections (IAIs) are common surgical emergencies and one of the leading causes of non-trauma deaths in hospitals worldwide. Because of limited resources, most patients in low-income countries experience delayed diagnosis and treatment. To the best of our knowledge, this is the first study to evaluate the epidemiological characteristics, antimicrobial susceptibility profile, and outcome of patients with complicated IAI at a tertiary hospital in Somalia.
Methods: This study included all patients with confirmed IAIs who underwent laparotomy or percutaneous drainage, either emergency or elective, and whose cultures showed growth. Sociodemographic and clinical characteristics, culture results, antimicrobial susceptibility profile, and the type of source control were reviewed.
Results: The prevalence of CIAI was 5.3%, 144 (70%) were male, and 61 (30%) were female. The mean age was 38.6± 8.5 years. Appendicitis was the most common source of infection, accounting for 32%, followed by bowel perforation in 37 (18%). Out of 15 patients with liver abscesses, ten patients had diabetes (67%). E. coli 82 (40%) was the most common isolated organism, followed by Klebsiella pneumonia (n = 44, 21.5%). The prevalence of extended-spectrum beta-lactamase-producing and multidrug-resistant pathogens was 6.8% and 5.9%, respectively. The pathogens revealed a higher antimicrobial resistance against penicillins in 62%, cephalosporins in 54%, and fluoroquinolones in 44%. E. coli showed 2.5– 13% antimicrobial resistance against carbapenems, lower than Klebsiella pneumonia in about 4.5%. Tigecycline, teicoplanin, and linezolid revealed the highest sensitivity against pathogens, about 100%. Source control was achieved by laparotomy in 81%, while the 19% were managed in a percutaneous approach. The mortality rate in our study was 9.3%.
Conclusion: The prevalence of CIAI in our study was 5.3%, with an increasing number of MDR microorganisms isolated from cultures. CIAI and intra-abdominal abscess are significant sources of high morbidity and mortality with sepsis and poor clinical outcome; thus, early detection and intervention are crucial.
Keywords: complicated intra-abdominal infection, antimicrobial resistance, source control, mortality
Introduction
Intra-abdominal infection (IAI) is a pathological condition ranging from uncomplicated appendicitis to advanced fecal peritonitis.1 It is classified as an uncomplicated and complicated intra-abdominal infection. If IAI is left untreated, it complicates intra-abdominal abscess and sepsis, which has significant morbidity and mortality.1 In the World Surgical Infection Society (WSIS) study, the mortality rate of 4553 patients with complicated intra-abdominal infections was 9.2%.2
The most common causes of complicated intra-abdominal infection are appendicitis, cholecystitis, and hollow viscus perforation.1,3
Although the most predominant pathogens related to the intra-abdominal infection are polymicrobial, aerobic, and aerobic microorganisms, the most common pathogen related to IAI is E. coli, followed by Klebsiella pneumonia.3
Age, gender, comorbidities, and immunocompromised patients are the most common risk factors associated with intra-abdominal abscesses. Several studies reported that elderly patients with perforated peptic ulcers had shown fewer signs of peritonitis with subsequent delayed presentation of an intra-abdominal abscess.2 Song et al reported that diabetes mellitus is a significant risk factor for liver abscess.4
Intra-abdominal infections are polymicrobial in origin, and it is associated with a higher antimicrobial resistance rate. For the last two decades, carbapenem-resistant Enterobacterales (CRE) have increased due to improper and epidemic misuse of broad-spectrum antimicrobials and the lack of knowledge about drug resistance.5 Due to limited therapeutic antimicrobial options available for infections caused by CRE lead to higher morbidity, increased risk of intensive care unit admissions, increased mortality, and subsequent healthcare-related expenses. Management of these patients needs to carefully selective use of antibiotics.6
The diagnosis and management of these patients are crucial, though most patients in low-income countries encounter delayed diagnosis and treatment because of restricted resources.
To date, there have been no studies regarding intra-abdominal abscesses reported from Somalia. This study is aimed to assess the etiology, the most common pathogens, antimicrobial susceptibility profile, management, and outcome of complicated intra-abdominal abscess at a tertiary hospital in Mogadishu, Somalia.
Method
This study involved 3840 patients admitted to the General Surgery department of Mogadishu Somalia Turkish Training and Research Hospital between 2018 and 2022, whose medical records were retrospectively reviewed using the hospital information system. All patients with confirmed complicated intra-abdominal abscesses whose cultures showed growth were selected for the study. The applied definition of IAI was described by the WSIS guidelines.
Adult patients (ie, aged 18-years and above) with complicated intra-abdominal abscesses who underwent surgeries or percutaneous drainage, either emergency or elective, were included in the study. Patients with extra-abdominal abscesses and pediatric cases were excluded from the study.
Patients’ demographic characteristics, comorbidities, the origin and location of the abscess, culture results, antimicrobial susceptibility profile, antimicrobial treatment duration, and the management approaches (percutaneous drainage vs open surgery) were extracted from the electronic medical records in the hospital information system (HIS). Patients who underwent percutaneous drainage and open surgery approach were compared in terms of length of hospitalization, treatment, and prognosis.
Cultures were collected intraoperatively and per percutaneous drainage appropriately. Through the standard Kirby-Bauer disk diffusion method, identifying the bacterial pathogens was achieved using eosin methylene blue agar (EMB) and blood agar following the system of the Clinical and Laboratory Standards Institute (CLSI) guidelines. Antimicrobial susceptibility testing (AST) was identified by the disk diffusion zone of growth inhibition using Mueller-Hinton agar and blood agar in cases of Enterococcus species. Cephalosporins combined with amoxicillin-clavulanic acid were used to identify the presence of extended-spectrum beta-lactamase from the positive cultures. The antibiotic susceptibility of the microorganism was studied by using Cefazolin 30 ug, Cefoxitin 30 mcg, Ceftazidime 30 ug, Cefepime 30 ug, Piperacillin/tazobactam 100/10 mcg, piperacillin 100 ug, Ertapenem 10 mcg, Meropenem 10 mcg, amikacin 30 mcg, clindamycin 2 mcg, penicillin G 1 U, Trimethoprim/Sulfamethoxazole 1.25/23.75 mcg, Tetracycline 30 mcg, Erythromycin 15 mcg, Ciprofloxacin 5 mcg, Nitrofurantoin 300 mcg, Tigecycline 15 ug, Colistin 10 mcg, Linezolid 30 mcg, Vancomycin 30 mcg, Daptomycin 30 mcg, and Teicoplanin 30 ug.
All patients gave their informed consent to use their data for research purposes. The ethics approval form was received from the ethics committee of Mogadishu Somalia Turkish Training and Research Hospital (REF. MSTH-8880).
Data were analyzed using Statistical Package for the Social Sciences for Windows version 26.0. The frequencies and percentages, as well as the mean ± (SD), were presented. Binary logistic regressions were performed to assess the association between independent and dependent variables. The 95% confidence interval was calculated. A p-value of <0.05 was considered statistically significant.
Results
This study included a total of 205 patients with an intra-abdominal abscess who underwent intervention. The prevalence of cIAI was 5.3%, 144 (70%) were male, and 61 (30%) were female. The mean age was 38.6±8.5 years [18–90 years]. In terms of comorbidities, most cases (74%) had no underlying associated comorbidities. However, the most common comorbidity associated with these patients was diabetes (n = 30, 15%), hypertension (6%), and malignancy (3%).
Regarding the abscess location, the most common was an intra-peritoneal collection in 90% (n = 185) of the cases. Most of these intra-peritoneal collection patients (n = 137) were related to intra-abdominal infection and luminal perforation. In contrast, 48 patients originated in the visceral organs such liver, spleen, and pancreatic, and the remaining 20 patients had a retroperitoneal origin.
The most common cause of intra-abdominal abscess in our patients was perforated appendicitis accounting for 32% (n = 66). About 86% of appendicitis patients had a perforated appendix with local peritonitis; an appendectomy was performed. The remaining 14% of the patients had a huge collection, followed by bowel perforation, right hemicolectomy, and end ileostomy was performed.
The second most common cause of intra-abdominal abscess was bowel perforation (37, 18%). Right hemicolectomy was performed for patients with cecal mass and cecal perforation, while Hartman procedure and colonic resection and anastomosis were done with diverticulitis and sigmoid tumor patients. In small bowel perforation, 14 patients with jejunoileal perforation resection and anastomosis were done, while six patients with terminal ileum perforation were done with an ileostomy.
Gastroduodenal perforation-related peptic ulcer perforation (PUD) was diagnosed in 30 (15%) patients and managed by graham procedure repair.
Liver abscess was the most common visceral abscess detected in 15 (7%) patients, followed by psoas abscess and pancreatic abscess 9 and 7 (4%), respectively. Out of 15 patients with liver abscesses, ten patients had diabetes (67%).
The most common organisms isolated from aspirated cultures in patients with intra-abdominal abscesses belonged to gram-negative bacteria (n = 143, 70%), while (n = 23, 11%) were gram-positive bacteria (Table 1). E. coli was the most common isolated organism, which accounted for 82 (40%), followed by Klebsiella pneumonia (n = 44, 21.5%), Enterococcus 22 (11%), Pseudomonas aeruginosa 9(4.7%), proteus 6(3%), and abdominal tuberculosis in 5 (2.5%) patients. Nonetheless, 13 (6.3%) patients admitted to the intensive care unit (ICU) had polymicrobial microorganisms. The prevalence of ESBL-producing pathogens was 6.8% (n = 14). The most common ESBL-producing pathogens were E. coli in about 10/14 of ESBL cases, followed by Klebsiella in about 4/14. Moreover, 5.9% (n = 12) had a multidrug-resistant pattern; Pseudomonas aeruginosa showed the highest MDR pattern at about 33%, followed by E. coli at 11%.
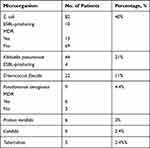 |
Table 1 Distribution of Microorganisms |
Most intra-abdominal abscess patients (n = 167, 81%) were managed in an open procedure, while 19% of the patients were managed in a percutaneous approach. Our review analysis regarding the mode of management, either an open procedure or percutaneous approach, revealed that patients who underwent percutaneous drainage had a prolonged length of drainage, 56% in more than 20 days compared to open procedure which was observed in 3.2% of the cases (p < 0.001) (Table 2). Furthermore, there was no statistically significant difference in length of hospitalization between open surgical procedures and percutaneous approaches (p = 0.115). In terms of duration of antibiotic therapy, 67% of percutaneous cases get antibiotic therapy for more than two weeks compared to open surgical procedure cases (32% vs 19.7%, respectively) (p < 0.001).
 |
Table 2 Patient Characteristics and Mode of Management |
The mortality rate in our study was 9.3%. No statistically significant difference was observed regarding the mortality of patients who underwent a percutaneous approach or an open procedure, 5% in the percutaneous group vs 10% in open procedure cases (p = 0.977).
The study findings revealed a higher antimicrobial resistance against pathogens (ie, penicillins in 62%, Cephalosporins in 54%, and Fluoroquinolones in 44%). (Table 3) demonstrates a deep insight view of antimicrobial resistance against pathogens.
 |
Table 3 Antimicrobial Resistance Rate Against Isolated Microorganisms |
Ampicillin (97%), SMX-TMP (80%), Cefazolin (69%), Cefotaxime (66%), and Cefuroxime (60%) showed the highest individual antimicrobial resistance against the pathogens. Nevertheless, the least antimicrobial resistance was observed against Imipenem (5%), Cefoperazone-sulbactam (4.4%), Ertapenem (4%), Amikacin (3%), and Vancomycin (3%). The highest sensitivity against pathogens was revealed in Tigecycline, Teicoplanin, and Linezolid at about 100%.
In our study, E. coli was the most common isolated pathogen that showed bacterial growth. The highest resistant against E. coli were seen in Ampicillin (96%), SMX/TMP (88%), Cefazolin (79.4%), Cefotaxime (76%), Cefixime (70%), and Cefuroxime (69%). Klebsiella pneumonia had 4.5% antimicrobial resistance against carbapenems, lower than E. coli in about 2.5–13%. The anti-pseudomonal antibiotics had revealed higher antimicrobial resistance against the Pseudomonas aeruginosa, 50% against Ceftazidime, 100% and 71% against Ciprofloxacin, and Levofloxacin, and 33% toward Amikacin. Fortunately, the pathogen had a 100% sensitivity rate against Colistin.
Discussion
Intra-abdominal infections (IAIs) are common surgical emergencies and one of the leading causes of non-trauma deaths in hospitals worldwide. Intra-abdominal abscess secondary to complicated intra-abdominal infection is a frequent and challenging issue manifested as peritonitis originating from gastrointestinal perforation, ischemia, anastomosis leakage, and after trauma. Because of limited resources, most patients in low-income experience delayed diagnosis and treatment. To the best of our knowledge, this is the first study to evaluate the epidemiological characteristics, antimicrobial susceptibility profile, and outcome of patients with complicated intra-abdominal infection at a tertiary hospital in Somalia. The prevalence of CIAI in our study was 5.3%, comparable to a prospective study of 465 patients admitted to ICU by Adrian et al, who reported a prevalence rate of about 5.7%.6 Another study from Germany revealed a large number of intra-abdominal infections, an estimated rate of 120,000 annually.7 A similar study by Toar et al from six tertiary hospitals in Indonesia reported a higher prevalence of cIAI at about 10%.8
According to the source of infection in our study, the most common cause was complicated appendicitis. Perforated appendicitis remains the most indication of laparotomy for virgin and relaparotomy cases in Africa, particularly in Sub-Saharan African countries.1,3,6 Most patients came with local or generalized peritonitis or septic condition with local paracolic, pelvic or huge intra-abdominal abscess. This is due to the late presentation and miss diagnosis of the patients and inadequate surgical service and expertise at the primary hospital.
Bowel perforation and gastro-duodenal perforations secondary to trauma and pathological causes were the second and third most common cause related to an intra-abdominal abscess, with similar studies reported from Lithuania and South Africa.9,10 In developing countries like Somalia, iatrogenic injuries and anastomotic leakage with secondary peritonitis and an intra-abdominal abscess were due to misdiagnoses and malpractice from non-specialized and expert surgeons in the country’s peripheries, where inadequate health service and weak health systems exist. Two-thirds of patients with liver abscesses had diabetes, and diabetes mellitus is a significant risk factor, a common related comorbid, and has a highly significant mortality rate in patients with primary liver abscess.11 Our patients with primary liver abscesses were managed with percutaneous drainage and antibiotics.
Although the most predominant pathogens related to the intra-abdominal infection are polymicrobial, aerobic, and aerobic microorganisms, the most common pathogen related to IAI is E. coli, followed by Klebsiella pneumoniae.3 In our study, the prevalence of ESBL-producing pathogens was 6.8%, E. coli and Klebsiella pneumonia was the most predominant EBSL-producing pathogens, which coheres to a six-year surveillance study by Adrian J. Brink, who reported a higher ESBL-producing E. coli and Klebsiella pneumonia of about 7.6% and 41.2%, respectively.12
Appropriate antimicrobial therapy is an essential component for the treatment of cIAI. Several studies reported an increasing antimicrobial resistance among pathogens causing complicated intra-abdominal infections. The increasing number of multidrug-resistant (MDR) microorganisms (a pathogen resistant to at least one antibiotic drug in three or more antimicrobial classes) isolated from cultures is an increasing health threat and a public health issue.13 The MDR rate in our study was 5.9%; Pseudomonas aeruginosa showed the highest MDR pattern, followed by E. coli. Second- and third-generation cephalosporins are the most common antibiotic classes prescribed for most admitted patients with cIAI as the initial empirical antimicrobial therapy. However, they have shown the highest resistance rate against microorganisms.14
The least antimicrobial resistance was observed against carbapenems, cefoperazone-sulbactam, amikacin, and vancomycin, while tigecycline, teicoplanin, and linezolid revealed the highest sensitivity against pathogens. Poorly controlled use of wide-spectrum antibiotics results in widespread antimicrobial resistance that necessitates increased health-care costs, prolonged hospital stay, intensive care unit admissions, and significant morbidity and mortality.15
Regarding the management aspect of patients with cIAI, most patients were managed in an open procedure, while 19% were managed in a percutaneous approach. Our review analysis regarding the mode of management, either an open procedure or percutaneous approach, revealed that patients who underwent percutaneous drainage had a prolonged length of drainage and antibiotic therapy than an open approach. However, percutaneous drainage benefits shorter hospitalization and procedure time and can be performed bedside for patients admitted to the ICU without the risk of anaesthesia, which carries lower morbidity.16 Source control can be achieved by an open surgical approach or minimally-invasive percutaneous drainage to identify the origin of peritonitis, control the cause of abdominal sepsis, and drain fluid collections. In low-resource countries like Somalia, surgery still remains a crucial part of our daily procedures.
A retrospective study conducted by Rausei et al of 111 patients affected by abdominal sepsis and treated with an open abdomen over nine years reported that early source control of severe IAI patients using an open abdomen could significantly improve the outcome.17
The intra-abdominal infection (IAI) remains a severe concern worldwide and is the second most common cause of sepsis in critically ill patients. Despite improvements in the management of cIAIs, mortality rates are still high, ranging from 2% in appendicitis to as high as 30–35% in patients with peritonitis, depending on the anatomic origin, severity of infection, and comorbidity.18 In our study, the mortality rate was 10%.
Intra-abdominal infection (IAI) is a fatal condition that requires urgent diagnosis and management, including fluid resuscitation, appropriate antibiotic therapy, and hemodynamic status measurements.
Conclusion
The prevalence of CIAI in our study was 5.3%, with an increasing number of MDR microorganisms isolated from cultures. The study findings revealed that patients who underwent percutaneous drainage have the benefits of shorter hospitalization and procedure time without the risk of anaesthesia, particularly for patients admitted to the ICU. In low-resource countries like Somalia, open surgery still remains a crucial part of our daily procedures and can be achieved with adequate source control. Complicated intra-abdominal infection and intra-abdominal abscess are significant sources of high morbidity and mortality with sepsis and poor clinical outcome; thus, early detection and intervention are crucial.
Abbreviations
AST, antimicrobial susceptibility testing; CIAI, complicated abdominal infection; CRE, carbapenem-resistant Enterobacterales; CLSI, Clinical and Laboratory Standards Institute; E. coli, Escherichia coli; ESBLs, extended-spectrum beta-lactamase; IAI, intra-abdominal infections; EMB, eosin methylene blue agar; ICU, intensive care unit; HIS, hospital information system; MDR, multidrug-resistant; PUD, peptic ulcer perforation; WSIS, World Surgical Infection Society.
Data Sharing Statement
Data included in the manuscript.
Institutional Review Board Statement
The ethical research board committee of Mogadishu Somalia Turkish Training and Research Hospital (REF. MSTH-8880) approved the research. This study was carried out in accordance to the Helsinki Declaration contents.
Informed Consent Statement
All patients gave their informed consent to use their data for research purposes.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that this study has not received any funding resources.
Disclosure
The authors report no conflicts of interest associated with this publication.
References
1. Sartelli M, Catena F, Ansaloni L, et al. Complicated intra-abdominal infections worldwide: the definitive data of the CIAOW Study. World J Emergency Surg. 2014;9(1):1–10. doi:10.1186/1749-7922-9-1
2. Sartelli M, Coccolini F, Kluger Y, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emergency Surg. 2021;16(1):1–48. doi:10.1186/s13017-020-00345-w
3. Mikamo H, Yuasa A, Wada K, et al. Optimal treatment for complicated intra-abdominal infections in the era of antibiotic resistance: a systematic review and meta-analysis of the efficacy and safety of combined therapy with metronidazole. Open Forum Infect Dis. 2016;3(3). doi:10.1093/ofid/ofw143
4. Blot S, Antonelli M, Arvaniti K, et al. “Epidemiology of intra-abdominal infection and sepsis in critically ill patients:“AbSeS”, a multinational observational cohort study and ESICM Trials Group Project.”. Intensive Care Med. 2019;45(12):1703–1717. doi:10.1007/s00134-019-05819-3
5. Lalisang TJ, Usman N, Hendrawidjaya I, et al. Clinical practice guidelines in complicated intra-abdominal infection 2018: an Indonesian perspective. Surg Infect (Larchmt). 2019;20(1):83–90. doi:10.1089/sur.2018.120
6. Abebe K, Geremew B, Lemmu B, Abebe E. Indications and outcome of patients who had re-laparotomy: two years’ experience from a teaching hospital in a developing nation. Ethiop J Health Sci. 2020;30(5):739. doi:10.4314/ejhs.v30i5.13
7. Sileikis A, Kazanavicius D, Skrebunas A, Ostapenko A, Strupas K. Prediction for a planned relaparotomy in secondary peritonitis. Cent Eur J Med. 2013;8(4):410–414.
8. Mnguni MN, Muckart DJ, Madiba TE. Abdominal trauma in Durban, South Africa: factors influencing outcome. Int Surg. 2012;97(2):161–168. PMID: 23102083; PMCID: PMC3723215. doi:10.9738/CC84.1
9. Yang CC, Chen CY, Lin XZ, Chang TT, Shin JS, Lin CY. Pyogenic liver abscess in Taiwan: emphasis on gas-forming liver abscess in diabetics. Am J Gastroenterol. 1993;88(11):43.
10. Wong OF, Ho PL, Lam SK; 黄凱峯, 何栢良, 林成傑. Retrospective review of clinical presentations, microbiology, and outcomes of patients with psoas abscess. Hong Kong Med J. 2013;19(5):416–423. doi:10.12809/hkmj133793
11. Ferraioli G, Garlaschelli A, Zanaboni D, et al. Percutaneous and surgical treatment of pyogenic liver abscesses: observation over a 21-year period in 148 patients. Dig Liver Dis. 2008;40(8):690–696. doi:10.1016/j.dld.2008.01.016
12. Brink AJ, Botha RF, Poswa X, et al. Antimicrobial susceptibility of gram-negative pathogens isolated from patients with complicated intra-abdominal infections in South African hospitals (SMART Study 2004–2009): Impact of the new carbapenem breakpoints. Surg Infect (Larchmt). 2012;13(1):43-49. doi:10.1089/sur.2011.074
13. Seguin P, Laviolle B, Chanavaz C, et al. Factors associated with multidrug-resistant bacteria in secondary peritonitis: impact on antibiotic therapy. Clin Microbiol Infect. 2006;12(10):980–985. doi:10.1111/j.1469-0691.2006.01507.x
14. Mohamed AH, Mohamud HA, Arslan E. Epidemiological characteristics and predisposing factors for surgical site infections caused by bacterial pathogens exhibiting multidrug-resistant patterns. Antibiotics. 2021;10(6):622. doi:10.3390/antibiotics10060622
15. Solomkin J, Hershberger E, Miller B, et al. Ceftolozane/tazobactam plus metronidazole for complicated intra-abdominal infections in an era of multidrug resistance: results from a randomized, double-blind, Phase 3 trial (ASPECT-cIAI). Clin Infect Dis. 2015;60(10):1462–1471. doi:10.1093/cid/civ097
16. Wu XW, Zheng T, Hong ZW, et al. Current progress of source control in the management of intra-abdominal infections. Chin J Traumatol. 2020;23(06):311–313. doi:10.1016/j.cjtee.2020.07.003
17. Rausei S, Pappalardo V, Ruspi L, et al. Early versus delayed source control in open abdomen management for severe intra-abdominal infections: a retrospective analysis on 111 cases. World J Surg. 2018;42:707–712. doi:10.1007/s00268-017-4233-y
18. Chong YP, Bae IG, Lee SR, et al. Clinical and economic consequences of failure of initial antibiotic therapy for patients with community-onset complicated intra-abdominal infections. PLoS One. 2015;10(4):e0119956. doi:10.1371/journal.pone.0119956
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
