Back to Journals » International Journal of General Medicine » Volume 15
Epidemiological Characteristics and Risk Factors Associated with Acute Myocardial Infarction in Somalia: A Single-Center Experience
Authors Farah Yusuf Mohamud M
Received 29 July 2022
Accepted for publication 23 September 2022
Published 30 September 2022 Volume 2022:15 Pages 7605—7617
DOI https://doi.org/10.2147/IJGM.S383690
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mohamed Farah Yusuf Mohamud
Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Mohamed Farah Yusuf Mohamud, Mogadishu Somali-Turkish Training and Research Hospital, 30 Street, Alikamin, Wartanabada District, Mogadishu, Somalia, Tel +252615591689, Email [email protected]
Introduction: Acute myocardial infarction (AMI) is a clinical emergency condition that encompasses STEMI and NSTEMI that leads to significant morbidity and mortality rate.
Methods: This prospectively cohort study was obtained from adult (≥ 18 years) patients with definitive diagnosis of AMI based on the International Classification of Diseases (ICD; codes I21, I22) those visiting to our hospital from December 2020 to November 2021. Patients with no definite diagnosis of MI and those having with stable or unstable angina were excluded from the study. Descriptive methods including frequency of tables and bar charts for different categories were used for data analysis.
Results: Of 23,147 patients, 3526 were presented with chest pain in our emergency unit over the study period. A total of 97 patients met the inclusion criteria of AMI for this analysis. Of them, 73 (75.3%) had STEMI, and 24 (24.7%) had NSTEMI. Those with STEMI, anterior MI was common occlusion site (n=24, 32.9%) followed by inferior MI (n=15, 20.5%). The mean age of patients was 54.2± 12.1 years. Of the total study subjects, 67 (69.1%) were males with no significant difference in subgroups. Most of the participants were married (n=41, 42.3%). More than half of the patients were employed (n=51, 52.6%), while most of the participants were no formal education (n-39, 44.2%). Regarding the ASCVD risk factors, history of hypertension, diabetes mellitus, previous history of coronary artery disease (CAD), and dyslipidemia were the most common comorbidities in STEMI and NSTEMI cases, 31 (41.2%), 36 (49.3%), 24 (32.9%) and 15 (20.5%) vs 14 (66.7%), 11 (45.8%), 11 (45.8%), and 6 (25%), respectively. On the initial clinical presentations, typical chest pain and palpitation were the most frequent clinical presenting symptoms in both STEMI and NSTEMI patients of our study (STEMI=80.4% vs NSTEMI=68% in each), followed by dyspnea (STEMI=72.6% vs NSTEMI=41.7%) and epigastric pain (STEMI=32.9% vs NSTEMI=29.2%). The use of aspirin, clopidogrel, and LMWH therapy within the first hours after the emergency were high and comparable in both subgroups (91.8%, vs 89.7% vs 89.7%). The majority of the patients developed heart failure (36.1%), arrhythmia (23.7%), and cardiogenic shock (18%).
Conclusion: As registered, the present study has a higher proportion of STEMI cases among the AMI participants when compared to the NSTEMI. Hypertension, diabetes, hyperlipidemia, and family history of CAD respectively were the highest prevalence risk factors of AMI.
Keywords: myocardial infarction, diabetic, hypertension, emergency, Somalia
Introduction
In 2020 as the World Health Organization reported, cardiovascular illnesses are a significant cause of morbidity and mortality. More than one billion people in Africa suffer from cardiovascular disease, with an estimated 1 million fatalities due to cardiovascular disease (CVD) in sub-Saharan Africa.1 Various factors have been found to have a strong link to the incidence of the acute coronary syndrome (ACS) and treatment outcomes. A history of hypertension, diabetes mellitus, hyperlipidemia, smoking, and familial history of ACS are substantial predictors of ACS outcomes.2,3
The acute coronary syndrome includes ST-elevated MI (STEMI), non-ST-elevated MI (NSTEMI), and unstable angina.4 Acute myocardial infarction (AMI) is a clinical emergency condition that encompasses STEMI and NSTEMI that leads to significant morbidity and mortality rate.4,5 STEMI is a clinical syndrome characterized by the clinical presentation of myocardial ischemia (mostly diagnosed in the presence of ischemic chest pain), persistent ST elevation, and subsequent increased biochemical markers (including troponin level that indicates myocardial necrosis due to complete occlusion of the coronary arteries or its branches).6 Whereas non-ST-elevation (NSTEMI) is characterized by the presence of ischemic chest pain and increased biochemical markers due to incomplete occlusion of the culprit artery in 60–90% of the cases in the.6,7
The majority of the patients with AMI have atherosclerotic cardiovascular disease (ASCVD) risk factors that are recognized to be the prime triggering factor in AMI6,8 Thromboembolism, congenital abnormalities, complications of cardiac catheterization, coronary arteritis, dissection, trauma, and cocaine abuse are among rare non-atherosclerotic causes of AMI.6
Somalia, a country in East Africa that is one of the poorest countries in the world and is currently recovering from a decade-old civil war that has shattered its healthcare system.
Despite the importance of this topic, in our knowledge, no touchable study or data exist on the epidemiological characteristics and risk factor profile of adult patients suffering from acute myocardial infarction (AMI) in Somalia. Therefore, this study aimed to 1) determine the epidemiological characteristics and risk factors in adult patients with no established ASCVD who present with their first AMI and 2) explore clinical presentation, complications, and in-emergency treatment patterns.
Method
This study was based on prospectively collecting data obtained from the Somali population visiting the emergency department at Mogadishu Somali Turkish Training and research Hospital, Mogadishu, Somalia in between December 2020 and November 2021. The hospital approximately has 1000 staff of which almost 600 are health-care professionals. It is mainly involved in the management of internal medicine, emergency medicine, dermatology, ophthalmology, maternal and child health, critical care unit, general surgery, urology, thoracic surgery, cardiovascular surgery, orthopedic, neurosurgery, Otorhinolaryngology mental health, and dental medicine services are functional. More than 50 cardiac patients are seen per day in the hospital.
This prospectively cohort study enrolled adult (≥18 years) patients with definitive diagnosis of AMI based on 2017 European Society of Cardiology Guidelines.2 Patients with no definite diagnosis of MI and those having with stable or unstable angina were excluded from the study. MIs are generally classified into ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI).5
The study used structured questionnaire guide to collect the information. The questionnaire comprised medical history, family history, selected socio-demographics included age, sex, level of education, marital status, and occupation. Lifestyle and other clinical variables included smoking, coffee drinking, and chat chewing habits were also included. The type of AMI, complications, management, and site of addition were reviewed hospital information system (HIS).
Before the data were collected from the field, a pretest was made, by identifying 10 respondents from the target population, in order to identify questions that did not make sense to participants, and other problems within the questionnaire that had probed biased answers. The questions that did not provide useful data were discarded, and final revisions of the questionnaire were made.
To avoid inconsistent about translating from English to Somali language verbally, the structured questionnaire guide which is written in English version was translated into Somali language and the respondents was subjected to a questionnaire with Somali version.
The participants were interviewed individually at their convenient places, and the questionnaire was made anonymous and kept in a lockable cabinet. The enumerators introduced themselves to the study participants and explained the aim of the study and the content of the questionnaire; the respondents were given an option that they could withdraw from process at any point in time. Written informed consent had obtained by each patient.
The data were entered using Microsoft Excel; later on, Statistical Package for the Social Sciences (IBM SPSS) version 23 was used to analyze. Descriptive methods including frequency of tables and bar charts for different categories were used for data analysis methods.
Results
Among the 23,147 participants in the emergency department of Mogadishu Somali Turkish Training and Research Hospital with complete data between December 2020 and November 2021, 3526 patients were presented with chest pain in our center over the study period. A total of 97 (2.8%) patients with first AMI met the inclusion criteria for this analysis. Of them, 73 (75.3%) had STEMI, and 24 (24.7%) had NSTEMI which is based on a clinical presentation, ECG, and laboratory findings (Figure 1). As shown in Figure 2, various sites of acute myocardial infarction were found in the study. Anterior MI was common about 32.9% of the occlusion site followed by inferior MI at 20.5%.
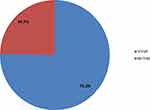 |
Figure 1 Shows the types of acute myocardial infarction in our study population. |
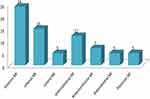 |
Figure 2 Shows various sites of acute myocardial infarction found in the study. |
The mean age of patients was 55.5 ± 17.1 years with a range of 18–95 years. Of the total study subjects, 67 (69.1%) were males with no significant association in both STEMI and NSTEMI subgroups.
According to the marital status of respondents, the majority of participants 42.3% were married, followed by 26.5% were divorced, 19.6% were widowed, while only 11.3% were single. Moreover, 52.6% were employed compared and 47.4% of the respondents unemployed. There is no significant difference between employed and unemployed patients. The majority of the patients had no formal education (n=39, 44.2%), whereas the primary school patients were 26.8%, and 22.5% of the AMI patients had secondary level of education, while 22.25% (n=14) had tertiary (university) level of education.
The prevalence of ASCVD risk factors was high at the time of presentation in both STEMI and NSTEMI cases as shown in Table 1. Diabetes, hypertension, and a family history of CAD were the most common ASCVD in STEMI and NSTEMI participants.
 |
Table 1 Socio-Demographic Characteristics and Risk Factors of AMI Patients in Tertiary Teaching Hospital, Somalia |
Regarding the ASCVD risk factors, 31 (41.2%) STEMI patients and 14 (66.7%) NSTEMI patients had hypertension at admission. Besides, 36 (49.3%) patients with STEMI as well as 11 (45.8%) patients with NSTEMI were found to have diabetes. Among 24 (32.9%) patients of STEMI and 11 (45.8%) patients with STEMI had a family history of CAD. Hyperlipidemia was diagnosed among 15 (20.5%) cases of NSTEMI and 6 (25%) patients with STEMI. Moreover, 29 (39.7%) STEMI and 10 (41.7%) STEMI patients were found to have a smoking history either current or previous. Regarding the history ofKhat Chewing, 27 (37%) patients with STEMI and 16 (66.7%) patients have either current or previous history of khat chewing as shown in Table 1.
Details on the initial clinical presentations, vital signs, and echocardiographic findings of both STEMI and NSTEMI patients are summarized in Table 2.
 |
Table 2 Initial Clinical Presentations, Vital Signs and Echocardiographic Findings prior to the Presentation of AMI Patients in a Tertiary Teaching Hospital, Somalia |
Although typical chest pain of ischemia and palpitation were the most frequent clinical presenting symptoms in both groups (STEMI=80.4% vs NSTEMI=68%), dyspnea (STEMI=72.6% vs NSTEMI=41.7%) and epigastric pain (STEMI=32.9% vs NSTEMI=29.2%) were also frequent.
With regard to vital signs on admission, the average systolic and diastolic blood pressure during admission was 138 (SD±28.1) with a range of 70–240 mmHg and 85.3 (SD±17.1) with a range of 45–140 mmHg respectively. The mean heart rate during the initial presentation was 110 (SD±29.1) with a range of 45–200 bpm.
During our investigation, all patients had performed echocardiography during their hospital stay, and more than two-third of the patients (68%) (STEMI and NSTEMI group) had normal ejection fraction. In this study, 14 (19.2%) patients with STEMI and 5 (20.8%) patients with NSTEMI had heart failure with reduced ejection fraction (HFrEF). Furthermore, 8 (11%) STEMI patients and 4 (16.7%) NSTEMI patients had heart failure with a mid-range ejection fraction (HFmrEF) (Table 2). On the other hand, most of the patients with STEMI or NSTEMI (n=21, (28.8%) vsn=9 (37.5%)) had a normal pulmonary arterial pressure (PAP) (<25mmHg), 23 (31.5%) patients with STEMI and 4 (16.7%) patients with NSTEMI were diagnosed severe pulmonary hypertension (>55 mmHg), and 19 (26%) patients with STEMI and 5 (20.8%) patients with NSTEMI were developed moderate pulmonary hypertension (41–55 mmHg), while 10 (13.7%) patients with STEMI and 6 (25%) patients with NSTEMI were detected mild pulmonary hypertension (25–40 mmHg).
On initial laboratory findings, troponin, creatine kinase-myocardial band (CK-MB), higher total cholesterol, triglycerides, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, electrolytes, and INR levels were evaluated for STEMI and NSTEMI cases as shown in Table 3.
 |
Table 3 Laboratory Findings Prior to the Presentation Among AMI Patients in a Tertiary Teaching Hospital, Somalia |
Regarding the STEMI group, the mean troponins, creatine kinase-MB (CK-MB), international normalized ratio (INR), total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglyceride values were 89.5±97.4, 182.8±221.3, 1.7±1.2, 197.6±42.8, 81.3±31.8, 66.1±24.1, and 145.1±33.3, respectively. Moreover, in the NSTEMI group, the mean Troponins, CKMB, INR, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglyceride values were 79.8±89.4, 162.7±150.7, 1.5±0.9, 185.5±71.8, 110.3±45.2, 61.4±24.4, and 131.2±69.5, respectively.
According to the initial treatment pattern given on admission in the emergency unit for both groups (STEMI and NSTEMI), aspirin was given to 89 (91.8%) patients, 87 (89.7%) patients had received clopidogrel, while 87 (89.7%) patients had received LMWH (6000-IU) and none of our patients received either un-fractionated heparin or enoxaparin. From patients who were eligible for taking morphine was 39.2% (n=38), while 35 (36.1%) patients were indicated to take nitroglycerine. About 28 (28.9%) patients had received beta blocker. As shown in Table 4, the utilization of thrombolysis and defibrillation in the emergency unit immediately after admission was 26 (26.8%) and 23 (23.7%), respectively.
 |
Table 4 Site of Admission, Treatment Patterns and Complications Prior to the Presentation for AMI Patients in a Tertiary Teaching Hospital, Somalia |
Regarding the site of admission, a total of 58 (59.8%) patients were admitted to the ICU, while the remaining 39 (40.2%) patients were admitted non-ICU inpatients departments with no significant difference between STEMI and NSTEMI subgroups.
According to the early complications STEMI and NSTEMI cases in the emergency unit, the majority of the patients developed heart failure (STEMI=27, 37% vs NTEMI=8, 33.3%), followed by arrhythmia (STEMI=18, 24.7% vs NSTEMI=5, 20.8%), and cardiogenic shock (STEMI=14, 19.2% vs NSTEMI=4, 16.7%).
Discussion
Despite the importance of this topic, to our knowledge, no touchable study or data exist on the epidemiological characteristics and risk factor profile of adult patients suffering from acute myocardial infarction (AMI) in Somalia. Therefore, the main purpose of our study is to determine the epidemiological characteristics and risk factors in adult patients with no established ASCVD who present with their first AMI and to explore clinical presentation, complications, and in-emergency treatment patterns.
The historical balance between communicable and non-communicable pathways to CVD in different African regions is dependent on external factors over the life course and at a societal level.9 The future risk of non-communicable forms of CVD (predominantly driven by increased rates of hypertension, smoking, and obesity) is a growing public health concern.
In our study, the mean age of patients was 55.5 ± 17.1 years with a range of 18–95 years. This is comparable with other studies in world like Ethiopia (56.4 ± 13 years), urban India (56.06 ± 11.29 years) and Gulf region of the Middle East (56.4 ± 13 years), but less than Kerala ACS registry in India (60.4 ± 12.1 years).1,10–12 While studies from Western countries were significantly higher in mean age than our study.13–15
In both STEMI and NSTEMI subgroups of the present study, more than two-thirds of patients (n=67, 69.1%) were male and only 30 (30.1%) were female patients (32%). Our findings are consistent with Ethiopian, Indian, and Libyan findings.1,10,16
As registered, the present study has a higher proportion of STEMI cases among the AMI participants when compared to the NSTEMI, which is consistent with prior studies.1,16 In contrast to our findings, studies from the Middle East (such as GULF RACE registry) and the West (such as the Second Euro Heart Survey and the GRACE registry) found that NSTEMI cases were more common than STEMI patients.11,17,18
According to the STEMI subgroup, the anterior wall MI was the most common type (32.9%) followed by inferior wall MI (20.5%) and anterolateral wall MI (16.4%) which is similar to the studies reported from India.10,19 In their investigation, Singh et al found that anterior and inferior MIs were the most common subtypes of STEMI, which differs from the findings of the current data.20
In terms of the present research, ischemic chest pain (60.5%), palpitation (60.5%), shortness of breath (53.5%), and abdominal pain (30.2%) were primarily initial clinical presentations among patients with STEMI and STEMI subgroups. However, ischemic chest pain, palpitation, dyspnea and epigastric pain were significantly higher in STEMI cases when compared to NSTEMI cases. The study from Ethiopia with ACS showed that the dominant presented symptoms were shortness of breath (49.3%), diaphoresis (26.2%), and nausea or vomiting (24.3%).1
According to the risk factors of AMI during our investigation, hypertension (31 (41.2%) patients with STEMI and 14 (66.7%) patients with NSTEMI), diabetes (36 (49.3%) patients with STEMI as well as 11 (45.8%) patients with NSTEMI), and family history of CAD (24 (32.9%) patients of STEMI and 11 (45.8%) patients with STEMI), hyperlipidemia (15 (20.5%) patients with NSTEMI and 6 (25%) patients with STEMI) were the highest prevalence ASCVD risk factors of our study which is compatible with the other studies reported from Greece, India, Ethiopia, Kenya.13,16,21,22 Moreover, in the present study, a large proportion of STEMI patients were more likely to have a current or previous history of cigarette smoking (39.7%), chat chewing (37%), and coffee drinking (31.5%), but they were less likely to have renal failure and COVID-19 pneumonia which is similar which is similar to previous data reported from Greece and South Trinidad.13,23 In contrast to our research, data from Ethiopia found that NSTEMI patients had a history of smoking when compared to STEMI patients (64.9% vs 35.1%).21
In our study, all patients had performed echocardiography, and more than two-third of the patients (68%) (STEMI and NSTEMI group) had normal ejection fraction. In this study, 14 (19.2%) patients with STEMI and 5 (20.8%) patients with NSTEMI had heart failure with reduced ejection fraction (HFrEF). Furthermore, 8 (11%) STEMI patients and 4 (16.7%) NSTEMI patients had heart failure with a mid-range ejection fraction (HFmrEF). In a study from Addis Ababa-Ethiopia, reduced EF (<50%) was higher (66.7%) than in the current study.1
As previously reported, the most inclusive essential component of therapy in STEMI patients still is the appropriate implementation of reperfusion therapy, by either PCI or fibrinolysis, while in NSTEMI cases, an earlier invasive strategy has been sustained.24
In the present research, reperfusion therapy (thrombolysis) was given to 21.9% of STEMI patients, which is much lower than urban India (71.5%), Gulf RACE registry (91%), and GRACE registry (78%) studies.10,11,18 These lower rates can be explained, sometimes lack of thrombolytic druds or its high cost at our center.
Correspondingly, several supplementary medications, including low-molecular-weight heparins, clopidogrel, factor Xa inhibitors, and glycoprotein IIb/IIIa inhibitors, have been proven to be effective.25–27 In the present data revealed that aspirin was given up to 89 (91.8%) patients, 87 (89.7%) patients had received Clopidogrel, while 87 (89.7%) patients had received LMWH (6000-IU) and none of our patients received either un-fractionated heparin or enoxaparin.
Similarly, to the previous studies from India, Kenya, and South Africa, in our analysis, the usage of guideline-recommended medication such as aspirin, clopidogrel, and low-molecular-weight heparin was completely high (91.8%), 89.7%%, and 89.7%%), but none of our patients received either unfractionated heparin or enoxaparin.10,28,29 Furthermore, it is also very high to use the guideline-recommended medications when compared with studies conducted in Ethiopia.1 The treatment of beta-blockers (28.9%) and nitrates (36.1%) during arrival at ED was low in our study compared to other studies from Ethiopia and South Africa.1,30 Moreover, the usage of morphine in our study was 39.2%, which is higher than that of Ethiopia.1
When compared to prior research, the incidence of in-hospital major cardiovascular complications for patients with their first AMI was higher in our current study.10,12,29,30 This is a result of the disease’s late presentation and low level of community awareness.
In the present study, both STEMI and NSTEMI subgroups had a higher incidence of cardiovascular complications, which is a comparable result in the previous studies of myocardial infarction that has been found.10
However, in our study, heart failure was the most frequent complication in our findings (STEMI=27, 37% vs NTEMI=8, 33.3%), which was significantly greater than prior findings.10,30 Moreover, 32.6% of our study population developed one of the different types of arrhythmias. In the current study, about 14 (24.7%) patients with STEMI and 4 (16.7%) patients with NSTEMI developed cardiogenic shock which is significantly higher incidence than studies from Ethiopia, India, Kenya, and Gulf Coast.1,10,28,30
Limitations
To the authors’ knowledge, although this investigation is the first study in determining the epidemiological characteristics, clinical presentation, risk factors, complications, and emergency treatment patterns in adult patients who present with their first AMI in Somalia, it has several limitations.
The limitations of our study include the following: First, the single-center and the small number of observed patients of our analysis might have resulted in a certain extent of bias. Second, deaths before arrival at the hospital and missed diagnoses were the other main limitations of our study. Third, certain risk factors like obesity and stress levels constituted another significant limitation. Third, another notable limitation was the absence of specific risk factors in our study such as obesity and stress levels.
Although our study had a lot of limitations, no touchable study exists on epidemiological characteristics and risk factors associated with acute myocardial infarction among adult patients in Somalia since the collapse of central government of Somalia, so it will be useful and a starting point for other researchers in our country and the region.
Conclusion
In our study of AMI in a prospective cohort study of the Somali population, patients were younger than the Western population, while they were of similar age at the period of index event as compared to low-income countries like Ethiopia and India.
As registered, the present study has a higher proportion of STEMI cases among the AMI participants when compared to the NSTEMI.
Hypertension, diabetes, family history, and hyperlipidemia of CAD (46.5%, 44.2%, 34.9%, and 18.6%) respectively were the highest prevalence risk factors of AMI, and there were no differences between STEMI and NSTEMI subgroups.
Early identification of modifiable risk factors is vital to set the strategy for prevention. However, special attention must be paid to individuals with hypertension, diabetes, family history, and hyperlipidemia.
The researcher argues that there is an influence of hypertension, diabetes, smoking, and dyslipidemia on the AMI status of Mogadishu, Somalia, and suggests the following recommendations:
- To lower the incidence of AMI, more programmes aiming the prevention and control of the ASCVD risk factors in our community should be implemented.
- To implement a coronary care unit and reperfusion center (percutaneous coronary intervention [PCI]) in Somali since there is no cardiac or coronary care unit in the country.
- Further research is needed, as some of the risk factors of AMI that were not mentioned in this research such as physical activity and obesity (BMI) to measure the association between risk factors and AMI. Also, it is needed to evaluate the incidence and long-term outcome of AMI.
Dissemination of Results or Availability of Data and Materials
The data that support the findings of this study are available from Mogadishu Somali Turkish Training and Research Hospital. Data are however available from the author upon reasonable request and with permission of Mogadishu Somali Turkish Training and Research Hospital.
Ethics Approval and Consent to Participate
We obtained an approval letter from the review board of Mogadishu Somali Turkish Training and Research Hospital and written informed consent was obtained for each patient. Patient data confidentiality was respected. This study was carried out in accordance with the Helsinki Declaration contents.
Consent for Publication
The objective of the study was explained in detail to the patients and the parents of unstable patients and all patients obtained informed consent.
Author Contributions
MFYMmade a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have decided on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Bogale K, Mekonnen D, Nedi T, Woldu MA. Treatment outcomes of patients with acute coronary syndrome admitted to TikurAnbessa Specialized Hospital, Addis Ababa, Ethiopia. Clin Med Insights. 2019;13. doi:10.1177/1179546819839417
2. Mirza AJ, Taha AY, Khdhir BR. Risk factors for acute coronary syndrome in patients below the age of 40 years. Egypt Heart J. 2018;70(4):233–235. doi:10.1016/j.ehj.2018.05.005
3. Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343(13):915–922.
4. Graham G. Acute coronary syndromes in women: recent treatment trends and outcomes. Clin Med Insights. 2016;10:CMC–S37145.
5. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
6. Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2021;42(14):1289–1367. doi:10.1093/eurheartj/ehaa575
7. Bob-Manuel T, Ifedili I, Reed G, Ibebuogu UN, Khouzam RN. Non-ST elevation acute coronary syndromes: a comprehensive review. Curr Probl Cardiol. 2017;42(9):266–305. doi:10.1016/j.cpcardiol.2017.04.006
8. Canto JG, Kiefe CI, Rogers WJ, et al. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA. 2011;306(19):2120–2127. doi:10.1001/jama.2011.1654
9. Keates AK, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: epidemiological profile and challenges. Nat Rev Cardiol. 2017;14(5):273–293. doi:10.1038/nrcardio.2017.19
10. Sidhu NS, Rangaiah SK, Ramesh D, Veerappa K, Manjunath CN. Clinical characteristics, management strategies, and in-hospital outcomes of acute coronary syndrome in a low socioeconomic status cohort: an observational study from urban India. Clin Med Insights. 2020;14. doi:10.1177/1179546820918897
11. Zubaid M, Rashed WA, Almahmeed W, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE). Actacardiologica. 2009;64(4):439–446.
12. Mohanan PP, Mathew R, Harikrishnan S, et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34(2):121–129. doi:10.1093/eurheartj/ehs219
13. Andrikopoulos G, Pipilis AT, Goudevenos JO, et al. Epidemiological characteristics, management and early outcome of acute myocardial infarction in Greece: the HELlenic infarction observation study. Hellenic J Cardiol. 2007;48(6):325–334.
14. Chang WC, Kaul P, Westerhout CM, et al. Impact of sex on long-term mortality from acute myocardial infarction vs unstable angina. Arch Intern Med. 2003;163(20):2476–2484. doi:10.1001/archinte.163.20.2476
15. Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin. The Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J. 2002;23(15):1190–1201. doi:10.1053/euhj.2002.3193
16. Abduelkarem AR, El Shareif HJ, Sharif SI. Evaluation of risk factors in acute myocardial infarction patients admitted to the coronary care unit, Tripoli Medical Centre, Libya. EMHJ. 2012;18(4):332–336. doi:10.26719/2012.18.4.332
17. Mandelzweig L, Battler A, Boyko V, et al. Van de Werf F. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27(19):2285–2293. doi:10.1093/eurheartj/ehl196
18. Steg PG, Goldberg RJ, Gore JM, et al.; GRACE Investigators. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE). Am J Cardiol. 2002;90(4):358–363. doi:10.1016/S0002-9149(02)02489-X
19. Jose VJ, Gupta SN. Mortality and morbidity of acute ST segment elevation myocardial infarction in the current era. Indian Heart J. 2004;56(3):210–214.
20. Singh Y, Satyawali V, Joshi A, Joshi SC, Khalil M, Kumar J. The clinical spectrum of acute coronary syndromes: a study from tertiary care centre of Kumaun region of Uttarakhand. Niger J Cardiol. 2014;11(1):27. doi:10.4103/0189-7969.130076
21. Tsegaye T, Gishu T, Habte MH, Bitew ZW. Recovery rate and predictors among patients with acute coronary syndrome in Addis Ababa, Ethiopia: a retrospective cohort study. Res Rep Clin Cardiol. 2021;30(12):9–21. doi:10.2147/RRCC.S307151
22. Chege PM. Multiple cardiovascular disease risk factors in rural Kenya: evidence from a health and demographic surveillance system using the WHO STEP-wise approach to chronic disease risk factor surveillance. S Afr Fam Pract. 2016;58(2):54–61. doi:10.1080/20786190.2015.1114703
23. Bahall M. Epidemiology of acute myocardial infarction in South Trinidad. WIMJ Open. 2016;3(2):1.
24. Kanakakis J, Ntalianis A, Papaioannou G, Hourdaki S, Parharidis G. Stent for Life Initiative–the Greek experience. EuroIntervention. 2012;8(SP):P116. doi:10.4244/EIJV8SPA20
25. Antman EM, Morrow DA, McCabe CH, et al. Enoxaparin versus unfractionated heparin with fibrinolysis for ST-elevation myocardial infarction. N Engl j Med. 2006;354(14):1477–1488. doi:10.1056/NEJMoa060898
26. Sabatine MS, Cannon CP, Gibson CM, et al. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med. 2005;352(12):1179–1189. doi:10.1056/NEJMoa050522
27. Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354(14):1464–1476. doi:10.1056/NEJMoa055443
28. Wachira BW, Owuor AO, Otieno HA. Acute management of ST-elevation myocardial infarction in a tertiary hospital in Kenya: are we complying with practice guidelines?: phase active de priseen charge des infarctus du myocarde avec élévation du segment ST dans un hôpitaltertiaire au Kenya. Les directives pratiquessont-ellesrespectées? Afr J Emerg Med. 2014;4(3):104–108.
29. Brieger D, Eagle KA, Goodman SG, et al.; GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126(2):461–469. doi:10.1378/chest.126.2.461
30. Alfaddagh A, Khraishah H, Rashed W, Sharma G, Blumenthal RS, Zubaid M. Clinical characteristics and outcomes of young adults with first myocardial infarction: results from Gulf COAST. IJC Heart Vasc. 2020;31:100680. doi:10.1016/j.ijcha.2020.100680
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
