Back to Journals » International Journal of General Medicine » Volume 16
Epidemiological and Clinical Characteristics of Measles in Jinan, Shandong Province, China, from 1991 to 2022
Authors Wang XY, Zhang XJ, Xia X, Chang SZ, Wu AZ
Received 3 February 2023
Accepted for publication 19 May 2023
Published 6 June 2023 Volume 2023:16 Pages 2305—2312
DOI https://doi.org/10.2147/IJGM.S407121
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Xiao-Yan Wang,1 Xiao-Jing Zhang,2 Xiao Xia,3 Shu-Zhen Chang,4 An-Zhao Wu4
1Infectious Diseases Department II, Shandong Public Health Clinical Center, Jinan, 250000, People’s Republic of China; 2Public Health Department, Shandong Public Health Clinical Center, Jinan, 250000, People’s Republic of China; 3Medical Insurance Office, Shandong Public Health Clinical Center, Jinan, 250000, People’s Republic of China; 4TCM & Western Medicine Department, Shandong Public Health Clinical Center, Jinan, 250000, People’s Republic of China
Correspondence: An-Zhao Wu, TCM & Western Medicine Department, Shandong Public Health Clinical Center, 2999 Gangxing West Road, High Tech District, Jinan, 250000, People’s Republic of China, Tel +86 531-86568184, Email [email protected]
Objective: This study aimed to analyze the epidemiological and clinical characteristics of measles in Jinan, Shandong, China, over a 32-year stage to facilitate measles prevention in the future.
Methods: Data on measles cases from 1991 to 2022 were obtained from the public health department and medical records of patients at Shandong Public Health Clinical Center. Retrospective analysis was conducted on the distribution of measles cases in different years, months, and age groups, and observation of the differences in clinical manifestations and complications among different age groups.
Results: From January 1991 to December 2022, 7531 measles cases were recorded at Shandong Public Health Clinical Center. During the 32-year period, there were two outbreaks of measles in 2008 and 2016, respectively. During the COVID-19 pandemic period from 2020 to 2022, the number of cases reached the lowest point in the past 30 years. The number and percentage of cases in the 0– 1y groups was significantly higher than in other age groups, and 97.75% patients in this group did not receive measles vaccine. Complications such as pneumonia and myocarditis appeared more frequent in patients under 12 years of age, but liver function damage is more common in adult patients.
Conclusion: Although the measles epidemic has been greatly controlled since the use of measles vaccine, intermittent outbreaks still exist, so there is still a long way to go to eliminate measles. The proportion of infants under the age of 1 without measles vaccine and adults over 24 years old accounts for nearly 80% of the total. This group of people should be of concern, and feasible measures should be designated to protect these susceptible populations.
Keywords: measles, epidemiology, clinical characteristics, vaccination, China
Introduction
Measles, caused by the measles virus, is an acute respiratory infectious disease characterized by high fever, cough, Koplik spots, and rash, which may result in severe complications, such as pneumonia and myocarditis. Persistent immunity can be obtained after the infection is cured.1 Measles is highly contagious and can spread rapidly among individuals, but it can be effectively prevented through vaccination. The development of measles vaccine has significantly reduced the global incidence and mortality rates of the disease. The Americas was the first World Health Organization (WHO) Region to declare measles elimination in September 2016, but periodic outbreaks continue to occur in developing countries and it is still one of the main causes of mortality in children.2 In 2018 alone, the global number of measles deaths exceeded 140,000, with the majority being children under the age of 5.1
In 1965, China initiated the use of measles vaccine, and it was integrated into the national immunization program in 1978.3 Subsequent years saw a marked increase in vaccination coverage, which resulted in the successful control of measles outbreaks. Between 1978 and 1990, China witnessed a significant decline of over 95% in incidences and deaths related to measles.4 At present, China uses the three dose measles vaccine vaccination plan, and children are vaccinated at 8 months, 18–24 months and 4–6 years old. Since 2006, the estimated coverage rate of two doses of measles vaccine in children has exceeded 95%.5 In 2005, all WHO Western Pacific member states, including China, committed to eradicating measles by 2012.6 Elimination is defined as the absence of endemic measles transmission in a region for ≥12 months in the presence of a well-performing surveillance system.2 However, due to China’s vast territory, large population, increase of migrating population and the uneven development of disease prevention and control work across the country, the control of measles is still unsatisfactory. In 2008, measles epidemic occurred in some parts of the country, with more than 130,000 reported cases and an incidence rate of 10/100 000.4 After the 2008 measles outbreak, in September 2010, a nationwide measles supplementary immunization activity was carried out. About 102 million children aged from 8 months to 4 years received measles booster vaccination. In 2011, the measles incidence rate in China decreased by 25.8% compared with the same period last year.7 However, after large-scale booster immunization in children, measles outbreaks still occur, especially from 2015 to 2016. Therefore, the elimination of measles is still a major challenge for China in the future.
Jinan is the capital city of Shandong Province. By the end of 2021, the permanent population was 9.415 million.8 Shandong Public Health Clinical Center (The name was Jinan Infectious Disease Hospital before 2020) is a referral hospital for the diagnosis, report and treatment of infectious diseases including the vast majority measles cases in Jinan area and severe referral patients from neighboring districts; therefore, the number of measles patients diagnosed and treated in our hospital can reflect the level of measles prevalence in this city and even the province. Early symptoms of measles before the appearance of a typical rash are fever and cough, which are not specific. Therefore, patients often seek medical attention at a pediatric or general outpatient clinic at first. If doctors cannot identify and diagnose measles in the first place and fail to take isolation measures, measles spread can occur within hospitals. This study was conducted to investigate the epidemiological and clinical characteristics of measles from 1991 to 2022 at Shandong Public Health Clinical Center. We aim to study the epidemic patterns, clinical characteristics and prevent measures of measles, enhance the medical practitioners’ understanding and awareness of measles, to facilitate the early detection, early isolation and early treatment of measles cases, decrease unnecessary deaths from vaccine preventable infectious disease and also provide reference for international people who have plan to visit here on the epidemic situation of measles in Jinan.
Methods
Data Resources
All the measles cases we included were laboratory-confirmed cases. A laboratory-confirmed measles case was defined as a patient having symptoms and signs compatible with measles and with a positive measles immunoglobulin M (IgM) test. The detection of measles virus RNA in nasopharyngeal aspirates or throat swabs by reverse transcriptase polymerase chain reaction (RT-PCR) was not widely used during the study period. The detection of measles-specific IgM in serum samples was conducted by enzyme-linked immunosorbent assay (Beijing Beier Bioengineering Co., Ltd anti-measles IgM test, China). The laboratory of the hospital operates according to the product manual and the quality control is qualified.
The Public Health Department (name was Epidemiology Department before 2020) of Shandong Public Health Clinical Center is responsible for collecting and organizing infectious disease information reported by clinical doctors, and reporting cases to Centers for Disease Control of Jinan or Shandong Province through the epidemiology report form. The gender, age, onset date, and confirmed date of measles cases can be obtained from the epidemiology report form, then trace the hospitalization medical record based on the personal information of the form. Clinical data, including symptoms, signs, vaccination status, and complications, were obtained from inpatient medical records. The outbreak of measles in 2008 attracted the attention of researchers, and subsequently, case data was collected by the study team in multiple stages to form a dataset, which was ultimately summarized for research and analysis.
Statistical Analysis
The data were analyzed using SPSS 24.0 (IBM, Armonk, New York, USA). Frequency (percentage %) was used to describe the counting data, and chi-square analysis (including Fisher’s exact probability method) was used to analyze the counting data. This study suggests that P<0.05 has statistical significance, and this test is a bilateral test.
Descriptive epidemiology measures were used to retrospectively analyze and describe the annual incidence, season, age distribution, and clinical features of the disease.
Results
Annual Distribution
From January 1991 to December 2022, there were a total of 7531 measles cases documented in Shandong Public Health Clinical Center. The annual distributions are shown in Table 1. From 1991 to 2004, the epidemic level remained extremely low. The number of cases began to increase in 2005 and reached a peak in 2008. Afterwards, the curve gradually declined, but did not decrease to the level before 2005. The number of cases increased significantly again from 2013 to 2016, reaching a highest peak in 2016, and then sharply declined to another extremely low level then likely to be stabilized. During the COVID-19 pandemic period from 2020 to 2022, the number of cases reached the lowest point in the past 30 years. The epidemic curve is shown in Figure 1.
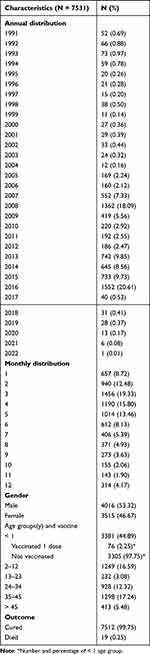 |
Table 1 Annual, Monthly, Gender and Age Groups Distribution of Measles Cases in Jinan, 1991–2022 |
 |
Figure 1 The epidemic trend of measles, 1991–2022. |
Monthly Distribution
The most epidemic months were March, April, and May, and the number of cases in these 3 months accounted for 48.59% of the total number (Table 1).
Age Groups and Gender
Among 7351 cases, 4016 (53.32%) were male and 3515 (46.67%) were female. The ratio was 1.14. The number of cases in different genders is described by the median (four score interval) to describe the distribution characteristics, and non-parametric tests are used for difference analysis. Non-parametric test p=0.541 (p>0.05), indicating no significant difference in the distribution between the genders.
The number of cases in the age groups is described by the median (four score interval) to describe the distribution characteristics, and non-parametric tests are used for difference analysis. There is a significant difference in the overall number of cases among different age groups, p=0.000, <0.05. Subsequent pairwise comparisons showed that the number and percentage of cases in the 0–1y groups was significantly higher than in other age groups. Among the 0–1 year old group, 97.75% patients did not receive any measles vaccine, and 2.5% patients received one dose.
There were 23 pregnant women in measles cases after 2005. The youngest patient was 18 days old, and the oldest patient was 78 years old. Between 2008 and 2016, the proportion of infants under 12 months increased to 52.08%, suggesting that this age group had a large number of susceptible populations.
Main Clinical Features
Table 2 shows that fever, catarrhal symptoms, conjunctivitis, Koplik spots, and rashes are the common clinical manifestations in both <12 years and ≥13 years age groups. Children <12 years are more prone to complications such as diarrhea, pneumonia, laryngitis, myocarditis and thrush, while people ≥13 years are more likely to experience high fever (>39°C), liver function impairment and conjunctivitis.
 |
Table 2 Main Clinical Manifestations and Complications in Different Age Groups (n, %) |
Deaths (16 cases ≤1 year old and 3 cases 1–2 years old) accounted for 0.25% of the total cases, and all the death cases were not vaccinated with measles vaccine.
Discussion
Measles is a systemic infection. The measles virus enters the human body through the respiratory tract or conjunctiva. The virus replicates in large quantities and enters various tissues and organs throughout the body with blood flow, causing inflammatory reactions and tissue damage. After being infected with the measles virus, the body can produce IgM antibodies, indicating a recent infection.9 Measles is also an ancient highly contagious disease, which was ever successfully controlled through vaccination and close to being eliminated in some developed countries. However, in recent years, measles epidemics are occurring again around the world, which raised concern in health practitioners and government departments. The WHO reports that only in 2018, the global number of measles deaths exceeded 140,000, with the majority being among children under 5 years old.1
A 32-year retrospective analysis of measles cases at the Shandong Public Health Clinical Center revealed that from 1991 to 2004, the epidemic level remained at a very low level. The number of cases began to increase in 2005 and reached a peak in 2008. After the 2008 measles outbreak, in September 2010, a nationwide measles supplementary immunization activity was carried out. About 102 million children aged from 8 months to 4 years received measles booster vaccination. In 2011, the measles incidence rate in China decreased by 25.8% compared with the same period last year.7 Otherwise, the number of cases increased significantly again from 2013 to 2016, reaching a highest peak in 2016. Simultaneously, in other areas of China, measles outbreaks were also reported.7 From 2009 to 2021, the vaccination rate of the first dose of measles vaccine for children in China has all reached 95%.10 So, besides children’s vaccination, there are other reasons that need to be investigated in the outbreaks of measles such as population mobility, adult vulnerable population and so on.
Cases in the months of March, April, and May accounted for 48.61% of the total cases, which is consistent with previous data. The age distribution of patients showed that the number and percentage of cases in the 0–1y groups was significantly higher than in the other age groups. Among the 0–1-year old group, 97.75% patients did not receive any measles vaccine, and 2.5% patients received one dose. The two groups of 24–45 years old contributed 29.56% of the total number, indicating that the two major age groups containing more vulnerable individuals. On the other hand, the patients aged 13–23 years and >45 years seem less likely to be affected by the disease. The reason why the infant group did not receive measles vaccine was because 89% of them did not reach the required vaccination age of 8 months and 10% due to suffering cold, fever and other diseases, as well as other contraindications of vaccination. The 8 months age was set eligible to get vaccine because infants younger than 8 months are supposed to get enough protective IgG antibodies from their mothers. But, nowadays the majority of women of childbearing age are being born after the 1980s, having had limited exposure to natural measles infection and relying on measles vaccination for immunity. However, vaccine-induced immunity wanes over time, resulting in insufficient protection for newborns and infants who may lack adequate measles antibodies.11,12 So the infants became vulnerable individuals before they are eligible for a vaccine. Therefore, vaccinating women of child-bearing age not only protects them but it also protects any children they give birth to from measles infection.
So, waning vaccine-induced immunity may have an impact on the control of measles in the future, especially when the vaccinated population becomes aged. People 24–45 years old have a high incidence rate of measles, and so they can also be the group who will benefit from a booster vaccination.10 It is important to maximize the coverage of the immunization program to eliminate susceptibility in the population, and prevent measles epidemic.13 To reschedule the time of measles vaccination or let women of childbearing age receive booster injections could be beneficial strategies.
In our study, certain typical clinical features have been recorded in both infants and adults infected with measles. Normally, fever and coughing are early but not specific symptoms. The infection can be mistaken for a simple upper respiratory tract infection unless further mouth membrane and conjunctiva examinations are performed. Prolonged febrile periods and a high temperature are also common, but some prematurely born or malnourished infants might not show a rise in temperature. In addition, Koplik spots present in 80–90% of all patients, but they are sometimes recognized as thrush in infant patients because the spots last for quite a few days and tend to fuse into patches. Typical eruptions are seen in more than 70% of infant patients, but those who have had their measles vaccine just before illness onset may present with only a mild cough, a temperature <38.5°C, and fewer rashes, making the infection hard to be diagnosed. Infants with malnutrition or those who have been treated with corticosteroids before being referred to the hospital may experience a stumbling eruption process and tend to develop severe conditions. Other symptoms include vomiting, diarrhea and elevated myocardial enzymes. Common complications consist of bronchitis, pneumonia and myocarditis, which can deteriorate and lead to respiratory failure and heart failure in some cases. Serious pneumonia-related respiratory and heart failure is the most serious complication and is the leading cause of death in infants. Severe cases and deaths are more frequently seen in infants under 1 year of age with pre-existing conditions, such as premature birth, malnutrition and congenital heart disease.
Adult patients exhibit common clinical features including high fever (>70%), toxemia, upper respiratory tract inflammation symptoms, conjunctivitis (>90%), gastrointestinal symptoms (37.85%), and Koplik spots. Koplik spots, which appear one to two days before the onset of body rashes, persist for four to five days, are indicative of the early stages of measles and are considered specific characteristic of the disease.14 Elevated alanine aminotransferase and aspartate aminotransferase levels are commonly seen in a liver function test, but they can normalize as the person recovers from the viral infection. In general, adult patients have fewer complications and better outcomes than infants.
Nosocomial infection is a significant transmission pathway of measles during outbreaks. This is because clinicians in general clinics and hospitals might have limited experience on measles, which makes the diagnosis delayed and the measles patients stay or travel in crowded hospital public areas for prolonged time.15,16 In the waiting rooms and outpatient vaccination rooms of some hospitals, many children may have to share a small space, and this facilitates the spread of measles. Early-stage measles infection before the rashes appear tends to spread among people easily, at the same time it is hard to differentiate from other febrile illnesses, so it is important to raise doctors’ awareness of the characteristic signs, such as Koplik spots and conjunctivitis, and to keep in mind that a comprehensive and detailed physical examination is of great importance.
The epidemic level of measles was extremely low during the COVID-19 pandemic years from 2000 to 2022, which may be related to strict isolation and personal protection measures. With the cancellation of control measures and a significant increase in population mobility, the risk for measles epidemic is also rising. There is a possibility of a rebound in the future measles epidemic, measures still need to be taken to prevent a rebound in the measles epidemic.
Conclusion
This study covered the stage from 1991 to 2022, suggesting significant outbreaks of measles still exist in Jinan, Shandong, especially from 2005 to 2016. Koplik’s spots are a specific sign of measles, with an appearance rate of 89%. In febrile patients before the onset of a typical rash, it is important to check oral mucosa to help detect measles patients early. Infants under 1 year accounted for 44.89% of all cases, 97.75% of which were not vaccinated with measles vaccine. The 19 deaths are all children under 2 years old, and none of them were vaccinated. How to protect the large vulnerable population of infants and young children and avoid deaths caused by vaccine-preventable diseases is a problem that we need to take into consideration. To reschedule the time of measles vaccination or let women of childbearing age receive booster injections could be beneficial strategies. Measles prevalence was extremely low during the 3-year COVID-19 pandemic. With the removal of isolation measures, people’s activities increased significantly, measures still need to be taken to prevent a rebound in the measles epidemic.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Shandong Public Health Clinical Center. This is a retrospective analysis of routinely collected anonymised data. Only medical record information was collected, and written informed consent from all patients and guardians was not obtained.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Measles fact sheet; 2023. Available from: http://www.who.int/mediacentre/factsheets/fs286/en/.
2. Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the postelimination era, 2001–2016. J Infect Dis. 2019;219(10):1616–1623. PMID: 30535027; PMCID: PMC6474820. doi:10.1093/infdis/jiy701
3. Wang X, Boulton ML, Montgomery JP, et al. The epidemiology of measles in Tianjin, China, 2005–2014. Vaccine. 2015;33(46):6186–6191. PMID: 26469719; PMCID: PMC4644448. doi:10.1016/j.vaccine.2015.10.008
4. Chinese Center for Disease Control and Prevention. It is imperative to eliminate measles in China; 2010. Available from: https://www.chinacdc.cn/jkzt/crb/zl/mz/gzjz/201004/t20100426_24210.html.
5. Montgomery JP, Zhang Y, Carlson B, Ewing S, Wang X, Boulton ML. Measles vaccine coverage and series completion among children 0–8 years of age in Tianjin, China. Pediatr Infect Dis J. 2015;34(3):289–295. PMID: 25259932; PMCID: PMC4355170. doi:10.1097/INF.0000000000000562
6. Moss WJ, Griffin DE. Global measles elimination. Nat Rev Microbiol. 2006;4(12):900–908. PMID: 17088933; PMCID: PMC7097605. doi:10.1038/nrmicro1550
7. Gao J, Chen E, Wang Z, et al. Epidemic of measles following the nationwide mass immunization campaign. BMC Infect Dis. 2013;13:139. PMID: 23506461; PMCID: PMC3606834. doi:10.1186/1471-2334-13-139
8. Jinan Municipal People’s Government. Ethnic and population; 2023. Available from: http://www.jinan.gov.cn/col/col24701/.
9. Preston J. Measles. Nurs Stand. 2015;29(27):60. PMID: 25736676. doi:10.7748/ns.29.27.60.s46
10. World Health Organization. Measles, 1st dose (MCV1) Immunization coverage estimates by country; 2021. Available from: https://apps.who.int/gho/data/view.main.80100?lang=en.
11. Chong KC, Rui Y, Liu Y, et al. Early waning of maternal measles antibodies in infants in Zhejiang Province, China: a comparison of two cross-sectional serosurveys. Int J Environ Res Public Health. 2019;16(23):4680. PMID: 31771262; PMCID: PMC6926550. doi:10.3390/ijerph16234680
12. Khampanisong P, Pauly M, Nouanthong P, et al. Waning of maternal antibodies against measles suggests a large window of susceptibility in infants in Lao People’s Democratic Republic. Pathogens. 2021;10(10):1316. PMID: 34684265; PMCID: PMC8538652. doi:10.3390/pathogens10101316
13. Yang X, Tang T, Yang Z, Liu L, Yuan S, Zhang T. Evaluation of measles vaccination coverage in Lincang City, Yunnan Province, China. Hum Vaccin Immunother. 2021;17(9):3145–3152. PMID: 33847247; PMCID: PMC8381781. doi:10.1080/21645515.2021.1911215
14. Zhang Y, Yu YS, Zang GQ. Maculopapular rash and Koplik’s spots in adult measles. Rev Soc Bras Med Trop. 2015;48(2):231. PMID: 25992944. doi:10.1590/0037-8682-0236-2014
15. Vink JP, Snell LB, Bernard K, et al. Mapping a nosocomial outbreak of measles, coinciding with a period of sustained transmission in South London in 2018. J Hosp Infect. 2020;105(4):747–751. PMID: 32544506. doi:10.1016/j.jhin.2020.06.004
16. Botelho-Nevers E, Gautret P, Biellik R, Brouqui P. Nosocomial transmission of measles: an updated review. Vaccine. 2012;30(27):3996–4001. doi:10.1016/j.vaccine.2012.04.023
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
