Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Environmental Factors in the Etiology of Mental Disorders in the Czech Republic
Authors Hosak L, Hosakova K , Malekirad M , Kamaradova Koncelikova D, Zapletalova J , Latalova K
Received 23 June 2022
Accepted for publication 24 December 2022
Published 7 February 2023 Volume 2023:19 Pages 349—359
DOI https://doi.org/10.2147/NDT.S379811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Ladislav Hosak,1 Kristyna Hosakova,1 Mohammad Malekirad,1 Dana Kamaradova Koncelikova,2 Jana Zapletalova,3 Klara Latalova2
1Department of Psychiatry, Charles University, School of Medicine in Hradec Kralove and University Hospital, Hradec Kralove, Czech Republic; 2Department of Psychiatry, Palacky University Olomouc, Faculty of Medicine and Dentistry and University Hospital, Olomouc, Czech Republic; 3Department of Medical Biophysics, Palacky University Olomouc, Faculty of Medicine and Dentistry, Olomouc, Czech Republic
Correspondence: Ladislav Hosak, Department of Psychiatry, University Hospital, Sokolska 581, Hradec Kralove, 500 05, Czech Republic, Tel +420 495 833 478, Fax +420 495 833 041, Email [email protected]
Background: Both genetic and environmental factors are important in etiology of mental disorders. Calculating polyenviromic risk/protective scores provides an updated perspective in research on the environmental causes of psychiatric disorders. We aimed to compare environmental risk and protective factors in patients with psychosis or a mood disorder (PSYCH+MOOD) and those with an anxiety disorder (ANX).
Methods: We administered the internationally accepted questionnaire from the EUropean Network of National Schizophrenia Networks Studying Gene-Environment Interactions (EU-GEI) study, enriched with mood and anxiety disorder-relevant measures, to patients at two large university hospitals in the Czech Republic.
Results: Ninety-four PSYCH+MOOD patients (average age 42.5 years; 46 males) and 52 ANX patients (average age 47.2 years; 17 males) participated. Neither polyenviromic risk score nor polyenviromic protective score differed significantly between PSYCH+MOOD and ANX groups (p = 0.149; p = 0.466, respectively).
Conclusion: Scientific validity of the polyenviromic risk/protective score construct must still be demonstrated in large psychiatric samples, ideally in prospective studies. Nevertheless, researchers have already started to investigate environmental factors in the etiology of mental disorders in their complexity, similarly to polygenic risk scores.
Keywords: anxiety disorders, environmental factors, mood disorders, schizophrenia, stress
Plain Language Summary
- Environmental factors, which may be biological, psychological, societal or spiritual, are important in etiology of mental disorders.
- Assessment of environmental factors may contribute to prevention and treatment of psychiatric disorders.
- A summarizing evaluation of environmental etiological factors using polyenviromic risk/protective scores is an updated approach.
- We examined polyenviromic risk/protective scores in 146 psychotic, mood or anxiety disorder patients hospitalized in two large university hospitals in the Czech Republic.
- Polyenviromic risk/protective scores did not differ significantly between the sample with psychoses/mood disorders versus the group with anxiety disorders.
- Our results emphasize the need for further research of environmental factors in the etiology of mental disorders in their complexity, similarly to polygenic risk scores.
Introduction
The lifetime prevalence of mental disorders is estimated at 12.0 −47.4%.1 A substantial portion of mental disorders are chronic or lifelong, including substance addictions,2 schizophrenia,3 bipolar disorder,4 recurrent major depression5 and obsessive-compulsive disorder.6 If we aim at full, lifelong remission, therapeutic outcomes are far from satisfactory. One reason for this is that we do not understand mental disorders´ etiology well, so therapy cannot be causal. In almost all mental disorders, both genetic and environmental etiological factors are needed to induce clinical symptoms.7 This is why “exposome” (which is the sum of significant environmental triggers) is studied. A novel avenue of research assesses the sum of an individual´s environmental exposures to create their polyenviromic risk score (PERS).8 An individual´s PERS is calculated as follows: first, the odds ratio for each evidence-based environmental risk factor is obtained based on literature; next, the presence or absence of each environmental risk factor is determined for the participant and the log of the odds ratio for each environmental risk factor is multiplied by either 1 (risk factor is present) or 0 (risk factor is absent); these values are summed and then divided by the total number of risk factors assessed.8 In this way, environmental risk factors are aggregated. Thus, the PERS is adapted from the formula used to calculate polygenic risk scores.9 It is also useful to study mental disorders as cumulative groups, rather than as individual diagnostic entities. This is because etiological factors overlap among disorders, meaning that higher-level, broad categorical constructs may be more appropriate targets of etiological research than specific diagnoses.10 Furthermore, both environmental risk factors and those that are protective should be assessed.11 The polyenviromic protective score is calculated like the PERS.
The aim of our study was to investigate the lifetime presence of both environmental risk factors and protective variables in patients with psychosis or a mood disorder (PSYCH+MOOD), compared with patients with an anxiety disorder (ANX). We used this group configuration because the genetic backgrounds of psychoses and mood disorders overlap, but are distinct from anxiety disorders.12,13 We tested the main hypothesis that the PERS and polyenviromic protective score differ between the PSYCH+MOOD and ANX groups. This hypothesis is based on the presumption that heritability is higher in psychoses and mood disorders compared with anxiety disorders.9,14 Schizophrenia, bipolar disorder and major depressive disorder are closely and causally linked; thus, using a broad mental illness category that encompasses major mood and psychotic disorders may be appropriate in research investigations.10
Materials and Methods
Study Sample
The PSYCH+MOOD group had International Classification of Diseases 10th Revision (ICD-10) F2 or F3 disorder diagnoses. The ANX group had ICD-10 F4 disorder diagnoses.
Participants were either hospitalized or treated at the outpatient office of the Department of Psychiatry, University Hospital at Hradec Kralove or Olomouc, Czech Republic. Their mental condition was stable (ie, without medication changes or clinical state deterioration within the past two weeks). The inclusion criteria were as follows: F2, F3 or F4 ICD-10 diagnosis; no concomitant F0, F1, F5 or F7 ICD-10 diagnosis; age 18 −65 years; male or female; and willingness to participate in research. The main rationale for the selection of F2, F3 and F4 diagnostic groups is the fact that they are markedly represented in the adult population of psychiatric patients and the difference in the etiological involvement of environmental risk/protective factors in F2+F3 vs F4 may be striking.13 By using the above mentioned inclusion criteria, we strove to minimize the distorting effect of other diagnoses with a different etiology.
Measures
Psychiatric Examination
Each patient´s ICD-10 diagnosis was confirmed by a professor of psychiatry (L. H. or K. L.). The diagnoses were based on clinical interviews; the Composite International Diagnostic Interview (CIDI) or the Mini International Neuropsychiatric Interview (MINI) were not applied. The psychiatric assessment included the family (genetic) history, the personal history (somatic diseases, childhood and adolescence, education, occupational history, marital and sexual history, social and economic history, psychoactive substance abuse, hobbies, premorbid personality, legal problems, military service and plans for the future), the history of the present mental disorder and its treatment, and the assessment of the present psychopathology (status praesens psychicus) as described in the literature.15
Stressful Life Events and Other Environmental Factors Questionnaire
We used the internationally accepted questionnaire from the EUropean Network of National Schizophrenia Networks Studying Gene-Environment Interactions (EU-GEI) study.16 This questionnaire covers the individual´s entire life, including obstetric complications, childhood adversities and serious stressful events in adulthood. Response options are YES/NO.
We enriched the EU-GEI questionnaire with variables that were not present in the original version, but for which literature-based effect sizes are known (ie, for schizophrenia,17 mood disorders18,19 and anxiety disorders20). To allow between-groups comparisons, we asked every participant about the each variables, even if it was not relevant in some cases.
Environmental risk factors for schizophrenia:
- advanced paternal age (>40 years) at conception (odds ratio 1.47),21
- presence of obstetric or perinatal complications (odds ratio 3.66),22
- whether the participant was born in the winter or spring (odds ratio 1.21),23
- upbringing in an urban area (odds ratio 1.19),24
- childhood history of physical abuse, sexual abuse or neglect (odds ratio 2.66),25
- death of a parent when the participant was a child (odds ratio 2.70),26
- history of cannabis abuse (odds ratio 1.37),27 and
- being a member of an ethnic minority (odds ratio 1.40).28
Environmental risk factors for mood disorders:
- serious chronic somatic disorder (odds ratio 1.53),29
- traumatic brain injury (odds ratio 2.00),30
- low level of physical activity (odds ratio 1.12),31
- obesity (odds ratio 1.40),32
- alcohol abuse (odds ratio 2.04),18
- smoking (odds ratio 1.50),33
- presence of any job-related stress (odds ratio 1.77),34
- serious stressful events in adulthood (odds ratio 2.85),19
- migration (odds ratio 2.94),35 and
- living a solitary lifestyle (odds ratio 2.90).36
Environmental risk factor for anxiety disorders:
- low level of physical activity (odds ratio 1.12).20
We also asked each participant about all protective environmental factors for which a literature-based effect size is known for our study populations (ie, mood37,38 and anxiety39 disorders). We did not inquire about environmental protective factors for schizophrenia because there is no convincing evidence of them.40
Environmental protective factors for mood disorders:
- Mediterranean diet (odds ratio 0.84),41
- sufficient physical activity (odds ratio 0.88),38 and
- good social support (odds ratio 0.74).42
Environmental protective factors for anxiety disorders:
Statistics
We used SPSS software, version 23 (IBM Corp., Armonk, NY, USA). We compared the two patient groups on continuous measures using the Mann–Whitney U-test and two-sample Student´s t-test. Categorical measures were compared by chi-squared test or Fisher’s exact probability test. Chi-square post-hoc tests with Bonferroni correction were used to analyze the difference between the PSYCH+MOOD and ANX groups in the marital status in more detail. Kruskal–Wallis test was used to compare the three patient groups (PSYCH vs MOOD vs ANX) on total PERS and polyenviromic protective score. Distribution normality was tested by the Shapiro–Wilk test. We used the Pearson´s correlation coefficient to establish possible intercorrelations between individual environmental risk or protective factors. The Spearman´s correlation coefficient was applied to detect a possible association of the polyenviromic risk/protective score with the duration of illness.
The alpha level required for statistical significance was 0.05 in all cases. The polyenviromic risk/protective score was calculated for each participant, as suggested by Padmanabhan.8
Results
Demographic and Clinical Data
Ninety-four patients were included in the PSYCH+MOOD group and fifty-two subjects were involved in the ANX group. Their demographic and clinical characteristics are presented in Table 1.
 |
Table 1 Demographic and Clinical Characteristics |
Diagnostic stratification for the PSYCH+MOOD group was: single episode of major depression (n = 24), schizophrenia (n = 23), bipolar disorder (n = 22), recurrent major depressive disorder (n = 14), brief psychotic disorder (n = 8) and delusional disorder (n = 3). For the ANX group: generalized anxiety disorder (n = 25), panic disorder (n = 11), agoraphobia (n = 5), somatization disorder (n = 5), neurasthenia (n = 3), post-traumatic stress disorder (n = 1), acute stress reaction (n = 1) and undifferentiated somatoform disorder (n = 1). Psychiatric comorbidity was found in 19 PSYCH+MOOD patients (all of them personality disorders) and in 16 ANX patients (another anxiety disorder n = 9, personality disorders n = 7). The PSYCH+MOOD subjects with an ANX comorbidity and vice versa were not included in our study.
Antipsychotics typically prescribed were olanzapine, risperidone, quetiapine, aripiprazole, clozapine and lurasidone. The most frequent antidepressants were es/citalopram, fluoxetine, sertraline, venlafaxine, mirtazapine, vortioxetine and trazodone. The most frequent anxiolytics were clonazepam, oxazepam, bromazepam, alprazolam, pregabalin and hydroxyzine. Mood stabilizers included lithium, valproate and lamotrigine. If antipsychotics were prescribed to ANX patients, the typical medication was quetiapine 25 −50 mg/day as a sedative.
Risk and Protective Environmental Factors
Among the individual risk factors, we found that compared with the ANX group, PSYCH+MOOD patients less frequently experienced obstetric complications (5.4% in PSYCH+MOOD vs 19.6% in ANX; chi-square = 7.149; p = 0.008; Chi-square test), were more frequently obese (29.8% in PSYCH+MOOD vs 13.7% in ANX; chi-square = 4.658; p = 0.031; Chi-square test) and more frequently experienced job-related stress (56.4% in PSYCH+MOOD vs 36.5% in ANX; chi-square = 5.275; p = 0.022; Chi-square test). There were no significant between-group differences on any other risk factors, or on any of the three protective factors. PERS and polyenviromic protective score did not differ significantly between the groups (PERS: PSYCH+MOOD 0.057±0.03; median 0.054 vs ANX 0.051±0.032; median 0.044, Mann–Whitney U = 2091; p = 0.149, Mann–Whitney U-test, Figure 1; polyenviromic protective score: PSYCH+MOOD −0.045±0.02; median −0.044 vs ANX −0.046±0.014; median −0.044, Mann–Whitney U = 2284; p = 0.466, Mann–Whitney U-test, Figure 2).
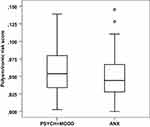 |
Figure 1 Polyenviromic risk score. |
Figure 1: Distribution of data was shown graphically by a box and whisker plot. In a box and whisker plot the ends of the box are the upper and lower quartiles, the median is marked by a horizontal line inside the box; the whiskers are the two lines outside the box that extend to the highest and lowest observations. Outliers and extremes are shown as separately plotted points and stars.
 |
Figure 2 Polyenviromic protective score. |
Figure 2: Distribution of data was shown graphically by a box and whisker plot. In a box and whisker plot the ends of the box are the upper and lower quartiles, the median is marked by a horizontal line inside the box; the whiskers are the two lines outside the box that extend to the highest and lowest observations. Outliers and extremes are shown as separately plotted points and stars.
We detected the following moderately severe positive intercorrelations between environmental risk factors: Death of a parent in childhood and ethnic minority (r = 0.427; p < 0.0001), ethnic minority and traumatic brain injury (r = 0.489; p < 0.0001) in the PSYCH+MOOD group; serious chronic somatic disorder and job-related stress (r = 0.487; p = 0.0003), death of a parent in childhood and abuse in childhood (r = 0.477; p = 0.0004) in the ANX category. Other intercorrelations between environmental risk factors or between environmental protective factors in both study groups were only weak or absent.
PERS was significantly associated with the duration of illness in the ANX group (Spearman´s correlation coefficient 0.287, r = 0.287; p = 0.039), but not in the PSYCH+MOOD subjects (Spearman´s correlation coefficient −0.036, r = −0.036; p = 0.732). Polyenviromic protective score was associated with the duration of illness in neither the ANX participants (Spearman´s correlation coefficient 0.001, r = 0.001; p = 0.996), nor the PSYCH+MOOD patients (Spearman´s correlation coefficient −0.042, r = −0.042; p = 0.690).
When we compared the three patient groups (PSYCH vs MOOD vs ANX) on total PERS and polyenviromic protective score, there were no significant differences (chi-square = 2.120; p = 0.346 for PERS; chi-square = 1.089; p = 0.580 for protective factors; Kruskal–Wallis test; detailed data not shown).
Discussion
We found that compared with the ANX group, PSYCH+MOOD patients were more frequently obese, single, childless, had a longer duration of illness and were more frequently hospitalized in spite of the fact that the ANX participants were generally older. That PSYCH+MOOD patients experience difficult, unsatisfactory lives from the medical, psychological, societal and economic perspectives has been described extensively.16 Our results correspond with this knowledge.
The more frequently experienced job-related stress in the PSYCH+MOOD group compared with the ANX patients may be attributable to cognitive deficit, which is present in psychoses44 as well as in mood disorders.45,46 On the other hand, our finding that obstetric complications were more frequent in the ANX participants compared with the PSYCH+MOOD group is atypical,22 and may be due to our insufficient explanation of this issue to the study participants before the research. The individual risk/protective factors had a different statistical weight (odds ratio), as stated in the Methods section.
PERS and polyenviromic protective score did not differ significantly between the groups.
This nonsignificant PSYCH+MOOD vs ANX difference in overall environmental risk/protective factors herein underlines the need to also assess factors´ exposure timing and unique combinations.10
We were unable to establish the effect size of the polyenviromic risk score because the individual odds ratios as stated in the Methods section come from different studies with different study populations. Generally, we do not doubt that the magnitude of the polyenviromic risk score is biologically/clinically meaningful, simply because the heritability of mental disorders is far from 100% (heritability based on twin studies: schizophrenia 70%, mood disorders 53%, anxiety disorders 30–60%).14,47 In the polyenviromic protective score, the knowledge is still inconclusive because protective factors of mental disorders have only recently been studied, and there is a lack of research data.
The detected moderately severe positive intercorrelations between individual environmental risk factors in the PSYCH+MOOD as well as ANX study subjects may lead to speculations, for example why being a member of an ethnic minority may be associated with the death of a parent in childhood or with experiencing a traumatic brain injury, but these findings should be at least replicated in an independent sample, before any reliable hypothesis is postulated.
Our finding that PERS was significantly associated with the duration of illness in the ANX group but not in the PSYCH+MOOD subjects may be explained by the fact that the longer exposition to adverse life events results in their more intensive influence on the individual´s psyche. This effect is more striking in anxiety disorders, whilst the background of psychoses and mood disorders is rather genetic/biological.
The only previous PERS-based study was performed by Padmanabhan et al.8 They examined whether an aggregate score reflecting exposure to nine environmental risk factors could predict conversion to psychosis in a pilot group of 83 young participants with high familial schizophrenia risk. They found that higher PERS was significantly associated with conversion to psychosis (OR = 1.97; p = 0.009), supporting the notion that an aggregate index of environmental risk may be a helpful predictor in that population. We are the second team to use the “PERS” to study the etiology of mental disorders.
The review by Serafini et al48 suggests that even if bipolar disorder and unipolar depressive disorder both belong to mood disorders, they are partially different from each other in brain morphological abnormalities. Reductions in the volume of basal ganglia and the hippocampus appear more specific for pediatric unipolar depression, whereas reduced corpus callosum volume and increased rates of deep white matter hyperintensities are more specific for pediatric bipolar disorder. With this knowledge in mind, scientists should be aware that some etiopathogenetic differences may be present within the same broad diagnostic category, which might also be true for environmental triggering factors. In addition to this, a part of mental disorders including their causes may be quite undetected and thus not studied. For example, Pompili et al49 state that above 2% of the alleged traffic accidents are suicidal behavior in reality.
Our study is not without limitations. We did not assess intercorrelations among, and time frames for exposure to individual environmental factors as suggested by Uher et al.10 Our cross-sectional design precludes deducing cause and effect.50 Assessing past stressful life events may have been influenced by recall bias, and the significance of these incidents was evaluated only subjectively, without use of any biological marker. Recall bias occurs when participants in a study are systematically more or less likely to recall and relate information on exposure depending on their outcome status, or to recall information regarding their outcome dependent on their exposure.51 Potential diagnostic biomarkers of chronic stress include cortisol, adrenocorticotropic hormone, brain-derived neurotrophic factor, catecholamines, glucose, hemoglobin A1c, triglycerides, cholesterol, prolactin, oxytocin, dehydroepiandrosterone sulfate, C-reactive protein, interleukin-6 and interleukin-8.52 Environmental risk factors like cannabis abuse may have dose-dependent effects that were not considered herein. Current evidence shows that high levels of cannabis use increase the risk of psychotic outcomes and confirms a dose-response relationship between the level of use and the risk for psychosis.53 Our small sample size may have provided insufficient statistical power; thus, replication with larger samples is needed. We were unable to ascertain odds ratios for each environmental risk and protective factor within each relevant diagnosis using the PERS simply because the data have yet to be identified, and we used a single representative odds ratio for each risk/protective factor if the data were available. Nearly all of our participants were hospitalized and thus may not be representative of all patients who meet the same ICD-10 criteria. These results from the Czech Republic, where there is a relatively homogenous ethnic demographics, may not generalize to other countries where international migration is higher. It is typical in the Czech Republic to live in a relatively small city (ie, fewer than 20.000 residents) or villages; thus, we considered being raised in Prague (1.3 million residents) to reflect a “childhood in an urban area”. This may also limit generalization of our results to countries with similar urban stratifications.
No genetic variant and no environmental exposure on its own is a sufficient cause of mental illness. The most likely scenario is that both genetic and environmental factors jointly contribute to the causation of mental illness. This phenomenon has been described as a gene‐environment interaction.10 We did not examine genetic background of the study participants, which is a shortcoming of our research.
The main advantage of our study is the application of a summarizing and complex concept of the assessment of environmental risk/protective factors in the etiology of mental disorders. This is a logical step in research, because the evaluation of individual environmental variables in isolation brought only a limited scientific benefit. In this way, we come after a similar trend in psychiatric genetics, where polygenic risk scores are already calculated.
We also expect that our sample may represent the whole of the Czech Republic well because a) Hradec Kralove is in Bohemia and Olomouc is in Moravia (two major sections of the country) and b) only 5.5% of the inhabitants are foreigners,54 none of whom were included in this sample.
Conclusions
Our results may be helpful toward prevention and personalized treatment of mental disorders. Some environmental risk factors are modifiable, including childhood abuse, smoking and illicit drug abuse, thus physicians should be especially aware of these. Further, environmental protective factors like a healthy diet can also be more intensively encouraged and supported. Further research should focus on the scientific validity of the polyenviromic risk/protective score construct, within large, diverse psychiatric cohorts, ideally using a prospective design. The scientific take-home message of our work is that researchers have started to consider environmental factors in the etiology of mental disorders in their complexity, as polyenviromic risk/protective scores, similarly to polygenic risk scores which have already been applied before.
Abbreviations
ANX, anxiety disorder; BMI, body mass index; CIDI, Composite International Diagnostic Interview; EU-GEI, EUropean Network of National Schizophrenia Networks Studying Gene-Environment Interactions; ICD-10, International Classification of Diseases 10th Revision; MINI, Mini International Neuropsychiatric Interview; MOOD, mood disorder; OR, odds ratio; PERS, polyenviromic risk score; PSYCH, psychosis.
Data Sharing Statement
The anonymized data that support the findings of this study are available upon reasonable request from the corresponding author (L.H.). The data are not publicly available because they contain information that could compromise the privacy of research participants.
Ethical Statement
The authors state that all procedures in this study complied with the World Medical Association Declaration of Helsinki. All procedures involving patients were approved by the Ethics Committee of University Hospital in Hradec Kralove (approval number 201903) and the Ethics Committee of University Hospital in Olomouc (approval number 25/19). Written informed consent was obtained from all participants.
Acknowledgments
The authors thank all the study participants for their contributions to this research.
Authors´ Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the MH CZ – DRO (UHHK, grant number 00179906). The sponsor was not involved at any stage, from study design to submission of the paper for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kessler RC, Angermeyer M, Anthony JC., et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168–176.
2. Lesch OM, Dietzel M, Musalek M, Walter H, Zeiler K. The course of alcoholism. Long-term prognosis in different types. Forensic Sci Int. 1988;36(1–2):121–138. doi:10.1016/0379-0738(88)90225-3
3. Vita A, Barlati S. Resovery from schizophrenia. Is it possible? Curr Opin Psychiatry. 2018;31(3):246–255. doi:10.1097/YCO.0000000000000407
4. Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2016;387(10027):1561–1572. doi:10.1016/S0140-6736(15)00241-X
5. Fava GA, Ruini C, Belaise C. The concept of recovery in major depression. Psychol Med. 2007;37(3):307–317. doi:10.1017/S0033291706008981
6. Soomro GM. Obsessive compulsive disorder. BMJ Clin Evid. 2012;2012:1004.
7. Zwicker A, Denovan-Wright EM, Uher R. Gene-environment interplay in the etiology of psychosis. Psychol Med. 2018;48(12):1925–1936. doi:10.1017/S003329171700383X
8. Padmanabhan JL, Shah JL, Tandon N, Keshavan MS. The “polyenviromic risk score”: aggregating environmental risk factors predicts conversion to psychosis in familial high-risk subjects. Schizophr Res. 2017;181:17–22. doi:10.1016/j.schres.2016.10.014
9. International Schizophrenia Consortium. Common polygenic variation contributes to risk of schizophrenia that overlaps with bipolar disorder. Nature. 2009;460(7256):748–752. doi:10.1038/nature08185
10. Uher R, Zwicker A. Etiology in psychiatry: embracing the reality of poly-gene-environmental causation of mental illness. World Psychiatry. 2017;16(2):121–129. doi:10.1002/wps.20436
11. Davies C, Segre G, Estrade A, et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(5):399–410. doi:10.1016/S2215-0366(20)30057-2
12. Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381(9875):1371–1379. doi:10.1016/S0140-6736(12)62129-1
13. Hosak L, Malekirad M, Latalova K. The Etiology of Mental Disorders. Concise, Clear and Synoptical.
14. Purves KL, Coleman JRI, Meier SM, et al. A major role for common genetic variation in anxiety disorders. Mol Psychiatry. 2020;25(12):3292–3303. doi:10.1038/s41380-019-0559-1
15. Hosak L, Hrdlicka M, et al. Psychiatry and Pedopsychiatry.
16. EUropean Network of National Networks studying Gene-Environment Interactions in Schizophrenia (EU-GEI). Identifying Gene-Environment Interactions in Schizophrenia: contemporary Challenges for Integrated, Large-scale Investigations. Schizophr Bull. 2014;40(4):729–736. doi:10.1093/schbul/sbu069
17. Jongsma HE, Turner C, Kirkbride JB, Jones PB. International incidence of psychotic disorders, 2002-17: a systematic review and meta-analysis. Lancet Publ Health. 2019;4(5):e229–244. doi:10.1016/S2468-2667(19)30056-8
18. Köhler CA, Evangelou E, Stubbs B, et al. Mapping risk factors for depression across the lifespan: an umbrella review of evidence from meta-analyses and Mendelian randomization studies. J Psychiatr Res. 2018;103:189–207. doi:10.1016/j.jpsychires.2018.05.020
19. Marangoni C, Hernandez M, Faedda GL. The role of environmental exposures as risk factors for bipolar disorder: a systematic review of longitudinal studies. J Affect Disord. 2016;193:165–174. doi:10.1016/j.jad.2015.12.055
20. Stubbs B, Koyanagi A, Hallgren M, et al. Physical activity and anxiety: a perspective from the World Health Survey. J Affect Disord. 2017;208:545–552. doi:10.1016/j.jad.2016.10.028
21. Byrne M, Agerbo E, Ewald H, Eaton WW, Mortensen PB. Parental age and risk of schizophrenia: a case-control study. Arch Gen Psychiatry. 2003;60(7):673–678. doi:10.1001/archpsyc.60.7.673
22. Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363(9426):2063–2072. doi:10.1016/S0140-6736(04)16458-1
23. Escott-Price V, Smith DJ, Kendall K, et al. Polygenic risk for schizophrenia and season of birth within the UK Biobank cohort. Psychol Med. 2019;49(15):2499–2504. doi:10.1017/S0033291718000454
24. van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468(7321):203–212. doi:10.1038/nature09563
25. Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2013;43(2):225–238. doi:10.1017/S0033291712000785
26. Misra S, Gelaye B, Koenen KC, et al. Early Parental Death and Risk of Psychosis in Offspring: a Six-Country Case-Control Study. J Clin Med. 2019;8(7):1081. doi:10.3390/jcm8071081
27. Vaucher J, Keating BJ, Lasserre AM, et al. Cannabis use and risk of schizophrenia: a Mendelian randomization study. Mol Psychiatry. 2018;23(5):1287–1292. doi:10.1038/mp.2016.252
28. Veling W, Hoek HW, Wiersma D, Mackenbach JP. Ethnic identity and the risk of schizophrenia in ethnic minorities: a case-control study. Schizophr Bull. 2010;36(6):1149–1156. doi:10.1093/schbul/sbp032
29. Chang-Quan H, Xue-Mei Z, Bi-Rong D, Zhen-Chan L, Ji-Rong Y, Qing-Xiu L. Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing. 2010;39(1):23–30. doi:10.1093/ageing/afp187
30. Perry DC, Sturm VE, Peterson MJ, et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: a meta-analysis. J Neurosurg. 2016;124(2):511–526. doi:10.3171/2015.2.JNS14503
31. Vancampfort D, Firth J, Schuch FB, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16(3):308–315. doi:10.1002/wps.20458
32. Zhao Z, Okusaga OO, Quevedo J, Soares JC, Teixeira AL. The potential association between obesity and bipolar disorder: a meta-analysis. J Affect Disord. 2016;202:120–123. doi:10.1016/j.jad.2016.05.059
33. Luger TM, Suls J, Vander Weg MW. How robust is the association between smoking and depression in adults? A meta-analysis using linear mixed-effects models. Addict Behav. 2014;39(10):1418–1429. doi:10.1016/j.addbeh.2014.05.011
34. Madsen IEH, Nybert ST, Magnusson Hanson LL, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med. 2017;47(8):1342–1356. doi:10.1017/S003329171600355X
35. Swinnen SG, Selten JP. Mood disorders and migration: meta-analysis. Br J Psychiatry. 2007;190:6–10. doi:10.1192/bjp.bp.105.020800
36. Chatterjee A, Banerjee S, Stein C, Kim MH, DeFerio J, Pathak J. Risk Factors for Depression Among Civilians After the 9/11 World Trade Center Terrorist Attacks: a Systematic Review and Meta-Analysis. PLoS Curr. 2018;10. doi:10.1371/currents.dis.6a00b40c8ace0a6a0017361d7577c50a
37. Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2014;99(1):181–197. doi:10.3945/ajcn.113.069880
38. Schuch FB, Vancampfort D, Firth J, et al. Physical Activity and Incident Depression: a Meta-Analysis of Prospective Cohort Studies. Am J Psychiatry. 2018;175(7):631–648. doi:10.1176/appi.ajp.2018.17111194
39. Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int J Obes. 2010;34(3):407–419. doi:10.1038/ijo.2009.252
40. Radua J, Ramella-Cravaro V, Ioannidis JP, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. 2018;17(1):49–66. doi:10.1002/wps.20490
41. Rahe C, Unrath M, Berger K. Dietary patterns and the risk of depression in adults: a systematic review of observational studies. Eur J Nutr. 2014;53(4):997–1013. doi:10.1007/s00394-014-0652-9
42. Gariepy G, Honkaniemi H, Quesnel-Vallee A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. 2016;209(4):284–293. doi:10.1192/bjp.bp.115.169094
43. Tang F, Wang G, Lian Y. Association between anxiety and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Psychoneuroendocrinology. 2017;77:112–121. doi:10.1016/j.psyneuen.2016.11.025
44. Weinberger DR, Harrison PJ. Schizophrenia.
45. Perini G, Ramusino MC, Sinforiani E, et al. Cognitive impairment in depression: recent advances a novel treatments. Neuropsychiatr Dis Treat. 2019;15:1249–1258. doi:10.2147/NDT.S199746
46. Sanches M, Bauer IE, Galvez JF, et al. The Management of Cognitive Impairment in Bipolar Disorder: current Status and Perspectives. Am J Ther. 2015;22(6):477–486. doi:10.1097/MJT.0000000000000120
47. Nurnberger JI, Berrettini W. Psychiatric Genetics.
48. Serafini G, Pompili M, Borgwardt S, et al. Brain changes in early-onset bipolar and unipolar depressive disorders: a systematic review in children and adolescents. Eur Child Adolesc Psychiatry. 2014;23(11):1023–1041. doi:10.1007/s00787-014-0614-z
49. Pompili M, Serafini G, Innamorati M, et al. Car accidents as a method of suicide: a comprehensive overview. Forensic Sci Int. 2012;223(1–3):1–9. doi:10.1016/j.forsciint.2012.04.012
50. Laake P, Benestad HB, Olsen BR. Research in Medical and Biological Sciences.
51. Wright P, Stern J, Phelan M. Core Psychiatry.
52. Noushad S, Ahmed S, Ansari B, et al. Physiological biomarkers of chronic stress: a systematic review. Int J Health Sci. 2021;15(5):46–59.
53. Marconi A, Di Forti M, Lewis CM, et al. Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophr Bull. 2016;42(5):1262–1269. doi:10.1093/schbul/sbw003
54. Prague: directorate of Foreign Police Service, Czech Republic; 2020. Available from: https://www.czso.cz/documents/10180/125507871/290027200101.pdf/72ac4e7b-0b22-4042-a242-05db5f009ae9?version=1.3.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
