Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 14
Environmental Enteropathy and Anaemia Status Among Under-Five Children, in Slum Areas of Jimma Town, Ethiopia
Authors Regassa R , Duguma M , Belachew T, Tamiru D
Received 9 September 2022
Accepted for publication 31 January 2023
Published 10 February 2023 Volume 2023:14 Pages 33—43
DOI https://doi.org/10.2147/PHMT.S387747
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Rediet Regassa,1 Markos Duguma,2 Tefera Belachew,1 Dessalegn Tamiru1
1Nutrition and Dietetics Department, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 2Jimma University Laboratory of Drug Quality (JuLaDQ) and School of Pharmacy, Jimma, Ethiopia
Correspondence: Rediet Regassa, Email [email protected]
Background: The most important anemia next to iron deficiency is anemia of inflammation. Micronutrient deficits, such as those in zinc and iron, can be caused by intestinal permeability and gut inflammation brought on by environmental enteric dysfunction. This study was aimed to evaluate the prevalence and association of anemia with Environmental Enteropathy.
Methods: Data on water sanitation and hygiene indicators and sociodemographic characteristics were collected using structured questionnaire. The lactulose to mannitol ratio (L:M) was calculated from the concentration of both sugars in the urine. Level of Hemoglobin was detected by using Hemocue− 301 digital photometer. Blood and urine sample was collected from three hundred children aged 12– 59 months to determine the status of Anaemia and Environmental Enteropathy respectively.
Results: Data were analyzed by using Descriptive statistics, cross-tabulation, and logistic regression model to indicate prevalence and association of anemia with environmental Enteropathy in children less than five years old. The prevalence of anemia in children with environmental enteropathy was 63.8% (95% CI: 57.6, 71.7), and there was a significant association (p = 0.0001, AOR 3.502, 95% CI: 1.929– 6.371) between anemia and environmental enteropathy. In a multivariate analysis, children aged 1– 3 years with caretakers who had no or only primary education and with monthly income of less than 3000 ETB were more likely to develop anemia.
Conclusion: The result of this study indicated that two-thirds of children less than five with environmental enteropathy had developed anemia, and there is a significant association between environmental enteropathy and anemia. Even though there are other causes of anemia, based on the findings of this study, more research is needed to identify factors associated with environmental enteropathy to mitigate anemia due to intestinal permeability or malabsorption and its impact in children under the age of five.
Keywords: environmental enteropathy, environmental enteric dysfunction, inflammation, lactulose mannitol test, Anaemia, WASH, Malnutrition
Introduction
Low hemoglobin (Hgb) levels in the blood are considered to be anemia.1 A child’s hemoglobin (Hgb) level needs to be less than 11.0 g/dl in order to be diagnosed as anemic.2 Low consumption and poor absorption of foods high in iron are the most common causes of anemia in children under the age of five.3 Anemia is a public health problem with an impact on the development of both developed and developing countries, as well as human health.4 Anemia affects between 47.4% and 67.6% of children under five worldwide and in developing countries like Ethiopia, respectively.1 In 2015, the World Health Organization (WHO) predicts that 800 million children will experience anemia globally. Similar to this, anemia is thought to afflict 273.2 million individuals worldwide, or around 47.4% of children less than the age of five, with developing countries estimated to have roughly 67.6% of those affected.1
Anemia affects 1.62 billion individuals worldwide. It is a serious public health problem in sub-Saharan Africa, where 83.5 million children and 67% of the population are affected.5 The most common anemia in the world is iron deficiency. It affects 10.7% of Bangladeshi children under the age of five, with slum areas having a prevalence of 27.2%.6 The most important micronutrient deficiency problem is anemia.7 Over 50% of anemia is caused by an iron shortage. Anemia can also occur due to inflammation, which is the most common next to iron deficiency.8 Environmental enteropathy causes micronutrient deficiencies in children due to gut inflammation and permeability.6 Chronic diseases associated with infection and inflammation cause mild to severe anemia.8 Inflammation decreases iron absorption, reduces the flow of iron by diverting its path to the reticuloendothelial storage site, disturbs iron homeostasis, and at last reduces iron for erythroid progenitor cells and iron-constrained erythropoiesis by lowering plasma retinol, which is important for erythropoiesis. This also has an effect on other target tissues that are crucial for a child’s growth.8 They hinder erythroblasts from absorbing iron, which causes anemia.8
Alterations in the metabolism and absorption of micronutrients like iron and zinc are also brought on by environmental enteric dysfunction. For the body’s various enzyme systems involved in growth and development, trace metals such as iron and zinc are essential.6 Environmental enteropathy is thought to be brought on by fecal-oral exposure to enteric pathogens.9 The morphological alterations brought on by fecal ingestion of microbes harm the intestinal epithelium, increase permeability, and allow germs to penetrate the lamina propria. By invading the colon, inflammatory cells produce both local and systemic inflammation, diverting resources meant for the growth and development of children.10 Stunting was associated with young children putting dirt in their mouths, living in poor sanitation areas, and caregivers with poor hygiene and elevated fecal markers of environmental enteropathy.11 Similarly, fecal markers of environmental enteric dysfunction were found to be associated with reduced ferritin levels in young children living in the slum regions of Bangladesh.6 According to other research, the main risk factors for pediatric environmental enteropathy were socioeconomic status, feeding practices, geophagy, animal and pathogen exposure, sickness, nutritional status, and caregiver hygiene.12 A study reports that iron therapies for anemic children, with or without nutrition intervention, did not decrease the burden of pediatric anemia.8 In children with environmental enteropathy, intestinal inflammation and decreased absorptive activity cause micro- and macronutrient malabsorption. Because nutrient leakage or malabsorption is an issue in these children, nutritional intervention would not be sufficient to correct a micro- or macronutrient deficiency caused by intestinal inflammation or environmental enteropathy.
Despite numerous studies on various factors associated with anemia, the disease’s prevalence remains high. This indicated that there is a research gap in identifying other factors for under-five anemia. There was no research on the prevalence of environmental enteropathy and its association with anemia in the study area or the country as a whole. In order to address the issue of anemia caused by environmental enteropathy, this study set out to indicate the association between environmental enteropathy and the anemia status of children under the age of five.
Methods and Materials
Study Design and Area
A community-based comparative cross-sectional study was conducted on children aged 12–59 months who are at risk of developing environmental enteropathy. The study was conducted in the slum areas of Jimma Town. Jimma town is among the top ten priority towns in the Oromia region. It is located in southern Ethiopia, 354 kilometers from the capital city of Addis Abeba. In Jimma town, there are 13 urban kebeles and 4 rural kebeles. In 2021/2022, the population of the city of Jimma, Ethiopia, was 207,573. The temperature varies from 48°F to 83°F. The town is bounded by Kersa woreda in the east, Manna woreda in the west, Mana and Seka woreda in the north, and Seka woreda in the south.
Population
Source population
All under five children living in slum areas of Jimma town.
Study Population
Children aged 12–59 months who were randomly selected and eligible for the lactulose mannitol test.
Sample Size Determination
A total of 300 children were calculated using the single population proportion formula, with the assumption of an estimated prevalence of (p) EE 50%, a 5% margin of error (d), and a 95% confidence level. The lactulose-mannitol test was performed to identify children with intestinal permeability or environmental enteropathy. Based on this, 58 children were found to have EE. For this study, those who developed EE were taken as cases, and the remaining 242 (who did not develop EE) were taken as controls to compare their anemia status.
Inclusion and Exclusion Criteria
Inclusion Criteria
All children age 12–59 months who were randomly selected from households with under-five children were included for the study.
Exclusion Criteria
Children who were very sick, who were on medication, and who had gastrointestinal symptoms for 2 weeks before administration of the lactulose/mannitol solution were excluded.
Data Collection Methods and Procedures
Health extension workers and lab technicians, who were able to communicate in Oromifa, were involved in data collection. Training was provided for data collectors and supervisors.
A day before administration of the lactulose mannitol solution Data collectors went to the homes of the children, gave general information about the test, took consent from caretakers, gave instructions on preparation for the test (about overnight fasting and voiding their first urine), and collected information on socio-economic and demographic characteristics of the caregivers, child characteristics, health status, frequency of diarrhea, hand washing practice, food preparation and storage practice, water quality, housing conditions, sanitation during feeding and food preparation, feco-oral behavior, and morbidity status of children, by using structured questionnaires.
Urine sample was collected after administration of lactulose and mannitol solutions to determine intestinal permeability, and finger-prick blood was taken to determine the level of Hgb. During data collection, data collectors observed the hand washing facility, toilet area, and water storage practice using an observation checklist.
Urine Sample Collection
A total of 300 kids (140 boys and 160 girls) between the ages of 12 and 59 months (median age, 3 years) who were at risk for EE and had no severe medical history or gastrointestinal symptoms for two weeks prior to receiving the lactulose-mannitol solution participated in the test. The test sugar solution, which contained 250 mg/mL of lactulose and 50 mg/mL of mannitol, was administered to the individuals at a dose of 2 mL/kg up to a maximum of 20 mL after an overnight fast. A liberal water intake was allowed to stimulate urine flow after 30 minutes. Food consumption was permitted after the first three hours. Before consuming the test sugar solution, the kids were instructed to empty their bladders. A urine collection bag (McKesson Medical-Surgical lnc. MFR #4822, Richmond, VA) was then put in and changed as necessary for the next five hours.13 After urinating, the amount of urine was measured; and one to two drops of chlorhexidine (20 mg/mL) were added. To prevent microbial growth, samples were divided into smaller portions and kept on ice. Before testing, urine aliquots were kept at −80°C.10
Blood Specimen Collection
After consent was obtained from their parents, a drop of blood was taken from a finger prick after cleansing with antiseptic. The hemoglobin analysis was carried out using a calibrated HemoCue 301 digital photometer. Based on the UNICEF/WHO guideline, Hgb values were adjusted for altitude. Hgb cutoff values for children aged 6 to 59 months were less than 11 g/dL; for anemia, values greater than 11 g/dl were considered normal.2
Laboratory Procedure
Sample Preparation
0.5 gm. of washed cation exchange resin was added to 2 mL of the thawed urine specimen, vortexed for 10 seconds, and centrifuged for 10 minutes at 3000 rpm. The supernatant layer was withdrawn and filtered through 0.2µL to inject into the HPLC system for analysis.13
HPLC System and Chromatographic Conditions
The samples were analyzed using an Agilent 1260 Infinity Series HPLC system (Model SP 8810; Spectra Physics, San Jose, CsA) along with a carbohydrate column (4.6 × 150 mm, 5µm) Zorbax, USA. The mobile phase was a mixture of acetonitrile/HPLC grade water (70/30%v/v). HPLC analysis was conducted at the column temperature, injection volume, and flow rate at ambient temperature, 10.0 µL and 1.0 mL/min, respectively. Calibration curves were prepared by analyzing appropriate concentrations of each compound in distilled water and plotting the peak-height obtained at 1.0 X l0 refractive index unit (full-scale) sensitivity of the detector. Urinary concentrations of sugar probes were calculated from the calibration curves by peak-area analysis (Figures 1 and 2).
Variables of the Study
Dependent Variable
The dependent variable in this study was under-five anemia.
Independent Variables
Intestinal Permeability, Leakage, /Environmental Enteropathy in Children
Socio-Economic and Demographic Variables
Head of HHs, marital status, child age, child sex, age of caregivers, family size, monthly household income, Mother’s occupation, Mother’s level of education, ownership of livestock, and farm land.
Child care practices; include feeding, hygiene, health care seeking, immunization, and morbidity status.
Environmental factors: hygiene practice, sanitation practice and quality of water.
Data Analysis
Data were entered and cleaned in Epi Data version 3.1, then transferred to SPSS version 26 for analysis. Urine analysis was performed by HPLC. A dual sugar concentration in the urine was used to calculate the lactulose-to-mannitol ratio. Hemoglobin analysis was performed using hem cue 301 digital photometer. A data summary was performed using descriptive statistics. For continuous variables, the mean and standard deviation (SD) were used. A bivariate and multivariable logistic regression model was used to estimate crude and adjusted odds ratios with 95% confidence intervals. Variables with a p-value less than 0.05 were considered statistically significant.
Data were entered and cleaned in Epi Data version 3.1, then transferred to SPSS version 26 for analysis. Urine analysis was performed by HPLC. A dual sugar concentration in the urine was used to calculate the lactulose-to-mannitol ratio. Hemoglobin analysis was performed using hem cue 301 digital photometer. A data summary was performed using descriptive statistics. For continuous variables, the mean and standard deviation (SD) were used. A bivariate and multivariable logistic regression model was used to estimate crude and adjusted odds ratios with 95% confidence intervals. Variables with a p-value less than 0.05 were considered statistically significant.
Ethical Statement
Approval of the study protocol was obtained from the Ethical Review Board of the University of Jimma, the College of Medicine and Health Sciences, the Institute of Public Health, and the Ethics Committee of the Oromia Regional Health Bureau. Before the study began, official permission was secured from each study district’s administrative as well as health offices. The purpose and importance of the study were explained to the participants. Written informed consent from a parent or guardian was obtained in accordance with the Declaration of Helsinki. The confidentiality of study participants was kept, and identification of study participants by name was avoided. All participants who were diagnosed with environmental enteropathy and anemia were linked to a nearby health facility for follow-up and management.
Operational Definitions
Environmental Enteropathy
Based on the meta analysis in 2018 cut-off point for “EE/EED” have found to be lactulose to mannitol ratio ≤0.15 and >0.15 for without and with EE, respectively.10
Anaemia; Hemoglobin concentration below 11.0 g/dl was considered anemic, whereas, hemoglobin concentrations of 11.0 g/dl and above were considered normal.2
Monthly Income
It was classified as low income (<3000 ETB), medium income (3000–7500 ETB), and high income (>7500 ETB) based on Ethiopian civil service proclamation.5
Results
Lactulose: Mannitol Test
This study was aimed at determining the prevalence and association of anemia with environmental enteropathy. Even though the best diagnosis for EED was a small intestinal biopsy, the lactulose-mannitol test was the most non-invasive proxy marker.
During data collection, overnight fasting and 5-hour urine collection after administration of a lactulose-mannitol solution posed significant challenges. Mannitol and lactulose recoveries indicate absorption and permeability of the intestine. The lactulose to mannitol ratio was directly related to the severity of intestinal abnormalities or environmental enteric dysfunction. The ratio was calculated from the concentration of dual sugars in the urine.
The mean SD % lactulose excreted was found to be 0.6 ± 0.1 and the mean SD % mannitol excreted was found to be 4.5± 1.6. The mean SD of the L:M ratio was found to be 0.27± 0.06. The lactulose to mannitol ratio of >0.15 was taken as children with Environmental Enteropathy. Of the study participants, the lactulose to mannitol ratio of 58 children was >0.15/with EED, while that of 242 with ≤0.15 was taken as without EED (Table 1).
 |
Table 1 Lactulose Mannitol Test to Determine the Magnitude of Environmental Enteropathy (n = 300) |
Socio Economic and Demographic Characteristics of Children with and without Environmental Enteropathy with Their Caregivers
The result for the sociodemographic characteristics indicated that the mean age (±SD) of children with and without environmental enteropathy was 0.2 (±0.6) and 1.1 (± 0.7), respectively. Concerning the cases, 39 (67.2%) fell within the age group of 1–3 and 19 (32.8%) fell within the age group of 4–5 years old. Most of the cases were male 30 (51.7%) and were from the age of care givers 18–35, 49 (84.5%) years old. Majority of children with cases were from family size of >5 and from income of caregivers <3000 Birr, 39 (67.2%) and 203 (83.9%). Thirty three (56.9%) of children with cases were from House wives.
Concerning controls, 147 (60.7%) and 95 (39.3%) were from the age groups of 1–3 and 4–5 years old, respectively. Thirty-two (54.5%) of the controls were female. Most of controls were from the age of caregivers 18–35 and from house wives, 215 (88.8%) and 98 (40.5%), respectively. Majority of controls were from family size of households ≥5 and family income of <3000 Birr, 143 (59.1%) and 203 (81.3%), respectively (Table 2).
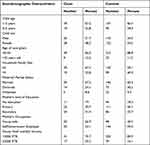 |
Table 2 Socio Demographic Characteristics of Children with and without Environmental Enteropathy n=300 |
Frequency Distribution and Association of Anaemia with Sociodemographic Characteristics of Cases and Controls
The frequency distribution of anemia in cases and controls indicated that cases with an age group of 1–3 developed more anemia 22 (59.5%) than controls 35 (47.3%). Cases from this age group also developed more anemia than their reference 15 (40.5%). Cases of children in the age group of their care (18–35), 30, (81.1%), developed more anemia than cases in the age group >35, 7, (18.9%). Children from family size ≥5 developed more anemia than children from family size <5, 22 (59.5%) and 15 (45.5%), respectively. Children from an income of <3000 Birr also developed more anemia than their references 26 (70.3%), 11 (29.7%), respectively. In multivariate analysis, even though no significant association observed with the sociodemographic characteristics, children with in age group 1–3, from care givers with no education, with primary education and from the average monthly income of care givers <3000 were more likely to develop Anaemia (Table 3).
 |
Table 3 Frequency Distribution and Association of Anaemia with Sociodemographic Characteristics of Cases and Controls n=300 |
Prevalence of Anemia and Its Association with Environmental Enteropathy
The mean (SD) hemoglobin concentration of the study participants, after adjusting for altitude, was 11.5 ± 1.2 g/dl. Overall percentage of anemia was 39.3% (95% CI: 33.7, 44.7). The prevalence of anemia among children with and without environmental enteropathy was 63.8% (95% CI: 57.6, 71.7) and 33.5% (95% CI: 29.3, 40.2), respectively (Figure 3).
 |
Figure 3 Prevalence of Anaemia by Environmental Enteropathy status. |
Discussion
Anemia is one of the public health problems that affect human health, social and economic development, and increased mortality and morbidity.14 It affects all age groups, especially children under the age of five, who have a great demand for iron during rapid growth.15 Even though different studies indicate that anemia is due to a variety of factors, 1,2,7,16,17 the aim of this study was to identify environmental enteropathy as one of the factors causing anemia in under-five children. Based on this, a lactulose mannitol test was performed to identify children with environmental enteropathy. Urine of children with the lactulose to mannitol ratio >0.15 was used to diagnose environmental enteropathy. Anemia status of children was determined by measuring hemoglobin levels. Children with hemoglobin concentration <11gm/dl was taken as anemic, to compare the prevalence and association of anemia with environmental enteropathy. Anemia due to intestinal inflammation is the second most prevalent anemia in developing countries.1 Environmental enteropathy (EE) is an inflammatory condition of the gut characterized pathologically by villous blunting, which is likely to result in a reduction of the surface area of the mature absorptive intestinal epithelial cells. Many studies have shown that chronic intestinal inflammation caused by environmental enteropathy causes permeability and micro- and macronutrient malabsorption. 1,6,8–12,17 Deficits in the absorption of essential nutrients arising from this loss of surface area could result in metabolic pathway derangement or simply a mismatch between the availability and consumption of micronutrients and macronutrients. Reduction in the absorption of iron (one of the micronutrients) leads to anemia.17
The overall prevalence of anemia in children with and without environmental enteropathy was 39.3% (95% CI: 33.7–44.7), according to the findings of this study.
Prevalence of anemia above 40%, 20% and 5% was classified as severe, moderate or mild, respectively, based on world health classification of anemia. Accordingly, the level of anemia in this study was classified as “severe” as it was near the classification of severe anemia. The prevalence of anemia in cases (children with environmental enteropathy) was 63.8% (95% CI: 57.6, 71.7) and higher than in controls (33.5%) (95% CI: 29.3, 40.2). This was higher than the prevalence in slum areas of Bangladesh (27.2%), and it was consistent with the prevalence in Africa and Southeast Asia, which were 67.6% and 65.5%, respectively.7 This was also a little higher than the finding in Ethiopia, which was found to be 56%.3 There was also a significant association (p < 0.0001, AOR 3.502, 95% CI: 1.929–6.371) between anemia and environmental enteropathy. This was consistent with the study done on links with water sanitation, hygiene, stunting, and anemia.8 A study done in slum areas of Bangladesh also indicated that a high fecal level of AAT (a fecal marker for EED) was associated with a decreased level of ferritin in children younger than 2 years.6
Concerning the distribution of anemia in cases and controls, the proportion of anemia in cases aged 1–3 was higher than that in controls. They were also more likely to develop anemia. The possible explanation for this was that, in addition to the higher demand for iron at this age group,16 The low level of immunity and high risk of contamination in younger children (less than five years old) leads them to develop environmental enteropathy and, in turn, anemia due to intestinal inflammation.8 The findings of this study also revealed that children in the age group of 1–3 developed more environmental enteropathy. The possible explanation for this is that children in the early age group were more prone to developing environmental enteropathy.18
Children from developing countries were more frequently come into contact with animal and human excrement while crawling outside the door.8 Children with environmental enteropathy and from family size of ≥5 developed more anemia than those without EE. The justification for this might be, in this study, most of the cases from the larger families developed more environmental enteropathy than controls. This is also consistent with the study that found that, as the number of children increased, the quality of care by parents decreased, and as a result, it was expected that children were at risk for contamination.14,19 This is also supported by a study that indicates a significant association between family size, low income, a low level of education, and the carelessness of care givers with anemia in children younger than five.16
The findings of this study also indicated that children from larger families were more likely to develop environmental enteropathy. Children from families with less income have been observed to develop more anemia than their counterparts. Similarly, children with environmental enteropathy/cases and from less income were observed to develop more anemia than children without environmental enteropathy/control. The possible explanation for this is that good income is related to better hygiene, sanitation, and frequent use of health services. 5,14,16,19 This was also consistent with the study, which found that children from poor households were more prone to develop anemia when compared to children from the richest households. This is because, children from families with good economic status can get iron-rich foods such as animal foods and vitamin-rich foods, especially vitamins A and C, which are very important for iron absorption.7 According to the findings of this study, cases from their caregivers’ occupations Housewives and cases from families with less education were more likely to develop anemia than controls. In addition to having less feeding experience, caregivers with no education are less aware of how to prevent exposure to unsafe sanitation and hygiene practices, as well as the consequences of exposing children to poor sanitation, which leads to environmental enteropathy.5,16
Even though it is far practiced in lots of countries, performing the lactulose mannitol test had never been done in Ethiopia as a biomarker for gut leakiness (permeability), which is used in this study. Performing the test to diagnose Environmental Enteric Dysfunction will give an objective indicator-based baseline for further study on EE/EED and problems associated with it.
Conclusion
To exclude other factors, this study did not assess the type of anemia, whether it was due to a deficiency of iron, vitamin B12, or folic acid, or a morphological change of the RBC or hemoparasites, which was also taken as a limitation of the study. Even though there are also other factors associated with anemia, the findings of this study indicated that two-thirds of children with EE developed anemia. There was also a significant association between environmental enteropathy and the anemia status of under-five children. Based on this, additional research is needed to identify factors associated with environmental enteropathy in order to mitigate the problem of anemia due to environmental enteropathy and its consequences.
Data and Materials Availability
Even though the data is for a Ph.D. project with many objectives, it can be accessed from the corresponding author on reasonable request, depending on the private policy of the journal.
Acknowledgments
The authors acknowledge health extension workers in the selected kebeles and the parents of the study participants, to Bio-Chemical Testing Laboratory Directorate Director and staffs in the laboratory of Ethiopian Conformity Assessment Enterprise in which the urine analysis was done.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Zewude BT, Debusho LK. Prevalence rate and associated risk factors of anaemia among under five years children in Ethiopia. Nutrients. 2022;14(13):1–13. doi:10.3390/nu14132693
2. Alemayehu M, Meskele M, Alemayehuid B, Yakob B, Vellakkal S. Prevalence and correlates of anemia among children aged 6–23 months in Wolaita Zone, Southern Ethiopia. PLoS One. 2019;14(3):1–13. doi:10.1371/journal.pone.0206268
3. Belachew A, Tewabe T. Under-five anemia and its associated factors with dietary diversity, food security, stunted, and deworming in Ethiopia: systematic review and meta-analysis. Syst Rev. 2020;9(1):10–12. doi:10.1186/s13643-020-01289-7
4. George CM, Sack RB, Kosek M, et al. Geophagy is associated with environmental enteropathy and stunting in children in rural Bangladesh. Am J Trop Med Hyg. 2015;92(6):1117–1124. doi:10.4269/ajtmh.14-0672
5. Kebede D, Getaneh F, Endalamaw K, Belay T, Fenta A. Prevalence of anemia and its associated factors among under-five age children in Shanan gibe hospital, Southwest Ethiopia. BMC Pediatr. 2021;21(1):1–9. doi:10.1186/s12887-021-03011-5
6. Fahim SM, Das S, Sanin KI, et al. Association of fecal markers of environmental enteric dysfunction with zinc and iron status among children at first two years of life in Bangladesh. Am J Trop Med Hyg. 2018;99(2):489–494. doi:10.4269/ajtmh.17-0985
7. Tesfaye TS, Tessema F, Jarso H. Prevalence of anemia and associated factors among ‘apparently healthy’ urban and rural residents in Ethiopia: a comparative cross-sectional study. J Blood Med. 2020;11:89–96. doi:10.2147/JBM.S239988
8. Ngure FM, Reid BM, Humphrey JH, Mbuya MN, Pelto G, Stoltzfus RJ. Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: making the links. Ann N Y Acad Sci. 2014;1308(1):118–128. doi:10.1111/nyas.12330
9. Korpe PS, Petri WA. Environmental enteropathy: critical implications of a poorly understood condition. Trends Mol Med. 2012;18(6):328–336. doi:10.1016/j.molmed.2012.04.007
10. Harper KM, Mutasa M, Prendergast AJ, Humphrey J, Manges AR. Environmental enteric dysfunction pathways and child stunting: a systematic review. PLoS Negl Trop Dis. 2018;12(1):1–23. doi:10.1371/journal.pntd.0006205
11. George CM, Burrowes V, Perin J, et al. Enteric infections in young children are associated with environmental enteropathy and impaired growth. Trop Med Int Health. 2018;23(1):26–33. doi:10.1111/tmi.13002
12. Vonaesch P, Randremanana R, Gody J-C, et al. Identifying the etiology and pathophysiology underlying stunting and environmental enteropathy: study protocol of the AFRIBIOTA project. BMC Pediatr. 2018;18(1):1–18. doi:10.1186/s12887-018-1189-5
13. Miki K, Butler R, Moore D, Davidson G. Rapid and simultaneous quantification of rhamnose, mannitol, and lactulose in urine by HPLC for estimating intestinal permeability in pediatric practice. Clin Chem. 1996;42(1):71–75. doi:10.1093/clinchem/42.1.71
14. Mugo NS, Agho KE, Zwi AB, Damundu EY, Dibley MJ. Determinants of neonatal, infant and under-five mortality in a war-affected country: analysis of the 2010 Household Health Survey in South Sudan. BMJ Glob Heal. 2018;3(1):1–15. doi:10.1136/bmjgh-2017-000510
15. Sorsa A, Habtamu A, Kaso M. Prevalence and predictors of anemia among children aged 6–23 months in Dodota District, southeast Ethiopia: a community-based cross-sectional study. Pediatr Heal Med Ther. 2021;12:177–187. doi:10.2147/phmt.s293261
16. Parbey PA, Tarkang E, Manu E, et al. Risk factors of anaemia among children under five years in the hohoe municipality, Ghana: a Case Control Study. Anemia. 2019;2019:1–9. doi:10.1155/2019/2139717
17. Kejo D, Petrucka P, Martin H, Kimanya M, Mosha T. Prevalence and predictors of anemia among children under 5 years of age in Arusha District, Tanzania. Pediatr Heal Med Ther. 2018;9:9–15. doi:10.2147/phmt.s148515
18. Prendergast A, Kelly P. Review: enteropathies in the developing world: neglected effects on global health. Am J Trop Med Hyg. 2012;86(5):756–763. doi:10.4269/ajtmh.2012.11-0743
19. Mebrahtom S, Worku A, Gage DJ. The risk of water, sanitation and hygiene on diarrhea-related infant mortality in eastern Ethiopia: a population-based nested case-control. BMC Public Health. 2022;22(1):1–14. doi:10.1186/s12889-022-12735-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.