Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Enhancing Surgical Nursing Student Performance: Comparative Study of Simulation-Based Learning and Problem-Based Learning
Authors Ma L, Yan R, Wang X, Gao X, Fan N, Liu L, Kang H
Received 14 September 2023
Accepted for publication 14 February 2024
Published 7 March 2024 Volume 2024:17 Pages 991—1005
DOI https://doi.org/10.2147/JMDH.S440333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lihe Ma,1 Rui Yan,1 Xiang Wang,2 Xiaohong Gao,1 Na Fan,1 Linmei Liu,3 Haifen Kang3
1Nursing College of Shanxi Medical University, Taiyuan, People’s Republic of China; 2Department of Foreign Language, Shanxi Medical University, Taiyuan, People’s Republic of China; 3Department of General Surgery, First Affiliated Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China
Correspondence: Rui Yan, Nursing College of Shanxi Medical University, No. 56 of Xinjian Road, Yingze District, Taiyuan, Shanxi, 030001, People’s Republic of China, Tel +86 13934168679, Email [email protected]
Background: Surgical nursing is a high-risk, high-pressure, and complex field. Nurses need extensive knowledge, skills, and abilities. Problem-Based Learning (PBL) and Simulation-Based Learning (SBL) are effective student-centered methods. Which method is better for surgical nurse training? More research is needed to determine the best approach for undergraduate surgical nurse education.
Purpose: To compare the impact of PBL and SBL on undergraduate nursing students’ performance and improve learning outcomes in surgical nursing education.
Methods: We used a pretest/post-test design with 318 nursing undergraduates randomly assigned to two groups. Participants completed three progressive scenarios focused on surgical nursing cases. Experts blindly reviewed video recordings using the 70-item Korean Nurses’ Core Competence Scale (KNCCS) to assess performance. The 13-item Satisfaction and Self-confidence in learning Scale (SSS) measured learning confidence and satisfaction. SBL participants also completed the 16-item Educational Practices in Simulation Scale (EPSS) and 20-item Simulation Design Scale (SDS).
Results: The study found significant positive effects on both groups, with noticeable improvements in post-test, retention, and follow-up test results (P < 0.001). The SBL group showed higher competency levels in nurses (P < 0.001). The Cohen’s d and effect size (r) for various skills were as follows: clinical performance (0.84767 and 6.39023), critical thinking (0.31017 and 0.15325), professional attitude (0.85868 and 0.39452), and communication skills (1.55149 and 0.61294). The satisfaction and self-confidence of nurses were higher in the SBL group (4.53± 0.596; 4.47± 0.611) compared to the PBL group (4.32± 0.689; 4.25± 0.632) in all dimensions of SSS (all P < 0.05). The SBL group also scored high in simulation design and EPSS. However, improvements are needed in fidelity, objectives, information, and students’ expectations.
Conclusion: SBL and PBL improve nurses’ core competence, satisfaction, and self-confidence. SBL is superior. This study promotes student-centered education, enhancing surgical nursing professionals’ quality and ensuring future patient safety.
Keywords: baccalaureate nursing, education, problem-based learning, simulation training, surgical nursing
Introduction
Surgical nursing is a field of work characterized by high risk, intense pressure, and complexity. Surgical nurses are required to possess extensive professional knowledge, skills, and comprehensive abilities. Both Problem-Based Learning (PBL) and Simulation-Based Learning (SBL) are student-centered learning methods and focus on cultivating learners’ comprehensive ability. PBL is an inquiry-based approach to learning that promotes students’ engagement and autonomy by presenting authentic real-world problems.1 The advantages of PBL include stimulating students’ intrinsic motivation, nurturing their problem-solving abilities, and fostering collaboration and communication skills. However, there are certain limitations associated with PBL: it often requires more time to resolve a problem, potentially causing delays in course progression. Due to the open-ended nature and complexity of the problems presented, students may develop biased understandings leading to suboptimal solutions. Additionally, students lack the opportunity to actually operate and make mistakes in a near-real situation. With the improvement of patients’ legal awareness, nursing students were not allowed to make mistakes in nursing practice, and even some invasive operations had no hands-on practice opportunities. The importance of patient safety in healthcare education and practice has prompted much progress in the use of SBL across various healthcare fields, such as medicine, nursing, and anesthetics.2 Regarded as a form of pedagogy, simulation provides an unparalleled student-centered educational experience, enabling learners to practice essential skills within simulated clinical scenarios without posing any harm to real patients.3 SBL is an instructional methodology that replicates real-life scenarios through virtual experiments, simulators, and other technological means. Its advantages encompass providing an authentic learning environment conducive to personalized instruction while mitigating experimentation risks and enhancing learning outcomes.4 However, SBL also entails certain drawbacks such as high technical costs and a slight disparity in authenticity when compared with actual working environments. Currently, there is no consensus regarding the optimal learning mode for enhancing the core competence of nursing students. Exploring how to design learning programs and materials tailored to surgical nursing practice education in order to better address students’ learning needs remains a subject requiring further investigation.
The International Nursing Association for Clinical Simulation and Learning (INACSL) released the standards of best practice: simulation in 2011 and has consistently updated it since then.5 Several studies have demonstrated that these standards play a crucial role in shaping education planning, research, and faculty development, ultimately leading to enhanced reliability and consistent clinical presentation.6–10 Consistent clinical presentation means a simulated patient consistently exhibiting uniform clinical manifestations across different scenarios. This implies that regardless of the circumstances, the symptoms, signs, and progression of the disease displayed by the simulated patient remain constant. Such consistency aids learners in understanding and identifying specific diseases or conditions. By ensuring consistent clinical presentations, simulation studies effectively enhance learners’ abilities to observe, analyze, and diagnose while enabling them to develop appropriate treatment strategies. Nonetheless, the effective implementation and assessment of standardized SBL warrant further investigation. Firstly, there is a need for more research to explore the integration of clinical nursing thinking into the design of SBL cases. Secondly, while SBL has been linked to improved academic performance and learning attitudes in students,11,12 the evaluation criteria used in these studies were incomplete. Thirdly, there is a scarcity of literature outlining dynamic and continuous evaluation methods for standardizing simulation programs. As a result, there is a pressing need to enhance the implementation of the international “Standards of Best Practice: Simulation” (BSPS) to optimize educational outcomes.13
In this study, nursing students were enrolled in college after high school. Undergraduate nursing education in China is a four-year program, the first year is a university equivalent program, the last two years are a nursing professional program, and the last year is a clinical internship. Traditional surgical practical courses in our university adopted the Asian version14–18 of PBL. In 2018, we adopted SBL in surgical practical curriculum. A common research practice in the field of simulation teaching involves comparing the effects of baseline and intervention groups. In this study, two intervention groups were used instead of a traditional baseline group for two reasons: 1) to compare the effects of two different interventions on study subjects directly, without the need for a traditional baseline group; and 2) to compare the two intervention methods before and after intervention, with the pre-intervention test serving as the baseline group.
The SBL instructional approach was shaped using the theoretical framework of the National League for Nursing (NLN/JSF)19 and SBPS. Our goal was to foster clinical thinking skills in learners by incorporating the nursing procedure into the design of learning cases. A series of simulated scenarios were created based on the nursing thinking process, aligning them more closely with real-world nursing practice, and encouraging innovative clinical thinking in students. Each learner acted in one of the medical team’s roles to complete the holistic care of simulated patients. Each team completed feedback guided by the facilitator after the training, and then repeated the teamwork nursing process. The difference between SBL and PBL in our study lies in that firstly, learners are in different learning environments, and secondly, SBL learning activities are guided feedback based on hands-on practice. The similarity of two methods was that both were learner-centered educational methods, and both learned in the form of group cooperation.
Through a comparative analysis of PBL and SBL methods, our aim was to identify the most suitable educational mode and enhance the effectiveness of surgical nursing practice in our university. Additionally, we explored conditions of SBPS’ implementation in the undergraduate nursing education in our country.
Methods
Design
Participants
This study mainly compared the effectiveness of PBL and SBL on the pre-, post-, retention, and transfer of nurses’ core competence in the simulated setting. We enrolled 318 third-year nursing undergraduates from a local university who had successfully finished all theoretical courses. The study received ethical approval from the Ethics Review Committee of the Research University (reference number: SYRL2018009). According to a computer-generated randomization list, students were distributed into with two groups. The inclusion criteria comprised third-year undergraduate nursing students who had completed all theoretical courses and provided informed consent. On the other hand, we excluded students who withdrew or dropped out, those pursuing non-nursing professions, and students below the third year of the 4-year curriculum.
Learning Cases
The SBL cases were created using authentic clinical cases combined with nursing procedures, encompassing conditions such as appendicitis, hemorrhagic shock, multiple injuries, acute pancreatitis, perforation of gastroduodenal ulcer, epidural hematoma, and open pneumothorax. Each learning case was composed of three sequential scenarios in surgical nursing. Specifically, the cases selected for learners in this study focused on hemorrhagic shock caused by a ruptured spleen. Hemorrhagic shock is a typical surgical disease, and the thinking methods, learning modes and nursing operations involved are representative in the learning of broader curriculums. The study of cases of hemorrhagic shock enables us to identify the commonality and universality of learning styles, thereby promoting the improvement of learning outcomes. These studies can be generalized to other courses of study.
Participants from both groups engaged in three sessions, all of which centered around the same case. The first session involved receiving new hospitalized patients, conducting nursing assessments and analyzing the collected data. Participants were tasked with identifying nursing diagnoses and prioritizing the primary problem. In the second session, students formulated a nursing plan and implemented appropriate measures when patients experienced changes in their condition or required surgical intervention. The third session focused on postoperative and pre-discharge nursing, where students carried out nursing evaluations and provided health education.
Throughout this series of progressive cases, learners had the opportunity to develop their comprehensive application of surgical nursing knowledge and enhance their multidimensional thinking abilities.20 The capacity for multi-dimensional thinking refers to an individual’s ability to concurrently consider and analyze diverse dimensions or perspectives of information, and effectively integrate them for comprehensive cognition and decision-making. This aptitude empowers individuals to acquire a more comprehensive comprehension of problems, unveil their intrinsic nature and internal connections, and provide holistic and efficacious solutions. Both sets of participants utilized the seventh edition of the national planning textbook “Surgical Nursing” during the surgical nursing practice course, which was specifically designed for third-year undergraduate nursing students. Both groups received an equal number of contact hours with educators, with the entire educational process spanning 40 class hours.
Students in both groups were divided into smaller groups and taught simultaneously by two instructors at different locations. The PBL group engaged in discussions within the PBL classroom, while the SBL group received training in a simulated ward as well as the PBL classroom.
One week before the training commenced, students received learning cases, questions, and learning objectives. They were encouraged to preview the material by consulting relevant resources. The teachers and team members responsible for organizing SBL/PBL had undergone specific professional training and possess a strong awareness of teamwork and communication skills. The training was scheduled to take place one month prior to the commencement of the course, lasting for a duration of 4 weeks. The training program primarily encompasses: (1) cultivating a clear student-centered teaching philosophy in order to achieve agreed-upon curriculum objectives; (2) comprehending the characteristics, learning content, and educational processes associated with each learning style; (3) thorough case preparation and problem formulation; (4) standardizing terminology; (5) mastering effective communication skills. This is part of the calibration process to ensure consistency in the intervention approach. Additionally, they collaborated on developing written, quantifiable learning objectives for the course.
Procedure
Educational Process
The educational process for the PBL group was organized as follows (Figure 1): (a) participants were randomly divided into groups of 5–6 people, (b) educators assisted groups in setting learning objectives and they were presented with real and complex “situational” questions designed by the instructors, (c) students engaged in independent learning to explore the problems, (d) group discussions took place, (e) students tackled the problems by applying new knowledge, (f) classroom presentations were made by students, and (g) the tutor leads the students to reflecting on their learning progress and dynamics in an evaluation phase at the end of each PBL session in the cycle.
 |
Figure 1 Details of the teaching process for Simulation-Based Learning group and Problem-Based Learning group. |
To begin with, instructors formulated authentic and intricate questions that were then presented to the students. These questions required the students to go through a step-by-step process, which involved identifying if a problem existed, precisely stating the problem, determining the necessary information to understand it, finding resources to gather the needed information, generating potential solutions, analyzing these solutions, and ultimately presenting their team’s solutions and results with PPT.
To explore these questions comprehensively, the students worked collaboratively in groups, allowing their knowledge to evolve continuously and be self- constructed. Group discussions became a valuable platform for understanding the different perspectives, actively participating in discussions, and collaboratively utilizing the newly acquired knowledge to address relevant problems.
Subsequently, each group showcased their accomplishments using presentation slides, and the instructor provided feedback on their achievements and performance. Additionally, the instructor guided the students in reflecting on their activities, fostering a deeper understanding of the learning process.
The SBL group followed a specific educational process, which consisted of the following steps: (a) participants were randomly divided into groups of 5–6 people, (b) providing a pre-briefing session, (c) conducting simulation training, (d) facilitating and debriefing the sessions, and (e) evaluating the instructors. The training took place in a surgical room bay at our institution, designed to replicate an authentic medical setting with patient beds, bedside monitors, and medical gases. Additionally, the SBL group had access to a high-fidelity simulation system. SBL technicians were responsible for inputting case information into the patient simulator, running and troubleshooting the cases.
Before the training commenced, participants of the SBL group completed a pre-briefing session, during which they were briefed about the learning objectives (Table 1), training content, and schedule, and they familiarized themselves with the simulation setup and the high-fidelity patient simulator. PBL focused on developing students’ comprehensive abilities and critical thinking skills, and students gained knowledge through problem solving. Different from the former, SBL paid more attention to the transformation of students’ knowledge from theory to practice in real situations. Through practical training, students could acquire comprehensive abilities such as knowledge, skills and teamwork ability.
 |
Table 1 Learning Objectives for Hemorrhagic Shock of the Simulation-Based Learning Group |
Debriefing
The pretest for each group of students was followed by a discussion session facilitated by a single instructor. For the SBL group, video-assisted debriefing occurred after both the post-test and retention test. In this process, students watched videos of their performances and those of other groups. The discussion was structured based on different segments in the video, and the instructor prompted students to reflect on various aspects, such as communication skills, teamwork, skill evaluation, and applying knowledge in clinical practice.
On the other hand, for the PBL group, their instructor provided a feedback sheet to each group and asked open questions to address any existing issues and guide students in their reflection and improvement. The students in the PBL group engaged in traditional oral problem discussions and group presentations, and they received timely feedback from their instructor. Unlike the SBL group, the PBL group did not watch any video, nor did they have access to observe their own or other groups’ performances.
Evaluation
The fundamental skills of the nursing students in the two groups were assessed in four stages: pre-test, post-test, retention test (two weeks later), and follow-up test (one month later). The evaluator was an experienced instructor with more than five years of clinical nursing and surgical educational experience at the affiliated hospital. The performance of the students was evaluated through video replays using KNCCS. The evaluator did not know which group the participants belonged to or how many training sessions they had completed.
Both groups of participants completed assessments of their satisfaction and self-confidence in learning using SSS within one week after the follow-up test.
For the SBL group, problems in the simulation training process were assessed using SDS and EPSS within one week after the follow-up test.
Pre- Post-, Retention, and Follow-Up Test
In the four-stage test, each team had a two-minute preparation period for equipment setup, followed by 15 minutes of practice in caring for a high-fidelity patient simulator. The test design utilized the “spacing effect”, meaning that test sessions were spaced out over time. Both groups of participants underwent a pre-test one week before the course began. They were required to complete the holistic nursing process for cases of hemorrhagic shock caused by splenic rupture. Right after the lesson, they took a post-test based on the same case. To assess retention, a follow-up test with the same case was conducted two weeks after the practice. One month later, in the follow-up test, the two groups completed three simulated scenarios of acute peritonitis caused by upper digestive tract perforation. During the follow-up test, participants received no feedback. The aim of this test was to investigate the core competency of nurses in different surgical cases which assessed by using the Nurses’ Competence Scale.21
Evaluation Tool
The evaluator used the KNCCS to assess the performance of the students, which consisted of 70 items categorized into 5 subscales: human understanding and communication skills (21 items), professional attitudes (13 items), critical thinking and evaluation (14 items), general clinical performance (13 items), and specific clinical performance (9 items). Each subscale adopted a Likert 5-level scale (scores 1 to 5, ranging from “strongly disagree” to “strongly agree”). Potential scores on this scale ranged from 70 to 350, with a higher score indicating that the evaluator believed the student’s core competence was stronger. Cronbach’s alpha coefficient (reliability) was high at 0.97, indicating strong internal consistency. Additionally, the content validity index was determined to be 0.88, demonstrating the relevance and representativeness of the items in measuring the intended construct.
The KNCCS was developed by Lee et al.22 Furthermore, the SSS, SDS, and EPSS were jointly compiled by the American Nursing Alliance and Nordo Corporation, and their synchronization was done by Wang et al.23 The SSS comprises 13 items, which form two subscales focusing on satisfaction and self- confidence. The SDS consists of 20 items, organized into five dimensions: target/information, support, problem-solving, feedback, and simulation. EPSS contains 16 items across 4 dimensions: active learning, cooperation, multiple learning methods, and meeting expectations. All scales were scored on a Likert 5-scale, ranging from “strongly disagree” to “strongly agree” (scores 1 to 5, respectively). The Cronbach’s alpha coefficients for SDS, SSS, and EPSS were 0.89, 0.94, and 0.82, respectively, indicating high internal consistency. Additionally, the content validity index for the scales was 0.88, 0.86, and 0.78, respectively, indicating the measures effectively captured the intended constructs. The last three scales were completed by the participants immediately after the follow-up test, and all responses were collected on the spot, achieving a 100% recovery rate.
Data Collection
All participants were fully briefed about the study’s purpose and provided their informed consent, along with signing non-disclosure agreements. Students were assured that their participation was voluntary and they could withdraw at any time without any impact on their academic performance. Notably, no participants chose to withdraw or refuse to participate in this study. Prior to the pretest, written consent for study involvement and video recordings were obtained. To ensure accurate observation, dual-position cameras were used to film the reactions and activities of the students during the study, strategically installed by a technician to allow clear recording even if participants changed their positions during the operation. The video recordings were securely saved using cloud storage. After completing 40 hours of practical lessons, the performances of the participants in the pretest, posttest, retention, and follow-up tests were evaluated by a blinded clinician in a random order.
The protection of subjects’ personal information was a crucial task in utilizing video evaluation for research purposes. By implementing anonymization, numbering, secure storage, restricted access, compliance measures, informed consent procedures, and data processing protocols, the personal information of the subjects could be safeguarded to the highest possible extent. In order to prevent subject identification, sensitive details such as the subject’s face, voice, and other identifiable information were blurred, obscured or deleted from the video recordings. Each subject was assigned a unique number instead of using their real name or any personally identifiable information, ensuring their anonymity throughout the study. The video data was securely stored with encryption and password protection mechanisms in place to ensure its confidentiality. Access to this data was strictly limited only to authorized personnel within the research team who required it for analysis purposes. Prior to commencing the study, detailed informed consent was provided to all participants outlining how their personal information would be utilized and protected during the research process. Subjects fully comprehended and agreed that their recorded video data would solely be used for research purposes. A comprehensive data processing agreement was signed with all members of the research team which explicitly outlined their responsibilities and obligations when handling video data including protecting personal information privacy rights. These aforementioned measures were implemented in order to uphold participant privacy regarding personal information as well as maintain objectivity in relation to research outcomes.
Data Analysis
GraphPad Prism 7.00 software was utilized to perform statistical analysis on the data. The simulated educational evaluation data exhibited a normal distribution, and the mean ± standard deviation ( ) was employed for statistical representation. To compare the differences in learning satisfaction, self-confidence, and overall scores of surgical nursing between the SBL group and the PBL group, the two independent samples t-test was employed. Additionally, a two-way mixed factorial analysis of variance (ANOVA) was utilized to assess the change trend of KNCCS in both groups throughout the learning process. The intra-group factors consisted of pre-test, post-test, retention, and follow-up tests, while the inter-group factors were SBL and PBL. The statistical significance level for all dependent measures was set at P < 0.05.
) was employed for statistical representation. To compare the differences in learning satisfaction, self-confidence, and overall scores of surgical nursing between the SBL group and the PBL group, the two independent samples t-test was employed. Additionally, a two-way mixed factorial analysis of variance (ANOVA) was utilized to assess the change trend of KNCCS in both groups throughout the learning process. The intra-group factors consisted of pre-test, post-test, retention, and follow-up tests, while the inter-group factors were SBL and PBL. The statistical significance level for all dependent measures was set at P < 0.05.
Results
The demographic characteristics of the groups (as shown in Table 2) were comparable. The overall study sample consisted of 38 males and 280 females, with ages ranging from 21 to 23 years and an average age of 21.53±0.62 years. The two groups had the same number of participants: SBL (n = 159) and PBL (n = 159).
 |
Table 2 Frequencies and Percentages of Categorical Demographic Variables (n=318) |
Evaluation of Nurses’ Core Competence
At baseline, there were no significant differences in Nurses’ Core Competences (KNCCS) (Figure 2) between the SBL group and the PBL group in specific clinical performance (23.71±5.26 vs 23.53±5.34, P > 0.05), general clinical performance (36.26±4.05 vs 36.39±6.42, P > 0.05), critical thinking (36.02±5.73 vs 36.18±6.94, P > 0.05), professional attitude (37.16±4.58 vs 36.32±5.57, P > 0.05), and human understanding and communication skills (70.82±5.38 vs 70.35±5.57, P > 0.05) (Figure 2). This suggests that both groups had similar competency levels before learning. The scores of specific clinical performance (31.26±4.83; 27.18±4.97; 29.84±4.53; P < 0.0001), general clinical performance (48.83±5.91; 45.79±6.14; 47.16±6.23; P < 0.0001), critical thinking (53.21±4.64; 52.19±4.85; 52.96±4.73; P < 0.0001), professional attitude (46.52±5.36; 45.78±5.85; 46.02±5.53; P < 0.0001), human understanding and communication skills (87.35±4.21; 85.19±4.65; 86.71±4.52; P < 0.0001) for the post-test, retention test, and follow-up test in the SBL group were significantly higher than those in the PBL group (27.17±4.82, 25.64±4.96, 25.92±4.6; 40.58±4.65, 38.71±4.26, 39.25±4.43; 40.67±5.36, 39.64±5.89, 39.11±5.47; 39.84±4.21, 39.25±5.63, 38.21±4.57; 81.74±4.36, 80.14±5.42, 80.27±4.73). The Cohen’s d and effect size (r) specific clinical performance, general clinical performance, critical thinking, professional attitude, and human understanding and communication skills are 0.84767 and 6.39023, 0.31017 and 0.15325, 0.85868 and 0.39452; 1.55149 and 0.61294, 3.61029 and 0.87474, 3.87875 and 0.8888; 2.50152 and 0.78105, 2.32168 and 0.75827, 2.61059 and 0.79382; 1.32262 and 0.5516, 1.44213 and 0.58487, 1.5396 and 0.60999; 1.30902 and 0.54764, 1.00006 and 0.44723, 1.39207 and 0.57128 for the post-test, retention test, and follow-up test.
In addition to the above findings, it was observed that after two weeks, the SBL group had slightly lower post-test scores than retention test scores in human comprehension, communication, general clinical presentation, and specific clinical presentation (P = 0.002, P < 0.0001, P < 0.0001). Additionally, the PBL group exhibited lower retention test scores compared to the post-test scores in the general clinical performances dimension (Figure 2C, P = 0.0192). However, no significant interaction between the test and group was found (P > 0.05). The post-test and retention test scores for specific clinical performance, general clinical performance, critical thinking, professional attitude, human understanding, and communication skills significantly increased in both the SBL and PBL groups compared to their pre-test scores (P < 0.0001). Follow-up test scores in each group significantly exceeded their pre-test scores (pre-test vs follow-up test, P < 0.0001).
Assessment of Students’ Satisfaction and Self-Confidence
The evaluation of students’ satisfaction and self-confidence revealed that the SBL group outperformed the PBL group in all aspects of SSS (P < 0.05). Particularly, SBL students achieved the highest average satisfaction scores for instructors (4.53±0.596) and self-confidence in gaining skills and knowledge (4.47±0.611). Compared to the PBL group, the SBL group showed significantly higher scores about the instructor educational methods, acquired skills and knowledge, and curriculum content (P < 0.01) (Table 3). There was little difference two groups in the score of the last entry of the scale: “It is the instructor’s responsibility to tell me what I need to learn of the simulation activity content during class” (P=0.0490).
 |
Table 3 Comparison of Satisfaction and Self-Confidence Between Simulation-Based Learning Group (n=159) and Problem-Based Learning Group of Junior Nursing Students (n=159) |
Effects of Simulation-Based Learning
In SBL, the average score of each of the five SDS and four EPSS dimensions was relatively high (Tables 4 and 5), among which, the scores of “guided reflection or feedback” (4.82±0.31) and “collaboration” (4.53±0.45) were higher and the scores of “fidelity” (4.43±0.41) and “high expectations” (4.47±0.42) were relatively low.
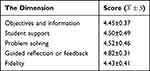 |
Table 4 Evaluation of High Simulation Teaching Design by Simulation-Based Learning Group of Junior Nursing Students (n=159) |
 |
Table 5 Evaluation of the Educational Practices of High Simulation Teaching by Simulation-Based Learning Group of Junior Nursing Students (n=159) |
Discussion
The aim of this study was to compare the disparities between PBL and SBL in terms of student learning outcomes and experiences. Through a comparative analysis, we could gain a deeper understanding of the strengths and weaknesses associated with these two instructional approaches, thereby establishing a robust foundation for educational practice. Initially, we assessed the efficacy of PBL and SBL in fostering nurses’ core competence, students’ satisfaction, self-confidence. The findings indicated that both SBL and PBL had positive impacts on enhancing these aspects; however, SBL outperformed PBL in this regard.
PBL is a methodology in which the starting point is a problem or a problematic situation. The situation enables students to develop a hypothesis and identify learning needs so that they can better understand the problem and meet the established learning objectives. On the other hand, SBL relies on simulation technology24 such as virtual reality and computer-based tools to let students experience, practice, and make decisions in a virtual environment for educational purposes.25 Simulation education involves utilizing medical simulation technology to create scenarios and patients that mimic real clinical situations, serving as substitutes for actual patients in educational settings.26 This approach offers learners a safe environment to acquire clinical knowledge and practice clinical skills without any risk. Nursing students can integrate their theoretical knowledge and operational skills with clinical challenges through simulation training, enhancing their capability to handle surgical clinical issues and fostering agile and accurate clinical thinking. This approach aims to decrease the occurrence of medical accidents and disputes during their future clinical practice.27 Our research findings indicate that the integration of SBL or PBL into surgical nursing practice courses significantly enhances the efficiency and learning experience for both groups of students, compared to pre-training conditions. By incorporating case-based design focused on nursing procedures into the surgical nursing curriculum, participants are provided with opportunities to engage actively in simulation scenarios, thereby improving their practical abilities through analysis and resolution of authentic cases. This ultimately equips them with better preparedness to handle diverse complex situations encountered during clinical work. In small group settings, students collaborate and communicate with each other to collectively solve problems, fostering the development of teamwork and communication skills while concurrently enhancing work efficiency and quality in practical applications. Furthermore, interval training sessions facilitate knowledge internalization among students while also encouraging self-reflection on areas for performance improvement. Importantly, this study reveals a significant increase in learning interest among both groups of students following the training intervention, consequently promoting greater engagement within the learning process itself. Through self-directed and collaborative learning approaches employed herein, students acquire improved comprehension and application capabilities pertaining to surgical nursing practice.
We found that SBL showed better outcomes than PBL in surgical nursing practical education, may be indicating that SBL was more effective for practical learning. However, it cannot be proved that the learning effect of SBL is better than that of PBL in non-practical fields. To enhance student performance, specific practical learning goals, accurate performance assessments, informative feedback and repeated practice are essential. The positive results observed in the SBL group were largely attributed to the standardized SBL approach, which involved a realistic learning environment with advanced simulation systems, performance evaluation, facilitated support to enhance performance, and repeated simulations to sharpen their skills.
Firstly, the SBL group employed a high-fidelity simulation system, effectively showcasing physiological and pathological indicators. This system could replicate real-life scenarios and disease images, enhancing the classroom learning experience by providing students with a more authentic understanding of diseases.28
Secondly, in our study, the SBL group utilized video-assisted feedback to stimulate the students’ interests through visual and auditory senses. By reviewing their performance in the instructional video and receiving intrinsic feedback from the simulator, students could identify issues from an external perspective regarding their behavior and subconscious mannerisms, enabling seamless learning.29 The video playback provided a perspective on their actual performance rather than their perceived performance during simulated encounters, facilitating the formation of accurate mental representations and application in different scenarios. On the other hand, the PBL group lacked video playback sessions and relied on problem-oriented discussions to create a group report, answer questions from the instructor, and then receive instructions. Interestingly, the test curves for understanding and communication ability, basic nursing ability, and specific nursing ability showed a decline in the SBL group, and the retention test curves for basic nursing ability in the PBL group also displayed a downward trend compared to their respective post-test curves. This suggests that it is essential to practice and reinforce newly acquired skills in order to prevent them from being forgotten and to ensure their successful transfer to novel contexts. Students develop their own mental representations through continuous experimentation, failure, and feedback,30 thus, they should be encouraged to enhance their problem-solving competence to improve knowledge acquisition and retention. According to Zapko et al,12,31–35 students in the SBL group demonstrated higher levels of satisfaction and self-confidence compared to those in the traditional teaching method. In our study, we designed the SBL approach based on best practices, while prioritizing involvement of students and considering them as the main focus. Through initiative-probing learning, students were encouraged to convert knowledge into problem-solving competence, foster interest, optimize learning behavior, and improve efficiency. The learners in our study enjoyed the simulation-based learning, and gained confidence in mastering the critical content and surgical skills. The structured debriefing in SBL facilitated positive learning experiences by creating a safe environment for learners to express their feelings and “de-role”, allowing for more open communication and deeper engagement. The feedback sessions also promoted meaningful discussions and knowledge sharing, helping learners address concerns and better comprehend the material. It is worth noting that a few possible suggestions are given for those students unable to participate in the enhanced learning opportunity provided by simulation-based training: ① Provide additional learning materials, teaching materials and guidance to help them bridge gaps in knowledge and skills.②Arrange for remedial or retaking opportunities so that they can participate in simulated learning and have a learning experience similar to other students. ③ Have one-on-one discussions to understand their needs and goals and develop a personalized learning plan to ensure they are able to gain a full learning experience in surgical care. ④Provide visiting internships, practical projects or other hands-on learning opportunities to make up for their deficiencies in simulated learning.
It is worth mentioning that the scores of both groups of students on the final item of the satisfaction scale, “What should be acquired from simulated classroom activities?”, showed relatively lower values (SBL=3.79±1.024, PBL=3.63±1.139, p=0.0490). This indicates that learners perceive classroom learning activities as a domain where they themselves should determine what needs to be learned rather than solely relying on teachers’ guidance. Based on these findings, it can be concluded that future PBL and SBL activities should prioritize fostering learners’ autonomy in determining their learning content while also incorporating more comprehensive and interconnected materials tailored to meet diverse learner needs.
In addition, the findings revealed that the ratings for each aspect in SDS and EPSS were relatively high, suggesting that the SBL approach is logical and effective. The most highly scored dimensions were teamwork and guided reflection or feedback, followed by active learning and problem solving. This indicates that SBL, as a student-centered active learning strategy, encourages self-reflection among students, helps identify areas for improvement, and has the potential to enhance knowledge and skill development in various areas like collaboration, communication, and decision-making. These findings align with previously reported research.36–40
The lower “fidelity” score can be attributed to the following factors: Firstly, while the environment and materials were standardized, students were not involved in the preparation process, leading to potential stress due to unfamiliarity. In the future, students should have the opportunity to select the required items from the storage area on their own, based on the case information provided, and check the name, dosage, model number and expiration date of the items.
Secondly, while advanced simulators can replicate changes in vital signs and show disease progression, they still fall short in fully mimicking real-life cases, including skin appearance and speech. To enhance learning, students can engage in case preparation, script creation, and simulator development to reconstruct clinical scenarios tailored to various cases. This approach fosters a better grasp of learning goals and a more authentic simulation experience.
Thirdly, it was important for relevant staff to run and debug cases program repeatedly, aiming to ensure a smooth and natural educational process that closely resembles real-life cases, thereby enhancing authenticity. The scores for “objectives and information” and “high expectation” were slightly lower compared to other aspects, suggesting that the educational objectives may not fully cater for the learning needs of individual students. This is primarily due to the high number of students and limited class hours. Students expressed a preference for SBL over PBL, and they wished for more learning time, which aligns with the findings of Jensen et al.41
By conducting pre-testing, post-testing, retention, and follow-up evaluations, the study documented the diverse performance and learning requirements of learners. Based on these data, personalized learning goals were formulated to cater for individual learners’ needs, resulting in the achievement of their specific educational objectives. Moreover, exceptional quality instructional videos were created utilizing the flipped classroom approach, enabling students to learn fundamental surgical nursing techniques at their own pace. Consequently, practical classes moved away from instructor-centered demonstrations and allowed more time for SBL. This combination of simulation education and the flipped classroom method optimizes class hours and effectively addresses the challenge of balancing large class capacity with personalized learning.
PBL and SBL offer benefits as they prioritize students as active participants while instructors serve as guides. By presenting problem scenarios, these methods foster critical thinking skills and encourage active and exploratory learning experiences that stimulate student interest in learning while developing their problem-solving abilities.42 However, for surgical nursing which involves acute and serious cases requiring practical skills development; SBL offers a more immersive learning experience. The highly simulated ward environment along with a simulation system enhances student engagement by providing pressure-free practice opportunities. Video-assisted briefing improves knowledge retention and skill acquisition ultimately enhancing overall satisfaction with the learning outcomes.
Compared to SBL, PBL lacks the sense of immersive experience and the opportunity to practice nursing through teamwork.43 Additionally, PBL also lacks video feedback, posing a challenge for students to directly observe their training progress. Conversely, SBL has its drawbacks including higher educational costs, the requirement for more instructors with specific qualifications, and the complexity of designing the learning environment.44 However, in the context of surgical nursing involving acute and critical cases that demand practical skills, SBL provides a more immersive learning experience. The highly simulated ward environment and simulation system enhance student engagement and facilitate pressure-free practice. Video-assisted briefing improves knowledge and skill retention, ultimately enhancing learning outcomes and satisfaction. This may be one reason why the learning effect and experience of PBL in this study were inferior to those of SBL. SBL serves as a supplementary method to traditional teaching rather than a complete replacement. Both PBL and SBL possess their own strengths and weaknesses; when used together, they can augment overall learning effectiveness and quality.45 In practical scenarios, selecting appropriate learning methods and tools should be based on specific objectives, content, and student characteristics to provide personalized high-quality educational experiences. As technology continues to advance, SBL is expected to play an increasingly vital role in education by contributing considerably to talent development and societal progress. However, while promoting and implementing SBL it is crucial to leverage its advantages while being mindful of challenges limitations, consistently striving towards enhancing refining methods order offer students optimal educational services.
The comparative study of PBL and SBL in China holds significant implications for educators, policymakers, and researchers across different countries and settings. Firstly, it can assist them in determining whether to implement these models within their own education systems and how to make necessary adjustments and enhancements. Secondly, it can aid teachers in gaining a better understanding of how to design and implement these models effectively to foster students’ active learning and comprehensive abilities. For students, comprehending the comparison between different educational approaches can facilitate their adaptation to diverse learning environments while enhancing their learning outcomes and capabilities. Moreover, this comparative study offers education researchers an opportunity to delve into the impact of various educational models on students’ learning outcomes, motivation levels, creativity, etc., thereby providing a scientific foundation for education reform initiatives and policy formulation. In conclusion, the comparative study of PBL and SBL in China bears immense significance for individuals across different countries and settings by offering valuable insights that can contribute towards promoting education reform efforts as well as improving overall educational quality.
Limitations
There were some limitations in our research. First, the use of a single site somewhat compromised the representativeness of the findings. Nevertheless, the samples showed relatively high homogeneity, with a large size, and participants were randomized to SBL or PBL, which still rendered the research results noteworthy. Second, due to a constrained number of class hours and a large student population, the current implementation of surgical nursing simulation cases was limited to key diseases, preventing full coverage of all knowledge points. Consequently, further investigation is required to understand the impact of SBL on comprehensive scores of surgical nursing. Third, these findings may not apply to students from other countries or cultures, so we need to have further discussions.
Conclusions
The study revealed that both PBL and SBL had positive effects on improvement in nursing students’ core competence and students’ satisfaction and confidence. The established standards for simulation proved to be suitable for the educational context and the characteristics of Chinese students. SBL showed a greater improvement in surgical practice education compared to PBL. It is important to note that these findings may be influenced by specific contexts, and PBL may still have its advantages in other settings. This study contributes to the promotion of student-centered concepts and methodologies in surgical nursing education, aiming to improve training quality by enhancing the core competency and comprehensive abilities of nursing students, ultimately ensuring patient safety.
Moving forward, future research will focus on two main aspects: firstly, integrating SBL with the flipped classroom approach and utilizing high-quality online resources can address the challenge of accommodating a large number of students in small class settings in China; secondly, combining SBL with PBL can maximize their respective strengths to enhance nursing students’ learning effectiveness. Additionally, implementing a simulation educational database will monitor long-term training outcomes for personalized learning objectives tailored to each individual.
Additional research is necessary to establish whether the observed enhancements during simulated training can be effectively applied to enhance nursing performance and promote better patient outcomes. Continuous independent investigation and exploration are vital in determining the applicability of our findings to students from diverse countries or cultures.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
I confirm that I have read the Editorial Policy pages. This study was conducted with approval from the Ethics Committee of Shanxi Medical University. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This study was supported by grants from the Natural Science Foundation of China (No. 82001872); the Natural Science Foundation for Young Scientists of Shanxi Province, China (No. 201701D221251); the General project of soft science research in Shanxi Province (No. 2017041036-5).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Trullàs JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1):104. PMID: 35177063; PMCID: PMC8851721. doi:10.1186/s12909-022-03154-8
2. Miles DA. Simulation learning and transfer in undergraduate nursing education: a grounded theory study. J Nurs Educ. 2018;57(6):347–353. PMID: 29863735. doi:10.3928/01484834-20180522-05
3. Jeffries PR, Rodgers B, Adamson K. NLN jeffries simulation theory: brief narrative description. Nurs Educ Perspect. 2015;36(5):292–293. doi:10.5480/1536-5026-36.5.292
4. Shorey S, Ng ED. The use of virtual reality simulation among nursing students and registered nurses: a systematic review. Nurse Educ Today. 2021;98:104662. doi:10.1016/j.nedt.2020.104662
5. International Nursing Association of Clinical Simulation and Learning. Standards of best practice: simulation. Clin Simul Nurs. 2011;7(4S):S1–S19.
6. Offenbacher J, Petti A, Xu H. Learning outcomes of high-fidelity versus table-top simulation in undergraduate emergency medicine education: prospective, randomized, crossover-controlled study. West J Emerg Med. 2022;23(1):20–25. PMID: 35060855; PMCID: PMC8782127. doi:10.5811/westjem.2021.12.53926.
7. Lee MN, Nam KD, Kim HY. Effects of simulation with problem-based learning program on metacognition, team efficacy, and learning attitude in nursing students: nursing care with increased intracranial pressure patient. Comput Inform Nurs. 2017;35(3):145–151. doi:10.1097/CIN.0000000000000308
8. Perretta JS, Duval-Arnould J, Poling S, et al. Best practices and theoretical foundations for simulation instruction using rapid-cycle deliberate practice. Simul Healthc. 2020;15(5):356–362. doi:10.1097/SIH.0000000000000433
9. Reed A, Andre A, Ananthakrishnan S, Korczak P. Effectiveness of simulation training on graduate audiology students’ auditory brainstem response testing skills. Am J Audiol. 2021;30(2):394–403. doi:10.1044/2021_AJA-20-00191
10. Sittner BJ, Aebersold ML, Paige JB, et al. INACSL standards of best practice for simulation: past, present, and future. Nurs Educ Perspect. 2015;36(5):294–298. doi:10.5480/15-1670
11. Gardner AK, Scott DJ, Pedowitz RA, et al. Best practices across surgical specialties relating to simulation-based training. Surgery. 2015;158(5):1395–1402. doi:10.1016/j.surg.2015.03.041
12. Zapko KA, Ferranto MLG, Blasiman R, Shelestak D. Evaluating best educational practices, student satisfaction, and self-confidence in simulation: a descriptive study. Nurse Educ Today. 2018;60:28–34. doi:10.1016/j.nedt.2017.09.006
13. Miller C, Deckers C, Jones M, Wells-Beede E, McGee E; INACSL Standards Committee. Healthcare simulation standards of best PracticeTM outcomes and objectives. Clin Simulat Nurs. 2021;58:40–44. doi:10.1016/j.ecns.2021.08.013
14. Hmelo-Silver CE. Problem-based learning: what and how do students learn? Educ Psychol Rev. 2004;16(3):235–266. doi:10.1023/B:EDPR.0000034022.16470.f3
15. Hung W. The 9-step problem design process for problem-based learning: application of the 3C3R model. Educational Research Review. 2009;4(2):118–141. doi:10.1016/j.edurev.2008.12.001
16. Tan OS, Hung DWL. Problem-based learning and creativity: a review of the literature. In: Tan OS, editor. Problem-Based Learning and Creativity. Singapore: Cengage Learning Asia; 2009:1–20.
17. Savery JR. Overview of problem-based learning: definitions and distinctions. Interdiscip J Prob Based Learn. 2006;1(1):9–20. doi:10.7771/1541-5015.1002
18. Hmelo-Silver CE, Barrows HS. Goals and strategies of a problem-based learning facilitator. Interdiscip J Prob Based Learn. 2006;1(1):21–39. doi:10.7771/1541-5015.1004
19. Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educ Perspect. 2005;26(2):96–103.
20. Marquez LP. Multidimensional thinking: economizing thinking and maximizing outcomes. In: Thinking: Bioengineering of Science and Art. Cham: Springer International Publishing; 2022:311–327.
21. J L, Saraswathi KN, Willimas S. A study to assess the effectiveness of concept map teaching method on knowledge regarding self-esteem among nursing students at selected nursing colleges of Mysuru. Int J Adv Nurs Manage. 2020;8(2):154–156. doi:10.5958/2454-2652.2020.00036.0
22. Lee W-H, Kim S, An J. Development and evaluation of Korean Nurses’ Core Competency Scale (KNCCS). Open J Nurs. 2017b;7(5):599–613. doi:10.4236/ojn.2017.75045
23. Wang AL, Fitzpatrick JJ, Petrini MA. Use of simulation among Chinese nursing students. Clin Simulat Nurs. 2013;9(8):e311–e317. doi:10.1016/j.ecns.2012.03.004
24. Yu JH, Chang HJ, Kim SS, et al. Effects of high-fidelity simulation education on medical students’ anxiety and confidence. PLoS One. 2021;16(5):e0251078. PMID: 33983983; PMCID: PMC8118241. doi:10.1371/journal.pone.0251078
25. Alsuwaidi L, Kristensen J, Hk A, Al Heialy S. Use of simulation in teaching haematological aspects to undergraduate medical students improves student’s knowledge related to the taught theoretical underpinnings. BMC Med Educ. 2021;21(1):271. PMID: 33980218; PMCID: PMC8114488. doi:10.1186/s12909-021-02709-5
26. He W, Lu J, Zheng W, et al. A study on the role of intelligent medical simulation systems in teaching first aid competence in anesthesiology. J Healthc Eng. 2022;2022:8163546. Retraction in: J Healthc Eng. 2023 Jul 12;2023:9867315. PMID: 35494522; PMCID: PMC9050259. doi:10.1155/2022/8163546
27. Kononowicz AA, Woodham LA, Edelbring S, et al. Virtual patient simulations in health professions education: systematic review and meta-analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(7):e14676. PMID: 31267981; PMCID: PMC6632099. doi:10.2196/14676
28. Farsoni S, Astolfi L, Bonfe M, Spadaro S, Volta CA. A versatile ultrasound simulation system for education and training in high-fidelity emergency scenarios. IEEE J Transl Eng Health Med. 2017;5:1800109. PMID: 29018630; PMCID: PMC5477762. doi:10.1109/JTEHM.2016.2635635
29. Armenia S, Thangamathesvaran L, Caine AD, King N, Kunac A, Merchant AM. The role of high-fidelity team-based simulation in acute care settings: a systematic review. Surg J. 2018;4(3):e136–e151. PMID: 30109273; PMCID: PMC6089798. doi:10.1055/s-0038-1667315
30. Mullem PV. Peak: secrets from the new science of expertise. Internat Sport Coaching J. 2016;3(3):368–370.
31. Alconero-Camarero AR, Sarabia-Cobo CM, González-Gómez S, Ibáñez-Rementería I, Lavín-Alconero L, Sarabia-Cobo AB. Nursing students’ emotional intelligence, coping styles and learning satisfaction in clinically simulated palliative care scenarios: an observational study. Nurse Educ Today. 2018;61:94–100. doi:10.1016/j.nedt.2017.11.013
32. Franklin AE, Burns P, Lee CS. Psychometric testing on the NLN student satisfaction and self-confidence in Learning, Simulation Design Scale, and Educational Practices Questionnaire using a sample of pre-licensure novice nurses. Nurse Educ Today. 2014;34(10):1298–1304. doi:10.1016/j.nedt.2014.06.011
33. Olaussen C, Heggdal K, Tvedt CR. Elements in scenario-based simulation associated with nursing students’ self-confidence and satisfaction: a cross-sectional study. Nurs Open. 2019;7(1):170–179. doi:10.1002/nop2.375
34. Powers K. Bringing simulation to the classroom using an unfolding video patient scenario: a quasi-experimental study to examine student satisfaction, self-confidence, and perceptions of simulation design. Nurse Educ Today. 2020;86:104324. doi:10.1016/j.nedt.2019.104324
35. Üzen Cura Ş, Kocatepe V, Yıldırım D, Küçükakgün H, Atay S, Ünver V. Examining knowledge, skill, stress, satisfaction, and self-confidence levels of nursing students in three different simulation modalities. Asian Nurs Res. 2020;14(3):158–164. doi:10.1016/j.anr.2020.07.001
36. Alinier G, Hunt B, Gordon R, Harwood C. Effectiveness of intermediate-fidelity simulation training technology in undergraduate nursing education. J Adv Nurs. 2006;54(3):359–369. doi:10.1111/j.1365-2648.2006.03810.x
37. Ansquer R, Oriot D, Ghazali DA. Evaluation of learning effectiveness after a simulation-based training pediatric course for emergency physicians. Pediatr Emerg Care. 2021;37(12):e1186–e1191. doi:10.1097/PEC.0000000000001961
38. Brannan JD, White A, Bezanson JL. Simulator effects on cognitive skills and confidence levels. J Nurs Educ. 2008;47(11):495–500. doi:10.3928/01484834-20081101-01
39. Cassara M, Schertzer K, Falk MJ, et al. Applying educational theory and best practices to solve common challenges of simulation-based procedural training in emergency medicine. AEM Educ Train. 2019;4(Suppl 1):S22–S39. doi:10.1002/aet2.10418
40. Ozkara San E, Dikec G, Ata EE, Sendir M. Evaluation of the use of diverse mental health simulation in nursing students’ learning experience: an International Multisite Study. Nurse Educ. 2021;46(6):E148–E153. doi:10.1097/NNE.0000000000001007
41. Jensen JK, Dyre L, Jørgensen ME, Andreasen LA, Tolsgaard MG. Simulation-based point-of-care ultrasound training: a matter of competency rather than volume. Acta Anaesthesiol Scand. 2018;62(6):811–819. doi:10.1111/aas.13083
42. Mamakli S, Alimoğlu MK, Daloğlu M. Scenario-based learning: preliminary evaluation of the method in terms of students’ academic achievement, in-class engagement, and learner/teacher satisfaction. Adv Physiol Educ. 2023;47(1):144–157. PMID: 36656963. doi:10.1152/advan.00122.2022
43. Agbor-Baiyee W. Problem-based learning case writing in medical science.
44. Chandrasekar H, Gesundheit N, Nevins AB, Pompei P, Bruce J, Merrel SB. Promoting student case creation to enhance instruction of clinical reasoning skills: a pilot feasibility study. Adv Med Educ Pract. 2018;9:249–257. doi:10.2147/AMEP.S155481
45. Gong T, Wang Y, Pu H, Yin L, Zhou M, Tang M. Study on the application value of PBL combined with situational simulation teaching method in Clinical Practice Teaching of Radiology Department. Comput Math Methods Med. 2022;2022:6808648. Retraction in: Comput Math Methods Med. 2023;2023:9870342. PMID: 35991150; PMCID: PMC9388287. doi:10.1155/2022/6808648
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

