Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Endoscopic Lung Volume Reduction Results in Improvement of Diaphragm Mobility as Measured by Sonography
Authors Boyko M, Vonderbank S, Gürleyen H, Gibis N, Schulz A, Erbuth A, Bastian A
Received 28 January 2020
Accepted for publication 24 May 2020
Published 22 June 2020 Volume 2020:15 Pages 1465—1470
DOI https://doi.org/10.2147/COPD.S247526
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Mariya Boyko, Sandy Vonderbank, Hakan Gürleyen, Natalie Gibis, Alina Schulz, Annika Erbuth, Andreas Bastian
Marienkrankenhaus Kassel, Kassel 34127, Germany
Correspondence: Andreas Bastian
Marienkrankenhaus Kassel, Marburger Strasse 85, Kassel 34127, Germany
Email [email protected]
Background: Hyperinflation in patients with pulmonary emphysema is an important cause of reduced diaphragm mobility. We investigated whether endoscopic lung volume reduction (ELVR) could improve diaphragm mobility.
Methods: Diaphragm mobility data obtained by sonography from 44 patients were compared before and 3– 6 months after ELVR therapy with a Spiration™ valve system. These patients were asked whether they wanted this procedure again after they had learned of their treatment outcome; this was a subjective indicator of outcome. Lung function parameters and blood gases were also measured.
Results: After ELVR, 30 patients (82%) developed atelectasis of ≥ 50% of the targeted lung lobe. These patients had a diaphragm mobility increase of 28.97 ± 15.93 mm, while the remaining patients experienced an improvement in diaphragm mobility of 16.07 ± 21.17 mm; this difference was significant (p = 0.030). All 30 patients with atelectasis and additional 6 patients without radiologically demonstrated atelectasis perceived an improved outcome after ELVR. Their diaphragm mobility increased by 28.89 ± 17.26 mm. Conversely, the patients with no perceived improvement in outcome had a diaphragm mobility increase of 6.75 ± 12.76 mm; this difference was significant (p = 0.001).
Conclusion: ELVR can improve diaphragm mobility, and this improvement is correlated with a perceived positive outcome in patients.
Keywords: COPD, emphysema, diaphragm mobility, endoscopic lung volume reduction, ultrasound, outcome
Introduction
In severe chronic obstructive pulmonary disease (COPD), lung hyperinflation impairs the function of respiratory muscles, especially the diaphragm,1 which results in a decrease in diaphragm mobility.2 Hyperinflation can also predict mortality in patients with COPD and emphysema.3,4
Endoscopic lung volume reduction (ELVR) can reduce hyperinflation in a preselected patient group with the absence of collateral ventilation. For such patients, ELVR has become an important option in the treatment of severe emphysema. The best responders are those with little-to-no collateral ventilation to adjacent lung lobes; in such subjects, atelectasis of the targeted lung lobe can be achieved. Collateral ventilation can be measured using the Chartis™ system (Pulmonx, Redwood City, CA, USA). Recently, advanced computed tomography (CT) analytical methods have been developed that can virtually eliminate the need for testing with the Chartis™ system.5 Such methods have become key elements in determining the suitability of candidates for ELVR, as confirmed by several short-term single-center studies.6,7
The aim of ELVR is to achieve volume reduction of the most emphysematous lung lobe. Efficacy has been assessed in several randomized controlled trials by measuring changes in lung-function parameters, by exercise tests, and by health-related quality-of-life questionnaires.7–10
The effects of ELVR therapy on diaphragm mobility have been postulated but, as yet, have not been demonstrated. The focus of the present study was to address this knowledge gap. The gold-standard therapy for the measurement of diaphragm mobility and strength is the electromagnetic stimulation of the phrenic nerve. This is a painful procedure and not repeatable in a patient. Thus, the use of ultrasonography has become a surrogate measure of diaphragm strength and is widely used by many investigators and researchers.
Methods
Ethical Approval of the Study Protocol
The protocol of this retrospective analysis was approved by the local ethics committee of Marienkrankenhaus (S-609/2017). All patients gave written informed consent for the scientific use of their data acquired during hospitalization.
Inclusion Criteria
The inclusion criteria for ELVR were (i) age >40 years; (ii) forced expiratory volume in 1 s (FEV1) between 15% and 45% of the predicted value; (iii) residual volume (RV) >200% of the predicted value; (iv) smokers or ex-smokers with a history of ≥30 pack-years; and (v) completeness of the relevant fissure >90% as a surrogate for absent collateral ventilation assessed by thin-section CT and lung-perfusion scintigraphy (LPS).
Study Population and Clinical Measurements
In this retrospective observational study, clinical data and a subjective marker of outcome (the patients were asked whether they wanted this procedure again, after they had learned of their treatment outcome) were examined. In 2014 and 2016, 78 patients were treated with ELVR using the Spiration™ valve system (Olympus, Hamburg, Germany). Forty-four patients were eligible for this study because, in addition to the inclusion criteria stated above, they had undergone sonographic evaluation of diaphragm mobility before, and 3–6 months after, ELVR. Additionally, they had also stated whether they would undergo ELVR again after they had learned of their treatment outcome.
Upon study initiation, fissure integrity was determined only visually. Subsequently, quantitative computed tomography (qCT) using a VIDA Diagnostics (Coralville, IA, USA) system was employed. qCT showed comparable results to those found when the Chartis system was used to predict fissural integrity.11–13 qCT was also used to measure lobar volumes and emphysematous destruction by lobe. qCT in addition to LPS was used to determine which lung lobe was best suited for ELVR. Particularly in patients with a low degree of disease heterogeneity, LPS helps target the lobe with the lowest perfusion, which is crucial for the prediction of clinical benefits.14,15 If LPS demonstrated a low level of perfusion and qCT showed a high degree of emphysematous destruction and fissure integrity was >90%, then ELVR was performed on the corresponding lung lobe.
Valve Placement
The Spiration™ valve system (Olympus, Hamburg, Germany) was used. Valve placement was undertaken under general anesthesia with jet ventilation via an endotracheal tube.
Sonography Measurement
Sonography measurement was carried out as described previously2 using the upward-downward movement of the lung silhouette in the scapular line—ie, on both sides in the scapular line, the distance of the lung from deep expiration to full inspiration was measured.
Sonography Examination
Participants were evaluated while sitting down. Sonography was undertaken using the Ascendus™ ultrasound system (Hitachi, Tokyo, Japan) using a 3.5-MHz curved probe. The transducer was placed at the lowest part of the lung silhouette in the scapular line. The participant was instructed to exhale as deeply as possible and then to inhale as deeply as possible. This maneuver was filmed. Afterwards, the distance between the highest and lowest point of the lung silhouette was measured. This maneuver was carried out on the right and left side. The mean value was calculated.
Additional Tests
All patients underwent the following lung-function tests: FEV1, vital capacity (VC), and RV. In addition, ventilatory muscle strength (airway occlusion pressure/maximal inspiratory pressure (P0.1/PImax)) and pulmonary blood gases were measured.
Statistical Analyses
The Student’s t-test was used to test the differences between groups with respect to the mean increase in diaphragm mobility and lung function.
Cross-tabulation with Fisher’s exact test was used to analyze the association between atelectasis and outcome. We calculated the Pearson correlation coefficient and p-values to evaluate the association between diaphragm mobility changes and lung-function parameters; a p-value of <0.05 was considered significant.
Results
Forty-four patients (31 women and 13 men; mean age 66.27 [range, 51–77] years) comprised the study cohort. A detailed list including patients’ lung function parameters, blood gas analyses, and diaphragm mobility is given in the supplementary appendix.
Association Between the Development of Atelectasis and Diaphragm Mobility
Thirty patients (68%) developed atelectasis of ≥50% of the targeted lung lobe. The patients with atelectasis had an increase (mean ± SD) in diaphragm mobility of 28.97 ± 15.93 mm. The 14 patients who did not develop atelectasis had an increase in diaphragm mobility of 16.07 ± 21.17 mm. This difference was significant (p = 0.030) (Table 1).
 |
Table 1 Patients Who Developed an Atelectasis Achieved a Higher Increase in Diaphragm Mobility Than Those Who Did Not |
Association Between the Development of Atelectasis and Outcome
All patients who developed atelectasis of ≥50% of the targeted lung lobe (30 patients) perceived a “positive” outcome. Of the 14 patients who did not develop atelectasis, 6 (43%) also perceived a positive outcome. In total, 36 patients perceived a positive outcome (82%) and stated they would undergo the procedure again (Table 2). This difference was significant (p<0.0005).
Association Between Outcome and Diaphragm Mobility
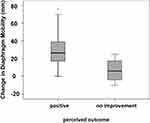
The 36 patients who perceived a positive outcome after ELVR had a mean increase in diaphragm mobility of 28.89 ± 17.25 mm (from 43.7 ± 16.3 mm to 72.6 ± 23.6 mm). The patients with no perceived improvement after ELVR also had an increase in diaphragm mobility but only of 6.75 ± 12.76 mm (from 35.4 mm ± 22.6 mm to 42.13 ± 17.12) (Figure 1). This difference was significant (p = 0.001). This mean difference equated to a correlation value of 0.55, which was highly relevant.
Lung Function
FEV1
The mean value of FEV1 of all study patients before ELVR was 692 mL (29.6% of the predicted value) and 793 mL after ELVR (33.9% of the predicted value). The difference was +101 mL (+14.5%). The patients who perceived a positive outcome after ELVR had an even higher increase in FEV1. The difference in their FEV1 before and after ELVR was +132 mL (+18.5%) (ie, from 714 mL before ELVR to 846 mL after ELVR, and from 29.2% to 34.6% of the predicted value). The patients with no perceived improvement after ELVR had a decrease in FEV1 of −66 mL (−11.1%), from 591 mL before and 525 mL after ELVR (and from 27.1% to 24.1% of the predicted value) (Figure 2). This difference was significant (p = 0.001), with a correlation value of r = 0.59.
VC
The mean value of VC for all study patients before ELVR was 1488 mL and after ELVR was 1709 mL. Their VC increase was 221 mL (+14.8%). The mean value of VC of patients who perceived a positive outcome after ELVR increased from 1531 mL before ELVR to 1819 mL after ELVR (+288 mL; +9.6%). The mean VC of patients with a perceived negative outcome after ELVR decreased from 1292 mL to 1215 mL (−77 mL; −3.1%) after ELVR. This difference was significant (p = 0.002), with a correlation value of 0.32.
RV
The mean value of RV of all study patients before ELVR was 6093 mL and after ELVR was 5520 mL (−573 mL; −9.4%). The mean RV value of patients with a perceived positive outcome after ELVR decreased from 6110 mL to 5325 mL (−785 mL; −12.8%) after ELVR. The mean RV value of patients with a perceived negative outcome after ELVR increased from 6016 mL before ELVR to 6350 mL after ELVR (+334 mL; −5.5%). This difference was not significant.
The differences in changes of base excess (BE) and P0.1/PImax were not significant.
Correlations Between Lung-Function Parameters and Diaphragm Mobility
A correlation was found between increases in FEV1 increases and increases in diaphragm mobility before and after ELVR treatment (r = 0.45). This correlation was significant (p = 0.002).
There was also a correlation between increases in VC increases and increases in diaphragm mobility before and after ELVR treatment (r = 0.36). This correlation was significant (p = 0.017).
The correlations between the RV, BE and P0.1/PImax differences and increased in diaphragm mobility before and after ELVR treatment were not significant.
Discussion
The main result of this observational retrospective study was that endoscopic lung volume reduction (ELVR) improved diaphragm mobility. This improvement could be measured by sonography. Moreover, improvement in diaphragm mobility measured by ultrasound assessment correlated with the perceived outcome of ELVR in patients.
The probability of improvement in diaphragm mobility was significantly higher when ELVR resulted in atelectasis of ≥50% of the targeted lung lobe. Of 44 patients, atelectasis of ≥50% of the targeted lung lobe developed in 30 patients after ELVR. All these patients had a diaphragm mobility increase. Their diaphragm mobility increase was significantly higher than the increase in diaphragm mobility experienced by patients with no atelectasis (28.97 ± 15.93 mm vs 16.07 ± 21.17 mm). Nevertheless, of the 14 patients with no radiologically relevant atelectasis, 6 patients also had a perceived positive outcome. These patients had also answered “Yes” to the question concerning whether they wanted to have the procedure again after they had learned of their treatment outcome.
The correlation between all patients who had perceived a positive outcome (30 with atelectasis of ≥50% of the targeted lung and 6 without) and diaphragm mobility was even higher than that between all patients with atelectasis alone and diaphragm mobility. Patients who perceived a positive outcome had a diaphragm mobility increase of 28.89 ± 17.26 mm. In contrast, the patients who did not perceive improvement after the procedure had a diaphragm mobility increase of only 6.75 ± 12.76 mm. Hence, the subjectively perceived success of ELVR was associated with a significantly higher increase in diaphragm mobility. These data support the notion that (i) diaphragm mobility may be an important factor of perceived good general health, and (ii) ELVR improves perceived better health by increasing diaphragm mobility.
Furthermore, our results demonstrated that the functional force of the diaphragm that is impaired by loss and quality of muscle in severe COPD16 can be improved by ELVR. However, our study did not demonstrate that the muscle force itself improved or that muscle mass increased after ELVR, but diaphragm mobility may improve because the diaphragm gains more space to move because of lung volume reduction.
The mean increase in FEV1 in our patients was 14.5% (+101 mL). The patients who perceived a positive outcome had an even higher increase in FEV1 (18.5%). These values are comparable with those of the most relevant studies on this topic. Valipour et al,7 reported a 13.7% (+100 mL) increase in FEV1 3 months after ELVR, Wang et al,17 reported an increase of 11.44%, van Geffen et al,18 demonstrated 21.77%, and Kemp et al,19 revealed 20.7%.
We included only patients who had diaphragm mobility measured by sonography before, and 3–6 months, after ELVR, and only patients who answered the question concerning whether they would have the procedure again now they knew their treatment outcome. Hence, our study did not reflect the results of our total ELVR treatment cohort. We included patients with homogeneous and heterogeneous emphysema. This strategy is not relevant to changes in diaphragm mobility, though it may influence the patient outcome with regard to lung function parameters.
The total number of pneumothoraces in our ELVR patient group was only 4 (9.1%). Two cases resolved with drainage alone. One patient needed removal of one valve and two patients needed surgery (including the one who had had a valve removed previously). The low number of pneumothoraces in our study was an additional indicator that our patient selection was not random—ie, patients were selected if they had undergone sonography of the thorax before, and 3–6 months after, ELVR. However, this selection bias was not relevant to our main result: ELVR can increase diaphragm mobility.
Another complication was missing atelectasis despite a high degree of fissure integrity or resolution of atelectasis over time. Four patients needed valve replacement. One patient had early valve replacement; the expected atelectasis was not detectable during the first week on chest radiography even though the relevant fissure was complete. A control bronchoscopy confirmed the expected valve displacement. The other three patients had already developed atelectasis before the collapsed lung lobe refilled with air. After valve replacement, the expected atelectasis was achieved. All these patients were included in the study but ultrasound results were included only after valve replacement had been carried out.
Abbreviations
ELVR, endoscopic lung volume reduction; P0.1/PImax, measurement of ventilatory muscle strength; CT, computed tomography; FEV1, forced expiratory volume in 1 s; VC, vital capacity; RV, residual volume; COPD, chronic obstructive pulmonary disease; BE, base excess; LPS, lung perfusion scintigraphy.
Data Sharing Statement
All data relevant to the study can be acquired from the corresponding author by email.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki 1975 and its later amendments. The ethics committee of the Marienkrankenhaus approved the study (S-609/2017). All patients gave written informed consent for the scientific use of the data acquired during hospitalization.
Consent for Publication
All authors have approved this manuscript for publication.
Funding
There was no financial support for this study.
Disclosure
None of the authors has competing interests or financial interests in the publication of this study.
References
1. Shah PL, Herth FJ, van Geffen WH, Deslee G, Slebos DJ. Lung volume reduction for emphysema. Lancet Respir Med. 2017;5(2):147–156. doi:10.1016/S2213-2600(16)30221-1
2. Scheibe N, Sosnowski N, Pinkhasik A, Vonderbank S, Bastian A. Sonographic evaluation of diaphragmatic dysfunction in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:1925–1930. doi:10.2147/COPD.S85659
3. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi:10.1371/journal.pmed.0030442
4. Casanova C, Cote C, de Torres JP, et al. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(6):591–597. doi:10.1164/rccm.200407-867OC
5. Gompelmann D, Eberhardt R, Slebos DJ, et al. Diagnostic performance comparison of the Chartis system and high-resolution computerized tomography fissure analysis for planning endoscopic lung volume reduction. Respirology. 2014;19(4):524–530. doi:10.1111/resp.12253
6. Herth FJ, Noppen M, Valipour A, et al. Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort: results from the International VENT Study Group. Eur Respir J. 2012;39(6):1334–1342. doi:10.1183/09031936.00161611
7. Valipour A, Slebos DJ, Herth F, et al. Endobronchial valve therapy in patients with homogeneous emphysema: results from the IMPACT study. Am J Respir Crit Care Med. 2016;194(9):1073–1082. doi:10.1164/rccm.201607-1383OC
8. Sciurba FC, Ernst A, Herth FJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363(13):1233–1244. doi:10.1056/NEJMoa0900928
9. Davey C, Zoumut Z, Jordan S, et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomized controlled trial. Lancet. 2015;386(9998):1066–1073. doi:10.1016/S0140-6736(15)60001-0
10. Klooster K, Ten Hacken NH, Hartman JE, Kerstjens HA, van Rikxoort EM, Slebos DJ. Endobronchial valves for emphysema without interlobar collateral ventilation. N Engl J Med. 2015;373(24):2325–2335. doi:10.1056/NEJMoa1507807
11. Slebos DJ, Shah PL, Herth FJ, Valipour A. Endobronchial valves for endoscopic lung volume reduction: best practice recommendations from expert panel on endoscopic lung volume reduction. Respiration. 2017;93:138–150. doi:10.1159/000453588
12. Schuhmann M, Raffy P, Yin Y, et al. Computed tomography predictors of response to endobronchial valve lung reduction treatment: comparison with Chartis. Am J Respir Crit Care Med. 2015;191(7):767–774. doi:10.1164/rccm.201407-1205OC
13. Koster TD, van Rikxoort EM, Huebner RH, et al. Predicting lung volume reduction after endobronchial valve therapy is maximized using a combination of diagnostic tools. Respiration. 2016;92:150–157. doi:10.1159/000448849
14. Argula RG, Strange C, Ramakrishnan V, Goldin J. Baseline regional perfusion impacts exercise response to endobronchial valve therapy in advanced pulmonary emphysema. Chest. 2013;144:1578–1586. doi:10.1378/chest.12-2826
15. Thomsen C, Theilig D, Herzog D, et al. Lung perfusion and emphysema distribution affect the outcome of endobronchial valve therapy. Int J Chron Obstruct Pulmon Dis. 2016;11:1245–1259. doi:10.2147/COPD.S101003
16. Ottenheijm CA, Heunks LM, Sieck GC, et al. Diaphragm dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172(2):200–205. doi:10.1164/rccm.200502-262OC
17. Wang Y, Lai TW, Xu F, et al. Efficacy and safety of bronchoscopic lung volume reduction therapy in patients with severe emphysema: a meta-analysis of randomized controlled trials. Oncotarget. 2017;8(44):78031–78043. doi:10.18632/oncotarget.19352
18. van Geffen WH, Slebos DJ, Herth FJ, Kemp SV, Weder W, Shah PL. Surgical and endoscopic interventions that reduce lung volume for emphysema: a systemic review and meta-analysis. Lancet Respir Med. 2019;7(4):313–324. doi:10.1016/S2213-2600(18)30431-4
19. Kemp SV, Slebos D-J, Kirk A, et al. A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (TRANSFORM). Am J Respir Crit Care Med. 2017;196(12):1535–1543. doi:10.1164/rccm.201707-1327OC
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.