Back to Journals » International Journal of Women's Health » Volume 14
Endometrial Cryoablation for the Treatment of Heavy Menstrual Bleeding: 36-Month Outcomes from the CLARITY Study
Authors Curlin HL , Anderson TL
Received 16 April 2022
Accepted for publication 3 August 2022
Published 10 August 2022 Volume 2022:14 Pages 1083—1092
DOI https://doi.org/10.2147/IJWH.S371044
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Howard L Curlin, Ted L Anderson
Department of Obstetrics and Gynecology, Vanderbilt University Medical Center, Nashville, TN, USA
Correspondence: Howard L Curlin, Email [email protected]
Study Objective: To examine long-term outcomes from the pivotal study that evaluated the safety and effectiveness of the Cerene® Cryotherapy Device (Channel Medsystems, Berkeley, CA) in premenopausal women with heavy menstrual bleeding due to benign causes who have completed childbearing.
Methods: The prospective, multicenter, single-arm, open-label study had eight sites in the USA, one in Mexico, and two in Canada. Inclusion criteria included uterine sound ≤ 10 cm, endometrial cavity length 2.5 to 6.5 cm, age 25 to 50 years, a pictorial blood loss assessment chart score of ≥ 150, no submucosal myomata and/or uterine obstruction, distortion, or abnormality. A total of 242 subjects underwent a 2.5-minute cryoablation. Long-term follow-up visits were conducted at Month 24 and Month 36. Data collected included gynecological adverse events, description of last menstrual period, contraception status, self-report of pregnancy, medical or surgical interventions to treat abnormal uterine bleeding, satisfaction, recommendation, and quality of life (QoL). QoL outcomes were measured with the Menorrhagia Impact Questionnaire (MIQ) and the Premenstrual Symptoms Impact Survey (PMSIS™).
Results: 201 subjects completed their Month 36 final study visit. Subject outcomes were comparable to those at Month 12. Eighty-nine percent of subjects reported amenorrhea, a lighter-than-normal, or normal period, 91% of subjects had no or slight limitations in MIQ measured activities, and 85% reported premenstrual symptoms at a low frequency. Eighty-five percent of the subjects were satisfied or very satisfied. The cumulative incidence of hysterectomy was 5% and reintervention was 8.7%. Forty-nine gynecologic adverse events (AE) were reported; one non-serious AE, postcoital bleeding, was reported as related to the procedure. No serious device-related or procedure-related AEs were reported.
Conclusion: Study data demonstrate that the positive effects of Cerene Cryotherapy Device treatment are sustained through Month 36 and that the risks associated with the device and procedure are low (ClinicalTrials.gov; NCT02842736).
Keywords: ablation, endometrial, menorrhagia, cryotherapy
Introduction
Heavy menstrual bleeding (HMB) affects more than 10 million (or 1 in 5) women annually in the USA.1 International studies report similar incidence rates, affecting 25% to 30% of the women.2,3 The incidence is variable because not all women seek care for their menstrual symptoms, while others may not be aware of when to seek professional advice or the types of treatments available.3,4 Impaired quality of life (QoL) of women affected by HMB significantly impacts health care utilization, which in turn places an economic burden on the healthcare system.5,6 Hysterectomy and endometrial ablation are two different surgical options for menstrual bleeding, although hysterectomy is generally recommended after other therapies have failed. The use of nonresectoscopic endometrial ablation (NREA) devices has become a mainstay in the treatment of HMB in women who no longer desire fertility and are not candidates for or who refuse medical therapy. Similarly, NREA offers a uterine sparing alternative to hysterectomy, the most invasive treatment for HMB. Compared to resectoscopic endometrial ablation (REA) techniques, NREA devices require less training, skill, and experience and have comparable effectiveness with fewer complications. The treatment has a shorter operative time, lower morbidity, faster recovery time, and improved QoL with high patient satisfaction. NREA is easier to perform and often offers the opportunity for the treatment to be completed in the office setting.7–9 In office, NREA can provide physicians with flexibility in their schedules and optimized resource utilization. Further, ability to provide NREA in the office setting may offer greater patient acceptance and access to treatment. To further expand in office use, physician training, patient comfort, anesthesia techniques, and reimbursement needs must be considered.9
The most often cited concern associated with endometrial ablation is the need for subsequent hysterectomy due to new pelvic pain and/or unresolved or recurrent HMB.9–13 Depending upon the type of endometrial ablation, this risk can be greater than 20% within 3 years of treatment.9,14 One issue driving hysterectomy after failed endometrial ablation is the inability to assess the endometrium histologically due to intracavitary scarring induced to varying degrees by some ablation techniques. Furthermore, intracavitary scarring can lead to long-term complications, such as central or cornual hematometra, post ablation tubal sterilization syndrome (PATSS), retrograde uterine bleeding potentially leading to the development of endometriosis, and the possible delay in diagnosis of an endometrial cancer.15 In particular, radiofrequency ablation (RFA), which makes up the majority of NREA (73%) performed annually in the US, has been associated with a high rate of post ablation intrauterine synechiae which may limit the ability to adequately evaluate the endometrium by biopsy or hysteroscopy to address subsequent abnormal uterine bleeding (AUB).10,16–19
The Cerene® Cryotherapy Device (Cerene Device; Channel Medsystems, Inc. Berkeley, CA) is a novel endometrial ablation device that uses nitrous oxide (N2O) to freeze and ablate the endometrium.20,21 The Cerene Device is approved by the Food and Drug Administration (FDA) for use in premenopausal women with HMB resulting from a spectrum of benign causes for whom childbearing is complete. It was developed to address the unmet clinical need for an endometrial ablation device that could be used in the office setting with limited requirements for anesthesia. Cryogenic fluid or gas is known to have an anesthetic effect on the nerves in the uterine tissue.22 During the CLARITY Study, all treatments were performed with paracervical block and 97% of the subjects had only oral pain medication or no pain medication at all during their procedure yet reported minimal discomfort. Seventy-four percent of the treatments were performed in the office setting, and the remainder were performed in a hospital treatment room. Previously published data confirmed that the Cerene device is safe, effective, and well tolerated in the office setting without the need for intravenous sedation.9 This report provides the 24- and 36-month outcomes of subjects after treatment.
Materials and Methods
Study Design
A prospective, multicenter, international, single-arm, open label, non-randomized, study (the CLARITY Study) was conducted to evaluate the safety and effectiveness of the Cerene® Cryotherapy Device. The details and Month 12 outcomes of this study conducted at 11 sites in Canada, Mexico, and the United States of America have been published previously.21 Inclusion criteria were refractory heavy menstrual bleeding with no definable organic cause, women aged between 25 and 50 years, uterine length ≤10cm, endometrial cavity length between 2.5 cm and 6.5 cm, myometrial thickness of ≥10mm, menstrual blood loss with a pictorial blood loss assessment chart (PBLAC) score of ≥150, premenopausal confirmed by follicle stimulating hormone level <30 IU/L when age is >40 years, agrees to use a reliable form of contraception following ablation treatment, and has predictable and cyclic menstruation. Exclusion criteria included pregnancy or a desire to conceive; endometrial hyperplasia; active endometritis; vaginal or uterine infection; active pelvic inflammatory disease or sexually transmitted infection; active genital infection; presence of bacteremia, sepsis, or other active systemic infection; known or suspected abdominal, pelvic, or gynecologic malignancy within the past 5 years; clotting defects or bleeding disorders; abnormal cytology or human papillomavirus testing not treated according to local standards; prior uterine surgery that interrupts the integrity of the uterine wall; a previous low transverse cesarean section with the myometrial thickness <10 mm; previous endometrial ablation procedure; clinically significant adenomyosis based on transvaginal ultrasound; abnormal uterine cavity; current use of an intrauterine device and unwilling to remove the intrauterine device; an implantable contraceptive device; and post-partum <6 months. Malignant or structural causes of heavy menstrual bleeding were ruled out through transvaginal ultrasound, endometrial biopsy, and diagnostic hysteroscopy in all patients.
The study received regulatory approval by Health Canada, Mexico COFEPRIS, and the US Food and Drug Administration (FDA), respectively. The 11 investigative sites utilized the same clinical protocol in accordance with FDA regulations, the Declaration of Helsinki, and the requirements of local ethics committees and regulatory bodies, including those for subject privacy, informed consent, and record retention. The study protocol was approved by Advarra Central Institutional Review Board (IRB) for sites that did not have a local IRB, by the local IRB at Vanderbilt University Medical Center (Nashville, TN), the Research Ethics Committee of the School of Medicine and University Hospital of the Universidad Autónoma de Nuevo León (Monterrey, Mexico), the Research Ethics Committee of the St. Mary Medical Center (Montreal, Quebec, Canada), and the Health Research Ethics Board of Alberta (Edmonton, Alberta, Canada). All required approvals were obtained prior to subject enrollment at each participating investigative site. All subjects provided written informed consent prior to the initiation of any study-related procedures.
A total of 242 women aged 25 to 50 years with HMB underwent endometrial ablation using the Cerene® Cryotherapy Device. Analgesia and local anesthesia were administered per investigator discretion. No subjects received general anesthesia, 3% received IV sedation, and 97% received oral or no medications in addition to a paracervical block. Seventy-four percent of Cerene treatments were performed in the office setting, and the remainder were performed in a hospital treatment room. The primary effectiveness endpoint was a reduction in menstrual bleeding, with success defined as a PBLAC score of ≤75 at Month 12, with the effectiveness rate compared to an FDA-established objective performance criterion (66% for NREA devices).23 The primary safety endpoint was the incidence of serious adverse events (SAEs) and serious device-related adverse events (AEs).
Long-term follow-up evaluations were conducted in person at the clinical site or by telephone by one of the study coordinators at month 24 and month 36. Data collected included gynecological adverse events, subject description of her last menstrual period prior to the follow-up visit (none, lighter than normal, normal, or heavy), contraception status, subject self-report of pregnancy, the need for medical or surgical interventions to treat abnormal uterine bleeding, subject satisfaction (very satisfied, satisfied, dissatisfied, or very dissatisfied), and subject recommendation (definitely, maybe, probably not, or definitely not). Quality of life (QoL) assessments were measured using two validated instruments: the Menorrhagia Impact Questionnaire (MIQ) and the Premenstrual Symptoms Impact Survey (PMSIS™).24,25
A sample size of 242 subjects was determined for the CLARITY study assuming a 75% success rate of the Cerene Device in the intention-to-treat (ITT) population. Considering the possibility of up to a 10% (24 subjects) drop-out, then the Cerene Device had to achieve a success rate of approximately 84% among subjects with a complete Month 12 PBLAC to achieve a success rate in the ITT cohort of 75%. The study protocol was registered at ClinicalTrials.gov (NCT02842736).
Device Description
The Cerene Cryotherapy Device is a single-use, disposable device that uses cryothermal energy to achieve ablation depths of 5 to 9 mm throughout the uterine cavity. The device can treat uterine cavities ranging in length between 2.5 and 6.5 cm with corresponding uterine soundings up to 10 cm. The diameter of the sheath is less than 6 mm. During treatment, liquid N2O flows from a small cylinder located in the device handle and into an inflow line with multiple jets. The cryothermic energy is provided by a liquid-to-gas phase change of nitrous oxide (N2O), which occurs at −86 ℃. The liquid N2O is infused into a polyurethane liner where it converts into gas. This conformable liner enables coverage of irregular surfaces of the uterine cavity. The status and sequential operating instructions are displayed on the device’s display screen and guide the user through the procedure. When treatment is initiated, automated leak and perforation detection tests are performed. After completion of these tests, N2O flows for the duration of the 2.5-minute treatment.20
Data Analysis
Descriptive statistical analyses were performed using SAS® software, version 9.3, and Microsoft Access version 2007. To analyze continuous variables, descriptive statistics were used and included the number of subjects (n), mean, standard deviation, median, minimum, and maximum. This study was conducted in accordance with the clinical protocol, Good Clinical Practice guidelines, and International Standards Organization standards. Prior to study enrollment, all required institutional review board approvals were obtained.
Results
Subject demographic data for the 242 subjects have been previously reported and are consistent with those of other GEA clinical studies.21 A total of 210 subjects were available for follow-up at 24 months and 201 subjects were available at 36 months. Subject disposition was compared with data from 12 months published previously (Table 1).21
 |
Table 1 Study Subject Disposition at Months 12, 24, and 36 |
There were no serious adverse device-related effects reported in the CLARITY Study. The primary effectiveness outcome, with success defined as a PBLAC score of ≤75, was met in 76.9% of the intention-to-treat (ITT) cohort at 12 months, exceeding the FDA success criteria.21 The PBLAC instrument was not used after the Month 12; instead, subjects were asked to describe the last menstrual period (LMP) experienced prior to follow-up visits at Month 12, Month 24, and Month 36. Subjects’ menstrual bleeding remained stable during the long-term follow-up. At Month 12, 90.9% of subjects described their LMP as none, lighter than normal, or normal and 9.1% reported heavy periods. This effect persisted at 36 months, with 88.6% of subjects describing their LMP as none, lighter than normal, or normal and 11.4% reporting heavy periods (Table 2). The full cohort of available subjects at 24 months (210) did not complete subject perception questions (last menstrual period, satisfaction, and recommendation) or QoL instruments because IRB/Ethics Committee approval of the protocol amendment had not been obtained by the time of their visit.
 |
Table 2 Study Description of Her Last Menstrual Period Prior to Follow-Up Visit |
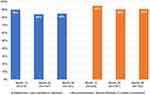
Subjects’ satisfaction with the outcome of Cerene treatment and willingness to recommend the procedure to others also remained stable. Eighty-five percent of the subjects reported that they were “satisfied” or “very satisfied” with Cerene treatment at the month 36 visit; 90.7% of the subjects reported they would “definitely” or “maybe” recommend the procedure (Figure 1).
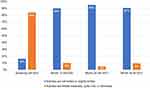
Improvement in subjects’ QoL, as measured by the impact of menstrual bleeding on daily activities and the occurrence of premenstrual symptoms, was sustained for 3 years after treatment. At screening, 84% of the subjects reported their daily activities as being limited often, most often, very often, or all the time in the MIQ. However, by month 12, 90% of the subjects reported their activities were not limited or only slightly limited, which persisted through the Month 36 visit (Figure 2). Likewise, 75% of the subjects reported a high incidence of premenstrual symptoms through the PMSIS tool at screening, whereas at 12 months after Cerene treatment, 83% of the subjects reported they were free of symptoms often, most often, very often or all the time. This reduction in premenstrual symptoms was also maintained at month 36 (Figure 3).
Adverse events during the first 12 months post-treatment have been reported previously.21 There were 52 gynecologic adverse events reported between months 12 and 36 (Table 3), including one incidence of postcoital bleeding determined to be procedure related. There have been 5 pregnancies reported through 36 months post-treatment, 1 of which was an ectopic pregnancy reported in the first year and was removed surgically. There were 4 pregnancies reported between 12 and 36 months of follow-up, all of which were intrauterine. One intrauterine pregnancy was terminated, and the subject continued in the study. Three pregnancies resulted in preterm (35–36 weeks) live births by caesarean delivery.
 |
Table 3 Gynecologic Adverse Events After Month 12 Through Month 36 |
By the end of 36 months follow-up, 21 (8.7%) subjects required medical or surgical interventions. Six (2.5%) subjects were treated with medications, 1 (0.4%) subject had a repeat endometrial ablation with another commercial GEA, 1 (0.4%) subject underwent a repeat endometrial ablation with a commercial GEA and concomitant placement of a levonorgestrel-eluting intrauterine device (IUD), and 1 (0.4%) subject had a levonorgestrel-eluting IUD placed (Table 1).
Twelve (5.0%) subjects underwent a hysterectomy by the end of 36 months post-treatment (Table 4). Of these, 6 (50%) were age 40 or less (range 29–39). Ten subjects elected hysterectomy despite decrease in post-ablation menstrual bleeding documented at the Month 12 follow-up visit; six of these subjects met the PBLAC endpoint for treatment success. Hysterectomy was performed prior to the Month 12 visit in two subjects, prior to the Month 24 visit in six subjects, and prior to the Month 36 visit in four subjects. New pelvic pain was not reported as the reason for hysterectomy in the three subjects that had a tubal ligation prior to treatment; one of the three subjects had non-intracavitary uterine fibroids and two reported increased menstrual bleeding.
 |
Table 4 Hysterectomy Post Treatment: Subject Characteristics |
Among the 101 subjects who had undergone a tubal ligation prior to cryoablation and were available for a follow-up visit at Month 12 (n=97), Month 24 (n=90), and Month 36 (n=87), none reported symptoms of new pelvic pain suggesting hematometra or post ablation tubal sterilization syndrome (PATSS). Six of these subjects had a reintervention. Three had hysterectomy (two due to unresolved heavy menstrual bleeding and one to symptomatic uterine fibroids). Of the remaining three, two were placed on a hormonal medication and one treated with a levonorgestrel-eluting IUD.
Discussion
This prospective, 3-year follow-up study demonstrated sustained safety and effectiveness of treatment with the Cerene Device, a novel cryoablation device for the treatment of HMB. Reduced bleeding patterns reported by subjects remained relatively constant from month 12 to month 36. Subject QoL improvements with two validated instruments, satisfaction with Cerene treatment, and likelihood of recommending the procedure to family and friends were maintained through the 36-month visit. Overall, the CLARITY study has demonstrated the durability of Cerene treatment. Following Cerene treatment, the cumulative incidence of medical and surgical interventions and hysterectomy was low. The reintervention rate for the Cerene device compares favorably with recently published data for a water vapor endometrial ablation device.14
Several studies have focused on the complications of late onset endometrial ablation failure that eventually requires a hysterectomy.26–31 Symptoms that are characteristic of endometrial ablation failure include persistent or recurrent vaginal bleeding, cyclic pelvic pain, and the inability to adequately access the endometrium.12,26 The number of women reported in the literature undergoing a hysterectomy after ablation is wide ranging. A retrospective cohort analysis of 3681 women aged 25–60 years, who underwent treatment with both resectoscopic and NREA techniques at 30 Kaiser Permanente Northern California facilities found that hysterectomy was subsequently performed in 21% of the subjects. The study demonstrated that women less than 40 years of age have a higher risk of hysterectomy after endometrial ablation and that the hysterectomy risk is highest during the first 3 years of endometrial ablation, but the rate continues to increase through 8 years of follow-up.27 An additional retrospective cohort study of 1169 women, mean age of 41.1, who underwent either a rollerball endometrial ablation or NREA procedure found that subsequent hysterectomy was significantly associated with the type of ablation. Women who underwent rollerball endometrial ablation had a statistically significant higher rate of hysterectomy than women who had a NREA procedure. Among all women who had undergone either rollerball, thermal balloon, radiofrequency, or cryoablation, 13.4% underwent hysterectomy, with 60% to 80% of the hysterectomies occurring within 2 to 3 years after treatment.28 Similarly, a retrospective cohort analysis of 5936 women, mean age of 42.7, who underwent ablation with NREA devices at a single academic affiliated community hospital, observed that 13.8% underwent a hysterectomy and 1.8% had repeat ablation; the overall reintervention rate increased over time.11
The incidence of hysterectomy within 36 months following Cerene treatment was low (5.0%). This is lower than the cited results for women having undergone endometrial ablation procedures with other modalities. Notably, half of the patients who ultimately underwent hysterectomy did so despite documented ablation treatment success by PBLAC score.
A small retrospective analysis of 55 subjects who underwent NREA found that 7.3% experienced PATSS between 8 months and 43 months following ablation. Of these, 3.6% presented with central hematometra.29 Another study that compared laparoscopic supracervical hysterectomy with NREA devices observed an incidence of <1.0% of hematometra for each group.13 In addition, a study of women who underwent thermal balloon ablation found hematometra occurred in 1% to 3% of the subjects.30 Overall, the incidence of PATSS following endometrial ablation procedures appears to be low, ranging from 6% to 8%, and developing within 2 to 3 years.30,31 Among the 101 subjects who underwent tubal sterilization prior to Cerene treatment, there were no reports or findings of hematometra or PATSS through 36 months. Although three subjects who underwent hysterectomy in the CLARITY study had undergone prior tubal sterilization, none had symptoms suggesting hematometra or PATSS. Indeed, one subject had symptomatic uterine fibroids and two had increased menstrual bleeding. Previously described hysteroscopic assessment of the uterine cavity at 12 months after Cerene treatment demonstrated that access to the uterine cavity is preserved in the majority of patients and this likely helps to explain the absence of PATSS thus far.21 As the CLARITY study used a multicenter design, we believe the results can be generalized to the larger population of women with HMB.
There were five pregnancies in subjects through 36 months post-ablation, one of which was an ectopic pregnancy. This reinforces the fact that endometrial ablation should not be regarded as a contraceptive, much less sterilization, procedure. Patients undergoing any type of endometrial ablation should be counseled on the need to continue a reliable form of contraception. Indeed, none of the subjects who became pregnant after Cerene ablation were using contraception despite counseling.
The strengths of our study are that it is a prospective multicenter trial with excellent retention of subjects through the final study visit. Ninety-three percent (n=225) of the subjects had a known outcome. Four (1.6%) subjects withdrew voluntarily and only 13 (5.4%) subjects were lost to follow-up. The limitations of our study include the under-representation of African American women and it was not randomized with a specific comparator ablation technique. Another potential limitation is some of the quality-of-life instruments were administered by phone for the Month 24 and Month 36 visit, thereby possibly introducing bias by the study coordinator. However, we think this risk is low as study coordinators were trained at the beginning of the study how to administer the instruments, questions were asked exactly as they appeared on the questionnaire, the subject was familiar with the questionnaires having completed them in person at screening, Months 3, 6, and 12, and the questionnaires were unchanged.
Conclusion
The Cerene Device provides safe, effective, and durable outcomes through 36 months for the treatment of heavy menstrual bleeding due to benign causes in women for whom childbearing is complete. It allows patients to be treated in the comfort of their physicians’ office in a convenient, efficient fashion which produces a high level of satisfaction.
Data Sharing Statement
Will individual deidentified participant data be available? No. What specific data will be shared? N/A. What other study documents will be available? N/A. How will the data be accessible? N/A. When will the data be available (start and end dates)? N/A.
Acknowledgments
- Channel Medsystems Inc. for sponsoring the study and coordinating statistical support from Gordon and Associates, Inc.
- Site Primary Investigators (PI) other than the authors: Bruce Allan, MD, PhD; Cindy Basinski, MD; Scott Boyd, MD; Amy Brenner, MD; Claude Fortin, MD; Jose Garza, MD; Eric Hawes, MD; Randall Kahan, MD; Gerard Reilly, MD; Todd Rumsey, MD; and Scott Schade, MD.
- Ginny Vachon, PhD (Principal Medvantage, LLC, Atlanta, GA) for editorial assistance.
- Portions of this manuscript were presented at the 49th AAGL Global Conference in Austin, Texas, USA, from November 14 to 17, 2021.
Funding
The CLARITY Study was sponsored by Channel Medsystems Inc., Berkeley, CA.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Centers Disease Control Prevention. Heavy menstrual bleeding. Centers for disease control and prevention; 2015. Available from: https://www.cdc.gov/ncbddd/blooddisorders/women/menorrhagia.html.
2. Hurskainen R, Grenman S, Komi I, et al. Diagnosis and treatment of menorrhagia. Acta Obstet Gynecol Scand. 2007;86(6):749–757. doi:10.1080/00016340701415400
3. Su S, Yang X, Su Q, Zhao Y. Prevalence and knowledge of heavy menstrual bleeding among gynecology outpatients by scanning a WeChat QR Code. PLoS One. 2020;15(4):e0229123. doi:10.1371/journal.pone.0229123
4. Santer M, Wyke S, Warner P. Women’s management of menstrual symptoms: findings from a postal survey and qualitative interviews. Soc Sci Med. 2008;66(2):276–288. doi:10.1016/j.socscimed.2007.08.018
5. Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194. doi:10.1111/j.1524-4733.2007.00168.x
6. Jensen JT, Lefebvre P, Laliberté F, et al. Cost burden and treatment patterns associated with management of heavy menstrual bleeding. J Women's Health. 2012;21(5):539–547. doi:10.1089/jwh.2011.3147
7. Levie MD, Chudnoff SG, Prospective A. Multicenter, pivotal trial to evaluate the safety and effectiveness of the AEGEA vapor endometrial ablation system. J Minim Invasive Gynecol. 2019;26(4):679–687. doi:10.1016/j.jmig.2018.07.012
8. Cooper J, Gimpelson R, Laberge P, et al. A randomized, multicenter trial of safety and efficacy of the NovaSure system in the treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9(4):418–428. doi:10.1016/S1074-3804(05)60513-0
9. Munro MG. Endometrial ablation. Best Pract Res Clin Obstet Gynaecol. 2018;46:120–139. doi:10.1016/j.bpobgyn.2017.10.003
10. Wortman M. Late-onset endometrial ablation failure. Case Rep Women's Health. 2017;12(15):11–28. doi:10.1016/j.crwh.2017.07.001
11. Klebanoff J, Makai GE, Patel NR, Hoffman MK. Incidence and predictors of failed second-generation endometrial ablation. Gynecol Surg. 2017;14(1):26. doi:10.1186/s10397-017-1030-4
12. Wortman M, Cholkeri A, McCausland AM, McCausland VM. Late-onset endometrial ablation failure–etiology, treatment, and prevention. J Minim Invasive Gynecol. 2015;22(3):323–331. doi:10.1016/j.jmig.2014.10.020
13. Cooper K, Breeman S, Scott NW, et al.; HEALTH Study Group. Laparoscopic supracervical hysterectomy versus endometrial ablation for women with heavy menstrual bleeding (HEALTH): a parallel-group, open-label, randomised controlled trial. Lancet. 2019;394(10207):1425–1436. doi:10.1016/S0140-6736(19)31790-8
14. Leyland N, Harris M. Water vapor endometrial ablation for heavy menstrual bleeding: 36-month follow-up of a prospective, multicenter pivotal clinical trial. Int J Women's Health. 2021;13:169–176. doi:10.2147/IJWH.S279864
15. McCausland A, McCausland V. Long-term complications of endometrial ablation: cause, diagnosis, treatment, and prevention. J Minim Invasive Gynecol. 2007;14:399–406. doi:10.1016/j.jmig.2007.04.004
16. Ahonkallio SJ, Liakka AK, Martikainen HK, et al. Feasibility of endometrial assessment after thermal ablation.”. Euro J Obstet Gynec Reprod Biol. 2009;147:69–71. doi:10.1016/j.ejogrb.2009.06.014
17. Luo X, Lim C, Li L, et al. Hysteroscopic appearance of endometrial cavity after microwave endometrial ablation. J Minim Invasive Gynecol. 2010;17:30–36. doi:10.1016/j.jmig.2009.09.012
18. MacMahon C, Hatti A, Bakour S, et al. Challenges of endometrial assessment after ablation in women with postmenopausal bleeding - A case series. Obstet Gynecol. 2018;38(3):432–434.
19. Wortman M, Daggett A, Deckman A. Ultrasound-guided reoperative hysteroscopy for managing global endometrial ablation failures. J Min Invasive Gynecol. 2014;21(2):238–244. doi:10.1016/j.jmig.2013.09.011
20. Cerene®. Cryotherapy Device Instructions for Use. Berkeley, CA: Channel Medsystems; 2019.
21. Curlin HL, Cintron LC, Anderson TL, Prospective A. Multicenter, clinical trial evaluating the safety and effectiveness of the cerene device to treat heavy menstrual bleeding. J Minim Invasive Gynecol. 2021;28(4):899–908. doi:10.1016/j.jmig.2020.08.013
22. Evans PJ. Cryoanalgesia. The application of low temperatures to nerves to produce anaesthesia or analgesia. Anaesthesia. 1981;36(11):1003–1013. doi:10.1111/j.1365-2044.1981.tb08673.x
23. FDA. Letter to endometrial ablation industry about objective performance criteria. Available from: https://www.fda.gov/media/94793.
24. Bushnell DM, Martin ML, Moore KA, Richter HE, Rubin A, Patrick DL. Menorrhagia Impact Questionnaire: assessing the influence of heavy menstrual bleeding on quality of life. Curr Med Res Opin. 2010;26(12):2745–2755. doi:10.1185/03007995.2010.532200
25. Wallenstein GV, Blaisdell-Gross B, Gajria K, et al. Development and validation of the Premenstrual Symptoms Impact Survey (PMSIS): a disease-specific quality of life assessment tool. J Women's Health. 2008;17(3):439–450. doi:10.1089/jwh.2007.0377
26. Sharp HT. Endometrial ablation: postoperative complications. Am J Obstet Gynecol. 2012;207(4):242–247. doi:10.1016/j.ajog.2012.04.011
27. Longinotti MK, Jacobson GF, Hung YY, Learman LA. Probability of hysterectomy after endometrial ablation. Obstet Gynecol. 2008;112(6):1214–1220. doi:10.1097/AOG.0b013e31818c1766
28. Shavell VI, Diamond MP, Senter JP, Kruger ML, Johns DA. Hysterectomy subsequent to endometrial ablation. J Minim Invasive Gynecol. 2012;19(4):459–464. doi:10.1016/j.jmig.2012.03.013
29. Talukdar S, Eisenstein D, Sangha R. Symptomatic central hematometra and postablation tubal sterilization syndrome (PATSS) after second generation endometrial ablation. J Minim Invasive Gynecol. 2015;22(6S):S189. doi:10.1016/j.jmig.2015.08.689
30. Hubert SR, Marcus PS, Rothenberg JM, Schilder JM, Hurd WW. Hematometra after thermal balloon endometrial ablation in a patient with cervical incompetence. J Laparoendosc Adv Surg Tech A. 2001;11(5):311–313. doi:10.1089/109264201317054627
31. Sinha P. Endometrial ablation–long-term complications. Wiad Lek. 2004;57(Suppl 1):276–277.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.