Back to Journals » Journal of Blood Medicine » Volume 13
Endocrine Complications and the Effect of Compliance with Chelation Therapy in Patients with Beta Thalassemia Major in Eastern Province of Saudi Arabia
Authors Habbash F, Al-Bati W, Al-Hashim H , Aldossari M , Alali A, Alalyani K, Al-Ebrahim Z, Hamed N, Eraqe S, Binayfan Z, Al Marri A, Aljaber T
Received 8 September 2022
Accepted for publication 18 November 2022
Published 7 December 2022 Volume 2022:13 Pages 763—774
DOI https://doi.org/10.2147/JBM.S386594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Fatema Habbash,* Wegdan Al-Bati,* Howra Al-Hashim,* Maryam Aldossari,* Ahmed Alali, Khalid Alalyani, Zainab Al-Ebrahim, Nouf Hamed, Samma Eraqe, Ziyad Binayfan, Azzam Al Marri, Thamer Aljaber
Department of Family and Community Medicine, College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Bahrain
*These authors contributed equally to this work
Correspondence: Maryam Aldossari, Tel +966 558322420, Email [email protected]
Background: Endocrinopathies and metabolic complications are common in beta thalassemia major patients receiving blood transfusions. Chelation therapy has a role in preventing or delaying such complications. However, patients may face difficulties adhering to chelation therapy for several reasons.
Aim: To evaluate endocrine complications in beta thalassemia major patients (2– 30 years) in the Eastern Province of Saudi Arabia and compare the onset of endocrine complications among compliant and noncompliant patients. Moreover, we assessed the barriers that hinder compliance with chelating therapy.
Methods: A cross-sectional study was conducted on 89 patients (43 males and 46 females) aged 2 to 30 years attending different hospitals in the Eastern Province of Saudi Arabia. A semi-structured questionnaire was used to collect demographic data and medical histories. The questionnaires were completed by face-to-face interviews with the patients or their caregivers, and the required laboratory data were retrieved from the medical records of patients.
Results: The most prevalent abnormality was underweight detected in (40.9%) of patients, followed by subclinical hypothyroidism (37.7%), short stature (35.2%), hypothyroidism in (17.0%) and diabetes mellitus in (13.6%). A significant difference between those who were compliant with iron chelation therapy and those who were not in terms of the prevalence of short stature (P value= 0.05) and hypothyroidism (P value= 0.05). The percentage of patients who were not compliant with chelation therapy was 21.6% and 9.1% of patients were not taking them at all.
Conclusion: Despite the role of chelation therapy in the management of iron overload, the risk of secondary endocrine and metabolic complications remained considerable. Subclinical hypothyroidism and short stature were the most frequent endocrine complications encountered in this study.
Keywords: iron overload, metabolic complications, hereditary blood diseases, blood transfusions
Introduction
Beta-thalassemia is a group of hereditary blood disorders characterized by anomalies in the synthesis of the beta chains of hemoglobin.1 These anomalies result in variable phenotypes ranging from severe anemia to clinically asymptomatic individuals. Beta thalassemia (“β-thal”) is classified into three forms depending on the severity of symptoms: thalassemia trait, thalassemia minor and thalassemia major. Among the three forms of thalassemia, thalassemia major is considered the most severe.2
The prevalence of beta-thalassemia is considered to be one of the highest among autosomal recessive disorders worldwide including in the Middle East. The prevalence of β-thal globally is approximately 1.5%3 and 0.05% in Saudi Arabia.4 Regarding β-thal prevalence in Saudi Arabia, there is a noticeable variance by region. The highest rates were observed in the region of Jazan, with 2% for the β-thal trait and 06% for the β-thal major. The second highest rate was reported in the eastern region with 37% for the β-thal trait and 04% for the β-thal major.5
Treatment options include transfusion along with chelation or stem cell transplantation with the latter being the only curative method with a success rate greater than 80.0%. However, due to its limited availability, transfusion along with chelation therapy becomes the common choice of management in most centers.6 Standard iron chelation therapy is based on the usage of deferoxamine. The effectiveness of this modality of treatment depends primarily on compliance with the medication.7 Deferiprone (Ferriprox) is another oral chelator that was recently approved in many countries, including the United States.8 The most common post-therapeutic complication due to iron chelation is liver fibrosis.9
Regularly observed endocrine complications in beta thalassemia patients (TM) include hypothyroidism, osteoporosis, delayed puberty, hypogonadism, short stature and failure to develop secondary sexual characteristics, with iron toxicity as the most likely cause of these complications. Delayed puberty and hypogonadism are the most common endocrine complications of iron overload respectively.8
Blood transfusion in beta thalassemia patients is mandatory to overcome and eliminate anemia, but iron overload that follows the transfusion process is the primary cause of endocrine and metabolic complications. These complications are frequently faced by TM patients, and for this reason chelation therapy is a necessity.
Several studies have suggested lack of awareness about receiving chelating therapy, especially among patients’ parents, and for that reason, awareness must be increased for a better outcome from chelation therapy.10
This study aims to assess the endocrine and metabolic complications in regularly transfused β thalassemia patients, and to study the relation of age, gender, and the compliance to iron chelation therapy to the prevalence of these complications. As well as the barriers, or reasons for not being compliant to iron chelation.
Despite the fact that, previous studies aimed to provide a better understanding of the prevalence of endocrine and metabolic complications, very few highlighted the efficiency of chelating agents in reducing these complications and the influence of different factors that affect patients’ intake and compliance with chelation.
Research Aim
- To evaluate endocrine complications that might occur in β thalassemia patients.
- To compare the onset of endocrine complications among patients who are compliant with chelation therapy and those who are not.
- To assess the barriers that hinder compliance with chelating therapy.
Materials and Methods
Data Sources
Haematology Units in public hospitals and medical centres in the Eastern Province of Saudi Arabia, including:
- Qatif Central Hospital
- King Fahad University Hospital- Al Khobar
- Hereditary Blood Disease Center- Al-Ahsa’a
- Maternity and Children Hospital- Dammam
Inclusion Criteria
Not establishing any of the above with the study population and exclusion criteria is sufficient to have the general characteristics of this study population.
Exclusion Criteria
- Patients with no medical history or no updates within one year.
- Pediatric patients who are not accompanied by their parents.
Sample size
A convenience sample of 89 patients was included in the study.
Study instrument
The tool used to collect the data was a semi-structured questionnaire. It is written in English and Arabic and contains three sections. The questionnaires were completed by face-to-face interviews with the patients or their caregivers. The first section of the questionnaire included the sociodemographic data of the child. The second section is composed of six questions to explore the history of the disease and the management received. The second section includes both open and closed-ended questions. Close-ended questions include yes/no and multiple choices with open-ended options in some of them. Endocrine abnormalities were assessed by evaluating the growth parameters, hormonal level and other laboratory data, which are included in the 3rd section of the questionnaire. Growth parameters consist of the weight, height, BMI for age and Z-score. Laboratory investigation result retrieved from the electronic files included the levels of fasting blood glucose, ferritin, serum thyroxine 3 and 4, thyroid stimulating hormone and parathyroid hormone. For participants aged 16 and above, females were asked about their menstrual history and testosterone levels were retrieved from medical records for males to assess gonadal complications. The results were considered normal or abnormal according to the World Health Organization and other international laboratory reference ranges attached in Appendix 1–3. Evidence for growth failure includes the assessment of height, body mass index for participants aged above 5 years and weight-height ratio for participants less than 5 years of age. All of these are abnormal in the event of a standard deviation less than −2. (Appendix 4–9) In addition, evidence for diabetes mellitus was based on the American Diabetes Association and World Health Organization criteria. Glucose tolerance was classified into 3 categories based on fasting blood glucose: (1) fasting blood glucose < 5.5 mmol/l was considered normal; (2) fasting blood glucose of 5.5–7 mmol/l was defined as impaired fasting glucose; and (3) fasting blood glucose ˃ 7 mmol/l warranted the diagnosis of diabetes (Appendix 1).
Evidence for the existence of primary hypothyroidism was considered when free thyroxine was less than normal ˂ 0.8 ng/dl and thyroid-stimulating hormone was greater than normal ˃ 4 mIU/l. evidence for subclinical hypothyroidism was when free thyroxine was normal at 0.8–1.8 ng/dl and thyroid stimulating hormone was greater than normal ˃ 4 mIU/l (Appendix 2 and 3).
Ethical Consideration
The research proposal was approved by the research committee of Arabian Gulf University. Additionally, approval from the Saudi Ministry of Health and the assigned hospitals was obtained.
Prior to data collection, verbal and written consent was obtained from the participants. We introduced ourselves as medical students and gave the patient an overview of the research topic and aim. Participants were informed that participation was voluntary, refusal to participate would not affect the treatment or involve any penalties, and the information would be confidential.
Statistical Analysis
The data were entered and analyzed using SPSS software version 23. Frequencies and percentages were computed for categorical variables. The mean and standard deviation were computed for quantitative variables. Cross-tabulation was performed between two categorical variables. A simple bar chart and pie chart were plotted to present a categorical variable. The chi-square test was used to determine whether there was a significant association between two categorical variables. A P-value =0.05 was considered statistically significant.
Results
The clinical data of 89 patients (43 males and 46 females) with thalassemia major were obtained from four hospitals in the Eastern Province of Saudi Arabia. Most participants were from the hereditary disease center in Al-Ahsa’a, accounting for 44.9% of the total study population. Participants ranged in age from 2 to 30 years. The mean age of the participants was 15.5 years [σ ± 8.3; CI 95%: 13.7–17.2], of which 20 males and 21 females were above 16 years of age. The majority of participants were between the ages of 11 and 20 years (37.1%) (Table 1).
 |
Table 1 Demographical Characteristics of Patients with Beta Thalassemia Major in Eastern Province of Saudi Arabia |
Most of the participants were diagnosed before the first year of life with a mean age of 1.91 years [σ ± 2.50; CI 95%: 1.34–2.48] with a minimum of 0 years and a maximum of 13 years and had started blood transfusion around the same age of diagnosis (mean age 2.12 years) [σ ± 2.72; CI 95%: 1.49–2.76]. Sixty four percent received blood transfusions once every month (Table 2).
 |
Table 2 Blood Transfusion and Chelation Therapy in the Study Population |
Information obtained from interviews with patients or their caregivers showed that 69.3% of participants were compliant with chelating agents, while 21.6% were not compliant (Figure 1).
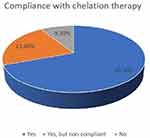 |
Figure 1 Percentage of compliance to chelation therapy among the study participants. |
Regarding receiving chelating agents, 21.6% of the study population were not compliant with taking chelating agents. At the same time (9.1%) of the same study population were not taking chelating agents at all. The main reason for non compliance was the fact that, it must be taken daily early in the morning on an empty stomach lifelong. On the other hand, the second most common reason was fearing side effects, which included nausea and vomiting (Figure 2).
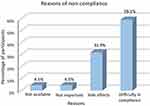 |
Figure 2 Reasons of non-compliance to chelation therapy among the study participants. |
Endocrine and metabolic complications were assessed in the study, with the most prevalent abnormalities being underweight (40.9%) followed by short stature (35.2%). Primary hypothyroidism was observed in 17.0% of participants with a mean age of 24.00 years [σ ± 7.43; CI 95%: 18.29–29.71], subclinical hypothyroidism was present in 37.7% and diabetes mellitus was observed in 13.6% of participants with a mean age of 19.56 years [σ ± 5.92; CI 95%: 15.01–24.10] (Table 3).
 |
Table 3 Prevalence of Endocrinopathies and Menstrual Abnormalities in Beta Thalassemia Major Patients in Eastern Province of Saudi Arabia |
The results of fasting blood glucose, serum T4, serum thyroid stimulating hormone (TSH), serum parathyroid (PTH) and testosterone were retrieved from the patients’ folders after interviewing the patients or their caregivers at the time of data collection, and the results showed that 25.8% of participants had impaired levels of glucose, while 10.6% had high levels. Moreover, 3.8% had T4 levels lower than normal, with 46.3% of participants having high levels of TSH. Testosterone levels for males aged 16 years or above showed that 36. %of them had low levels. Differences between the diagnosed cases and obtained serum levels could be explained by either the effect of receiving medications or failure to diagnose the cases early. Not all participants were featured in this table due to missing laboratory data from the participants’ records at the time of collection (Table 4).
 |
Table 4 Hormonal and Biochemical Tests Related to Endocrine Disorders in Beta Thalassemia Major in Eastern Province of Saudi Arabia |
The relationship between receiving chelating agents and endocrine disorders among beta thalassemia major patients in Eastern Province of Saudi Arabia was studied and showed that patients who were compliant with chelation therapy had a statistically significant lower prevalence of short stature (P value=0.05). and hypothyroidism (P value=0.05). In contrast, BMI (P value <0.289) and diabetes (P value <0.521) were poorly correlated with compliance with chelation therapy (Table 5).
 |
Table 5 Relationship Between Receiving Chelating Agents and Endocrine Disorders Among Beta Thalassemia Major Patients in Eastern Province of Saudi Arabia |
The relationship between gender and age with endocrine disorders among beta thalassemia major patients in the Eastern Province of Saudi Arabia showed that the prevalence of short stature was statistically significantly lower in females than in males (P value=0.05). Nonetheless, no significant difference was seen between males and females in the prevalence of BMI (P value <0.177), diabetes (P value <0.430) and Hypothyroidism (P value <0.146) (Table 6).
 |
Table 6 Chi-Square Test for Relationship Between Gender and Each of Height, BMI, Diabetes, and Hypothyroidism |
Moreover, Endocrine Disorders were poorly correlated to a specific age group in the study. The proportion of patients with short stature (P value <0.366), BMI (P value <0.473), diabetes (P value <0.139) and Hypothyroidism (P value <0.239) was not significantly distinctive between different age groups (Table 7).
 |
Table 7 Chi-Square Test for Relationship Between Age and Each of Height, BMI, Diabetes, and Hypothyroidism, Having Period |
Discussion
This study aims to evaluate endocrine complications that might occur in beta thalassemia patients, and the relationship between receiving chelation therapy, and the onset of these complications. The sample consisted of 89 patients, 2–30 years of age, attending hospitals in the Eastern Province of Saudi Arabia in 2019–2020. Endocrinopathies are common among beta thalassemia major patients, as has been reported by several studies.11–13 Chelation therapy has a major role in decreasing or delaying such complications. The findings of this study might help improve the quality of healthcare services provided to these patients by exploring barriers that hinder compliance with chelating therapy.
Underweight was observed less frequently in our population (40.9%), compared to other studies including a study conducted in Tehran, where the prevalence of underweight participants reached 64.2% with a positive association between patients age and BMI (P value <0.002) as opposed to our study which no significant difference was seen between different age groups (P value <0.473). Moreover, there was no significant relationship between gender and BMI in the study (P value <0.89), along with ours (P value <0.177).12 Participants were considered underweight according to The Growth Charts for Saudi Children and Adolescents endorsed by The Health Services Council of Saudi Arabia, where a BMI less than −2 standard deviations was identified as underweight.
In this study, the prevalence of short stature (35.2%) is lower compared to data from a study performed across 16 countries and reported that 53.0% were short, with a positive association between gender and short stature (P value<0.006) showing prevalence of 61.49% in males and 38.5% in females.13 While, the prevalence of short stature in our study was statistically significantly lower in females than in males (P value=0.05). Short stature was present in 29% of female patients based on the growth charts for Saudi children and adolescents compared to 71% of males in the study.
However, the prevalence of short stature in our study was higher than that reported from a study of endocrinopathies in beta-thalassemia major northwest Saudi Arabia, which was identified in 20.9% of their cohort. Along, with a positive association between age and short stature (P value<0.02) with a prevalence of 31.1% in those aged 10–28 years.11 In contrast, there was no marked association between age and short stature in this study (P value <0.366).
On the contrary, primary hypothyroidism was observed to have a higher prevalence than that reported in other studies conducted in Tehran,14 Italy15 and Northwest Saudi Arabia.11 This difference in prevalence from other countries could be explained by the difference in cut-off hormone levels and/or variation in management protocols and patient compliance between different centers. The prevalence of hypothyroidism in the study was based on participants diagnosed with hypothyroidism and participants who met the diagnostic criteria at the time of data collection.
Moreover, the rate of diabetes mellitus in this study was higher 13.6% (66.7% males, 33.3% females), than that reported in a study conducted in Tabriz, Iran (8.9%).16 In addition to that, no significant difference was seen between males and females in the prevalence of diabetes mellitus (61.1% male, 38.9% female).16
This has been suggested to be due to risk factors for diabetes, including age, increased amount of blood transfusion, serum ferritin level, compliance with iron chelating therapy, family history of diabetes and pubertal status. The prevalence of diabetes in the study was calculated based on those who had high levels of glucose at the time of data collection and those who were already diagnosed with DM.
To our knowledge, no other studies have compared receiving chelation therapy and the onset of complications. However, in this study, there was a statistically significant association between compliance with iron chelation therapy and the prevalence of some endocrine complications. Those who were compliant with chelation therapy had a lower prevalence of short stature (P value=0.05) and hypothyroidism (P value=0.05). In contrast, there was no significant difference in BMI (P value <0.289) or diabetes (P value <0.521).
Although most of the patients knew the importance of chelation therapy, some of them were non-compliant. There is a number of reasons, for patients to refuse or to not comply to iron chelation therapy, with the major reason being, that the chelation therapy is a lifelong medication that must be taken daily on an empty stomach, which is difficult to incorporate into their daily life routine. The second most common reason was fearing the side effects, which included nausea and vomiting and a minority thought it was not important or available.
When compared with a study that assessed the reasons behind patients missing chelation therapy in several countries, including Iran, India and the United States.17 It has been shown that access to the drug was the main concern in India (51.0%), which was also a common response in Iran (25.0%), which was not the major cause in our study.
In other countries, however, the most common reason for non-compliance was related to their beliefs in taking the treatment (58.0%). The second most common reason was the side effects of the treatment (42.0%).
Conclusion
Despite the role of chelation therapy in the management of iron overload, the risk of secondary endocrine and metabolic complications remains considerable. Subclinical hypothyroidism and short stature were the most frequent endocrine complications encountered in this study. Hypothyroidism, hypoparathyroidism, diabetes mellitus and hypogonadism were also detected. Evaluating patients with TM should be carried out at an early age and regularly. Patient education regarding the importance of compliance with chelation therapy since it has a role in decreasing several iron overload-related endocrine and metabolic complications is essential.
Data Sharing Statement
All relevant data are within the paper. The questionnaire used is included in (Appendix 10 and 11).
Recommendations
Endocrinopathies and metabolic complications are common beta thalassemia major patients receiving blood transfusions. Chelation therapy has a role in preventing or delaying such complications. Further longitudinal studies with a larger sample size are needed to assess such complications and evaluate the role of chelation therapy. Proper protocols and guidelines should be developed and implemented by a multidisciplinary team with the emphasis of endocrine and metabolic complication screening to improve the quality of care provided to this group of patients.
Limitations
There are a few limitations to be considered in relation to the findings of our study.
First, the initial estimate of the sample size was 200, and we aimed to conduct random sampling. However, the duration of data collection was limited to the summer in which most of the patients were away or traveling; hence they were not within easy reach. For that reason, we had a convenience sample of 89 patients.
Second, we could not attain approval from hospitals easily; for instance, one of the hospitals that was included in our protocol did not have the chance for data collection at all, making the sample size smaller; therefore, the statistical analysis remains of limited power.
In addition, the cohort is young which must have had an influence on the prevalence of age-related complications such as diabetes.
Another point to consider is the fact that many of the laboratory tests required to assess endocrinopathies were not conducted or documented in some of the centers, which made the assessment of complications challenging.
Data Sharing Statement
A semi-structured questionnaire was used to collect demographic data and medical histories. The questionnaires were completed by face-to-face interviews with the patients or their caregivers, and the required laboratory data were retrieved from the medical records of patients attending hematology clinics across four different centers in Eastern Province, Saudi Arabia.
Ethics Approval and Consent to Participate
This study complies with the declaration of Helsinki. The research and ethical committee of Arabian Gulf University approved the research. Signed written consent was obtained from all participants above the age of 18 and from the caregivers of participants who were below 18 (Appendix 12).
Consent for Publication
The authors affirm that the participants provided informed consent for publication.
Acknowledgments
Our team would like to extend its deepest appreciation and recognition to a number of individuals and organizations, to which the success and outcome of this research would not have been possible had it not been for their help and supervision. Our team would first and foremost, like to thank Dr. Fatima Ebrahim Habbash for providing us with all the information and support needed to conduct and write this research. Her constant feedback and encouragement helped us to reach our goal, to which we are indebted to her. We owe our respects to Saudi Arabia’s Ministry of Health for giving us permission to interview the patients in the mentioned hospitals. Furthermore, Dr. Muneer Albagshi the head of the department of the Hereditary Disease Centre in Al-Ahsa’a welcomed us and asked the 21 working team to cooperate with us to facilitate our data collection. We also highly appreciate the help from Dr. Abdulmohsin Aljasim, who introduced us to the facilities and services provided by the hematology department and helped us in the retrieval of the laboratory investigations that we required in our study. We also appreciate Al-Qatif Central Hospital’s administration, the nurse team, and the research department for their collaboration. In addition, we thank King Fahad University Hospital and pediatrics unit for offering us an online course on ethics and morality before interviewing the patients. A special thanks to Dr. Mona AlSaleh, consultant pediatrician at King Fahad Hospital University. Dr. Hawazen Shash, consultant pediatrician at King Fahad Hospital University. Dr. Osama AlSultan, consultant internist at King Fahad Hospital University.
Disclosure
The authors have declared that no competing interests exist. The products used for this research are commonly and predominantly used products in our area of research and country. There is absolutely no conflict of interest between the authors and producers of the products because we do not intend to use these products as an avenue for any litigation but for the advancement of knowledge. Additionally, the research was not funded by the producing company rather it was funded by the personal efforts of the authors.
References
1. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5(1). doi:10.1186/1750-1172-5-11
2. Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010;12(2):61–76. doi:10.1097/GIM.0b013e3181cd68ed
3. Colah R, Gorakshakar A, Nadkarni A. Global burden, distribution and prevention of β-thalassemias and hemoglobin E disorders. Expert Rev Hematol. 2010;3(1):103–117. doi:10.1586/ehm.09.74
4. Alsaeed ES, Farhat GN, Assiri AM, et al. Distribution of hemoglobinopathy disorders in Saudi Arabia based on data from the premarital screening and genetic counseling program, 2011–2015. J Epidemiol Glob Health. 2018;7(1). doi:10.1016/j.jegh.2017.12.001
5. Ahmad AS. Prevalence of β -thalassemia trait in premarital screening in Al-Hassa, Saudi Arabia. Ann Saudi Med. 2006;26(1):14–16. doi:10.5144/0256-4947.2006.14
6. Mohamed SY. Thalassemia major: transplantation or transfusion and chelation. Hematol Oncol Stem Cell Ther. 2017;10(4):290–298. doi:10.1016/j.hemonc.2017.05.022
7. Piga A, Roggero S, Marletto F, Sacchetti L, Longo F. Combined use of oral chelators and desferrioxamine in thalassemia. Hematology. 2005;10(Suppl 1):89–91. doi:10.1080/10245330512331389737
8. Belmont A, Kwiatkowski JL. Deferiprone for the treatment of transfusional iron overload in thalassemia. Expert Rev Hematol. 2017;10(6):493–503. doi:10.1080/17474086.2017.1318052
9. Olivieri NF, Brittenham GM, McLaren CE, et al. Long-term safety and effectiveness of iron-chelation therapy with deferiprone for thalassemia major. N Engl J Med. 1998;339(7):417–423. doi:10.1056/nejm199808133390701
10. Goyal JP, Hapani PT, Gagiya H. Prevalence of human immunodeficiency virus and hepatitis B among multi-transfused thalassemia children. J Appl Hematol. 2015;6(2):70–73. doi:10.4103/1658-5127.160204
11. Habeb AM, Al-Hawsawi ZM, Morsy MM, et al. Endocrinopathies in beta-thalassemia major. Prevalence, risk factors, and age at diagnosis in Northwest Saudi Arabia. Saudi Med J. 2013;34(1):67–73. Available from: https://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=23299162&site=eds-live.
12. Yousefian S, Aliabad GM, Saleh R, Khedmati M. Association of Body mass index and serum ferritin level in pediatrics with Beta-thalassemia major disease. Iran J Pediatr Hematol Oncol. 2022;12(1):34–40. doi:10.18502/ijpho.v12i1.8359
13. Arab-Zozani M, Kheyrandish S, Rastgar A, Miri-Moghaddam E. A systematic review and meta-analysis of stature growth complications in β-thalassemia major patients. Ann Glob Health. 2021;87(1):1–17. doi:10.5334/aogh.3184
14. Shamshirsaz AA, Bekheirnia MR, Kamgar M, et al. Metabolic and endocrinologic complications in beta-thalassemia major: a multicenter study in Tehran. BMC Endocr Disord. 2003;3:4–6. doi:10.1186/1472-6823-3-4
15. Casale M, Citarella S, Filosa A, et al. Endocrine function and bone disease during long-term chelation therapy with deferasirox in patients with β-thalassemia major. Am J Hematol. 2014;89(12):1102–1106. doi:10.1002/ajh.23844
16. Farzad N, Akbar A, Naser A, et al. A cross-sectional study of metabolic and endocrine complications in beta-thalassemia major. Ann Saudi Med. 2008;28(5):361–366. doi:10.5144/0256-4947.2008.361
17. Ward A, Caro JJ, Green TC, et al. An international survey of patients with thalassemia major and their views about sustaining life-long desferrioxamine use. BMC Clin Pharmacol. 2002;2:3. doi:10.1186/1472-6904-2-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
