Back to Journals » OncoTargets and Therapy » Volume 10
Emerging role of nivolumab in the management of patients with non-small-cell lung cancer: current data and future perspectives
Received 10 October 2016
Accepted for publication 23 March 2017
Published 24 July 2017 Volume 2017:10 Pages 3697—3708
DOI https://doi.org/10.2147/OTT.S97903
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr William C. Cho
Emily Feld, Leora Horn
Department of Internal Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
Abstract: Immune-checkpoint inhibitors have become valuable therapies in the treatment of patients with non-small-cell lung cancer (NSCLC). Recent clinical trials have shown promising results with regard to efficacy and toxicity profiles of these agents compared to cytotoxic chemotherapy. Nivolumab was one of the first immune-checkpoint inhibitors to demonstrate clinical activity in patients with NSCLC, and is currently approved in the US for treatment of patients with advanced squamous and nonsquamous NSCLC who have progressed on or after platinum-based chemotherapy. This review provides an update on nivolumab’s pharmacology, safety, and efficacy, as established by the CheckMate trials. We also discuss specific applications and strategies for the use of nivolumab in NSCLC patients, as well as predictive biomarkers and their role in treatment selection.
Keywords: nivolumab, non-small-cell lung cancer, immune-checkpoint inhibitor, PD1
Introduction
For the majority of patients with advanced non-small cell lung cancer (NSCLC), cytotoxic chemotherapy has been the mainstay of treatment for decades. First-line standard therapy for patients without an activating mutation is platinum-based chemotherapy, with or without a maintenance regimen.1 Despite initial responses to chemotherapy, the majority of patients will progress and ultimately require second-line therapy, which until recently has only included three approved agents in the US.2,3 While cytotoxic chemotherapy provides palliation and can prolong life compared to supportive care, the median overall survival (OS) for patients with metastatic disease and no actionable mutation is less than 1 year.4–6 Moreover, treatment has significant and sometimes debilitating side effects, including nausea, fatigue, and myelosuppression, often limiting use in patients with medical comorbidities.
Immune-checkpoint inhibitors are changing the landscape of treatment options for patients with NSCLC. These agents work by blocking inhibitory interactions between T cells and antigen-presenting cells or tumor cells, which normally allow malignant cells to proliferate undetected by immunosurveillance. By preventing this interaction, checkpoint inhibitors allow T cells to become activated against cancer cells.
In a subset of patients with NSCLC, checkpoint inhibitors have demonstrated more durable responses than conventional chemotherapy or targeted therapy, without the challenging side effects. Checkpoint inhibitors include agents targeting cytotoxic CTLA4, PD1, and PDL1. The PD1 inhibitor nivolumab (Opdivo, Bristol-Myers Squibb, NY, USA) is one of the most widely studied checkpoint inhibitors to date. It was the first PD1 inhibitor to demonstrate activity in NSCLC patients. As of October 2015, it was approved by the US Food and Drug Administration (FDA) for advanced squamous and nonsquamous NSCLC on or after platinum-based chemotherapy7 and approved in Europe for locally advanced or metastatic squamous or nonsquamous NSCLC after prior chemotherapy.8 This review focuses on nivolumab’s pharmacology, efficacy, safety, and application in the treatment of NSCLC patients.
Pharmacology
Mechanism of action
Within the tumor microenvironment, the inhibitory T-cell receptor PD1 engages its ligands PDL1 (or B7H1) and PDL2 (or B7DC) on tumor cells and antigen-presenting cells.9,10 PDL1 is expressed in both adenocarcinoma and squamous-cell histologies of NSCLC (50% in each subtype). Overall, studies have shown that approximately 25%–65% of patients with NSCLC harbor PDL1.11–14 The wide range of variability stems from heterogeneity within the tumor microenvironment, differing levels of expression over multiple time points, multiple immunohistochemistry (IHC)-detection assays currently in use, and the varying definitions of what constitutes PDL1 positivity. It is unclear whether PDL1 expression in NSCLC confers a survival benefit or a poor prognosis, as studies to date have demonstrated conflicting results.12–17 PDL2 expression is more limited than PDL1, and it is primarily found in macrophages and dendritic cells, suggesting that PDL2 plays a more minor role in regulating T-cell response.12,18 Expression of PDL2 in NSCLC may be associated with a poor prognosis.15
In the normal physiologic state, cytokines, including IL4, IL10, and IFN, promote interaction between PD1 and PDL1/PDL2. This interaction downregulates the body’s immune system, which is a beneficial effect to avoid unwanted inflammation or autoimmunity.19 When malignant cells harbor PDL1 and PDL2, they can elude recognition by immunosurveillance, as the interaction between PD1 and its ligands on tumor cells halts cytotoxic T-lymphocyte proliferation, survival, and activity.20,21 Nivolumab binds to the PD1 receptor on T cells, disrupting the interaction of the receptor with its ligands and promoting a state of immunoactivation. This immunoactivation remains fairly targeted, as PDL1 expression is relatively confined to the tumor microenviroment.22
Pharmacokinetics and pharmacodynamics
Nivolumab is a human IgG4 monoclonal antibody. Brahmer et al described the pharmacokinetics and pharmacodynamics of nivolumab in their Phase I study of 39 patients with various advanced malignancies. At a dose of 3 mg/kg every 2 weeks, nivolumab reached a steady state at 12 weeks and had a half-life of 12 days. The pharmacokinetics were linear, as the maximal concentration and area under the curve were proportional to the dose administered. The pharmacodynamics were evaluated by assessing PD1-receptor occupancy. At 4–24 hours, mean peak PD1-receptor occupancy was 85% and mean plateau occupancy was 72% at 57 days and beyond, demonstrating nivolumab’s high affinity for PD1, as well as its ability to produce a durable response, even when serum levels are low (Table 1).23
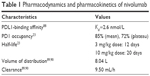  | Table 1 Pharmacodynamics and pharmacokinetics of nivolumab |
In a larger Phase I trial, Topalian et al evaluated 296 patients with advanced melanoma, NSCLC, castration-resistant prostate cancer, renal cell carcinoma, or colorectal carcinoma, and demonstrated the median time to peak concentration was 1–4 hours, also with linear pharmacokinetics. Pharmacodynamics were assessed according to PD1-receptor occupancy and after treatment with one cycle of nivolumab; median PD1-receptor occupancy was 64%–70%.24 Nivolumab is cleared by proteolytic degradation via receptor-mediated or nonspecific endocytosis in hepatic or reticuloendothelial cells.25 The clearance of nivolumab increases with greater body weight, leading initially to treatment based on weight-based dosing. Its clearance is not affected by age, sex, race, PDL1-expression levels, renal impairment, or mild hepatic impairment; however, its clearance has not been evaluated in moderate or severe hepatic impairment.7,8 Nivolumab has a low risk of drug interactions, and is not known to affect cytochrome P450 substrates.25
Efficacy
Phase I trials
The first Phase I study of nivolumab enrolled 39 patients with metastatic melanoma, colorectal carcinoma, castrate-resistant prostate carcinoma, NSCLC, or renal cell carcinoma. Six patients had NSCLC. Patients were given a single dose of nivolumab at 0.3, 1, 3, or 10 mg/kg, followed by a 15-patient expansion cohort receiving 10 mg/kg every 2 weeks. Nivolumab was tolerated well. One of the six NSCLC patients had a significant response, but not meeting partial response (PR) criteria. Overall, 12 of the 39 patients demonstrated stable disease (SD) or tumor regression. There was one durable complete response in a patient with colorectal cancer.23
Subsequently, a larger Phase I dose-escalation trial of nivolumab was conducted of 296 patients with NSCLC, melanoma, and renal cell carcinoma.24 Patients with NSCLC received nivolumab at 1, 3, or 10 mg/kg every 2 weeks in 8-week cycles for up to 12 cycles. In this cohort, the objective response rate (ORR) across all doses was 18%. Responses were durable, with 20 of 31 responses lasting longer than 1 year. Further study of 129 NSCLC patients (54% of whom received three or more prior therapies) demonstrated a difference in RR between doses: 3% for the 1 mg/kg cohort compared to 24.3% and 20.3% for the 3 mg/kg and 10 mg/kg cohort, respectively.26 Based on these data, the 3 mg/kg dose was chosen for further investigation. At 3 mg/kg (n=37), the OS rates were 56%, 42%, and 27% at 1, 2, and 3 years, respectively. The median OS was 14.9 (95% confidence interval [CI] 7.3–30.3) months. Across all doses, the median OS was 9.9 (95% CI 7.8–12.4) months. Squamous and nonsquamous histologies demonstrated similar RRs. Current and former smokers had higher RRs compared to never-smokers. Response and survival were not influenced by tumor PDL1 status (positive versus negative), although assessment of this was limited as only half the patients in this study had tumor samples available for examination, and these were archival rather than fresh samples.
Phase II and III trials
The CheckMate 063 and 017 trials led to nivolumab’s approval as second-line therapy in squamous NSCLC. CheckMate 063 was a single-arm, Phase II, open-label trial of nivolumab in 117 advanced-stage squamous-cell LC patients who had progressed on two or more prior therapies. The majority of patients (65%) received three or four prior therapies. The primary outcome was ORR, which was 14.5% (95% CI 8.7%–22.2%), with a median time to response of 3.3 months. The median duration of response was not reached. OS at 1 year was 39% (95% CI 30%–48%), a significant improvement over historical controls, with an estimated 1-year survival rate of 6%–18% for patients with advanced squamous-cell NSCLC. At 18 months, OS remained high – 27%.27 Benefit was seen regardless of PDL1 expression.28
Comparison of nivolumab to standard therapy with docetaxel was done in CheckMate 017, an open-label randomized Phase III trial of 272 previously treated patients with squamous NSCLC after progression on one prior platinum regimen. The trial met its primary end point of improved median OS of 9.2 (95% CI 7.3–13.3) months in the nivolumab arm compared to 6.2 (95% CI 5.1–7.3) months in the docetaxel arm. The 1-year survival nearly doubled with nivolumab compared to docetaxel: 42% (95% CI 34%–50%) compared to 24% (95% CI 17%–31%), respectively. At 18 months, this benefit was maintained, with survival of 28% and 13%, respectively, as well as at 2 years, with survival of 23% and 8%, respectively. The ORR with nivolumab was 20% (95% CI 14%–28%), more than double that of docetaxel (ORR 9%, 95% CI 5%–15%).29–31
For patients with nonsquamous NSCLC, the phase III CheckMate 057 trial randomized 582 patients who had failed platinum-based chemotherapy or tyrosine kinase-inhibitor therapy (if EGFR- or ALK-positive tumors) to receive nivolumab or docetaxel. The primary end point of improved median OS was met: 12.2 months with nivolumab (95% CI 9.7–15 months) versus 9.4 months with docetaxel (95% CI 8.1–10.7 months). Survival rates at 1 year and 18 months were 51% (95% CI 45%–56%) and 39% (95% CI 34%–45%) for nivolumab versus 39% (95% CI 33%–45%) and 23% (95% CI 19%–28%) for docetaxel, respectively (1-year hazard ratio 0.73, 95% CI 0.59–0.89; 18-month hazard ratio 0.72, 95% CI 0.6–0.88).32 At 2 years, responses remained durable, with OS of 29% for nivolumab and 16% for docetaxel.31 The ORR was 19% for nivolumab versus 12% for docetaxel. Despite this, nivolumab was not associated with a longer progression-free survival (PFS; median of 2.3 months for nivolumab and 4.2 months for docetaxel, hazard ratio 0.92).32
With interest in PDL1 as a potential predictive biomarker, the CheckMate 063, 017, and 057 trials included an analysis of the prognostic implications of PDL1 positivity. In the CheckMate 063 trial, PR rates were higher in those with more than 5% of cells positive for PDL1 by immunohistochemical assay compared to individuals with less than 5% positivity (24% versus 14%). However, some PDL1-negative patients still demonstrated response to nivolumab (ten of 31 patients with <1% PDL1 positivity had either PR or SD). In the CheckMate 017 trial, greater levels of PDL1 expression had little correlation with improved outcomes (expression levels at ≥1%, ≥5%, and ≥10% were evaluated), suggesting that PDL1 may not reliably predict response to PD1 therapy.28,30 Other research has also highlighted that PD1 therapy can still be beneficial in PDL1 negative patients.33 In the CheckMate 057 trial, however, a higher ORR and improved OS were found in patients with greater levels of PDL1 expression.32 OS at 2 years for nivolumab-treated patients by PDL1 expression was 37% with ≥1% PDL1 expression, 44% with ≥5% PDL1 expression, and 45% with ≥10% PDL1 expression compared to 13%–18% in patients considered to be PDL1-negative.31 This trial allowed archival tissue and did not require new tissue biopsy for evaluation of PDL1 positivity, which some might argue could skew the results. However, archival and fresh tissue seem to correlate fairly well with regard to levels of PDL1 expression.34
Nivolumab in the first-line setting
Currently, nivolumab is not approved for use in the first-line setting. The CheckMate 012 trial evaluated nivolumab 3 mg/kg every 2 weeks as initial monotherapy for squamous and nonsquamous NSCLC.35 Of 52 patients, the ORR was 23%, with 8% demonstrating a complete response. ORR was higher in PDL1-positive patients. Patients expressing ≥50% PDL1 had an ORR of 50% compared to 14% for those expressing <1%.36 At 1 year, OS is 73%. The CheckMate 026 trial did not meet its primary end point of improved PFS when comparing nivolumab to platinum-based chemotherapy in treatment-naïve patients with stage IV NSCLC and PDL1 expression in ≥5% of tumor cells. Among 423 patients, PFS was 4.2 months with nivolumab and 5.9 months with chemotherapy. OS was 14.4 months for nivolumab compared with 13.2 months for chemotherapy.37 Notably, 60.4% of patients in the chemotherapy arm crossed over to receive nivolumab subsequently.
Combination therapy
As nivolumab has demonstrated improved survival and toxicity profiles compared to standard chemotherapy, the efficacy and safety of checkpoint-inhibitor combinations has been investigated. Encouraging results have been seen when nivolumab was combined with ipilimumab (Yervoy, Bristol-Myers Squibb, NY, USA) in patients with metastatic melanoma, where nivolumab plus ipilimumab demonstrated a greater ORR (61% vs 11%) and PFS (not yet reached vs 4.4%) than ipilimumab alone, albeit with more toxicities in the combination arm.38
In lung cancer, a multiarm Phase I study of 148 patients investigated combination nivolumab plus ipilimumab in the first-line setting.39 Four dose schedules of these agents were administered: nivolumab 1 mg/kg every 3 weeks plus ipilimumab 1 mg/kg every 3 weeks followed by nivolumab 3 mg/kg every 2 weeks; nivolumab 1 mg/kg every 2 weeks plus ipilimumab 1 mg/kg every 6 weeks; nivolumab 3 mg/kg every 2 weeks plus ipilimumab 1 mg/kg every 12 weeks; and nivolumab 3 mg/kg every 2 weeks plus ipilimumab 1 mg/kg every 6 weeks. The cohorts receiving nivolumab 3 mg/kg every 2 weeks had the highest ORR. The ORR was 39% when combined with ipilimumab every 12 weeks versus 31% when combined with ipilimumab every 6 weeks. Median PFS was 8 months versus 8.3 months for these two groups, respectively.36 Patients with greater PDL1 expression demonstrated superior ORR. ORR with ≥50% PDL1 expression was 100% for patients treated with nivolumab 3 mg/kg every 2 weeks with ipilimumab 1 mg/kg every 12 weeks. The ORR for patients with ≥1% PDL1 expression was 57%. Similarly, patients treated with nivolumab 3 mg/kg every 2 weeks plus ipilimumab 1 mg/kg for 6 weeks demonstrated an ORR of 86% with ≥50% PDL1 expression and an ORR of 57% with ≥1% PDL1 expression.36
For patients with EGFR-mutant NSCLC, nivolumab has been combined with erlotinib in the first-line setting in a study of 21 patients. Although the study included a limited number of patients (and one patient was EGFR tyrosine kinase-naïve), three patients attained PR and nine patients had SD. The ORR was 19%, and the 24-week PFS rate was 51%.40
Investigation in the first-line setting for patients with stage IV or recurrent NSCLC continues with CheckMate 227, a Phase III trial of nivolumab alone versus nivolumab plus ipilimumab versus nivolumab plus platinum-based chemotherapy versus platinum-based chemotherapy. The primary end points are OS and PFS (NCT02477826).
Additional combinations of nivolumab with cytotoxic chemotherapy are also being investigated. This is of particular interest, as cytotoxic chemotherapy can modulate immunoresponse to tumors through a variety of mechanisms,41–44 potentially creating a favorable synergism when combined with checkpoint inhibitors. One arm of the CheckMate 012 trial investigated nivolumab plus platinum-based doublet chemotherapy (cisplatin–gemcitabine, pemetrexed–cisplatin, or paclitaxel–carboplatin) in 56 chemotherapy-naïve patients. The ORR was 33%–47%, 24-week PFS 36%–71%, and 1-year OS 59%–87%.45
Table 2 outlines many of the aforementioned major clinical trials of nivolumab, with comparisons of ORR, median PFS, median OS, and toxicities. Table 3 highlights ongoing trials to date.
  | Table 3 Selected ongoing trials of nivolumab |
Toxicity
Owing to its mechanism of action involving T-cell activation and upregulation of immunoresponse, nivolumab has the potential to cause autoimmune-like toxicities. Nonspecific T-cell activation can lead to loss of self-tolerance and reactivity against normal tissue, resulting in elevated levels of CD4 T-helper cell cytokines or increased migration of CD8 T-cells into normal tissues. Dermatologic toxicities, hepatitis, and endocrinopathies are among the most frequent immunorelated adverse events (irAEs) observed from nivolumab. Pneumonitis is rare, but one of the most severe irAEs.46 Several other rare irAEs that may occur with PD1 inhibitors include Guillain–Barré syndrome, myasthenia gravis, and encephalitis.32,47,48 There are also case reports of PD1 inhibitors triggering type I diabetes, both in genetically predisposed adults and de novo.49–51
The timing of irAEs is variable, ranging from several days after the first dose to after discontinuation of therapy. The mean time to onset is 6–12 weeks after treatment initiation.47 Early toxicities are more frequently rash and colitis (although colitis on the whole is less common with nivolumab compared to ipilimumab),52 appearing as early as 4–5 weeks.47 Hepatitis and endocrinopathies generally present later, closer to weeks 12–24.47
In the Phase I trial conducted by Topalian et al,24 the most common side effects of nivolumab were fatigue (24%), decreased appetite (12%), and diarrhea (10%). Grade 3–4 treatment-related AEs were observed in 14% of patients. Three treatment-related deaths occurred, related to pneumonitis.24,26 In the CheckMate 063 trial, the most frequently observed toxicities were fatigue (33%), decreased appetite (19%), nausea (15%), weakness (12%), rash (11%), and diarrhea (10%). The most common grade 3–4 AEs were fatigue (4%), pneumonitis (3%), and diarrhea (3%). More than 25% of patients had dose delays due to toxicity, 74% of patients experienced toxicity of any grade, and 17% experienced a grade 3 or 4 AE. Two treatment-related deaths occurred from pneumonia and ischemic stroke.28 Similar rates of AEs were observed in the CheckMate 057 trial.32 No treatment-related deaths occurred. While this study, like most of the CheckMate trials, included only patients with Eastern Cooperative Oncology Group (ECOG) performance status of 0–1, it appears that patients with an ECOG performance status of 2 may have similar rates of AEs. This is supported by the ongoing CheckMate 153 trial, where 8% of patients have an ECOG performance status of 2 and AEs are similar to those, with a performance status of 0–1.53 The comparison of nivolumab and docetaxel in the CheckMate 017 trial demonstrated higher rates of grade 3–4 AEs in the docetaxel group: 58% compared to 8% of patients receiving nivolumab. Ten percent of patients discontinued treatment due to AEs related to docetaxel compared to 5% of patients in the nivolumab arm.29 Pneumonitis was seen in 5% of patients treated with nivolumab, but only 1% were classified as grade 3 or higher.30
Notwithstanding the prevalence of irAEs with nivolumab, the majority of these AEs are only grade 1 or 2.23,24,28,54 Most toxicities are reversible by stopping therapy and initiating corticosteroids.55,56 Therefore, one of the major benefits of nivolumab compared to traditional cytotoxic chemotherapy is its more favorable side-effect profile.
Compared to anti-CTLA4 therapy, PD1 and PDL1 agents appear to have more tumor-specific activity and produce fewer immune-related AEs.57,58 Interestingly, irAEs associated with CTLA4 blockade become more frequent with increasing doses, whereas irAEs associated with PD1 blockade do not appear to be dose-related. Grade 3–4 diarrhea and colitis are more common in patients treated with CTLA4 inhibitors (10%)59 than in patients treated with PD1 inhibitors (1%–2%).24,60 Transaminitis is also more common with anti-CTLA4 agents than with PD1 inhibition.47 Nivolumab does have higher rates of pneumonitis compared to anti-CTLA4 therapy, which can be particularly challenging when it is used in the treatment of LC, where pneumonitis can be difficult to distinguish from tumor progression or inflammatory response (pseudoprogression).
While there may be potential for increased efficacy with combinations of checkpoint inhibitors, this must be balanced by the potential for increased toxicity. In the CheckMate 012 trial, grade 3–4 AEs were reported in 28%–35% of patients across the four cohorts. AEs leading to treatment discontinuation occurred in 5%–13% across the cohorts, with the lowest rates of discontinuation in those treated with ipilimumab at less frequent intervals (every 6 weeks or every 12 weeks).36
Combinations of chemotherapy and nivolumab have also shown higher rates of grade 3–4 AEs. In the CheckMate 012 cohort combining nivolumab with platinum-based doublet chemotherapy, the rate of grade 3–4 AEs was 45%, with the commonest toxicities being pneumonitis (7%), fatigue (5%), and acute renal failure (5%).45 In the nivolumab-plus-erlotinib arm of CheckMate 012, AEs were observed in all 21 participants, although only 24% were grade 3 or higher. Two patients discontinued treatment due to AEs.40
Application of nivolumab in NSCLC treatment
As mentioned previously, nivolumab is approved for advanced squamous and nonsquamous NSCLC on or after platinum-based chemotherapy. According to US National Comprehensive Cancer Network guidelines, nivolumab and pembrolizumab are the preferred agents for treatment of patients with advanced NSCLC without sensitizing EGFR mutations or ALK translocations who have an ECOG performance status of 0–2 and progression following first-line therapy with platinum-based doublet chemotherapy or bevacizumab plus chemotherapy.61 In contrast to pembrolizumab, nivolumab is approved irrespective of PDL1 expression, although a companion diagnostic is FDA-approved for nonsquamous NSCLC patients. Pembrolizumab is approved only for PDL1-positive pretreated patients (with PDL1 positivity defined as a tumor-proportion score of ≥50% using the FDA-approved companion diagnostic test).
Dosing
The recommended dose of nivolumab was 3 mg/kg by intravenous infusion over 60 minutes every 2 weeks, but has recently moved to a fixed-dosing schedule of 240 mg at each infusion. This is in contrast to pembrolizumab, which requires less frequent administration at a dose of 200 mg over 30 minutes every 3 weeks. Neither of these drugs needs adjustment for renal or hepatic impairment, unless impairment is secondary to immunomediated nephritis or hepatitis. Treatment at this time should be continued until disease progression or unacceptable toxicity, although studies are ongoing evaluating the optimal duration of therapy.
Comparison with other PD1 and PDL1 agents
No direct comparison of nivolumab with other PD1 or PDL1 inhibitors has been conducted; however, from current trial results, nivolumab appears to have similar efficacy and toxicity compared to these other agents. Pembrolizumab has an ORR of 15%–24%.62 The PDL1 inhibitors atezolizumab and durvalumab have ORRs of 23% and 14%, respectively.63,64 All of the PD1 and PDL1 agents are similarly tolerated, with grade 3–4 AEs approximately 15% or less.62–66 Given their similarities, the choice of PD1 or PDL1 inhibitor depends largely on FDA approval, PDL1 status (if pembrolizumab is to be used), and provider preference. At this time, all agents are priced equally, although with time and more agents becoming available, hopefully that will change.
The role of PDL1 as a biomarker
Not all patients with NSCLC will respond to nivolumab. To date, there is no established biomarker that predicts whether a patient will have a favorable outcome. Level of PDL1 expression on tumor cells by IHC is a promising potential predictor of response to anti-PD1/PDL1 therapy, although the role of PDL1 testing in terms of treatment decision making is still being clarified. Many of the trials presented herein suggest superior clinical responses with PD1 inhibitors in those with PDL1-expressing tumors. This was further supported by a 2016 pooled analysis of 914 patients, where the ORR was higher for patients with PDL1-positive tumors (IHC cutoff >1%, odds ratio 2.44, 95% CI 1.61–3.68).67 However, the relationship between PDL1 expression and response is not linear, as individuals with low levels of expression also respond to treatment, with RRs as high as 15%. When deciding who should receive PD1/PDL1 therapy, this inconsistency in response makes PDL1 an especially challenging biomarker.
The high degree of variability in PDL1 expression within the tumor microenvironment makes it an imperfect biomarker. Poor correlation between PDL1 expression on lung biopsies and resected tumors suggests significant intratumor heterogeneity.68,69 Furthermore, different levels of expression exist comparing primary versus metastatic lesions, as well as tumor cells, immune cells, and stromal cells. This intratumor heterogeneity is influenced by a variety of intrinsic and extrinsic factors, including local tissue hypoxia, underlying tumor genetics, and prior chemotherapies. Illustrating this heterogeneity is a study of 73 cases of NSCLC patients with metastatic brain lesions. When disease sites in the lung and brain were compared, tumor PDL1 expression differed in 14% of cases and tumor-infiltrating lymphocyte PDL1 expression differed in 26% of cases. In the majority of these spatially discordant cases, there was greater expression of PDL1 in primary LCs than the associated brain metastases. Furthermore, most lesions with varying tumor-cell PDL1 expression were evaluated 6 months or more apart, indicating the possibility of temporal heterogeneity as well.70 The mechanism underlying PDL1 expression is also variable, occurring either in the form of constitutive oncogene activation or dynamic IFNγ-induced expression. The latter is more common, and results in high levels of PDL1 at T-cell-rich sites, often at the invasive margin of tumors.71
Methodological issues further limit the reliable use of PDL1 as a biomarker. Currently, multiple detection PDL1 IHC antibodies are in use, and several different companion diagnostics exist. Recently, several PDL1 IHC assays have been compared for concordance, and found similar rates of staining for PDL1-positive tumor cells across assays 22C3, 28-8, and SP263.72,73 However, in one analysis, assay SP142 had fewer tumor cells stained compared to the others. All assays had greater variability on immune-cell staining than tumor-cell staining.72 Complicating standardization, there is no consensus definition for PDL1 positivity, with IHC cutoff points ranging from 1% to 50%. Without uniform procedures for PDL1 detection, it not only becomes challenging to interpret outcomes but also to make decisions about who should receive treatment.
Patient population
Patients with autoimmune conditions have been excluded from clinical trials of checkpoint inhibitors, so the safety and efficacy of therapy is unknown in this population. Case reports have documented several of these patients who have tolerated checkpoint inhibitors, although these have been with ipilimumab in patients with melanoma, rather than with nivolumab for NSCLC.74,75 However, there have also been reports of therapy exacerbating patients’ underlying autoimmune disease.76,77 Given the lack of data in this cohort of patients with autoimmune disease, decisions about treatment need to be made on an individual basis.
Patients on systemic corticosteroids or other immunosuppressants have been excluded from trials of checkpoint inhibitors as well. Theoretically, these immunosuppressive agents will diminish the effect of checkpoint inhibitors. Therefore, patients on supraphysiological doses of corticosteroids may not suitable candidates for checkpoint inhibitors, although studies in this population are lacking.78 Individuals on low-dose steroids are likely still appropriate for treatment. It also appears that even at doses of corticosteroids used to treat irAEs, checkpoint inhibition is still effective and can likely be continued in this population.79
Monitoring disease progression
Tumor evaluation assessed by computed tomography is recommended every 2 months. Assessment of response to treatment with immunotherapy presents unique challenges compared to traditional cytotoxic chemotherapy. By activating the immune system, checkpoint inhibitors induce lymphocyte infiltration into the tumor environment, leading to inflammation, which can appear as increased tumor burden by Response Evaluation Criteria in Solid Tumors (RECIST) criteria on imaging. This phenomenon has been referred to as “pseudoprogression”. Therefore, clinicians must be cautious with their interpretation of initial imaging, as the appearance of increased disease may not be true progression. Immunorelated response criteria (irRC) have been developed to characterize responses to immunotherapy better. With these criteria, the emphasis is on overall tumor burden, rather than reliance on dimensions of index lesions alone. Furthermore, documentation of progressive disease requires more than one assessment. For example, progressive disease is defined in RECIST as ≥20% relative increase in the sum of diameters of target lesions (with an absolute increase ≥5 mm) or the appearance of at least one new lesion,80 whereas irRC define progressive disease as an increase in tumor burden ≥25% in two consecutive assessments ≥4 weeks apart.81
A comparison of RECIST and irRC was done in 411 patients receiving pembrolizumab for melanoma.82 A total of 51 patients were classified as having progressive disease by RECIST, but complete response, PR, or SD by irRC, which translates to an underestimation of response in 12% of patients. Despite this, irRC have not yet been fully validated and accepted in clinical practice, and current trials of checkpoint inhibitors still rely on RECIST.81
Monitoring toxicity
In addition to having their response and disease progression monitored, patients should be monitored closely for toxicities, which can occur at any time during the course of treatment. This includes baseline thyroid-function studies, complete blood count, and complete metabolic panel, and then at each treatment and every 6–12 weeks for the first 6 months after treatment is stopped.47 Symptoms of severe fatigue should prompt consideration of checking adrenocorticotropic hormone, cortisol, and testosterone levels (in males). Patients with pneumonitis represent a particular challenge, as described previously. Presenting symptoms include dyspnea, sputum production, fever, and/or hemoptysis, and any of these symptoms warrants evaluation with computed tomography of the chest.23,24,47,52 Chest X-ray often demonstrates diffuse bilateral infiltrates, which correspond to lymphocytes on bronchoscopic evaluation.
Immunorelated AEs are typically reversible with early detection and initiation of treatment. Dose reductions are not recommended. Supporting this, in the initial trial conducted by Brahmer et al, there was no maximum tolerated dose across the 0.3, 1, 3, or 10mg/kg doses and the percentage of patients with any grade AE or grade 3–4 AEs was similar across the 1–10mg/kg doses.23 This is in contrast to CTLA4 inhibitors, where there is dose-dependent toxicity.
Grade 1 toxicities are typically managed symptomatically, and do not require discontinuation of therapy. For grade 2 toxicities, treatment should be discontinued, and symptoms usually resolve with this intervention alone. If the patient’s symptoms do not improve in 1 week or if they initially present with a grade 3–4 AE, corticosteroids should also be initiated. For grade 2 toxicities requiring corticosteroids, a dose of 0.5 mg/kg/day of prednisone is recommended.47 For high-grade toxicities, patients should be started on prednisone 1–2 mg/kg/day, which can be tapered slowly once their clinical status improves. For patients who are refractory to corticosteroids and particularly those with refractory colitis, infliximab 5 mg/kg has been shown to be helpful.83 Of note, patients treated with corticosteroids for pneumonitis can have a prolonged recovery period, and improvement in radiographic findings typically lags behind clinical improvement.47
Future perspectives
Nivolumab is a good treatment option as second-line therapy in patients with advanced squamous and nonsquamous NSCLC; however, many questions remain with regard to its use. There is uncertainty regarding the most effective duration of therapy, safety and effectiveness of retreatment in select patient populations, the sequence of therapy in relation to chemotherapy, the appropriate combinations (with chemotherapy, targeted therapy, or combining anti-PD1 and anti-CTLA therapies), and the safety of these agents with radiation, given the rare but life-threatening risk of pneumonitis. While the toxicity profile of nivolumab is well established as to the time of treatment, long-term side effects remain unknown. The CheckMate 153 trial aims to elucidate the potential of long-term toxicities up to 6.5 years on from therapy with nivolumab (NCT02066636).
While the aforementioned trials highlight encouraging RRs for nivolumab, even greater responses may be attainable with further study. One way to achieve this may be with combination therapy with other immunotherapy, chemotherapy, targeted therapy, and/or radiation. Many of these combinations have already demonstrated encouraging synergistic effects. An additional combinatorial approach involves using immunotherapy and angiogenesis inhibitors, which has already shown promising results in renal cell carcinoma.84 VEGF has the ability to modulate the function of T cells and stroma in the tumor microenvironment, leading to an immunosuppressive state.85 This can then prime cells for a heightened response to PD1/PDL1 therapy, and thus deserves further investigation in combination with immunotherapy. Another strategy to improve RRs lies in knowing which patients will have the best response to therapy and establishing a personalized treatment plan. To date, we have not yet identified a biomarker capable of making this distinction. PDL1 has been the most researched biomarker thus far; however, there are multiple factors precluding its widespread, reliable use. Other than PDL1 status, smoking history has some potential as a biomarker, due to the observation in several studies that many smokers have higher RRs.24,86 High mutation burden has also been correlated with improved RRs.87
Conclusion
Nivolumab has expanded treatment options and prognosis for a cohort of pretreated NSCLC patients, demonstrating encouraging results as both single-agent therapy and in combination with other therapies. It has shown superior efficacy compared to docetaxel, and responses appear durable even beyond cessation of treatment. Compared to cytotoxic chemotherapy, toxicities of nivolumab are generally more acceptable and manageable. Combination therapy with other checkpoint inhibitors has resulted in higher RRs than monotherapy, although with more frequent AEs. With additional clinical trials under way, it is expected that there will continue to be increasing roles for nivolumab in the treatment of NSCLC patients.
Disclosure
LH consults for AbbVie, Lilly, Genentech, Merck, Bristol-Myers Squibb, Boehringer Ingelheim, Xcovery, and EMD Serono. EF reports no conflicts of interest in this work.
References
Leighl NB. Treatment paradigms for patients with metastatic non-small-cell lung cancer: first-, second-, and third-line. Curr Oncol. 2012;19 (Suppl 1):S52–S58. | ||
Hanna N, Shepherd FA, Fossella FV, et al. Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated with chemotherapy. J Clin Oncol. 2004;22(9):1589–1597. | ||
Shepherd FA, Pereira JR, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353(2):123–132. | ||
Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346(2):92–98. | ||
Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26(21):3543–3551. | ||
Delbaldo C, Michiels S, Syz N, Soria JC, Le Chevalier T, Pignon JP. Benefits of adding a drug to a single-agent or a 2-agent chemotherapy regimen in advanced non-small-cell lung cancer: a meta-analysis. JAMA. 2004;292(4):470–484. | ||
Opdivo (nivolumab) injection for intravenous use [prescribing information]. New York: Bristol-Myers Squibb; 2015. | ||
European Medicines Agency. Opdivo (nivolumab) [EU summary of product characteristics]. 2016. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003985/WC500189765.pdf. Accessed May 29, 2016. | ||
Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366(26):2517–2519. | ||
Topalian SL, Drake CG, Pardoll DM. Targeting the PD-1/B7-H1(PD-L1) pathway to activate anti-tumor immunity. Curr Opin Immunol. 2012;24(2):207–212. | ||
Konishi J, Yamazaki K, Azuma M, Kinoshita I, Dosaka-Akita H, Nishimura M. B7-H1 expression on non-small cell lung cancer cells and its relationship with tumor-infiltrating lymphocytes and their PD-1 expression. Clin Cancer Res. 2004;10(15):5094–5100. | ||
Chen YB, Mu CY, Huang JA. Clinical significance of programmed death-1 ligand-1 expression in patients with non-small cell lung cancer: a 5-year-follow-up study. Tumori. 2012;98(6):751–755. | ||
Boland JM, Kwon ED, Harrington SM, et al. Tumor B7-H1 and B7-H3 expression in squamous cell carcinoma of the lung. Clin Lung Cancer. 2013;14(2):157–163. | ||
Yang CY, Lin MW, Chang YL, Wu CT, Yang PC. Programmed cell death-ligand 1 expression in surgically resected stage I pulmonary adenocarcinoma and its correlation with driver mutations and clinical outcomes. Eur J Cancer. 2014;50(7):1361–1369. | ||
Zhang Y, Wang L, Li Y, et al. Protein expression of programmed death 1 ligand 1 and ligand 2 independently predict poor prognosis in surgically resected lung adenocarcinoma. Onco Targets Ther. 2014;7:567–573. | ||
Azuma K, Ota K, Kawahara A, et al. Association of PD-L1 overexpression with activating EGFR mutations in surgically resected nonsmall-cell lung cancer. Ann Oncol. 2014;25(10):1935–1940. | ||
Velcheti V, Schalper KA, Carvajal DE, et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Invest. 2014;94(1):107–116. | ||
Rozali EN, Hato SV, Robinson BW, Lake RA, Lesterhuis WJ. Programmed death ligand 2 in cancer-induced immune suppression. Clin Dev Immunol. 2012;2012:656340. | ||
Freeman GJ, Long AJ, Iwai Y, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192(7):1027–1034. | ||
Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8(6):467–477. | ||
Dong H, Strome SE, Salomao DR, et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8(8):793–800. | ||
Brahmer JR, Pardoll DM. Immune checkpoint inhibitors: making immunotherapy a reality for the treatment of lung cancer. Cancer Immunol Res. 2013;1(2):85–91. | ||
Brahmer JR, Drake CG, Wollner I, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28(19):3167–3175. | ||
Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. | ||
Passey C, Simon J, Hong Q, Roy A, Agrawal S. Assessment of drug interaction potential by nivolumab using cytokine modulation data. Clin Pharm Ther. 2015;97 (Suppl 1):S96. | ||
Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004–2012. | ||
Horn L, Rizvi N, Mazieres D, et al. Longer-term follow-up of a phase 2 study (CheckMate 063) of nivolumab in patients with advanced, refractory squamous non-small cell lung cancer. J Thorac Oncol. 2015;10 (Suppl 2):S175. | ||
Rizvi NA, Mazières J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257–265. | ||
Reckamp K, Spigel D, Rizvi N. Phase 3 randomized trial (CheckMate 017) of nivolumab vs docetaxel in advanced squamous cell non-small cell lung cancer. Poster presented at: 16th World Conference on Lung Cancer; September 6–9, 2015; Denver, CO. | ||
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. | ||
Borghaei H, Brahmer JR, Horn L. Nivolumab vs docetaxel in patients with advanced NSCLC: CheckMate 017/057 2-y update and exploratory cytokine profile analyses. J Clin Oncol. 2016;34 Suppl:9025. | ||
Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–1639. | ||
Schmidt LH, Kümmel A, Görlich D, et al. PD-1 and PD-L1 expression in NSCLC indicate a favorable prognosis in defined subgroups. PLoS One. 2015;10(8):e0136023. | ||
Taube JM, Klein A, Brahmer JR, et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res. 2014;20(19):5064–5074. | ||
Gettinger S, Hellman M, Shepherd F. First-line monotherapy with nivolumab (NIVO; anti-programmed death-1 [PD-1]) in advanced non-small cell lung cancer (NSCLC): safety, efficacy and correlation of outcomes with PD-1 ligand (PD-L1) expression. J Clin Oncol. 2015;33 Suppl:8025. | ||
Hellmann MD, Gettinger SN, Goldman JW. CheckMate 012: safety and efficacy of first-line nivolumab and ipilimumab in advanced NSCLC. J Clin Oncol. 2016;34 Suppl:3001. | ||
Socinski M, Creelan B, Horn L, et al. NSCLC, metastatic CheckMate 026: a phase 3 trial of nivolumab vs investigator’s choice (IC) of platinum-based doublet chemotherapy (PT-DC) as first-line therapy for stage iv/recurrent programmed death ligand 1 (PD-L1)-positive NSCLC. Ann Oncol. 2016;27 (Suppl 6):LBA7. | ||
Postow MA, Chesney J, Pavlick AC, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015;372(21):2006–2017. | ||
Rizvi N, Gettinger S, Goldman J. Safety and efficacy of first-line nivolumab and ipilimumab in non-small cell lung cancer. J Thoracic Oncol. 2015;10(9 Suppl 2):S176. | ||
Gettinger S, Chow LQ, Borghaei H, et al. Safety and response with nivolumab (anti-PD-1; BMS-936558, ONO-4538) plus erlotinib in patients (Pts) with epidermal growth factor receptor mutant (EGFR MT) advanced non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys. 2014;90(5):S34–S35. | ||
Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic cell death in cancer therapy. Annu Rev Immunol. 2013;31:51–72. | ||
Liu WM, Fowler DW, Smith P, Dalgleish AG. Pre-treatment with chemotherapy can enhance the antigenicity and immunogenicity of tumours by promoting adaptive immune responses. Br J Cancer. 2010;102(1):115–123. | ||
Ghiringhelli F, Menard C, Puig PE, et al. Metronomic cyclophosphamide regimen selectively depletes CD4+CD25+ regulatory T cells and restores T and NK effector functions in end stage cancer patients. Cancer Immunol Immunother. 2007;56(5):641–648. | ||
Zhang L, Dermawan K, Jin M, et al. Differential impairment of regulatory T cells rather than effector T cells by paclitaxel-based chemotherapy. Clin Immunol. 2008;129(2):219–229. | ||
Antonia SJ, Brahmer JR, Gettinger S, et al. Nivolumab (anti-PD-1; BMS-936558, ONO-4538) in combination with platinum-based doublet chemotherapy (PT-DC) in advanced non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys. 2014;90(5):S2. | ||
Langer CJ. Emerging immunotherapies in the treatment of non-small cell lung cancer (NSCLC): the role of immune checkpoint inhibitors. Am J Clin Oncol. 2015;38(4):422–430. | ||
Weber JS, Yang JC, Atkins MB, Disis ML. Toxicities of immunotherapy for the practitioner. J Clin Oncol. 2015;33(18):2092–2099. | ||
Antonia S, Bendell J, Taylor M. Phase I/II study of nivolumab with or without ipilimumab for treatment of recurrent small cell lung cancer (SCLC): CA209-032. J Clin Oncol. 2015;33 Suppl:7503. | ||
Martin-Liberal J, Furness AJ, Joshi K, Peggs KS, Quezada SA, Larkin J. Anti-programmed cell death-1 therapy and insulin-dependent diabetes: a case report. Cancer Immunol Immunother. 2015;64(6):765–767. | ||
Hughes J, Vudattu N, Sznol M, et al. Precipitation of autoimmune diabetes with anti-PD-1 immunotherapy. Diabetes Care. 2015;38(4):e55–e57. | ||
Okamoto M, Gotoh K, Masaki T, et al. Fulminant type 1 diabetes mellitus with anti-programmed cell death-1 therapy. J Diabetes Investig. 2016;7(6):915–918. | ||
Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311–4318. | ||
Hussein M, McCleod M, Chandler J, et al. Safety and efficacy of nivolumab in an ongoing trial of a PD-L1 patient population with metastatic non-small cell lung cancer. J Thorac Oncol. 2015;10(9 Suppl 2):S175. | ||
Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–2465. | ||
Scarpace SL. Metastatic squamous cell non-small-cell lung cancer (NSCLC): disrupting the drug treatment paradigm with immunotherapies. Drugs Context. 2015;4:212289. | ||
Weber JS, Kahler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30(21):2691–2697. | ||
Postow MA, Callahan MK, Wolchok JD. Immune checkpoint blockade in cancer therapy. J Clin Oncol. 2015;33(17):1974–1982. | ||
Chow LQ. Exploring novel immune-related toxicities and endpoints with immune-checkpoint inhibitors in non-small cell lung cancer. Am Soc Clin Oncol Educ Book. 2013;33:e280. | ||
Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. | ||
Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–144. | ||
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): non-small cell lung cancer (version 4.2016). 2016. Available from: http://www.vitromolecularlaboratories.com/wp-content/uploads/2016/07/NCCN-Clinical-Practice-Guidelines-in-Oncology-NCCN-Guidelines%C2%AE.pdf. Accessed March 29, 2017. | ||
Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–2028. | ||
Soria J, Cruz C, Bahleda R. Clinical activity, safety and biomarkers of PD-L1 blockade in non-small cell lung cancer (NSCLC): additional analyses from a clinical study of the engineered antibody MPDL3280A (anti-PDL1). Eur J Cancer. 2013;49 Suppl:3408. | ||
Rizvi N, Brahmer J, Ou SH. Safety and clinical activity of MEDI4736, an anti-programmed cell death-ligand (PD-L1) antibody, in patients with non-small cell lung cancer (NSCLC). J Clin Oncol. 2015;33 Suppl:8032. | ||
Spigel D, Chaft J, Gettinger S. Clinical activity and safety from a phase II study (FIR) of MPDL3280A (anti-PD-L1) in PD-L1-selected patients with non-small cell lung cancer (NSCLC). J Clin Oncol. 2015;33 Suppl:8028. | ||
Besse B, Johnson M, Janne P. Phase II, single-arm trial (BIRCH) of atezolizumab as first-line or subsequent therapy for locally advanced or metastatic PD-L1-selected non-small cell lung cancer (NSCLC). Eur J Cancer. 2015;51 (Suppl 3):S717–S718. | ||
Passiglia F, Bronte G, Bazan V, et al. PD-L1 expression as predictive biomarker in patients with NSCLC: a pooled analysis. Oncotarget. 2016;7(15):19738–19747. | ||
Ilie M, Long-Mira E, Bence C, et al. Comparative study of the PD-L1 status between surgically resected specimens and matched biopsies of NSCLC patients reveal major discordances: a potential issue for anti-PD-L1 therapeutic strategies. Ann Oncol. 2016;27(1):147–153. | ||
McLaughlin J, Han G, Schalper KA, et al. Quantitative assessment of the heterogeneity of PD-L1 expression in non-small-cell lung cancer. JAMA Oncol. 2016;2(1):46–54. | ||
Mansfield AS, Aubry MC, Moser JC, et al. Temporal and spatial discordance of programmed cell death-ligand 1 expression and lymphocyte tumor infiltration between paired primary lesions and brain metastases in lung cancer. Ann Oncol. 2016;27(10):1953–1958. | ||
Ilie M, Hofman V, Dietel M, Soria JC, Hofman P. Assessment of the PD-L1 status by immunohistochemistry: challenges and perspectives for therapeutic strategies in lung cancer patients. Virchows Arch. 2016;468(5):511–525. | ||
Hirsch FR, McElhinny A, Stanforth D, et al. PD-L1 immunohistochemistry assays for lung cancer: results from phase 1 of the Blueprint PD-L1 IHC Assay Comparison Project. J Thorac Oncol. 2017;12(2):208–222. | ||
Ratcliffe MJ, Sharpe A, Midha A, et al. Agreement between programmed cell death ligand-1 diagnostic assays across multiple protein expression cut-offs in non-small cell lung cancer. Clin Cancer Res. Epub 2017 Jan 10. | ||
Kyi C, Carvajal RD, Wolchok JD, Postow MA. Ipilimumab in patients with melanoma and autoimmune disease. J Immunother Cancer. 2014;2(1):35. | ||
Pedersen M, Andersen R, Nørgaard P, et al. Successful treatment with ipilimumab and interleukin-2 in two patients with metastatic melanoma and systemic autoimmune disease. Cancer Immunol Immunother. 2014;63(12):1341–1346. | ||
Narita T, Oiso N, Taketomo Y, et al. Serological aggravation of autoimmune thyroid disease in two cases receiving nivolumab. J Dermatol. 2016;43(2):210–214. | ||
Gettings EJ, Hackett CT, Scott TF. Severe relapse in a multiple sclerosis patient associated with ipilimumab treatment of melanoma. Mult Scler. 2015;21(5):670. | ||
Harvey RD. Immunologic and clinical effects of targeting PD-1 in lung cancer. Clin Pharmacol Ther. 2014;96(2):214–223. | ||
Harmankaya K, Erasim C, Koelblinger C, et al. Continuous systemic corticosteroids do not affect the ongoing regression of metastatic melanoma for more than two years following ipilimumab therapy. Med Oncol. 2011;28(4):1140–1144. | ||
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. | ||
Wolchok JD, Hoos A, O’Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15(23):7412–7420. | ||
Hodi F, Ribas A, Daud A. Evaluation of immune-related response criteria (irRC) in patients with advanced melanoma treated with the anti-PD-1 monoclonal antibody MK-3475. J Clin Oncol. 2004;22(14 Suppl):3006. | ||
Minor DR, Chin K, Kashani-Sabet M. Infliximab in the treatment of anti-CTLA4 antibody (ipilimumab) induced immune-related colitis. Cancer Biother Radiopharm. 2009;24(3):321–325. | ||
Amin A, Plimack E, Infante J, et al. Nivolumab (anti-PD-1; BMS-936558, ONO-4538) in combination with sunitinib or pazopanib in patients (pts) with metastatic renal cell carcinoma (mRCC). J Clin Oncol. 2014;32(5 Suppl):5010. | ||
Ott P, Hodi FS, Buchbinder EI. Inhibition of immune checkpoints and vascular endothelial growth factor as combination therapy for metastatic melanoma: an overview of rationale, preclinical evidence, and initial clinical data. Front Oncol. 2015;5:202. | ||
Hellman M, Creelan B, Woo K. Smoking history and response to nivolumab in patients with advanced NSCLCs. Ann Oncol. 2014;25(4):iv429. | ||
Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology: mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348(6230):124–128. | ||
Wang C, Thudium KB, Han M, et al. In vitro characterization of the anti-PD-1 antibody nivolumab, BMS-936558, and in vivo toxicology in non-human primates. Cancer Immunol Res. 2014;2(9):846–856. | ||
Feng Y, Bajaj G, Wang X. Model-based analysis of nivolumab to support clinical pharmacology profiling in subjects with solid tumors. Clin Pharmacol Ther. 2015;97 (Suppl 1):S41–S42. | ||
Scott LJ. Nivolumab: a review in advanced melanoma. Drugs. 2015;75(12):1413–1424. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

