Back to Journals » Infection and Drug Resistance » Volume 16
Emergence of Extended-Spectrum Beta-Lactamase and Carbapenemase Producing Gram Negative Non-Fermenters at Selected Hospitals of Northeast Ethiopia: A Prospective Cross-Sectional Study
Authors Tadesse S, Geteneh A , Hailu T
Received 3 February 2023
Accepted for publication 5 July 2023
Published 27 July 2023 Volume 2023:16 Pages 4891—4901
DOI https://doi.org/10.2147/IDR.S407151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Selamyhun Tadesse,1 Alene Geteneh,1 Tilahun Hailu2
1Department of Medical Laboratory Science, College of Health Sciences, Woldia University, Woldia, Ethiopia; 2School of Public Health, College of Health Sciences, Woldia University, Woldia, Ethiopia
Correspondence: Selamyhun Tadesse, Email [email protected]
Background: The emergence and spread of extended-spectrum β-lactamases (ESβLs) and carbapenemase (CP) producing gram negative non-fermenters are becoming a serious public health threat globally. Infections caused by these pathogens limit treatment options and contribute to the significant morbidity and mortality. Thus, to reduce their spread, early detection of these superbugs is very crucial. This study therefore aimed to assess the prevalence of ESβLs and CP producing gram negative non-fermenters at selected hospitals of North East Ethiopia.
Methods: A cross-sectional study was conducted from January to June 2021. Acinetobacter baumannii (A. baumannii) and Pseudomonas aeruginosa (P. aeruginosa) were identified using standard bacteriological techniques. ESβL and CP production were detected by combined disk diffusion and modified carbapenem inhibitory methods, respectively. Data were collected via face-to-face interview and patient card review. Chi-squared and Fisher’s exact tests were calculated and p-value < 0.05 was considered statistically significant.
Results: A total of 384 patients participated in this study. Overall, 30 (7.8%) patients had positive culture for A. baumannii and P. aeruginosa. The prevalence of A. baumannii was 20 (5.2%) and that of P. aeruginosa was 10 (2.6%). From the overall isolates, 16 (53.3%) were ESβL and the proportion of carbapenemase production was 4 (13.3%). ESβL production was 8 (40%) in A. baumannii and 8 (80%) in P. aeruginosa isolates. ESβL production infections were significantly associated with hospitalization (p=0.004). Intravenous catheterization, hospitalization, and surgery had significant association with ESβL production (p< 0.005). All isolates of A. baumannii and P. aeruginosa were MDR.
Conclusion: ESβL and carbapenemase production among A. baumannii and P. aeruginosa were high in the selected hospitals. The treatment of such resistant infectious agents should be guided by antimicrobial susceptibility test in a study setting. Thus, restricted and wise use of antibiotics is highly recommended to contain the spread of these superbugs. Hospitals should develop infection prevention guidelines to prevent the spread of resistant pathogens in hospitalized patients.
Keywords: ESβL, CP, MDR, A. baumannii, P. aeruginosa, Ethiopia
Background
Acinetobacter baumannii (A. baumannii) and Pseudomonas aeruginosa (P. aeruginosa) are gram negative non-fermenter (GNNF) superbugs responsible for multi-drug resistant infections at different clinical sites.1–3 They are the main etiologic agents of blood stream infection (BSI), urinary tract infection (UTI), wound infection, and lower respiratory tract infection (LRTI).1 Infection with these multi-drug resistant (MDR) strains seriously compromise treatment options.4
A. baumannii and P. aeruginosa are ubiquitous in nature, easily survive in moist environments and have innate resistance to many antibiotics.5,6 They frequently contaminate healthcare facility surfaces and shared medical equipment, and challenge the treatment of hospitalized patients.7Acinetobacter baumannii is mainly associated with BSI, pneumonia, and wound infections.5,8 Besides its potential for substantial antimicrobial resistance,7 carbapenem-resistant A. baumannii is one of the critical-priority pathogens on the WHO priority list of antibiotic-resistant bacteria for effective drug development.8 Similarly, Pseudomonas aeruginosa is involved in serious BSI, UTI, and LRTI and wound infections predominantly affecting hospitalized and immunocompromised individuals, and is highly resistant to many of the available antimicrobial agents including carbapenem.9–11
Different virulence factors have been isolated for A. baumannii, including hemolytic factors, iron acquisition systems, efflux pumps, lipopolysaccharides and OmpA, which can induce host immune system responses or bacterial adherence to epithelial cells.12 The production of phospholipases and elastases also facilitates the infection by degrading phospholipids, elastin and destruction of host cell tissue.13,14 Multiple intrinsic and acquired virulence factors are exploited by P. aeruginosa, including modification of drug targets, inactivation of antibiotics, expression of efflux systems, attenuation of membrane permeability, formation of biofilms and quorum-sensing, which, collectively, contribute to its distinctly low antibiotic susceptibility.15,16
Besides A. baumannii’s and P. aeruginosa’s intrinsic resistance to many antibiotics, the bacteria constantly develop new paths of resistance.17 Hence, the resistance to carbapenem drugs among these bacteria is a current challenge worldwide. They acquire genes encoding for beta-lactamases which are their foremost mechanisms of MDR.18 Extended spectrum β-lactamases (ESβL) and cabapenemases (CP) are now spreading among GNNFs causing serious infections with poor clinical outcomes and high mortality rates, mainly in hospitalized and immunocompromised patients.19,20 Carbapenems such as doripenem, ertapenem, imipenem and meropenem are the last resort antibiotics against both A. baumannii and P. aeruginosa infections.21 However, their efficacy is influenced by the production of carbapenemases. Carbapenemases are enzymes capable of hydrolyzing one or more carbapenem antibiotic in addition to penicillins, cephalosporins, and monobactams.22 Resistance of A. baumannii and P. aeruginosa to one of the carbapenem drugs is considered carbapenem resistance according to the Clinical and Laboratory Standards Institute (CLSI) guideline.23 Thus, infections caused by carbapenem resistant A. baumannii and P. aeruginosa are of particular concern because treatment options are extremely limited and they are often difficult to treat with available antibiotics.24
A few studies in the world documented 14.5–100% and 31–60.3% rates of carbapenem resistance among clinical isolates of A. baumannii and P. aeruginosa, respectively.25–28 A surveillance study done in Switzerland indicated there was 10.8% carbapenem resistance among A. baumannii species.29 A systematic review done in Africa also revealed the pooled prevalence of CP P. aeruginosa and CP A. baumannii among the clinical specimens was 21.36% and 56.97%, respectively.30 Because the increased incidence of infections with these resistant pathogens is associated with over-use of antimicrobials, prescription without susceptibility test, self-medication, and prolonged hospitalization, and the high immunocompromisation in resource-limited settings,31,32 the burden could be higher, and containment of these superbugs remains a challenge throughout the world. These highly MDR pathogens; A. baumannii and P. aeruginosa, are the WHO critical-priorities for effective drug development. Despite this concern, epidemiological data presenting the magnitude are limited in low-income countries including Ethiopia. Therefore, this study planned to estimate the burden of ESβL and CP producing GNNFs (A. baumannii and P. aeruginosa) in the selected hospitals in Northeast Ethiopia.
Methods
Study Design, Period and Setting
A hospital-based cross-sectional study was conducted between January and June 2021 among 384 patients presumed to have urinary tract, blood stream, lower respiratory or wound infections at selected hospitals in Northeast Ethiopia. Woldia Comprehensive Specialized Hospital, Lalibela General Hospital, and Kobo primary hospitals were selected among North Wollo Zone. These hospitals provide services to more than 3 million people around the area, but basic antimicrobial susceptibility tests were not performed in the hospitals. The laboratory testing for this study was done at Woldia University microbiology laboratory which is found in Woldia Town.
Eligibility Criteria
All patients attending those hospitals and clinically presumed to have UTI, BSI, LRTI and wound infections during the study period were included. However, study participants whose data were incomplete and gave inappropriate specimens (saliva and/or contaminated sputum, insufficient amount of all specimens, and delayed specimen during transportation) in the study period were excluded.
Data Collection
Information on demographic variables was collected from each participant with face-to-face interview using a structured questionnaire. Clinical data related to chronic disease, history of hospitalization, intravenous catheterization, surgery and use of antibiotics were collected through reviewing patients’ medical records in consultation with the respective physicians. With the study team, patients admitted to the different wards and ICU of selected hospitals of Northeast Ethiopia were carefully diagnosed with bacterial infections by different specialists.
Specimen Collection and Processing
Clinical specimens (blood, urine, sputum and wound swab/pus aspirate) were collected by the study team as soon as infection was reported following standard bacteriological procedures.23–25
Isolation and Identification of Bacteria
All isolates of A. baumannii and P. aeruginosa were identified by manual standard microbiological methods.33 All A. baumannii and P. aeruginosa suspected isolates were also further confirmed by an automated Vitek2 Compact (BioMérieux, France). Acinetobacter was identified by Gram staining, and colony morphology, positive catalase test, negative oxidase test and absence of motility. Speciation of Acinetobacter was performed on the basis of glucose oxidation, gelatin liquefaction, beta hemolysis, growth at 37°C and 42°C, colorless on MacCkonkey agar and arginine hydrolysis.34 Pseudomonas was also identified by Gram staining and colony morphology. Aerobically grow showing beta haemolysis in blood agar, colorless colonies on MacConkey. It was catalase, oxidase and citrase positive, whereas indole and urease negative.35
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing of A. baumannii and P. aeruginosa isolates was performed according to the criteria of Clinical and Laboratory Standard Institute (CLSI) using the Kirby-Bauer disk diffusion method on Mueller-Hinton Agar.36,37 The antibiotic discs tested were: penicillin category including: amoxicillin (25µg; Oxoid®, Basingstoke, England) and amoxicillin-clavulanic acid (20/10μg; Oxoid®, Basingstoke, England). Cephalosporin category: cefotaxime (30µg; Oxoid®, Basingstoke, England), ceftazidime (30µg; Oxoid®, Basingstoke, England), cefoxitin (30µg; Oxoid®, Basingstoke, England). Carbapenem family: meropenem (10µg; Oxoid®, Basingstoke, England) and ertapenem (10µg; Oxoid®, Basingstoke, England). Fluoroquinolones category: ciprofloxacillin (25µg; Oxoid®, Basingstoke, England), nitrofurantoin (300μg; Oxoid®, Basingstoke, England). Folate pathway inhibitors: trimethoprim-sulfamethoxazole (25μg; Oxoid®, Basingstoke, England). Aminoglycosides: gentamicin (10μg; Oxoid®, Basingstoke, England). These antimicrobial drug disks were selected based on CLSI guidelines and considering the availability and frequency of prescriptions of these drugs in the study area. The diameters of the zones of inhibition around the discs were measured using a digital caliper. The interpretation of the results of the antimicrobial susceptibility tests was based on CLSI criteria for resistance.23
Detection of Extended-Spectrum β-Lactamase and Carbapenemase Production
Initial screening for ESβL was done by considering the diameters of zones of inhibition produced by either ceftazidime (30 µg) or cefotaxime (30µg) from the antimicrobial susceptibility tests. After initial screening, ESβL production was confirmed with phenotypic combined disk method according to CLSI guidelines.23 The organism to be tested was uniformly inoculated onto MHA plates. Ceftazidime (30 µg) and cefotaxime (30µg) disks were used alone and in combination with clavulanic acid (30 µg/10 µg) for phenotypic confirmation of the presence of ESβLs at the same time. After incubation at 37°C for 24 h, a ≥ 5mm increase in diameter of zone of inhibition for either the ceftazidime-clavulanate and/or cefotaxime-clavulanate disk combination versus the zone diameter of the respective cephalosporin disk alone was considered positive and the isolate was interpreted as ESβL producer.23
Isolates resistant or intermediate for ertapenem (10µg) and/or meropenem (10µg) disk diffusion antimicrobial resistance screening was further tested for the production of carbapenemase by phenotypic modified carbapenem inhibitory method.23 With this method, the bacterial isolates were emulsified in tryptic soy broth and meropenem disk (10 µg) was added, then incubated for 4 h. McFarland standard equivalent suspension carbapenem sensitive indicator organism (E. coli ATCC®25922) was evenly swabbed onto MHA, and then the meropenem in the tryptic soy broth was dispensed. After incubation for 24 h at 37°C, the zone of inhibition for meropenem was measured. If the zone of inhibition was between 6–15 mm or 16–18 mm with pin points at the inhibition zone, the bacterial isolate was considered as carbapenemase producer.23
Quality Control
The sterility of the media was checked by incubating 5% of the batch at 35–37°C overnight. For antimicrobial sensitivity testing on MHA, American Type Culture Collection (ATCC) standard reference strains (E. coli ATCC 25922, P. aeruginosa ATCC 27853) for carbapenem and Escherichia coli ATCC 35218 (for β-lactam/β-lactam inhibitor combination) were used as quality control strains for culture and susceptibility testing throughout the study.23 For ESβL production, E. coli ATCC 25922 and K. pneumoniae ATCC 700603, for carbapenemase production K. pneumoniae ATCC BAA1705 were used as positive controls and K. pneumoniae ATCCBAA 1706 as carbapenemase negative control according to CLSI guidelines.23 All reference strains were obtained from APHI.
Data Analysis
Data were checked, entered, and analyzed using Statistical Package for Social Sciences 25 (IBM Corp, Released 2011, IBM SPSS statistics, Armonk, NY). Descriptive statistics were used to describe relevant variables. Chi-squared test and Fisher's exact test were utilized to determine association between dependent and independent variables. P-value of < 0.05 was considered statistically significant.
Results
Gram negative non-fermenters are known to cause different types of infections mainly in hospital settings. Due to the ubiquitous nature of these bacteria they can easily acquire resistant genes and become multidrug resistant. This study was done to determine the prevalence of ESβL and carbapenemase producing A. baumannii and P. aeruginosa isolated at different sites of infections by performing standard bacteriological methods.
A total of 384 study participants presumed to have BSI, UTI, LRTI and wound infections were screened for Gram negative non-fermenters. Gram negative non-fermenters recovered were phenotypically characterized in terms of susceptibility for commonly prescribed antibiotics and production of ESBL and carbapenemase. Overall, 20 (5.2) and 10 (2.6%) patients were culture positive for A. baumannii and P. aeruginosa, respectively and co-infection with the two species was not found. The frequency of isolation of A. baumannii and P. aeruginosa was 26 (4.9%) among inpatients and four (3.4%) among outpatients. Culture positivity was prominent in wound specimens: 12 (12.6%) followed by blood specimens: 10 (10.4). Table 1 illustrated the isolation rate of A. baumannii and P. aeruginosa.
 |
Table 1 Prevalence of A. baumannii and P. aeruginosa and Demographic Characteristics of Patients at Selected Hospitals of North East Ethiopia |
Phenotypic Characteristics of the Recovered Isolates
Overall, 20 (66.7%) isolates, of which 14 (70%) and 6 (60%) was A. baumannii and P. aeruginosa isolates, were carbapenem resistant, respectively. ESβL production was found in 16 (53.3%) of the total isolates. The distribution was 8 (40%) and 8 (80%) among A. baumannii and P. aeruginosa isolates, respectively. Four (13.3%) of the non-fermenter isolates; two each A. baumannii and P. aeruginosa isolates were carbapenemase producers (Table 2).
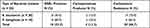 |
Table 2 Distribution of ESBL and Carbapenemase Production and Carbapenem Resistance Among A. baumannii and P. aeruginosa Isolates from Patients at Selected Hospitals of North East Ethiopia |
Both A. baumannii and P. aeruginosa isolates were 100% resistant to chloramphenicol and cefoxitin. Acinetobacter baumannii isolates were 100% resistant to sulfamethoxazole-trimethoprim while P. aeruginosa isolates were 100% resistant to amoxicillin-clavulanic acid, gentamicin, nitrofurantoin and cefotaxime. Acinetobacter baumannii isolates revealed 90% resistance to third generation cephalosporins (cefotaxime and ceftazidime). It also revealed 60% and 50% resistance to meropenem and ertapenem, respectively. On the other hand, P. aeruginosa isolates revealed 80% resistance to both ceftazidime and ciprofloxacin. Moreover, P. aeruginosa isolates revealed 60% resistance to carbapenem drugs either meropenem or ertapenem (Table 3).
 |
Table 3 Antibiotic Resistance Profiles of A. baumannii and P. aeruginosa Isolates from Participants Presumed to have Bacterial Infections at Selected Hospitals of North East Ethiopia |
All A. baumannii and P. aeruginosa isolates were found to be MDR (100%) (Table 4). All A. baumannii isolates revealed resistance to antibiotics representatives of 5–10 different classes. All P. aeruginosa isolates revealed resistance to antibiotics representatives of nine different classes (Table 4). All carbapenem resistant isolates were MDR. Likewise, all ESBL and carbapenemase producers were MDR.
 |
Table 4 Antibiogram of A. baumannii and P. aeruginosa Isolates from Patients Clinically Presumed for Different Clinical Sites of Infections at Selected Hospitals of North East Ethiopia |
Risk Factors of ESβL and Carbapenemase Production
No statistical difference was obtained for ESβL production in terms of sex, residence, and hospital patients setting. The proportion of ESβL production was significantly higher among patients with history of intravenous catheter for the last 12 months (8.7%) than their counterparts (2.7%) (p = 0.015). Furthermore, ESBL production was significantly higher among patients with history of admission for the last 12 months than their counterparts (p = 0.007). The proportion of ESBL production was 14.3% among patients who had surgery than their counterparts (2.7%) (p = 0.006) (Table 5). The proportion of carbapenem resistant isolates was significantly higher among patients with history of hospital admission for the last 12 months (12.7%) than their counterparts (2.8%) (p = 0.004) (Table 5).
Discussion
This study revealed the emergence of MDR strains of carbapenem resistant and beta-lactamases (CP and ESβL) producing A. baumannii and P. aeruginosa superbugs among patients with different sites of infections in a referral hospital, which is a major concern for patients and health care providers.
The prevalence of A. baumannii and P. aeruginosa infections was relatively higher than in a study in Jimma, Ethiopia,27 but lower than in a study in Addis Ababa, Ethiopia.1 However, the prevalence of A. baumannii and P. aeruginosa infection in the present study was lower than in studies from Uganda,28 Madagascar,7 Nepal,38 and India.39
The prevalence of A. baumannii infection in the present study was lower than in studies in other parts of Ethiopia.40,41 However, it was consistent with studies from other African countries,42–44 and Asia.38 A. baumannii was predominantly isolated from blood samples (5.2%) followed by sputum (2.1%), wounds (2.1%) and urine (1%) in the present study. This study corroborated a study from India at a tertiary care hospital,45 and from Madagascar.7 However; the finding of the present study is not in agreement with a study from Ethiopia.1 In this study, the highest number of P. aeruginosa was isolated from wound infection rather than other site infections. This is concurrent with the results of studies from Asia.38,45,46 The predominance of P. aeruginosa in wound infections might be linked to contamination of the wound from health care workers’ fomites, hands and hospital environments rather than other site of infections.
The current carbapenem resistance rate (66.7%) among non-fermenters is higher than other studies from Ethiopia,27 Bangladesh (14.5%),25 and USA (4.5%),26 This shows the rising prevalence of carbapenem resistance among non-fermenter GNB isolates, which is a threat to clinical practices. This could be due to drug prescription with improper susceptibility testing and indiscriminate use of antibiotics. Widespread use of third generation cephalosporins might contribute to the problem of carbapenem resistance. Furthermore, data on carbapenem drug resistant isolates are limited in Ethiopia and there is no regular tracking of such resistance profiles using antimicrobial susceptibility testing.
The proportion of carbapenem resistant A. baumannii isolates in this study was consistent with a study in eastern India,45 India,3 Nepal7 and Ethiopia,47 India.45 However, it was higher than a study from Uganda.28 On the other hand, it was lower than a study from Ethiopia,27 United States,26 and Latin America.46 The proportion of carbapenem resistant P. aeruginosa isolates in the present study is consistent with studies done in Egypt,42 India,45 and United States.26 However, it was higher than a study from Ethiopia27 and Libya (24%).18 Moreover, both meropenem and ertapenem resistance was shown by maximum isolates of P. aeruginosa.
In the current study, 10% of A. baumannii isolates were carbapenemase producers. Slightly lower rates were reported from Ethiopia41 and Japan.48 Moreover, the proportion of carbapenemase producing P. aeruginosa isolates in the present study was higher than studies from Ethiopia41 and Japan.48 This shows that there is an emergence of carbapenemase enzyme production among gram negative non-fermenters in the study area, which is one of the major resistance mechanisms for MDR.
The proportion of ESβL producing P. aeruginosa in the present study was 8 (80%). This is higher than rates reported from previous studies done in Ethiopia,1,47 India,38 and Nepal.7 However, the prevailing proportion of ESβL producing [8 (40%)] A. baumannii in this study was consistent with reports from other parts of Ethiopia,1,47 India,38 and Nepal.7 Thus, the occurrence of ESβL production on maximum isolates of non-fermenter might be linked to the extensive use of beta-lactams and heavy use of third generation cephalosporin antimicrobial drugs. This is because greater than 90% of A. baumannii and P. aeruginosa isolates were resistant to cefotaxime and ceftazidime in the present study. This showed that these two organisms are majorly resistant to most effective drugs (third generation cephalosporins) which makes it cumbersome to choose effective antibiotics for the treatment of these organisms.
The overall drug resistance profiles of A. baumannii and P. aeruginosa (commonly prescribed antibiotics) was high (86.7–100%). Similarly, the resistance profiles of A. baumannii and P. aeruginosa against cephalosporins were also high (93.3–100%). A. baumannii isolates’ resistance to cefotaxime (90%) and ceftazidime (90%) in the present study was consistent with a previous study done in Ethiopia,1 where 67.9% and 96.4% of isolates were resistant to ceftazidime and cefotaxime, respectively. Moreover, a study in Bithanda, India,38 reported 96.6% resistant isolates of A. baumannii to ceftazidime. In a study from Ethiopia,47 A. baumannii isolates were resistant to ceftazidime (63.1%) and cefotaxime (69.8%). Studies from eastern India45 and Madagascar37 reported 88.9% and 62% rate of resistance to ceftazidime, respectively.
The proportion of P. aeruginosa isolates resistant to ceftazidime (80%) and cefotaxime (100%) in the present study was higher than in other reports in Ethiopia and elsewhere in the world,1,37,47,49 where 1.9–66.9% and 70.8–91.8% isolates were resistant to ceftazidime and cefotaxime, respectively. This shows the rising spread of resistance toward extended-spectrum cephalosporins, which may lead to increased prescription of more broad-spectrum and expensive drugs. Thus, restriction on antibiotic use is required to contain them.
The rate of resistance of A. baumannii isolates to ciprofloxacin in the current study was lower than studies in Ethiopia.1,47 However, fewer and higher results were also documented in other parts of the world.7,37,45,49 On the other hand, the frequency of P. aeruginosa isolates’ resistance to ciprofloxacin (80%) in the present study was consistent with studies from Ethiopia,47 and India.45 But lower results were found in Ethiopia,1 Madagascar,37 and Nepal.7
All isolates of A. baumannii and P. aeruginosa were MDR (100%). This is consistent with previous studies in Ethiopia (100%).50 Moreover, higher MDR proportions were documented in Addis Ababa, Ethiopia (92.9%) for A. baumannii and (91.8%) for P. aeruginosa isolates.1 Furthermore, 62% and 81% of A. baumannii and P. aeruginosa were MDR in a similar study from Libya.18
The proportion of ESBL producing A. baumannii and P. aeruginosa infection was significantly higher among patients with prior intravenous catheterization, hospitalization, and surgery. This might be due to the increased colonization of resistant nosocomial strains in the hospital environment. Moreover, invasive procedures and hospitalization lower the immune status of patients which increases their susceptibility to hospital contaminants.51 Furthermore, intravenous catheterization, hospitalization, and invasive procedures allow resistance determinant genes to be acquired among isolates of the same species or Enterobacteriaceae which are common in the clinical area.24,52 According to CDC report, Acinetobacter infections typically occur in people in healthcare settings. People most at risk include patients in hospitals, especially those who have devices such as catheters and open wounds from surgery, are in intensive care units, and have prolonged hospital stays.24
Conclusion
This study highlighted high prevalence of carbapenem and cephalosporins resistant A. baumannii and P. aeruginosa isolates in the study area. Moreover, there was a considerable emergence of ESβLs and CP, and all isolates were MDR and resistant to at least five antibiotics representative of different classes. This necessitates the restricted and wise use of commercially available antibiotics, and need for regular screening of these superbugs and continued infection control practices in the clinical area. To conclude, treatment of infections caused by non-fermenter gram negative bacilli should be guided by drug susceptibility testing. Furthermore, antimicrobial resistance testing studies on the drug resistant determining genes are recommended.
Abbreviations
ATCC, American Type Culture Collection; AMR, Antimicrobial resistance; BSI, Blood stream infection; CLSI, Clinical and Laboratory Standards Institute; CP, Carbapenemase; ESβLs, Extended-Spectrum β- lactamases; GNNF, Gram negative non-fermntor; ICU, Intensive Care Unit; LRTI, Lower respiratory tract infection; MDR, Multi-drug resistance; UTI, Urinary tract infection.
Data Sharing Statement
The finding of this study was generated from the data collected and analyzed based on the stated methods and materials. All of the data are already in the manuscript and there are no supplementary files. The original data supporting this finding will be available from the corresponding author any time upon request.
Ethical Approval and Informed Consent
The study was approved by the Institutional Review Board (IRB) of College of Health Sciences, Woldia University with IRB no CHS/IRB/03-008. Prior to data collection, written informed consent was obtained from each participant. Written assent was also obtained from parents and/or surrogates to obtain information from children and those who cannot give data. Subject confidentiality and any special data security requirements were maintained and ensured by giving only codes for questionnaires. Results of the laboratory examinations that had a direct benefit to the health of the study participants were provided to physicians and the participants received their results and treatment duly as required. This study was in line with the Declaration of Helsinki.
Acknowledgments
This research received assistance from the College of Health Sciences, Woldia University. We would like to acknowledge selected hospitals for their permission to carry out the laboratory work in their setting. We also acknowledge Woldia University microbiology laboratory for their permission to conduct the laboratory tests.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Bitew A. High prevalence of multi-drug resistance and extended spectrum beta lactamase production in non-fermenting gram-negative bacilli in Ethiopia. Infect Dis. 2019;12:1178633719884951.
2. World Health Organization. Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter Baumannii and Pseudomonas Aeruginosa in Health Care Facilities. World Health Organization; 2017.
3. Shanthi M, Sekar U. Multi-drug resistant Pseudomonas aeruginosa and Acinetobacter baumannii infections among hospitalized patients: risk factors and outcomes. J Assoc Physicians India. 2009;57(636):8–40, 45.
4. Santajit S, Indrawattana N. Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res Int. 2016;2016:1–8. doi:10.1155/2016/2475067
5. Ding C, Yang Z, Wang J, et al. Prevalence of Pseudomonas aeruginosa and antimicrobial-resistant Pseudomonas aeruginosa in patients with pneumonia in mainland China: a systematic review and meta-analysis. Int J Infect Dis. 2016;49:119–128. doi:10.1016/j.ijid.2016.06.014
6. Lee C-R, Lee JH, Park M, et al. Biology of Acinetobacter baumannii: pathogenesis, antibiotic resistance mechanisms, and prospective treatment options. Front Cell Infect Microbiol. 2017;7:55. doi:10.3389/fcimb.2017.00055
7. Koirala A, Agrahari G, Dahal N, Ghimire P, Rijal K. ESBL and MBL mediated resistance in clinical isolates of nonfermentating Gram negative bacilli (NFGNB) in Nepal. J Microb Antimicrob Agents. 2017;3(1):18–24.
8. Kanafani Z, Kanj S. Acinetobacter infection: Treatment and prevention; 2020.
9. Lee C-S, Doi Y. Therapy of infections due to carbapenem-resistant gram-negative pathogens. Infect Chemother. 2014;46(3):149–164. doi:10.3947/ic.2014.46.3.149
10. Lemos E, de La Hoz F, Einarson T, et al. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect. 2014;20(5):416–423. doi:10.1111/1469-0691.12363
11. Riedel S, Morse SA, Mietzner TA, Miller S. Jawetz Melnick & Adelbergs Medical Microbiology 28 E. McGraw Hill Professional; 2019.
12. Ali HM, Salem MZ, El-Shikh MS, Megeed AA, Alogaibi YA, Talea IA. Investigation of the virulence factors and molecular characterization of the clonal relations of multidrug-resistant Acinetobacter baumannii isolates. J AOAC Int. 2017;100(1):152–158. doi:10.5740/jaoacint.16-0139
13. Antunes LC, Visca P, Towner KJ. Acinetobacter baumannii: evolution of a global pathogen. Pathog Dis. 2014;71(3):292–301. doi:10.1111/2049-632X.12125
14. Aliramezani A, Soleimani M, Fard RMN, Nojoomi F. Virulence determinants and biofilm formation of Acinetobacter baumannii isolated from hospitalized patients. Germs. 2019;9(3):148–153. doi:10.18683/germs.2019.1171
15. Taylor PK, Yeung AT, Hancock RE. Antibiotic resistance in Pseudomonas aeruginosa biofilms: towards the development of novel anti-biofilm therapies. J Biotechnol. 2014;191:121–130. doi:10.1016/j.jbiotec.2014.09.003
16. Gellatly SL, Hancock RE. Pseudomonas aeruginosa: new insights into pathogenesis and host defenses. Pathog Dis. 2013;67(3):159–173. doi:10.1111/2049-632X.12033
17. Control CfD, Prevention. Antibiotic Resistance Threats in the United States, 2019. US Department of Health and Human Services, Centres for Disease Control; 2019.
18. Mathlouthi N, Areig Z, Al Bayssari C, et al. Emergence of carbapenem-resistant Pseudomonas aeruginosa and Acinetobacter baumannii clinical isolates collected from some Libyan hospitals. Microbial Drug Res. 2015;21(3):335–341. doi:10.1089/mdr.2014.0235
19. Llaca-Díaz JM, Mendoza-Olazarán S, Camacho-Ortiz A, Flores S, Garza-González E. One-year surveillance of ESKAPE pathogens in an intensive care unit of Monterrey, Mexico. Chemotherapy. 2012;58(6):475–481. doi:10.1159/000346352
20. Ruppé É, Woerther P-L, Barbier F. Mechanisms of antimicrobial resistance in Gram-negative bacilli. Ann Intensive Care. 2015;5:1–15. doi:10.1186/s13613-015-0061-0
21. Papp-Wallace KM, Endimiani A, Taracila MA, Bonomo RA. Carbapenems: past, present, and future. Antimicrob Agents Chemother. 2011;55(11):4943–4960. doi:10.1128/AAC.00296-11
22. Mehrad B, Clark NM, Zhanel GG, Lynch JP III. Antimicrobial resistance in hospital-acquired gram-negative bacterial infections. Chest. 2015;147(5):1413–1421. doi:10.1378/chest.14-2171
23. Wayne. Performance standards for antimicrobial disk susceptibility tests. PA: (CLSI) CaLSI; 2020).
24. Control CfD, Prevention. Antibiotic resistance threats report; 2019. Available from: https://www.cdc.gov/drugresistance/biggest-threatshtml.
25. Begum N, Shamsuzzaman S. Emergence of carbapenemase-producing urinary isolates at a tertiary care hospital in Dhaka, Bangladesh. Tzu Chi MedJ. 2016;28(3):94–98. doi:10.1016/j.tcmj.2016.04.005
26. Cai B, Echols R, Magee G, et al. Prevalence of carbapenem-resistant Gram-negative infections in the United States predominated by Acinetobacter baumannii and Pseudomonas aeruginosa. Open Forum Inf Dis. 2017;2017:1.
27. Gashaw M, Berhane M, Bekele S, et al. Emergence of high drug resistant bacterial isolates from patients with health care associated infections at Jimma University medical center: a cross sectional study. Antimicrob Resist Infect Control. 2018;7:1–8. doi:10.1186/s13756-018-0431-0
28. Kateete DP, Nakanjako R, Namugenyi J, Erume J, Joloba ML, Najjuka CF. Carbapenem resistant Pseudomonas aeruginosa and Acinetobacter baumannii at Mulago hospital in Kampala, Uganda (2007–2009). Springerplus. 2016;5:1–11. doi:10.1186/s40064-016-2986-7
29. Ramette A, Kronenberg A, Burnens A, et al. Prevalence of carbapenem-resistant Acinetobacter baumannii from 2005 to 2016 in Switzerland. BMC Infect Dis. 2018;18(1):159. doi:10.1186/s12879-018-3061-5
30. Kindu M, Derseh L, Gelaw B, Moges F. Carbapenemase-producing non-glucose-fermenting gram-negative Bacilli in Africa, Pseudomonas aeruginosa and Acinetobacter baumannii: a systematic review and meta-analysis. Int J Microbiol. 2020;2020:9461901. doi:10.1155/2020/9461901
31. Morales E, Cots F, Sala M, et al. Hospital costs of nosocomial multi-drug resistant Pseudomonas aeruginosa acquisition. BMC Health Serv Res. 2012;12(1):1–8. doi:10.1186/1472-6963-12-122
32. Subramaniyan SJ, Sundaram JM. Occurrence of bla -genes encoding carbapenem‑ resistant Pseudomonas aeruginosa and Acinetobacter baumannii from Intensive Care Unit in a tertiary care hospital. J Lab Physicians. 2018;10(2):208–213. doi:10.4103/JLP.JLP_108_17
33. Cheesbrough M. District laboratory practice in tropical countries. IJMS. 2006;2(7.16):137.
34. Elham B, Fawzia AJ. Colistin resistance in Acinetobacter baumannii isolated from critically ill patients: clinical characteristics, antimicrobial susceptibility and outcome. Afr Health Sci. 2019;19(3):2400–2406. doi:10.4314/ahs.v19i3.13
35. Gopal MA. Isolation and identification of Pseudomonas aeruginosa FROM UROPATHOGENS. University of Yangon Res J. 2020;7:11.
36. Desta M, Amha H, Anteneh Bishaw K, et al. Prevalence and predictors of uterine rupture among Ethiopian women: a systematic review and meta-analysis. PLoS One. 2020;15(11):e0240675. doi:10.1371/journal.pone.0240675
37. Randrianirina F, Vaillant L, Ramarokoto CE, et al. Antimicrobial resistance in pathogens causing nosocomial infections in surgery and intensive care units of two hospitals in Antananarivo, Madagascar. J Infect Dev Ctries. 2010;4(02):074–82. doi:10.3855/jidc.454
38. Kaur A, Singh S. Prevalence of Extended Spectrum Betalactamase (ESBL) and Metallobetalactamase (MBL) Producing Pseudomonas aeruginosa and Acinetobacter baumannii Isolated from Various Clinical Samples. J Pathog. 2018;2018:1–7. doi:10.1155/2018/6845985
39. Wasihun AG, Wlekidan LN, Gebremariam SA, et al. Bacteriological profile and antimicrobial susceptibility patterns of blood culture isolates among febrile patients in Mekelle Hospital, Northern Ethiopia. Springerplus. 2015;4(1):1–7. doi:10.1186/2193-1801-4-1
40. Ampaire L, Nduhura E, Wewedru I. Phenotypic prevalence of extended spectrum beta-lactamases among Enterobacteriaceae isolated at mulago national referral hospital: Uganda. BMC Res Notes. 2017;10(1):1–4. doi:10.1186/s13104-017-2786-3
41. Moges F, Eshetie S, Abebe W, et al. High prevalence of extended-spectrum beta-lactamase-producing Gram-negative pathogens from patients attending Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, Amhara region. PLoS One. 2019;14(4):e0215177. doi:10.1371/journal.pone.0215177
42. El-Baky RM A, Farhan SM, Ibrahim RA, Mahran KM, Hetta HF. Antimicrobial resistance pattern and molecular epidemiology of ESBL and MBL producing Acinetobacter baumannii isolated from hospitals in Minia, Egypt. Alexandria J Med. 2020;56(1):4–13. doi:10.1080/20905068.2019.1707350
43. Goel V, Hogade SA, Karadesai S. Prevalence of extended-spectrum beta-lactamases, AmpC beta-lactamase, and metallo-beta-lactamase producing Pseudomonas aeruginosa and Acinetobacter baumannii in an intensive care unit in a tertiary care hospital. J Sci Soc. 2013;40(1):28. doi:10.4103/0974-5009.109691
44. Ntirenganya C, Manzi O, Muvunyi CM, Ogbuagu O. High prevalence of antimicrobial resistance among common bacterial isolates in a tertiary healthcare facility in Rwanda. Am J Trop Med Hyg. 2015;92(4):865. doi:10.4269/ajtmh.14-0607
45. Bandyopadhyay M, Chakraborty B, Kumar S, et al. A study on burden of carbapenem-resistant pseudomonas aeruginosa and Acinetobacter baumannii infections in a tertiary care hospital of eastern India; 2019.
46. Labarca JA, Salles MJC, Seas C, Guzmán-Blanco M. Carbapenem resistance in Pseudomonas aeruginosa and Acinetobacter baumannii in the nosocomial setting in Latin America. Crit Rev Microbiol. 2016;42(2):276–292. doi:10.3109/1040841X.2014.940494
47. Solomon FB, Wadilo F, Tufa EG, Mitiku M. Extended spectrum and metalo beta-lactamase producing airborne Pseudomonas aeruginosa and Acinetobacter baumannii in restricted settings of a referral hospital: a neglected condition. Antimicrob Resist Infect Control. 2017;6:1–7. doi:10.1186/s13756-017-0266-0
48. Kuntaman K, Shigemura K, Osawa K, et al. Occurrence and characterization of carbapenem‐resistant Gram‐negative bacilli: a collaborative study of antibiotic‐resistant bacteria between Indonesia and Japan. Int J Urol. 2018;25(11):966–972. doi:10.1111/iju.13787
49. Defaee S, Farasatinasab M, Makani MJ, Rahimipour H, Alinia P, Defaee S. Prevalence of gram negative infections by Acinetobacter and pseudomonas severely resistant to antibiotic susceptibility based on minimum growth inhibitor concentration. J Pharmaceut Res Inter. 2019;29(3):1–6. doi:10.9734/jpri/2019/v29i330235
50. Motbainor H, Bereded F, Mulu W. Multi-drug resistance of blood stream, urinary tract and surgical site nosocomial infections of Acinetobacter baumannii and Pseudomonas aeruginosa among patients hospitalized at Felegehiwot referral hospital, Northwest Ethiopia: a cross-sectional study. BMC Infect Dis. 2020;20:1–11. doi:10.1186/s12879-020-4811-8
51. Ibrahim ME. Prevalence of Acinetobacter baumannii in Saudi Arabia: risk factors, antimicrobial resistance patterns and mechanisms of carbapenem resistance. Ann Clin Microbiol Antimicrob. 2019;18(1):1. doi:10.1186/s12941-018-0301-x
52. Huang H, Chen B, Liu G, et al. A multi-center study on the risk factors of infection caused by multi-drug resistant Acinetobacter baumannii. BMC Infect Dis. 2018;18:1–6. doi:10.1186/s12879-017-2932-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

