Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Eleven-Year Trends in Lipid-Modifying Medicines Utilisation and Expenditure in a Low-Income Country: A Study from the Republic of Srpska, Bosnia and Herzegovina
Authors Kalinić D , Škrbić R, Vulić D, Stoisavljević-Šatara S , Stojaković N , Stojiljković MP, Marković-Peković V, Golić Jelić A , Pilipović-Broćeta N , Divac N
Received 3 March 2023
Accepted for publication 2 June 2023
Published 29 June 2023 Volume 2023:15 Pages 513—523
DOI https://doi.org/10.2147/CEOR.S410711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Dragan Kalinić,1 Ranko Škrbić,2 Duško Vulić,3 Svjetlana Stoisavljević-Šatara,2 Nataša Stojaković,2 Miloš P Stojiljković,2 Vanda Marković-Peković,4 Ana Golić Jelić,4 Nataša Pilipović-Broćeta,5 Nevena Divac6
1Centre for Biomedical Research, Faculty of Medicine, University of Banja Luka, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina; 2Department of Pharmacology, Toxicology and Clinical Pharmacology, Faculty of Medicine, University of Banja Luka, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina; 3Centre for Specialisations and Continuous Medical Education, Faculty of Medicine, University of Banja Luka, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina; 4Department of Pharmacy, Faculty of Medicine, University of Banja Luka, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina; 5Family Medicine Teaching Centre, Primary Healthcare Centre of Banja Luka, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina; 6Department of Pharmacology, Clinical Pharmacology and Toxicology, Faculty of Medicine, University of Belgrade, Belgrade, 11000, Serbia
Correspondence: Dragan Kalinić, Centre for Biomedical Research, Faculty of Medicine, University of Banja Luka, Save Mrkalja 14, Banja Luka, 78000, Republic of Srpska, Bosnia and Herzegovina, Tel/Fax +387 51 234 101, Email [email protected]
Background: In last two decades, there have been substantial changes in the pattern of lipid-modifying medicines utilisation following the new treatment guidelines based on clinical trials. The main purpose of this study was to analyse the overall utilisation and expenditure of lipid-modifying medicines in the Republic of Srpska, Bosnia and Herzegovina during an 11-year follow-up period and to express its share in relation to the total cardiovascular medicines (C group) utilisation.
Methods: In this retrospective, observational study, medicines utilisation data were analysed between 2010 and 2020 period using the ATC/DDD methodology and expressed as the number of DDD/1000 inhabitants/day (DDD/TID). The medicines expenditure analysis was used to estimate the annual expenditure of medicines in Euro based on DDD.
Results: During the analysed period, the use of lipid-modifying medicines increased almost 3-times (12.82 DDD/TID in 2010 vs 34.32 DDD/TID in 2020), with a rise in expenditure from 1.24 million Euro to 2.15 million Euro in the same period. This was mainly driven by an increased use of statins with 163.07%, and among these, rosuvastatin increased more than 1500-fold, and atorvastatin with 106.95% increase. With the appearance of generics, simvastatin showed a constant decline, while the other lipid-modifying medicines in relation to the total utilisation had a neglecting increase.
Conclusion: The use of lipid-modifying medicines in the Republic of Srpska has constantly increased and strongly corresponded to the adopted treatment guidelines and the positive medicines list of health insurance fund. The results and trends are comparable with other countries, but still the utilisation of lipid-lowering medicines represents the smallest share of total medicines use for the treatment of cardiovascular diseases, compared to high-income countries.
Keywords: lipid-modifying medicines, medicines utilisation, ATC/DDD methodology, medicines expenditure, medicines positive list
Introduction
Cardiovascular diseases (CVDs) are the leading cause of death globally, taking an estimated 17.9 million lives each year and representing 32% of all deaths worldwide1. More than four out of five cardiovascular deaths are related to atherosclerotic cardiovascular diseases (ASCVDs) presented as heart attacks and strokes, and one-third of these deaths occur prematurely in people under 70 years of age. Over three-quarters of cardiovascular deaths take place in low- and middle-income countries.1,2 According to the World Health Organisation, it is estimated that these diseases will cause nearly 23 million deaths by 2030. Ischaemic heart diseases cause more than 4 million deaths per year in Europe. Data from the available literature show that a third of ischaemic diseases are associated with high cholesterol values, representing about 4.5% of total mortality.2–4
The most common risk factors for ASCVDs are nonhealthy nutrition, lack of physical activity, harmful use of tobacco and alcohol, which can be further manifested as an increase in blood pressure, blood glucose, lipids and body weight.5 ASCVDs as leading causes of death today are preventable in 80% of cases, meaning that elimination or reduction of risk factors, such as decreasing the low-density lipoprotein (LDL) cholesterol, smoking secession, or better controlling of blood pressure,3 could reduce the incidence of ASCVDs for 75%.6 One of the main goals of treating dyslipidaemia is to decrease the risk of ASCVD, as well as to reduce early disability and mortality. The latest guidelines of the European Society of Cardiology (ESC) and the European Athero-sclerosis Society (EAS) strictly recommended that if the goal for high and very-high risk patients is to prevent the CVDs, then the LDL cholesterol must be reduced as much as possible.7 To prevent high CV risk, the high-density lipoprotein (HDL) cholesterol values must be above 1.3 mmol/L, while the total blood cholesterol values should be below 5 mmol/L and in CV patients below 4.5 mmol/L.8,9
The growing incidence of CVDs is consequently followed by an increased use of cardiovascular medicines over the years.10 Among these, lipid-lowering medicines are crucial to reduce the risk of ASCVD, and several classes of medicines have been effectively used over the years or decades like 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins), bile acid sequestrants, fibrates, nicotinic acid, omega-3-triglycerides, and others.
Statins are the most prescribed lipid-lowering medicines worldwide, and this class of medicines is known as a cornerstone of pharmacological therapy for dyslipidaemia and ASCVD in all major international guidelines. Although all statins share the same mechanism of action, the degree of LDL cholesterol reduction depends on the dose and type of statin. Based on the intensity of lipid-lowering effect, all statins can be categorised as high- (atorvastatin 40–80 mg, rosuvastatin 20–40 mg), moderate- (atorvastatin 10–20 mg, fluvastatin 40–80 mg, lovastatin 40 mg, pravastatin 40–80 mg, rosuvastatin 5–10 mg) and low-intensity statins (fluvastatin 20–40 mg, lovastatin 20 mg, pravastatin 10–20 mg, simvastatin 10 mg). These statin dose regimens are individual for each patient, since there is an individual variation in LDL-C reduction obtained by the same statin dose 90.11
Although the main effect of statins is to lower the level of LDL cholesterol, statins also moderately increase the level of HDL cholesterol (1–10%).12 Indeed, many studies confirm that statins possess other cholesterol-independent or “pleiotropic” properties such as anti-oxidative, anti-inflammatory and antiapoptotic effects that contribute to improvement of endothelial function, stabilisation of atherosclerotic plaques, or inhibition of thrombogenic response.12–17
Statins are used in the primary and secondary prevention of coronary heart disease, reducing very effectively the incidence of major coronary events.8 In the Republic of Srpska, statins are on the medicines list of Health Insurance Fund (HIF) for primary and secondary prevention of coronary heart disease, as well as for patients with diabetes mellitus and familiar hyperlipoproteinaemia.
Recommendations for use of statins and other lipid-modifying medicines in these conditions are derived from the national clinical guidelines for primary healthcare that were developed as a joint document of both the Association of Cardiologists and Association of Family Physicians of the Republic of Srpska published in 2004. Five years later, the second edition was released in 2009, followed by the third one in 2015.14 The most recent recommendations have followed the 2016 and 2019 ESC/EAS guidelines for secondary prevention of ASCVDs, and new medicines have been added to the list, like proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors and cholesterol absorption inhibitor, ezetimibe.7,11 These guidelines have significantly influenced the lipid-modifying medicines utilisation over the years. The main purpose of this study was to analyse the overall utilisation and financial expenditure of lipid-modifying medicines during eleven-year period with special emphasis on statins.
Materials and Methods
A retrospective, observational study was conducted to analyse the utilisation of lipid-modifying medicines in the Republic of Srpska during the period 2010–2020. The Republic of Srpska is one of the two constitutive entities of Bosnia & Herzegovina with a total population of 1.2 million.18 It has executive and legislative functional responsibilities covering all aspects of healthcare policies. The Ministry of Health and Social Welfare is responsible for planning, regulation and management functions, while the HIF provides compulsory health insurance coverage for the entire population based on solidarity and mutuality.19
Health institutions in the Republic of Srpska that have signed a contract with HIF, regardless of whether they are at primary, secondary or tertiary level, provide all its residents with free and equal access to health care. The HIF reimburses prescribed medicines, which are on the essential, or so-called “positive” medicines list. The positive medicines list is based on Anatomical Therapeutic Chemical (ATC) classification, and all medicines are listed by international non-proprietary names (INN-ATC level 5).19 The list is updated regularly, at least twice a year, and published in Official Gazette.20 Cardiovascular medicines that are recommended by a doctor at the secondary or tertiary level are further prescribed by family medicine doctors at the primary health care and can be dispensed from community pharmacies, only.21
The medicines utilisation and expenditure data were retrieved from Public Health Institute (PHI) of the Republic of Srpska. The PHI is responsible for collecting medicines utilisation and expenditure data from all pharmacies. All data which are presented in an annual report comprising 100% of pharmacies.19,22 Medicines utilisation analysis was undertaken using the ATC/DDD (Defined Daily Dose) methodology,23 which is the internationally accepted methodology for measuring medicines utilisation within and across populations.24 DDD is defined as the number of medicines most commonly used for the most common indication in adults. It is a suitable measure to describe and compare medicines utilisation patterns between different geographical regions and health facilities.24,25 Data on outpatient medicines utilisation are typically expressed in DDD/1000 inhabitants/day (DID/TID) for comparative purposes.24
According to the official data from PHI with retail prices, the financial data were analysed to get an insight on overall medicines expenditure during the observed period. The results will be presented as follows: a) utilisation in DDD/TID, b) expenditure in Euro, c) total expenditure in Euro per DDD and d) as a share of utilisation and expenditure of subgroups in relation to total or cardiovascular medicines utilisation and expenditure. The financial data were initially calculated in local currency (convertible mark-BAM) before their conversion to Euro. In order to obtain a more detailed analyses of the statin use, an additional set of data from HIF covering prescribed utilisation of statins only was collected for years 2013, 2016 and 2019. This study was based on anonymous data analyses and did not involve direct patient contacts or intervention with patient’s electronic records. Therefore, it was not necessary to obtain permission from the Ethics Committee.
Results
Trends in Lipid-Modifying Medicines Utilisation
The cardiovascular medicines (group C) were the most utilised group of medicines in the Republic of Srpska with a 40% share of total medicine utilisation during last eleven years of observation (Table 1). The utilisation of lipid-modifying medicines (C10) has shown a growing trend with an almost 3-fold utilisation increase, from 12.82 DDD/TID in 2010 to 34.32 DDD/TID in 2020 (Table 1 and Figure 1). The utilisation of lipid-modifying medicines (subgroup C10) in the Republic of Srpska was lower than in other European countries26 as shown in Figure 2. Among these, statins (C10AA) were the most utilised medicines with over 96% share of all lipid-modifying medicines. The utilisation of statins increased from 12.62 DDD/TID in 2010 to 33.2 DDD/TID in 2020 (Table 1 and Figure 1).
 |
Table 1 The Utilisation of Total Medicines, Cardiovascular Medicines, Lipid-Modifying Medicines and Statins in the Republic of Srpska During 2010–2020, Expressed in DDD/TID and Share (%) |
 |
Figure 2 The utilisation of lipid-modifying medicines in the Republic of Srpska in 2019 and 2020 vs other European countries in the same years expressed in DDD/TID (Adapted from OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en).25 DDD/TID – Defined Daily Dose/Thousand Inhabitants per Day; The solid blue lines – the utilisation of lipid-modifying medicines in European countries in 2020; The green dashed lines – The utilisation of lipid-modifying medicines in European countries in 2019; The red text – The utilization of lipid-modifying medicines in the Republic of Srpska in 2019 and 2020. |
Atorvastatin, rosuvastatin and simvastatin were the most used statins over the years of observation. The utilisation of simvastatin in the 11-year period had the tendency of decline, from 4.84 DDD/TID in 2010 to 1.30 DDD/TID in 2020 (a decrease by almost 73%). At the same time, the utilisation of atorvastatin increased from 7.77 DDD/TID in 2010 to 16.08 in 2020 (a total increase of 106.95%). The highest increase was observed for rosuvastatin, from 0.01 DDD/TID in 2010 to 15.82 in 2020 (Table 2 and Figure 1). The total share of fibrates was very low and varied from 1.01% in 2010 to 3.03% in 2020. Gemfibrozil was the most prescribed fibrate in 2010, while in 2011 it was ciprofibrate. During the last nine observed years fenofibrate was the leading fibrate and its utilisation increased from 0.14 to 1.03 DDD/TID, as presented in Table 2.
 |
Table 2 The Utilisation of Lipid-Modifying Medicines in the Republic of Srpska in the Period from 2010 to 2020, Expressed by the DDD/TID Day and Share (%) |
The utilisation of other lipid-modifying medicines (subgroup C10AX) was quite low, with the share of 1%. Ezetimibe, as the representative of this subgroup, was added to the positive list of medicines in 2019 and its utilisation in that year was 0.02 DDD/TID, followed by 0.09 DDD/TID in 2020 (Table 2). These medicines were prescribed as monotherapy or in a fixed combination with medicines belonging to C10AA subgroup.
The cross-sectional analysis of data for prescribed cardiovascular and lipid-lowering medicines in 2013, 2016 and 2019 also showed an increase in utilisation (Table 3). The share of the prescribed cardiovascular medicines in comparison with their total utilisation decreased from 89.93% in 2013 to 68.44% in 2019. The share of the prescribed lipid-modifying medicines within their total utilisation decreased from a half in 2013 to a third in 2019. The highest utilisation of these medicines was recorded in the age group over 60 and was higher in women than in men regarding the utilisation of all cardiovascular medicines (group C), while higher utilisation of lipid-modifying medicines was recorded in men (subgroup C10) (Table 1 and Table 3).
Trends in Lipid-Modifying Medicines Expenditure
The total expenditure of medicines increased from 55.85 million Euro in 2010 to 78.75 million Euro in 2020. The expenditure share for cardiovascular medicines ranged from 29.27% in 2010 to 25.38% in 2020. The expenditure share of these medicines increased from 16.08 million Euro in 2010 to 19.98 million Euro in 2020 (Table 4). In the same period, the expenditure for lipid-modifying medicines showed a constant growth from 1.24 million Euro in 2010 to 2.15 million Euro in 2020.
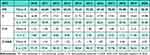 |
Table 4 Expenditure of Total Medicines, Cardiovascular Medicines, Lipid-Modifying Medicines and Statins in Republic of Srpska During 2010–2020, Expressed in Million Euro and the Shares (%) |
Over 95% of the market share for lipid-modifying medicines refers to statins, with expenditure rise of approximately 70% in 2020 compared to 2010 (Table 4 and Figure 1). Related to the total lipid-modifying medicines expenditure, the expenditure for simvastatin had a negative trend with a decrease in share from 42.62% in 2010 to 4.77% in 2020. On the other hand, the expenditure for atorvastatin increased from 0.67 million Euro in 2010 to 0.97 million Euro in 2020. However, the highest expenditure increase was observed for rosuvastatin, from 0.01 million Euro in 2010 to 1.00 million Euro in 2020, and with share from 0.58% to 46.61%, respectively (Figure 1).
The total expenditure of lipid-modifying medicines expressed as price per DDD showed an initial increase from 2010 to 2011, which was followed by a nearly 32% reduction in expenditure/DDD in 2020 vs 2010. A similar trend was seen for simvastatin and atorvastatin. However, when rosuvastatin appeared on the market in 2010, its price per DDD was very high (1.66 Euro), but after being added to the positive list in 2011, its price per DDD decreased significantly and then constantly declined in the following years (Figure 1).
Discussion
The results of this study have shown that during an eleven-year period, the utilisation of lipid- modifying medicines in the Republic of Srpska increased almost three times. Of all lipid-modifying medicines, statins were the most prescribed with more than 95% utilisation, while the rest belonged to fibrates and the so-called “other lipid-modifying medicines”, such as omega-3-triglycerides and ezetimibe. There are several reasons for such a significant increase in statin utilisation over the years: first, there have been an increased number of patients with CVD over the years, based on real data obtained from HIF; second, the introduction of more accurate data collection through the web-based health information system; and third, the strict adherence to national and ESC/EAS guidelines for prevention of ASCVDs that recommended the use of statins for these conditions.7,11,13–15,27,28 Atorvastatin and rosuvastatin were the most prescribed statins during whole period, and their prescribing growth properly followed the treatment recommendations towards the use of high-potency statins.28–30 The CURVES study clearly showed that atorvastatin treatment resulted in greater reduction in LDL cholesterol level than the equivalent doses of simvastatin.31 Additionally, a multicentre STELAR study confirmed that rosuvastatin was superior in lowering LDL cholesterol levels than atorvastatin given at the same dose.32 The promising results of these two studies were the basis for the recommendations of clinical guidelines directed toward the use of atorvastatin, and rosuvastatin as the most potent statins for primary and secondary prevention of ASCVDs.12
As stated in clinical guidelines, the patients with high-risk for ASCVDs should be treated as much as needed to achieve both, a target LDL cholesterol level and a minimum 50% of its relative reduction, respectively. It is known that statins pose different potency for LDL cholesterol reduction and their efficacy is dose-dependent. Therefore, a high-intensity regimen is required to achieve the LDL cholesterol reduction by ≥50%, while the moderate-intensity therapy is proposed as the dose that reduces the LDL-cholesterol by 30–50%. If patients cannot tolerate the highest statin doses due to adverse effects, or if they cannot achieve defined therapeutic goals, then the addition of another lipid-modifying medicine to a maximally tolerated statin should be considered.7
PCSK9 inhibitors are very effective in reducing LDL-C values (up to 60%) as additional therapy to statin treatment. PCSK9 inhibitors should be considered in primary and secondary prevention for patients with high and very high risk due to already developed CVD, premature coronary atherosclerotic disease in the family history or if the value of LDL-C is significantly higher than the target value despite a high-dose statin treatment regimen, eg atorvastatin 40–80 mg daily or rosuvastatin 20–40 mg daily.30,33
Randomized clinical trials have shown that for every 1 mmol reduction in LDL-cholesterol, the major vascular events could be decreased by 22%, major coronary events by 23%, coronary mortality disease by 20%, total stroke by 17%, and total mortality by 10%. This is one of the main reasons why the treatment of hyperlipoproteinaemias is very important tasks for CVD prevention.34
The results of PURE study comprising 22 countries showed that in high-income countries, like Sweden and Canada, 66% of patients with CVD use statins, while in upper-middle-income countries (Poland, Turkey, Brazil and China) or in lower-middle-income countries (India) the percentage of patients treated with statins was 27% and about 5%, respectively.35,36 In the SHARE study, only 42% of patients with CVD were treated with cholesterol-lowering therapy with large variations between countries; 55–56% in Norway, Denmark and Belgium and 27–29% in Slovenia and Estonia.35,37
Variations between different countries of the use of lipid-modifying medicines were also noticed in a study that was conducted in Serbia between 2015 and 2017, which showed a 3–4 times lower use of lipid-modifying medicines than in the Nordic countries. The share of lipid-modifying medicines relative to the total cardiovascular medicines in Serbia was between 5% and 6%, while the share of lipid-modifying medicines in Norway was much higher, around 30%, and around 20% in Finland.
At the same time, the utilisation shares of statins relative to lipid-modifying medicines in Nordic countries were over 95%, while in Serbia that share was around 90%.38 In comparison with that study, the utilisation of lipid-modifying medicines in the Republic of Srpska expressed as relative share to all cardiovascular medicines followed the Serbia trend (5–6%), while the utilisation of statins expressed as share relative to the lipid-modifying medicines followed the Nordic trend with over 95%. Similar results were seen in North Macedonia with over 95% of the market share for lipid-modifying medicines, which mainly refers to statins in the period from 2013 to 2016.39
After the intensive growth of statin use at the beginning of the 21st century, their use has been stabilised in recent years, with constant slight annual growth. One of the reasons for a significantly lower prescribing of lipid-modifying medicines and therefore statins in the Republic of Srpska comparing with the neighbouring and other European countries could be found in the prescribing policy. The HIF of the Republic of Srpska has very strict criteria for statin prescribing and reimbursement. The indications for which statins can be prescribed and reimbursed are based on risk assessment for primary and secondary prevention of heart diseases, diabetes mellitus, familiar hyperlipoproteinaemia, chronic renal failure and transplanted organ condition with hyperlipoproteinemia and presence of implants and grafts on the heart and blood vessels.40 All statins that are available on the market of the Republic of Srpska are included in the positive medicines list, but as “group B medicines” with 50% reimbursement by HIF,20 meaning that half of statin’s price refers to patient’s co-payment.
The financial expenditure for lipid-lowering medicines expressed in Euro increased a bit less than two-fold during the period of eleven years. Statin expenditure followed this trend and increased proportionally with some variabilities related to different types of statins. More than half of the current statin expenditure was related to atorvastatin, while in 2020 rosuvastatin expenditure almost equalised with atorvastatin.
The decreasing trend in the share of the prescribed lipid-modifying medicines within their total utilisation in years 2013, 2016 and 2019 could be the result of several factors. First, expiration of the patent protection of new originator molecules, followed by the occurrence of numerous generics, has a direct impact on prices which makes them more available for patients without prescriptions. Second, strict co-payment policy and higher generic availability of statins have been the major reasons for the shift from prescription only towards the higher dispensing of these medicines without prescription.
Our study confirmed that cardiovascular medicines have been mostly used by elderly patients and primarily by women, while lipid-lowering medicines were utilised predominantly by men. This could be explained by the fact that the incidence of cardiovascular diseases is high in elderly population and increased in postmenopausal women.25,41–43
Comparing to our study that was conducted at the period 2004–2010, the statin utilisation in the period 2010–2020 continued to rise but not as much as during the previous period. The similarity between these two studies is in the finding that utilisation and financial growth were mostly driven by atorvastatin. The reduction in expenditure/DDD is smaller than in the earlier analysis, except for rosuvastatin that was at that time included as new medicine in the positive list.19 The appearance of generic medicines with lower prices, but with the same safety and efficacy, apparently caused significant changes in the overall statin utilisation, with the significant influence on total statin expenditure.44
The similar trend of statin utilisation and expenditure during the period of 20 years can be seen in a Danish study. The overall use of statins from 1996 to 2015 increased 62-fold, from 2.2 to 137.3 DDD/TID, while the expenditure for statins increased from ≈$20 million to ≈$33 million. Total spending for statins was below that in 1998, due to a large reduction in the cost of statins per DDD and the introduction of generic forms of medicines and generic prescribing policy.45 Similarly, after the statin generics were introduced in the Republic of Srpska in 2011, the expenditure of these medicines has decreased. Other lipid-modifying medicines, such as fibrates and ezetimibe, had negligible effects on total utilisation and expenditure.
Strengths and Limitations
The strengths of this study are a fairly long period of observation and accurate and reliable data comparable to other studies. This type of study enables adequate monitoring and decision-making process in accordance with the utilisation data and gives us the insight in the appropriateness of treatment guidelines. The study has some limitations. First, it was not able to assess the medicines utilisation data according to patients’ diagnoses, including the established and confirmed ASCVD in statin users with comorbidities that could influence the medicines utilisation figures. Second, this study cannot give us the insight into the actual users of lipid-modifying medicines since treatment adherence has always been a problem in the management of dyslipidaemia. Nevertheless, the main purpose of this study was to analyse the overall utilisation trends, and therefore, this limitation has not influenced the conclusion.
Conclusion
Our study provides detailed and important insights into the increased trends of lipid-modifying medicines utilisation and expenditure in the Republic of Srpska between 2010 and 2020. The overall increase was driven by increased prescribing of statins as generic medicines, primarily atorvastatin at the period from 2013 to 2014, and then rosuvastatin at the period from 2017 to 2018. At the same time, simvastatin utilisation trend has shown constant decline. These data are comparable with utilisation and expenditure trends of other countries, with the fact that the use of these medicines in low-income country still represents a smaller share in overall use of cardiovascular medicines compared to high-income countries.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest.
References
1. World Health Organisation. Cardiovascular diseases. Fact sheets. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
2. World Health Organisation. Global health estimates: life expectancy and leading causes of death and disability. Global Health Observatory. Data. Available from: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates.
3. World Health Organisation. Cardiovascular Disease. Data and statistics. Available from: https://www.euro.who.int/en/health-topics/non-communicable-diseases/cardiovascular-diseases/data-and-statistics.
4. World Health Organization. European health for all database 2019; 2019. Available from: http://www.euro.who.int/hfadb.
5. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;34976:2982–3021. doi:10.1016/j.jacc.2020.11.010
6. Milašinović G. National Guide of Clinical Practice for the Diagnosis and Treatment of Lipid Disorders. Belgrade: Accreditation Agency for Health Institutions of Serbia; 2012. Serbian.
7. Mach F, Baigent C, Catapano AL, et al; ESC Scientific Document Group. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–188. doi:10.1093/eurheartj/ehz455
8. Hoover LE. Cholesterol management: ACC/AHA updates guideline. Am Fam Physician. 2019;99(9):589–591. doi:10.1161/CIR.0000000000000452
9. Karr S. Epidemiology and management of hyperlipidemia. Am J Manag Care. 2017;36023(9):S139–S148.
10. Kalinić D, Škrbić R, Vulić D, et al. Trends in antihypertensive medicine utilisation in the Republic of Srpska, Bosnia and Herzegovina: an eleven-year follow-up. Front Pharmacol. 2022;13:889047. doi:10.3389/fphar.2022.889047
11. Catapano AL, Graham I, De Backer G, et al.; ESC Scientific Document Group. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058. doi:10.1093/eurheartj/ehw272
12. Visseren FL, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies. Eur Heart J. 2021;42:3227–3337. doi:10.1093/eurheartj/ehab484
13. Guidelines Committee. Hyperlipoproteinaemia, Guideline for Clinical Practice. Ministry of Health and Social Welfare of the Republic of Srpska; 2004.
14. Guidelines Committee. Hyperlipoproteinaemia, Guideline for Clinical Practice. Ministry of Health and Social Welfare of the Republic of Srpska; 2008.
15. Ministry of Health and Social Welfare of Republic of Srpska. Guideline for clinical practice: hyperlipoproteinaemia 2015; 2015. Available from: https://www.vladars.net/sr-SP-Cyrl/Vlada/Ministarstva/MZSZ/Documents/15.%204.%20Hiperlipoproteinemije.pdf.
16. Nežić L, Škrbić R, Dobrić S, et al. Simvastatin and indomethacin have similar anti-inflammatory activity in a rat model of acute local inflammation. Basic Clin Pharmacol Toxicol. 2009;104(3):185–191. doi:10.1111/j.1742-3837843.2008.00302.x
17. Nežić L, Škrbić R, Amidžić L, Gajanin R, Kuča K, Jaćević V. Simvastatin protects cardiomyocytes against endotoxin-induced apoptosis and up-regulates survivin/NF-κB/p65 expression. Sci Rep. 2018;8(1):14652. doi:10.1038/s41598-018-32376-4
18. Republic of Srpska Institute of Statistics. Demographic Statistics. Statistical Yearbook 2020; 2020. Available from: http://www.rzs.rs.ba/.
19. Marković PV, Škrbić R, Godman B, Gustafsson LL. Ongoing initiatives in the Republic of Srpska to enhance prescribing efficiency: influence and future directions. Expert Rev Pharmacoecon Outcomes Res. 2012;12:661–671. doi:10.1586/erp.12.48
20. Health Insurance Fund of Republic of Srpska. Drug lists. Available from: https://www.zdravstvo-srpske.org/files/cjenovnici/lijekovi.pdf.
21. Health Insurance Fund of Republic of Srpska. The rights of the insured; 2021. Available from: https://www.zdravstvosrpske.org/files/regulativa/osig/Pravilnik%20o%20son%20ostvarivanja%20prava%20na%20zz.PDF.
22. World Health Organization. Introduction to Drug Utilisation Research. WHO International Working Group for Drug Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology, WHO Collaborating Centre for Drug Utilisation Research and Clinical Pharmacological Services; 2003. Available from: https://apps.who.int/iris/bitstream/handle/10665/42627/924156234X.pdf.
23. Public Health Institute of Republic of Srpska. Analysis of population health in Republic of Srpska, 2019 and 2020. (in Serbian language) Available from: https://www.phi.rs.ba/pdf/publikacije/Izvjestaj%20o%20potrosnji%20lijekova%20za%202019.%20i%202020.%20godinu.pdf.
24. Godman B, Wettermark B, van Woerkom M, et al. Multiple policies to enhance prescribing efficiency for established medicines in Europe with a particular focus on demand-side measures: findings and future implications. Front Pharmacol. 2014;5:106. doi:10.3389/fphar.2014.00106
25. Marković PV, Škrbić R, Petrović A, et al. Polypharmacy among the elderly in the Republic of Srpska: extent and implications for the future. Expert Rev Pharmacoecon Outcomes Res. 2016;16:609–618. doi:10.1586/14737167.2016.1115347
26. OECD. Health at a Glance 2021: OECD Indicators. Paris: OECD Publishing; 2021.
27. Armitage J, Baigent C, Barnes E; Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–415. doi:10.1016/S0140-6736(18)31942-1
28. Stone NJ, Robinson JG, Lichtenstein AH, et al. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129(25):S1–45. doi:10.1161/01.cir.0000437738.63853.7a
29. NICE Clinical Guideline. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. London: National Clinical Guideline Centre; 2014.
30. Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32(14):1769–1818. doi:10.1093/eurheartj/ehr158
31. Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study). Am J Cardiol. 1998;81(5):582–587. doi:10.1016/s0002-9149(97)00965-x
32. Jones PH, Davidson MH, Stein EA, et al.; STELLAR Study Group. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR* Trial). Am J Cardiol. 2003;92(2):152–160. doi:10.1016/s0002-9149(03)00530-7
33. Farnier M. An evaluation of alirocumab for the treatment of hypercholesterolemia, Expert 441Rev. Cardiovasc Ther. 2015;13(12):1307–1323. doi:10.1586/14779072.2015.1111759
34. De Backer G, Jankowski P, Kotseva K, et al. EUROASPIRE V collaborators management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis. 2019;285:135–146. doi:10.1016/j.atherosclerosis.2019.03.014
35. Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388(10059):2532–2561. doi:10.1016/S0140-6736(16)31357-5
36. Yusuf S, Islam S, Chow CK, et al; Prospective 450 Urban Rural Epidemiology (PURE) Study Investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–1243. doi:10.1016/S0140-6736(11)61215-4
37. Börsch-Supan A, Brandt M, Hunkler C, et al; SHARE Central Coordination Team. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013;42(4):992–1001. doi:10.1093/ije/dyt088
38. Martić NB, Zečević DD, Đurđević MV, et al. Comparative analysis of the use of lipid-modifying medicines in the republic of Serbia and Nordic countries in the period 2015–2017. Hospital Pharmacol. 2020;7(3):966–461 975. doi:10.5937/hpimj2003966M
39. Naumovska Z, Nestorovska AK, Grozdanova A, et al. Evaluation of statin utilisation in the Republic of Macedonia during 2013–2016. Clinicoecon Outcomes Res. 2018;10:339–347. doi:10.2147/CEOR.S157842
40. Health Insurance Fund of Republic of Srpska. Medicines - list of indications. Available from: https://www.zdravstvo-srpske.org/files/cjenovnici/lista_ind.pdf.
41. Ruokoniemi P, Helin SA, Klaukka T, Neuvonen PJ, Huupponen R. Shift of statin use towards the elderly in 1995–2005: a nation-wide register study in Finland. Br J Clin Pharmacol. 2008;66(3):405–410. doi:10.1111/j.1365-2125.2008.03258.x
42. Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–602. doi:10.1007/s12471-010-0841-y
43. Rodgers JL, Jones J, Bolleddu SI, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. 2019;6(2):19. doi:10.3390/jcdd6020019
44. Jackevicius CA, Tu JV, Krumholz HM, et al. Comparative effectiveness of generic atorvastatin and lipitor® in patients hospitalized with an acute coronary syndrome. J Am Heart Assoc. 2016;5:e003350. doi:10.1161/JAHA.116.003350
45. Mortensen MB, Falk E, Schmidt M. Twenty-year nationwide trends in statin utilisation and expenditure in Denmark. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003811. doi:10.1161/CIRCOUTCOMES.117.003811
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


