Back to Journals » Infection and Drug Resistance » Volume 16
Elevated High Sensitivity Cardiac Troponin T is Nonlinearly Associated with Poor Prognosis in Aging COVID-19 Patients: A Retrospective Study
Authors Jin X, Yang H, Ma W, Yuan Y, Li T
Received 22 May 2023
Accepted for publication 3 August 2023
Published 9 August 2023 Volume 2023:16 Pages 5155—5163
DOI https://doi.org/10.2147/IDR.S422492
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Xiaxia Jin,1,* Haideng Yang,2,* Weiwei Ma,1,* Yuan Yuan,1 Tao Li3
1Department of Clinical Laboratory, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Linhai, People’s Republic of China; 2Department of Gastroenterology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Linhai, People’s Republic of China; 3Department of Cardiovascular Medicine, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Linhai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuan Yuan, Department of Clinical Laboratory, Taizhou Hospital of Zhejiang Province, 150 Ximen Road, Linhai, Zhejiang Province, People’s Republic of China, Email [email protected] Tao Li, Department of Cardiovascular Medicine, Taizhou Hospital of Zhejiang Province, 150 Ximen Road, Linhai, Zhejiang Province, People’s Republic of China, Email [email protected]
Objective: To evaluate the relationship between high-sensitivity cardiac troponin T (hs-cTnT) and prognosis in elderly patients with coronavirus disease 2019 (COVID-19).
Methods: This study recruited 1399 COVID-19 patients aged 65 years or older admitted to Taizhou Hospital or Enze Hospital in Zhejiang Province from December 15, 2022, to January 4, 2023. The Cox regression model was used to evaluate the relationship between hs-cTnT level and in-hospital death. The logistic regression model was used to evaluate the relationship between hs-cTnT level and major adverse events. The restricted cubic spline (RCS) model is used for nonlinear analysis.
Results: The increase of peak hs-cTnT was associated with the increased risk of death (HR 9.49; 95% CI 1.19– 75.48; trend p = 0.012) and major adverse events (OR 20.59; 95% CI 10.41– 40.71; trend p < 0.001). RCS model showed the association between peak hs-cTnT and death and major adverse events were nonlinear (P for non-line < 0.001). Starting from the limit of quantification of hs-cTnT (3ng/L), the risk of death and major adverse events had a steep S-shaped increase until hs-cTnT reached the 90th percentile point (hs-cTnT = 131 ng/L), followed by a plateau period. Peak hs-cTnT has good predictive value for death and major adverse events, with AUC of 0.834 and 0.804, respectively.
Conclusion: Peak hs-cTnT has high predictive value for the risk of in-hospital death and major adverse events in elderly patients with COVID-19. The association between peak hs-cTnT and death and major adverse events were nonlinear.
Keywords: high-sensitivity cardiac troponin T, elderly, COVID-19, nonlinearly, prognosis
Introduction
The Coronavirus disease 2019 (COVID-19), which has killed at least 7 million people, is a severe challenge to global public health.1 It is noteworthy that COVID-19 related deaths mainly occur in the elderly.2–4 Moreover, the ICU admission rate in older patients with COVID-19 was higher than in younger patients.5 In the past 100 years, human life expectancy has increased significantly.6 According to the World Health Organization survey, the global population over 65 exceeded 700 million in 2019 and will at least double in the next 30 years.7 Therefore, early risk assessment of elderly patients with COVID-19 is crucial to identifying high-risk patients.
Except for typical respiratory manifestations, COVID-19 patients often have cardiac involvement. And its existence is not only related to the severity of the disease but also closely related to adverse outcomes such as death.8–11 High-sensitivity cardiac troponin T (hs-cTnT) is a preferred high sensitivity cardiac injury marker, which will be released into the blood when myocardial tissue is injured.12 Many studies show that the prognosis of COVID-19 patients with elevated hs-cTnT levels is worse. A multicenter retrospective study in the United States found that COVID-19 patients with elevated hs-cTnT levels had a higher risk of death.13 A study of COVID-19 patients in the ICU found that admission hs-cTnT was a predictor for death.14 Similarly, another study involving 2450 hospitalized patients with COVID-19 further confirmed elevated hs-cTnT was associated with an increased risk of death.15 However, there is a non-specific increase in the hs-cTnT level in the elderly. Some scholars found that the 99th percentile hs-cTnT levels of the elderly observed in the general population is three times the reference value.16 Therefore, it is necessary to evaluate the relationship between hs-cTnT and the prognosis of elderly patients with COVID-19.
This study analyzed the relationship between peak hs-cTnT levels and poor prognosis in elderly patients with COVID-19. We explored the prognostic role of hs-cTnT in elderly patients and its ability as a risk stratification tool.
Methods
Study Population
This study was conducted in Taizhou Hospital and Enze Hospital in Zhejiang Province. The hospitalized geriatric COVID-19 patients (age ≥ 65 years old) from December 15, 2022, to January 4, 2023, were analyzed retrospectively. These patients had COVID-19 symptoms and were diagnosed with COVID-19 by nucleic acid or antigen detection. At least one hs-cTnT test was performed. Patients younger than 65, without laboratory diagnosis of COVID-19, and no hs-cTnT test during hospitalization were excluded. This research was approved by the ethics of Taizhou Hospital of Zhejiang Province (k20230116) and conforms to the declaration of Helsinki. As this is a retrospective observational study, informed consent was waived.
Study Variables and Data Extraction
All clinical data were collected through the hospital medical record of Taizhou Hospital and Enze Hospital in Zhejiang Province. (1) General information, including gender, age, and length of stay (LOS). (2) Clinical manifestations, including blood pressure, heart rate, fever, throat discomfort, cough, sputum production, myalgia, fatigue, headache or dizziness, poor appetite, digestive symptoms, chest pain, and chest distress; (3) Coexisting comorbidities, including hypertension, diabetes mellitus (DM), coronary artery disease (CAD), atrial fibrillation (AF), chronic obstructive pulmonary disease (COPD), heart failure (HF), asthma, chronic kidney disease (CKD), cerebrovascular disease, and cancer. (4) Laboratory findings, including white blood cell (WBC) and high-sensitivity C-reactive protein (hs-CRP). Neutrophil-to-lymphocyte (NLR) was calculated as neutrophils count divided by lymphocytes count. (5) Treatment, including intravenous antibiotics, intravenous antivirals, and immune therapy. COVID −19 reporting and data system (CORADS) was evaluated based on the standards developed by Prokop M et al.17 CORADS 6 is not included because it depends on RT-PCR positivity.18
Hs-cTnT Assay
The hs-cTnT was detected by the Roche Cobas E801 electrochemiluminescence instrument (Roche Diagnostics, Germany). The 99th percentile reference upper limit was 14 ng/L, and the minimum detection limit was 3 ng/L.
Peak hs-cTnT values were defined over the duration of hospitality.
Outcomes
The poor prognosis included in-hospital death and major adverse events including shock, respiratory failure requiring mechanical utilization, continuous renal replacement therapy (CRRT), ICU admission, cardiac arrest, and in-hospital death.
Statistical Analysis
R software (version 4.1.2) was used for statistical analysis. Categorical variables are represented by counts (percentages), and continuous variables are represented by median (interquartile distance [IQR]). The participants were divided into four groups according to the quartile of hs-cTnT (≤ 13, 13–23, 23–52, >52ng/L) to analyze the association between the hs-cTnT level and the prognosis of patients with COVID-19. Kruskal Wallis test was used to compare the differences between continuous variables. Chi-squared test or Fisher’s exact test was used to compare the differences between categorical variables. The Cox regression model was used to evaluate the relationship between hs-cTnT level and in-hospital death. The logistic regression model was used to evaluate the relationship between hs-cTnT level and major adverse events. We constructed two progressive adjustment models: model 1 was adjusted according to age and gender; based on model 1, model 2 was adjusted with the addition of fever, throat discomfort, cough, sputum production, myalgia, headache/dizziness, hypertension, DM, AF, CAD, heart failure, cerebrovascular disease, CKD, heart rate, WBC, NLR, hs-CRP, and CORADS.19–22 The restricted cubic spline (RCS) model, adjusted for the same variables as model 2, was used to analyze the association of hs-cTnT level between prognosis. The bilateral P value <0.05 was considered statistically significant.
Results
Baseline Characteristics of the Study Population
As shown in Figure 1, we analyzed the clinical and laboratory data of 1399 elderly patients with COVID-19. The median age of the patients was 77 (IQR, 72–84) years old, 890 (63.6%) males, and the median LOS was 10 (IQR, 7–15) days. Among the included patients, 48 (3.4%) patients died and 231 (16.5%) had major adverse events during hospitalization.
 |
Figure 1 Study flowchart. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; hs-cTnT, high-sensitivity cardiac troponin T. |
The median (IQR) of hs-cTnT was 23 (13–52) ng/L, according to the quartile of hs-cTnT, and the participants were divided into four groups (≤ 13, 13–23, 23–52, >52ng/L). Their baseline characteristics are shown in Table 1. The patients with higher hs-cTnT levels were older, had longer LOS, had higher rates of hypertension, diabetes, AF, CAD, HF, cerebrovascular disease, and CKD, had higher levels of WBC, NLR, and hs-CRP, and had poorer prognosis but had fewer symptoms such as fever, throat discomfort, cough, sputum production, myalgia, and headache or dizziness.
 |
Table 1 Baseline Characteristics of Participants Across Quartiles of Hs-cTnT Levels |
The Relationship Between Peak Hs-cTnT and Prognosis
Figure 2 shows that the peak hs-cTnT level of patients with poor prognosis (death and major adverse events) is higher than that of patients with good prognosis, even if they are grouped according to sex, HP, DM, AF, CAD, HF, and CKD history. Supplementary Figure 1 shows that the risk of in-hospital death in the four groups increased in turn. Table 2 shows that compared with the first quartile of hs-cTnT, the fully adjusted HR of death from the third to the fourth quartile in model 2 is 2.91 (0.35–24.31) and 9.49 (1.19–75.48), respectively (p = 0.012 for trend); The adjusted OR of major adverse events from the second to the fourth quartile were 2.23 (1.08–4.60), 4.98 (2.50–9.89) and 20.59 (10.41–40.71), respectively (p<0.001). And the HR and OR were adjusted for sex, age, fever, throat discomfort, cough, sputum production, myalgia, headache/dizziness, hypertension, DM, AF, CAD, HF, cerebrovascular disease, CKD, heart rate, WBC, NLR, hs-CRP, and CORADS score.
 |
Table 2 Odds Ratios or Hazard Ratios and 95% CI of Prognosis for Quartiles of Hs-cTnT |
Elevated Hs-cTnT Nonlinearly Associated with Poor Prognosis in Aging COVID-19 Patients
The RCS model showed the association between peak hs-cTnT and death and major adverse events were nonlinear after adjusting for sex, age, fever, throat discomfort, cough, sputum production, myalgia, headache/dizziness, hypertension, DM, AF, CAD, HF, cerebrovascular disease, CKD, heart rate, WBC, NLR, hs-CRP, and CORADS score (P for non-linearity < 0.001). Starting from the limit of quantification of hs-cTnT (3 ng/L), the risk of death and major adverse events had a steep S-shaped increase until hs-cTnT reached the 90th percentile point (hs-cTnT = 131 ng/L), followed by a plateau period (Figure 3).
Comparison of Dynamic Changes of Hs-cTnT During the Hospitalization
During hospitalization, the hs-cTnT level of elderly patients with COVID-19 in the death or major adverse events groups maintained at a high level. In addition, regardless of the outcome, the hs-cTnT level of elderly patients with COVID-19 was higher than the reference value of our laboratory (≤ 14 ng/L) (Supplementary Figure 2).
Performance of Peak Hs-cTnT as a Biomarker for a Different Outcome
As shown in Figure 4, peak hs-cTnT has good predictive value for death and major adverse events, with AUCs of 0.834 and 0.804, respectively.
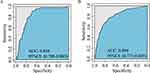 |
Figure 4 ROC analysis of hs-cTnT for death (A) and major adverse events (B). |
Discussion
This study analyzed the relationship between peak hs-cTnT levels and prognosis in 1399 hospitalized patients with COVID-19 and the trends of hs-cTnT levels during hospitalization. We found that: (1) high peak hs-cTnT level was an independent risk factor for poor prognosis in elderly patients with COVID-19. (2) Peak hs-cTnT was nonlinear correlated with poor prognosis. Starting from the limit of quantification of hs-cTnT (3 ng/L), the risk of death and major adverse events had a steep S-shaped increase until hs-cTnT reached 131 ng/L, followed by a plateau period. (3) During hospitalization, the hs-cTnT level of aging COVID-19 patients in the poor prognosis group was always maintained at a high level.
Our research has several significant and unique advantages. (1) It uses hs-cTn measurement, which has higher sensitivity than the ordinary cardiac troponin measurement, and slight myocardial damage can be detected. (2) We found that the higher the peak hs-cTnT level, the higher the risk of poor prognosis. The mortality risk curve tended to be stable when the level of hs-cTnT was higher than 131 ng/L. (3) We analyzed the dynamic changes in hs-cTnT level during hospitalization.
Hs-cTnT is the most sensitive biomarker of myocardial injury and is widely used in the diagnosis of cardiovascular diseases. However, hs-cTnT may be nonspecific elevated in male patients and patients with hypertension, diabetes, and chronic kidney disease.23–26 To rule out the impact of these diseases on the results, we divided the patients into two groups according to sex, HP, DM, AF, CAD, HF, and CKD history and compared the hs-cTnT levels of patients with poor prognosis and patients with good prognosis. We found that the hs-cTnT levels in patients with poor prognosis were always higher than those patients with good prognosis. Therefore, the results of this study can be extended to all elderly patients hospitalized for COVID-19.
Hs-cTnT as a marker related to the prognosis of COVID-19 has received extensive attention.27,28 A Danish study of 346 patients with COVID-19 found that dynamic changes of hs-cTnT changes were associated with death.29 Other research had found that hs-cTnT can predict the in-hospital death in aging COVID-19 patients.30 Similarly, we also observed that older patients with elevated hs-cTnT had a higher risk of death. A study of 367 COVID-19 patients found that hs-cTnT was a predictor of major adverse events.13 Our study confirmed that hs-cTnT was also an independent risk factor for major adverse events in elderly patients with COVID-19.
Our study also found that the hs-cTnT level was S-shaped and correlated with the risk of death and major adverse events, and the risk curve tended to be stable after the level of hs-cTnT > 131 ng/L. An Italian study of 343 patients older than 60 with COVID-19 also found a similar phenomenon. They pointed out that the level of cardiac troponin I (cTnI) was linearly correlated with mortality before 0.3μg/L, followed by a plateau period.31 However, this study only confirmed the relationship between cTnI and mortality. Our study not only confirmed the relationship between hs-cTnT level and mortality but also found the nonlinear relationship between hs-cTnT level and major adverse events, and we used high-sensitivity troponin T with higher sensitivity.
There are the following areas for improvement in this study. First, because this study was carried out at the peak of COVID-19 infection in China, and the medical resources were relatively insufficient, only patients with severe illness could be hospitalized, and not all COVID-19 patients were tested for hs-cTnT, and this study was only aimed at Taizhou, China, which may lead to the existence of selective bias. Secondly, this study is a retrospective study, and the monitoring of hs-cTnT is not at a fixed time. Finally, this study only analyzed the state of patients at discharge and did not carry out long-term follow-up of patients.
Conclusion
Our study proved the predictive effect of hs-cTnT on the risk of in-hospital death and major adverse events such as ICU admission and shock in elderly patients with COVID-19. When peak hs-cTnT level is higher than 131 ng/L, the risk of death and major adverse events will not increase significantly with the increase of peak hs-cTnT level.
Abbreviations
COVID-19, coronavirus disease 2019; SARS-COV-2, severe acute respiratory syndrome coronavirus 2; hs-cTnT, high-Sensitivity Cardiac Troponin T; LOS, length of stay; HR, heart rate; SBP, systolic pressure; DBP, diastolic pressure; bpm, beats per minute; DM, diabetes mellitus; AF, atrial fibrillation; CAD, coronary artery disease; HF, heart failure; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; CRRT, continuous renal replacement therapy; IQR, interquartile distance; RCS, restricted cubic spline; CORADS, COVID-19 Reporting and Data System; WBC, white blood cell; NLR, neutrophil-to-lymphocyte; hs-CRP, high sensitivity C-reactive protein.
Data Sharing Statement
The data that support the findings of this study will be available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the ethics committee of Taizhou hospital in Zhejiang Province (approval number: k20230116) and conformed to the declaration of Helsinki. As a retrospective study, this study only collected clinical data of patients without interfering with the treatment plan of patients, which will not bring physiological risks to patients. Therefore, the ethics committee did not require informed consent. The researchers will protect the information provided by patients to avoid disclosing personal privacy or breaching confidentiality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from Taizhou Municipal Science and Technology Bureau (22ywa12).
Disclosure
The authors declare that they have no conflicts of interest to this work.
References
1. Vosko I, Zirlik A, Bugger H. Impact of COVID-19 on cardiovascular disease. Viruses. 2023;15(2). doi:10.3390/v15020508
2. Ramos-Rincon JM, Buonaiuto V, Ricci M, et al. Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain. J Gerontol a Biol Sci Med Sci. 2021;76(3):e28–e37. doi:10.1093/gerona/glaa243
3. Henkens M, Raafs AG, Verdonschot JAJ, et al. Age is the main determinant of COVID-19 related in-hospital mortality with minimal impact of pre-existing comorbidities, a retrospective cohort study. BMC Geriatr. 2022;22(1):184. doi:10.1186/s12877-021-02673-1
4. Bonafe M, Prattichizzo F, Giuliani A, Storci G, Sabbatinelli J, Olivieri F. Inflamm-aging: why older men are the most susceptible to SARS-CoV-2 complicated outcomes. Cytokine Growth Factor Rev. 2020;53:33–37. doi:10.1016/j.cytogfr.2020.04.005
5. Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020;80(6):e14–e18. doi:10.1016/j.jinf.2020.03.005
6. Amuthavalli Thiyagarajan J, Mikton C, Harwood RH, et al. The UN Decade of healthy ageing: strengthening measurement for monitoring health and wellbeing of older people. Age Ageing. 2022;51(7). doi:10.1093/ageing/afac147
7. Rehatta NM, Chandra S, Sari D, et al. Comorbidities and COVID-19 status influence the survival rate of geriatric patients in intensive care units: a prospective cohort study from the Indonesian Society of Anaesthesiology and Intensive Therapy. BMC Geriatr. 2022;22(1):523. doi:10.1186/s12877-022-03227-9
8. Jansson S, Blixt PJ, Didriksson H, et al. Incidence of acute myocardial injury and its association with left and right ventricular systolic dysfunction in critically ill COVID-19 patients. Ann Intensive Care. 2022;12(1):56. doi:10.1186/s13613-022-01030-8
9. Efros O, Barda N, Meisel E, et al. Myocardial injury in hospitalized patients with COVID-19 infection-Risk factors and outcomes. PLoS One. 2021;16(2):e0247800. doi:10.1371/journal.pone.0247800
10. Chu X, Zhang GF, Zheng YK, et al. Clinical features and risk factors of severely and critically ill patients with COVID-19. World J Clin Cases. 2022;10(3):840–855. doi:10.12998/wjcc.v10.i3.840
11. Ruzzenenti G, Maloberti A, Giani V, et al. Covid and Cardiovascular Diseases: direct and Indirect Damages and Future Perspective. High Blood Press Cardiovasc Prev. 2021;28(5):439–445. doi:10.1007/s40292-021-00464-8
12. Januzzi JL, Mahler SA, Christenson RH, et al. Recommendations for Institutions Transitioning to High-Sensitivity Troponin Testing: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;73(9):1059–1077. doi:10.1016/j.jacc.2018.12.046
13. De Michieli L, Ola O, Knott JD, et al. High-Sensitivity Cardiac Troponin T for the Detection of Myocardial Injury and Risk Stratification in COVID-19. Clin Chem. 2021;67(8):1080–1089. doi:10.1093/clinchem/hvab062
14. Demir OM, Ryan M, Cirillo C, et al. Impact and Determinants of High-Sensitivity Cardiac Troponin-T Concentration in Patients With COVID-19 Admitted to Critical Care. Am J Cardiol. 2021;147:129–136. doi:10.1016/j.amjcard.2021.01.037
15. Khaloo P, Shaqdan A, Ledesma PA, et al. Distinct etiologies of high-sensitivity troponin T elevation predict different mortality risks for patients hospitalized with COVID-19. Int J Cardiol. 2022;351:118–125. doi:10.1016/j.ijcard.2021.12.029
16. Lowry MTH, Doudesis D, Wereski R, et al. Influence of Age on the Diagnosis of Myocardial Infarction. Circulation. 2022;146(15):1135–1148. doi:10.1161/CIRCULATIONAHA.122.059994
17. Prokop M, van Everdingen W, van Rees Vellinga T, et al. CO-RADS: a Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020;296(2):E97–E104. doi:10.1148/radiol.2020201473
18. Yildirim Ayaz E, Coskun ZU, Kaplan M, et al. Comparison of Initial CT Findings and CO-RADS Stage in COVID-19 Patients with PCR, Inflammation and Coagulation Parameters in Diagnostic and Prognostic Perspectives. J Belg Soc Radiol. 2022;106(1):67. doi:10.5334/jbsr.2714
19. Inanc IH, Bursa N, Gultepe A, Bayramoglu M, Sabanoglu C, Inanc FA. Association among CO-RADS score, co-morbid diseases, and short-term prognosis in COVID-19 infection. Eur Rev Med Pharmacol Sci. 2022;26(2):653–663. doi:10.26355/eurrev_202201_27892
20. Villoteau A, Asfar M, Otekpo M, et al. Elevated C-reactive protein in early COVID-19 predicts worse survival among hospitalized geriatric patients. PLoS One. 2021;16(9):e0256931. doi:10.1371/journal.pone.0256931
21. Maloberti A, Giannattasio C, Rebora P, et al. Incident Atrial Fibrillation and In-Hospital Mortality in SARS-CoV-2 Patients. Biomedicines. 2022;10(8). doi:10.3390/biomedicines10081940
22. Maloberti A, Ughi N, Bernasconi DP, et al. Heart Rate in Patients with SARS-CoV-2 Infection: prevalence of High Values at Discharge and Relationship with Disease Severity. J Clin Med. 2021;10(23). doi:10.3390/jcm10235590
23. Welsh P, Preiss D, Shah ASV, et al. Comparison between High-Sensitivity Cardiac Troponin T and Cardiac Troponin I in a Large General Population Cohort. Clin Chem. 2018;64(11):1607–1616. doi:10.1373/clinchem.2018.292086
24. McCarthy CP, Yousuf O, Alonso A, Selvin E, Calkins H, McEvoy JW. High-Sensitivity Troponin as a Biomarker in Heart Rhythm Disease. Am J Cardiol. 2017;119(9):1407–1413. doi:10.1016/j.amjcard.2017.01.032
25. Chesnaye NC, Szummer K, Barany P, et al. Association Between Renal Function and Troponin T Over Time in Stable Chronic Kidney Disease Patients. J Am Heart Assoc. 2019;8(21):e013091. doi:10.1161/JAHA.119.013091
26. Chaulin A. Cardiac Troponins: contemporary Biological Data and New Methods of Determination. Vasc Health Risk Manag. 2021;17:299–316. doi:10.2147/VHRM.S300002
27. Maloberti A, Biolcati M, Giannattasio C. Troponin elevation in COVID-19 patients: an important stratification biomarker with still some open questions. Int J Cardiol. 2021;341:107–109. doi:10.1016/j.ijcard.2021.07.049
28. Maino A, Di Stasio E, Grimaldi MC, et al. Prevalence and characteristics of myocardial injury during COVID-19 pandemic: a new role for high-sensitive troponin. Int J Cardiol. 2021;338:278–285. doi:10.1016/j.ijcard.2021.06.028
29. Polcwiartek C, Krogager ML, Andersen MP, et al. Prognostic implications of serial high-sensitivity cardiac troponin testing among patients with COVID-19: a Danish nationwide registry-based cohort study. Am Heart J Plus. 2022;14:100131. doi:10.1016/j.ahjo.2022.100131
30. Menditto A, Protic O, Di Rosa M, Bonfigli AR, Lattanzio F, Antonicelli R. Admission high-sensitivity cardiac troponin levels as a prognostic indicator for in-hospital mortality rates in the elderly and very elderly COVID-19 patients. Arch Gerontol Geriatr. 2023;104:104822. doi:10.1016/j.archger.2022.104822
31. De Marzo V, Di Biagio A, Della Bona R, et al. Prevalence and prognostic value of cardiac troponin in elderly patients hospitalized for COVID-19. J Geriatr Cardiol. 2021;18(5):338–345. doi:10.11909/j.issn.1671-5411.2021.05.004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


