Back to Journals » Orthopedic Research and Reviews » Volume 11
Electrodiagnostic Findings in 441 Patients with Ulnar Neuropathy - a Retrospective Study
Authors Raeissadat SA, Youseffam P, Bagherzadeh L , Rayegani SM , Bahrami MH, Eliaspour D
Received 6 September 2019
Accepted for publication 11 November 2019
Published 2 December 2019 Volume 2019:11 Pages 191—198
DOI https://doi.org/10.2147/ORR.S230116
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Seyed Ahmad Raeissadat,1 Parisa Youseffam,2 Leila Bagherzadeh,3 Seyed Mansoor Rayegani,4 Mohammad Hasan Bahrami,4 Dariush Eliaspour5
1Clinical Development Research Center of Shahid Modarres Hospital, Physical Medicine and Rehabilitation Department and Research Center, Shahid Beheshti University of Medical Sciences, School of Medicine, Tehran, Iran; 2Clinical Development Research Center of Shahid Modarres Hospital, Physical Medicine and Rehabilitation Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 3Department of Orthopedics, Faculty of Medicine, Zabol University of Medical Sciences, Zabol, Iran; 4Physical Medicine and Rehabilitation Research Center, Shohada-E-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 5Physical Medicine and Rehabilitation Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Correspondence: Leila Bagherzadeh
Department of Orthopedics, Faculty of Medicine, Zabol University of Medical Sciences, Zabol, Iran
Tel/Fax +989122213218
Email [email protected]
Purpose: Ulnar neuropathy (UN) is the second most common focal neuropathy in the upper extremities. Electrodiagnostic studies (EDx), including nerve conduction study (NCS) and electromyography (EMG), are reliable tools for the diagnosis of ulnar neuropathy. We aimed to retrospectively analyze the medical records of patients diagnosed with ulnar neuropathy in a seven-year period and report our findings.
Patients and methods: In this retrospective study, documents of the patients whose ulnar nerve injury was confirmed through electrodiagnostic study in two departments of Physical Medicine and Rehabilitation were collected and demographic data, subjective complaints of the patient, the cause, and electrodiagnostic findings were extracted from each patient’s file. The following points were specifically evaluated in the electrodiagnostic records; type of injury, location, accompanying injuries, sensory nerve action potentials (SNAP) of the fifth finger, SNAP of dorsal ulnar cutaneous nerve (DUCN), compound muscle action potential (CMAP) of abductor digiti minimi (ADM) muscle, nerve conduction velocity (NCV) across elbow, patterns of muscle involvement, and the severity of insult.
Results: Out of 441 records, 305 (69.2%) were male and 68.1% were non-traumatic. Based on our clinical criteria, the intensity of the injury was mild in most cases. The elbow and forearm were the most involved regions in non-traumatic and traumatic cases respectively. Across elbow nerve conduction velocity showed decreased velocity in 71% of records. In non-traumatic cases, the most affected muscle was ADM (97%) and then FDI (85%).
Conclusion: In focal entrapments such as ulnar neuropathy, electrodiagnostic findings are very helpful in assessing location, severity, and type of injury. If a consensus is achieved for the diagnosis of UN, even retrospective studies can become valuable sources for studying UN.
Keywords: ulnar nerve, electrodiagnostic study, nerve lesion
Introduction
After carpal tunnel syndrome, ulnar neuropathy is the second most commonly occurring neuropathy of the upper extremities.1,2 As the ulnar nerve passes a relatively long distance in the upper extremity, it becomes vulnerable to traumatic and non-traumatic lesions.
A clear understanding of ulnar nerve anatomy is necessary to accurately locate the affected area of the nerve. The ulnar nerve carries both sensory and motor fibers. As it descends through the arm region, it descends down the arm and passes posterior to the medial epicondyle into the forearm between the two heads of the flexor carpi ulnaris (FCU) muscle. Continuing distally, it crosses superficially to the flexor retinaculum into the hand. Approximately 10 cm above the wrist, the dorsal ulnar cutaneous nerve (DUCN) originates from the main stem of the ulnar nerve. At the wrist, the ulnar nerve passes the Guyon canal and gives off deep and superficial branches. The superficial branch of the ulnar nerve innervates the palmaris brevis muscle. The deep branch splits into its terminal branches innervating the hypothenar area, the lumbericals and interosseous muscles.3 The transverse portion of adductor pollicis (AP) and first dorsal interosseous (FDI) are the last muscles innervated by the ulnar nerve.
Although the ulnar nerve is most commonly affected at the elbow, this can also happen at the upper arm, forearm, and wrist.4,5 The most common causes of nerve lesion at elbow are entrapment by ligaments and external compression. Symptoms of ulnar neuropathy (UN) may start acutely or insidiously, the former more commonly occurring with trauma. Weakness of ulnar nerve innervated intrinsic hand muscles can also be seen in severe or prolonged lesions.2
When used appropriately in combination with physical examination; electrodiagnostic studies (EDx), including nerve conduction studies (NCSs) and electromyography (EMG), are essential tools in diagnosis of ulnar neuropathy.3,4,6,7 While the use of ultrasound and MRI has become a growing diagnostic tool, EDx continue to be the cornerstone of diagnosis.8–10
The goal of electrodiagnosis is to confirm that the lesion is confined to the ulnar nerve, localize ulnar nerve dysfunction, and to assess the severity.2,11,12 In traumatic cases, the electrodiagnostic test assists with both diagnosis of the injury and predicting outcome.13
Tests used by the electrodiagnostic provider to assist in diagnosis include needle EMG, motor nerve conduction study (NCS) of ulnar innervated muscles in the hand, and sensory NCSs. Furthermore, ulnar nerve conduction latencies, amplitudes, waveforms, and velocities can be compared across the elbow segment to localize injury to the elbow. Despite a variety of tests being available, the diagnosis of UN can still be challenging and controversial.2,9,14–18
Sensory Responses
The ulnar sensory nerve action potential (SNAP) of the fifth digit is a finding which has a high sensitivity and is impaired in most cases of ulnar neuropathy.19 Another sensory response of the ulnar nerve is dorsal ulnar cutaneous nerve sensory nerve action potential (DUCN SNAP).
Motor Response
Compound muscle action potential (CMAP) of the ulnar nerve is routinely measured through stimulation of the ulnar nerve and measuring the motor response through the ADM muscle. The stimulus is performed at the wrist, above and below the elbow region, while NCV is measured at the forearm and across elbow. An NCV less than 50m/s in the elbow region is the most sensitive finding in the diagnosis of ulnar neuropathy at the elbow (UNE).14
Inching Short Segment
Another diagnostic method is the inching short segment nerve conduction studies. In this technique, a series of points, each at a 1 cm distance, are stimulated and a change in latency of more than 0.4 ms indicates a lesion in that area.
The Across Elbow Region Length
To obtain across elbow nerve conduction velocity (NCV), one should stimulate the ulnar nerve below and above elbow region while measuring the distance to calculate velocity. Nevertheless, there is debate surrounding this method. In the AAEM guideline, 10 cm has been suggested as the optimal distance for two stimulation sites. Recently, in a study by Omejec et al, it has been proposed that if the results of using 10 cm across elbow segments are negative, adding 2 stimulating points in the elbow region may help increase the sensitivity of the diagnosis of UN at the elbow.16 In addition, this study has stated that measuring CMAP from both the abductor digiti minimi (ADM) and first dorsal interosseous (FDI) muscles has no additional effect on the sensitivity of across elbow studies.
Electromyography (EMG)
According to the AAEM guideline for ulnar neuropathy at the elbow, performing a needle exam on the FDI and ADM muscles has been recommended, while assessment of flexor digitorum profundus (FDP) and flexor carpi ulnaris (FCU) has been considered optional.
After this brief introduction to electrodiagnostic studies routinely applied for ulnar neuropathy, it is worth mentioning that with the increase in high quality literature in this area, a variety of techniques have been suggested in the diagnosis of UN; nonetheless, the time-consuming and invasive nature of EDx may negatively impact the compliance of patients in continuing the diagnostic studies. For this reason, a consensus must be reached regarding the most sensitive and time-efficient methods that increase patients’ compliance and result in more time-efficient ways which all have a role in the final diagnosis.
Our aim in this study was not to discuss electrodiagnostic patterns of ulnar neuropathy. Nonetheless, we aimed to retrospectively analyze the medical records of patients diagnosed with ulnar neuropathy in a seven-year period and report our findings.
Materials and Methods
After obtaining the appropriate ethical approval from the local ethics committee, patients' records (diagnosed with ulnar neuropathy) were screened in our database over a seven-year period (2008–2015).
Nine records were not included in the analysis due to incomplete data. For the remaining 441 records, demographic data including age, gender, symptoms, causes of lesion and electrodiagnostic results were charted in special layouts. Their electrodiagnostic records were reviewed and the following points were noted: type of injury (demyelinating vs axonal), ulnar SNAP of the fifth finger, SNAP of dorsal ulnar cutaneous nerve, accompanying injury, (CMAP) of ulnar nerve, nerve conduction velocities across elbow, effects of ulnar nerve injury on corresponding muscles, and regeneration in these muscles.
In our department, we perform antidromic ulnar SNAP of the fifth finger. To obtain the response, a surface electrode is placed on the proximal phalanx of the fifth digit as an active electrode and the reference electrode is fixed 4 cm distally. Wrist stimulation is performed 14 cm proximal to the active electrode, near the tendon of the flexor carpi ulnaris at the wrist.20 Dorsal ulnar cutaneous nerve (DUCN) SNAP is measured by placing the active electrode along the dorsum of the fifth metacarpal bone and the reference 4 cm distal. Stimulation is applied 8 to 10 cm proximal to the ulnar styloid between the flexor carpi ulnaris and ulna.20
For ulnar CMAP, the standard technique in our laboratory is ulnar motor response recording from the abductor digiti minimi (ADM). The active electrode is placed over the belly of the abductor digiti minimi (ADM) while the reference electrode is attached to the proximal phalanx of the fifth digit. The elbow is flexed to 90 degrees and stimulation is applied at 3 points: at wrist, 8 cm proximal to the active electrode, just lateral to the flexor carpi ulnaris tendon, the elbow approximately 3 to 4 cm distal to the medial epicondyle, and mid-arm about 6 to 8 cm proximal to the medial epicondyle, between the biceps and medial head of the triceps. A low-amplitude AE (and BE) ulnar CMAP (<5 mV in our laboratory) is suggestive of ulnar neuropathy. Amplitude reduction of more than 50% across elbow is considered as conduction block.14,16,21,22 Depending on across elbow findings, we may perform the inching technique as well. On the basis of NCS findings, we perform EMG studies with standard concentric method on appropriate muscles of the upper extremity including flexor carpi ulnaris (FCU), (FDP), first dorsal interosseous (FDI), and abductor digiti minimi (ADM).22,23 We routinely pierce FDI for assessment of ulnar lesions.
To classify the severity of lesion we considered mild cases as reduction of ulnar SNAP, mild neurogenic findings in ulnar innervated muscles without reduction in recruitment. Severe cases were those with absent SNAP or CMAP or significant recruitment decrease in the relevant muscles. We considered some cases as moderate if they were neither mild nor severe. It should be noted that this categorization was based on expert opinion in our clinics and is not mentioned in other articles.
Since we had assessed patients’ records retrospectively, we had some missing data, which are presented in results. SPSS software for windows v.22 (IBM Corp., Chicago, IL, USA) was used for data analysis.
Results
Out of 450 records, nine were omitted because of missing data; the remaining 441 were entered into the study. 69.2% of patients were male. Mean (SD) age of patients was 46.5 (19.1) years old, with symptom duration, on average, of 16.4 (9.08) months. The mean age of females was significantly higher (p-value=0.005). The right side alone was affected in 44.8% and the left side in 41.4%; while bilateral involvement accounted for 13.9% of cases (Table 1). Among the symptoms, sensory complaints had the highest rate with a prevalence of 36.5% (Table 2).
 |
Table 1 Patients’ Characteristics |
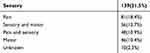 |
Table 2 Frequency of Patients’ Complaints |
Our findings were categorized based on the site of the lesion and etiology. We had two groups regarding area of neuropathy: involvements at the elbow (UNE) versus involvements at all other areas. Based on etiology there were also two groups: traumatic (T) in addition to non-traumatic (NT).
Involvement of the elbow region was the most common, which would reach up to 71% in non- traumatic cases, whereas when the cause was traumatic, the forearm was mostly involved (30.9%) (Table 3).
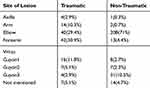 |
Table 3 Localization in Traumatic vs Non-Traumatic Ulnar Neuropathy |
In 31.9% of cases, trauma was the cause of nerve damage. In traumatic injuries (TI) of the ulnar nerve, a significantly lower mean age was observed (p-value=0.001) (Table 4).
 |
Table 4 Relationship Between Etiology, Gender, and Severity |
Severity of involvement was mild in 61.7% of patients, moderate in 18.4%, and severe in 19.7%. Most of the traumatic cases were severe. Regarding disease severity and gender, severity was generally higher in males, although no significant difference was observed between the severity of disease in men and women in both TI and NTI groups (Table 4).
Severity of disease was lower in the higher mean ages, although no significant difference was seen between any of the groups (Table 5).
 |
Table 5 Association of Age and Lesion Severity |
Regarding electrodiagnostic studies, fifth finger SNAP amplitude was normal in 32%, reduced in 30%, and absent in 35%. The SNAP peak latency of the ulnar nerve of the fifth finger was normal in 79% and increased in 19.7%.
Ulnar nerve’s motor response (ulnar nerve CMAP) was normal in 47.6% and showed a reduction in amplitude in 34%.
Type of nerve insult in traumatic and non-traumatic cases is summarized in Table 6.
 |
Table 6 Type of Nerve Pathophysiology |
While evaluating the needle EMG findings, FDI was the most evaluated muscle and FDP the least; their presence in the records was 58.7 and 4.08%, respectively. In cases with UNE, ADM was the most commonly involved muscle (97%); followed by FDI (85%) (Table 7).
 |
Table 7 Findings in Ulnar Neuropathies at Elbow |
In general assessment, nerve conduction velocity in the elbow segment was registered in 58.7% of the records. 84% of these cases were non-traumatic, from which 75% showed a reduced NCV (Table 8).
 |
Table 8 Association Between Lesion Type and Across Elbow Nerve Conduction Velocity (NCV) |
Assessment of UNE showed that 83.8% of injuries were non-traumatic, among which, in 79%, nerve conduction speed across the elbow had been reported. 94.8% of the NTIs showed reduced conduction velocity. Among the non-traumatic UNE, 94.8% showed reduction in conduction velocity (Table 7). UNE was bilateral in 12.2% of cases. Left side and right side lesions were 45.9% and 41.9% respectively.
Regarding coexisting disease, in both TI and NTI groups, solitary ulnar nerve involvement without any other involvements was the most common (Tables 9 and 10).
 |
Table 9 Concomitant Nerve Lesion in Traumatic Lesions |
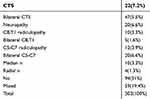 |
Table 10 Concomitant Nerve Lesion in Non-Traumatic Lesions |
Dorsal ulnar cutaneous nerve (DUCN) SNAP was present in 17% of records, among which 40% showed abnormal response. Abnormal responses of DUCN SNAP (reduced amplitude or no response) were reported in 54.8% of cases having axonal damage in the elbow region, and 51.9% in mixed injury. In all cases of pure demyelinating lesions, dorsal ulnar sensory response was normal (Table 11).
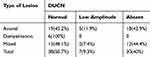 |
Table 11 Relationship Between DUCN Sensory Nerve Action Potential and Type of Lesion |
Discussion
Electrodiagnostic studies (EDx) are considered the standard method for evaluation of ulnar neuropathy. Since most ulnar neuropathies occur at the elbow, the majority of studies on the ulnar nerve focus on this region. Recently EDx protocol for UNE was recommended by Omejec G.17 Contrary to most studies, which focus on UNE, in this research we retrospectively evaluated EDx studies of all ulnar neuropathy cases. To the best of our knowledge, this is the only research work to retrospectively study this number of ulnar neuropathy cases. In our research both TI and NTI cases of ulnar nerve lesions were included, although NTIs comprised the majority.
Although the ulnar nerve can be damaged in any part of its path, this occurs in the elbow region more often, especially in non-traumatic cases.22,24 This is in concordance with our findings.
Both non-traumatic (NT) and traumatic injuries (TI) were more common among men rather than women.25,26 Other studies on ulnar neuropathy at elbow (UNE) have also reported this gender-related difference.4,5,27–29 The mean age of onset was significantly lower in males compared to females. Regarding gender distribution, men had more severe involvement than women, and no significant difference was found between men and women in T and NT groups. The overall results showed higher severity in lower ages, with no significant difference between T and NT groups. These findings can be explained by the fact that men of younger age are more involved in traffic accidents and work-related injuries.
Regarding the affected side, our study did not find a meaningful difference between left and right side involvement in NTI and TI cases. This is different from the study of Omejec et al which reported UNE to be more common on the left side.16 This could be attributed to our study’s assessment of the UN throughout the whole nerve’s pathway instead of the elbow alone.
In a study by Todnem et al in 2009, 127 patients with clinical and EDx findings of UNE were evaluated. Paresthesia (95%) was reported to be more common than weakness (48%), which was similar in our study.17
According to Eser’s report, ulnar nerve damage is the most common injury following upper limb trauma, which is often caused by road traffic accidents.26 In our study, one third of the TI cases occurred in the forearm region and were caused by road traffic accidents. The forearm is usually the most exposed part to trauma, which may explain this finding.
To date, a multitude of research regarding EDx studies focusing on ulnar neuropathy has been published. Because of the high prevalence of ulnar neuropathy at elbow, the majority of these studies have focused on this region. Although our study covers EDx findings in the whole anatomic length of the nerve, we also focused on the elbow region. The diagnosis of UNE has always been challenging and various opinions have been published about it. Newer methods for localization of injury in UNE have also been suggested.30 Since discussing the most appropriate EDx methods in detail is not within the scope of this study, we will just suffice with a brief review.
The studies performed on UNE have largely focused on sensory and motor nerve conduction studies. In Kern’s research, the most reliable finding in UNE was slowing of across elbow NCV to lower than 50 m/sec.14 Attention to the position of elbow, anatomical variations of innervation and temperature are important factors to consider while performing an across elbow conduction study.2,12,21 In a recent study by Omejec, the role of utilizing short-segment nerve conduction studies (SSNCSs) in localizing entrapment of the ulnar nerve at the elbow was evaluated.16 In our research, during general assessment, across elbow nerve conduction velocity (NCV) was mentioned in the records in 60% of cases, of which 84% were NT and of these, 75% showed a reduction in conduction speed.
In a study which evaluated DUCN sensory reduction in UNE, 25 patients had conduction block or slowing across the elbow. In 15 of these cases (60%), DUCN SNAP was normal. This study suggests that DUCN is not reliable in localization of ulnar nerve lesions at the elbow.31 In our study, DUCN SNAP was noted in 17% of the records; among which 40% had abnormal responses. The low number of DUCN SANP mentioned in our clinic records could be due to the difficult and time-consuming nature of this method, or because the diagnosis had already been reached without taking these measurements.
Our study confirmed the finding of the previous studies regarding needle EMG results. In non-traumatic UN of the elbow region, ADM was the most frequently involved muscle (97%), followed by FDI with 85%.16,22,32 This can be explained by difference in topography of fascicles within the nerve, meaning nerve fibers of these two muscles are more prone to damage in the elbow area.29,32
In the previous studies, severity of UN was not mentioned. There are no definite criteria for severity of ulnar neuropathy. After reviewing the records, we categorized the severity based on our own clinic’s criteria, which were mentioned in Table 1. Severity of involvement in our cases was 61.7% mild, 18.4% moderate, and severe in 19.7%. In most of the traumatic cases, severe involvement had been reported.
Since data for this study were gathered from patient records, some data such as weight and height, occupation, exact reason of trauma and degree of improvement over time in serial assessments had not been registered.
Difference of opinion exists in normal values for ulnar sensory and motor responses among various references and EDx specialists. This caused our references to be a range of different numbers that had led to the diagnosis stated in that record.
In some records, despite mentioning the diagnosis of ulnar neuropathy, its axonal or demyelinating nature, and the location of involvement, NCS parameters confirming this diagnosis, such as amplitude, sensory and motor response and NCV in the elbow region had not been mentioned. NCV was only recorded in 58.7% and DUCN in 17% of records. Since our study was performed in a teaching university clinic with changes of shifts and work periods, different doctors were responsible for recording patient information. The discrepancy observed in the records can be explained by lack of a proper record-keeping protocol.
The strengths of the study include a high number of cases, simultaneous assessment of traumatic and non-traumatic cases, and inclusion of all the ulnar neuropathies anywhere in the course of the nerve.
Conclusion
Considering the importance of EDx studies of ulnar neuropathies as well as the value of knowledge about the severity, location, and type of injury in the treatment protocol, we recommend the preparation of a comprehensive, step by step EDx guideline for UN in which all stages from history and physical examination to EDx are documented. In preparation of these guidelines, and in addition to use of the techniques mentioned in the literature, standard methods of measurement including a standard for positioning during taking measurements must be performed. If this is achieved, even retrospective studies can become valuable sources for studying UN.
Abbreviations
UN, ulnar neuropathy; EDx, electrodiagnostic studies; NCS, nerve conduction study; EMG, electromyography; NCV, nerve conduction velocity; NAP, sensory nerve action potentials; DUCN, dorsal ulnar cutaneous nerve; CMAP, compound muscle action potential; ADM, abductor digiti minimi; FDP, flexor digitorum profundus; FCU, flexor carpi ulnaris; AP, adductor pollicis; UNE, ulnar neuropathy at the elbow; AAEM, American Association of Electrodiagnostic Medicine; AE, above elbow; BE, below elbow; NTI, non-traumatic injury; TI, traumatic injury; SSNCSs, short-segment nerve conduction studies.
Ethics Approval and Consent to Participate
The data of the research have been employed from hospital records of patients who have signed and stated their consent for using their not-identifying data for the aim of research. The study was approved by ethics committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran
Availability of Data and Materials
The data of the research are based on hospital records that are available as a part of hospital HIS (Health Information System). It should be mentioned that in all Iranian public hospitals, data of patients are electronically recorded.
Acknowledgements
The authors would like to thank hospital personnel who contributed to this national project.
This article has been extracted from the thesis written by Dr. Parisa Yuseffam in the School of Medicine Shahid Beheshti University of Medical Sciences (Registration No: 424m).
Author Contributions
Seyed Ahmad Raeissadat has designed and made definition of intellectual content. Leila Bagherzadeh searched the literature. Parisa Youseffam gathered the data and performed statistical analysis. Leila Bagherzadeh and Seyed Ahmad Raeissadat prepared the manuscript. Seyed Mansour Rayegani edited the manuscript. Mohammad Hasan Bahrami and Dariush Eliaspour reviewed and made revision on the manuscript. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bouche P. Compression and entrapment neuropathies. Handb Clin Neurol. 2013;115:311–366.
2. Landau ME, Campbell WW. Clinical features and electrodiagnosis of ulnar neuropathies. Phys Med Rehabil Clin N Am. 2013;24(1):49–66. doi:10.1016/j.pmr.2012.08.019
3. Depukat P, Henry BM, Popieluszko P, et al. Anatomical variability and histological structure of the ulnar nerve in the guyon’s canal. Arch Orthop Trauma Surg. 2017;137(2):277–283. doi:10.1007/s00402-016-2616-4
4. Halac G, Topaloglu P, Demir S, et al. Ulnar nerve entrapment neuropathy at the elbow: relationship between the electrophysiological findings and neuropathic pain. J Phys Ther Sci. 2015;27(7):2213–2216. doi:10.1589/jpts.27.2213
5. Mondelli M, Giannini F, Ballerini M, Ginanneschi F, Martorelli E. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy). J Neurol Sci. 2005;234(1–2):5–10. doi:10.1016/j.jns.2005.02.010
6. Thibault MW, Robinson LR, Franklin G, Fulton-Kehoe D. Use of the AAEM guidelines in electrodiagnosis of ulnar neuropathy at the elbow. Am J Phys Med Rehabil. 2005;84(4):267–273. doi:10.1097/01.PHM.0000156893.12433.C7
7. Kitzinger H, Aszmann O, Moser V, Frey M. Significance of electroneurographic parameters in the diagnosis of chronic neuropathy of the ulnar nerve at the elbow. Handchir Mikrochir Plast Chir. 2005;37(4):276–281.
8. Wiesler ER, Chloros GD, Cartwright MS, Shin HW, Walker FO. Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J Hand Surg Am. 2006;31(7):1088–1093. doi:10.1016/j.jhsa.2006.06.007
9. Assmus H, Antoniadis G, Bischoff C, et al. Cubital tunnel syndrome–a review and management guidelines. Cent Eur Neurosurg. 2011;72(02):90–98. doi:10.1055/s-0031-1271800
10. Bedewi MA, Yousef AM, Abd-Elghany AA, Sherif El-sharkawy M, Awad EM. Estimation of ultrasound reference values for the ulnar nerve fascicular number and cross-sectional area in young males: a cross-sectional study. Medicine. 2017;96:10.
11. Campbell W, Carroll D, Greenberg M, Krendel D, Pridgeon R, Sitaram K. Practice parameter for electrodiagnostic studies in ulnar neuropathy at the elbow: summary statement. Muscle Nerve. 1999;22(3):408–411.
12. Dimberg EL. Electrodiagnostic evaluation of ulnar neuropathy and other upper extremity mononeuropathies. Neurol Clin. 2012;30(2):479–503. doi:10.1016/j.ncl.2011.12.003
13. Feinberg JH, Nadler SF, Krivickas LS. Peripheral nerve injuries in the athlete. Sports Med. 1997;24(6):385–408. doi:10.2165/00007256-199724060-00004
14. Kern RZ. The electrodiagnosis of ulnar nerve entrapment at the elbow. Can J Neurol Sci. 2003;30(4):314–319. doi:10.1017/S0317167100003012
15. Omejec G, Božikov K, Podnar S. Validation of preoperative nerve conduction studies by intraoperative studies in patients with ulnar neuropathy at the elbow. Clin Neurophysiol. 2016;127(12):3499–3505. doi:10.1016/j.clinph.2016.09.018
16. Omejec G, Podnar S. Proposal for electrodiagnostic evaluation of patients with suspected ulnar neuropathy at the elbow. Clin Neurophysiol. 2016;127(4):1961–1967. doi:10.1016/j.clinph.2016.01.011
17. Todnem K, Michler RP, Wader TE, Engstrøm M, Sand T. The impact of extended electrodiagnostic studies in ulnar neuropathy at the elbow. BMC Neurol. 2009;9(1):52. doi:10.1186/1471-2377-9-52
18. Karakis I, Liew W, Fournier HS, Jones HR
19. Kwon H-K, Lee HJ, Hwang M, Lee S-H. Amplitude ratio of ulnar sensory nerve action potentials in segmental conduction study: reference values in healthy subjects and diagnostic usefulness in patients with ulnar neuropathy at the elbow. Am J Phys Med Rehabil. 2008;87(8):642–646. doi:10.1097/PHM.0b013e31816de327
20. Garibaldi SG, Nucci A. Dorsal ulnar cutaneous nerve conduction: reference values. Arq Neuropsiquiatr. 2002;60(2B):349–352. doi:10.1590/S0004-282X2002000300001
21. Landau ME, Barner KC, Campbell WW. Optimal screening distance for ulnar neuropathy at the elbow. Muscle Nerve. 2003;27(5):570–574. doi:10.1002/(ISSN)1097-4598
22. Eliaspour D, Sedighipour L, Hedayati-Moghaddam MR, Rayegani SM, Bahrami MH, Roghani RS. The pattern of muscle involvement in ulnar neuropathy at the elbow. Neurol India. 2012;60(1):36. doi:10.4103/0028-3886.93586
23. Won SJ, Yoon JS, Kim JY, Kim SJ, Jeong JS. Avoiding false‐negative nerve conduction study in ulnar neuropathy at the elbow. Muscle Nerve. 2011;44(4):583–586. doi:10.1002/mus.22131
24. Artico M, Pastore F, Nucci F, Giuffre R. 290 surgical procedures for ulnar nerve entrapment at the elbow: physiopathology, clinical experience and results. Acta Neurochir (Wien). 2000;142(3):303–308. doi:10.1007/s007010050039
25. Kouyoumdjian JA, Graça CR, Ferreira VF. Peripheral nerve injuries: a retrospective survey of 1124 cases. Neurol India. 2017;65(3):551. doi:10.4103/neuroindia.NI_987_16
26. Eser F, Aktekin LA, Bodur H, Atan C. Etiological factors of traumatic peripheral nerve injuries. Neurol India. 2009;57(4):434–437. doi:10.4103/0028-3886.55614
27. Adeyemi-Doro HO. Pattern of peripheral traumatic neuropathy of the upper limb in Lagos. Injury. 1988;19(5):329–332. doi:10.1016/0020-1383(88)90105-2
28. Chang C-W, Wang Y-C, Chu C-H. Increased carrying angle is a risk factor for nontraumatic ulnar neuropathy at the elbow. Clin Orthop Relat Res. 2008;466(9):2190. doi:10.1007/s11999-008-0308-2
29. Contreras MG, Warner MA, Charboneau WJ, Cahill DR. Anatomy of the ulnar nerve at the elbow: potential relationship of acute ulnar neuropathy to gender differences. Clin Anat. 1998;11(6):372–378. doi:10.1002/(ISSN)1098-2353
30. Campbell WW, Carroll C, Landau ME. Ulnar neuropathy at the elbow: five new things. Neurol Clin Pract. 2015;5(1):35–41. doi:10.1212/CPJ.0000000000000097
31. Venkatesh S, Kothari MJ, Preston DC. The limitations of the dorsal ulnar cutaneous sensory response in patients with ulnar neuropathy at the elbow. Muscle Nerve. 1995;18(3):345–347. doi:10.1002/(ISSN)1097-4598
32. Caliandro P, Foschini M, Pazzaglia C, et al. IN-RATIO: a new test to increase diagnostic sensitivity in ulnar nerve entrapment at elbow. Clin Neurophysiol. 2008;119(7):1600–1606. doi:10.1016/j.clinph.2008.03.007
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
