Back to Journals » Orthopedic Research and Reviews » Volume 15
Efficacy and Safety Study of Low-Molecular-Weight Heparin and Fondaparinux Sodium After Hip Arthroplasty: A Retrospective Cohort Study
Authors Haibier A , Yusufu A, Lin H, Kayierhan A, Abudukelimu Y, Abudurexiti T
Received 7 September 2023
Accepted for publication 9 November 2023
Published 24 November 2023 Volume 2023:15 Pages 253—261
DOI https://doi.org/10.2147/ORR.S431372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Abuduwupuer Haibier,1,2,* Alimujiang Yusufu,1,2,* Hang Lin,1,2 Aiben Kayierhan,1,2 Yimuran Abudukelimu,1,2 Tuerhongjiang Abudurexiti1,2
1Minimally Invasive Spine Surgery, Sixth Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China; 2Xinjiang Medical University, Urumqi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tuerhongjiang Abudurexiti, Email [email protected]
Background: Low molecular heparin(LMWH) and sodium sulfadiazine heparin(FPX) are commonly used to prevent deep vein thrombosis(DVT) after total hip arthroplasty(THA). In this study, we compared the role of these drugs in preventing DVT after THA.
Methods: Patients who underwent unilateral THA at the Sixth Affiliated Hospital of Xinjiang Medical University from April 2020 to December 2022 were retrospectively analyzed for inclusion in this study. According to the anticoagulant drugs used, the patients were divided into LMWH group (n=106) and FPX group (n=97). Changes in perioperative coagulation-related indices, hemoglobin, blood loss And the postoperative complications.
Results: The preoperative indexes of the two groups of patients, the difference was not statistically significant (P> 0.05); the indexes of Intraoperative blood loss, Visible blood loss, Hidden blood loss, and Total blood loss of the two groups of patients were compared, and the difference was not significant (P> 0.05); PT activity and INR in the LMWH group were significantly lower than those in the FPX group on the 1st and 5th postoperative days, and the differences were significant (P< 0.05); Platelets, Hemoglobin, Hematocrit, D-dimer, and Fibrinogen were compared between the two groups on the 1st and 5th postoperative days, and the differences were not significant (P< 0.05). The differences were not significant (P> 0.05). The differences in blood transfusion rate and blood volume between the two groups were not significant (P> 0.05); the total hospitalization cost of the LMWH group was significantly lower than that of the FPX group, and the difference was significant (P< 0.05); and the differences in the incidence of postoperative complications between the two groups were not significant (P> 0.05).
Conclusion: In this study, we found that the efficacy and safety of FPX and LMWH in preventing VTE after THA were basically the same, and the total cost of hospitalization in the LMWH group was significantly lower than that in the FPX group; however, due to the limited inclusion of the sample size, high-quality, large-sample, long-term follow-up clinical studies are necessary.
Keywords: hip osteoarthritis, total Hip arthroplasty, low-molecular-weight heparin, fondaparinux sodium, coagulation indicator, thrombosis
Background
As the population lives longer, the number of patients with osteoarthritis increases, so does the number of patients treated with artificial joint replacement.1,2 Total hip arthroplasty (THA) is one of the most popular treatments for the hip. Total hip arthroplasty (THA) is currently an effective treatment for hip diseases.3 Deep vein thrombosis (DVT) is a disease of impaired venous return caused by abnormal clotting of blood in deep veins, which is a serious complication after total hip arthroplasty (THA), affecting the recovery of joint function and even threatening the recovery of joint function.4 DVT is a serious complication after total hip arthroplasty (THA), affecting the restoration of joint function and even threatening life5 It is a serious complication after total hip arthroplasty (THA). Relevant literature reports6 The incidence of DVT after THA can be as high as more than 50% if relevant preventive measures are not taken. Therefore, active and effective measures should be taken to reduce the incidence of DVT after THA to improve the prognosis of patients. Low molecular heparin (LMWH) and sodium pentoxifylline (FPX) are commonly used to prevent DVT after THA. However, data on the effects of both after TKA are still lacking. In this study, we compared the preventive effects of LMWH and FPX on lower extremity DVT after THA. Our findings may inform the selection of appropriate anticoagulation therapy after THA.
Methods
Patients and Design
This was a retrospective study approved by the Ethics Committee of the Sixth Affiliated Hospital of Xinjiang Medical University under the ethical approval number LFYLLSC20230618-01. All study subjects signed an informed consent form (Figure 1).
 |
Figure 1 Patient flow chart. |
Based on recommendations in the literature, all LMWH groups in our trial received half of the normal dose of low molecular heparin calcium subcutaneously at 4–6 hours postoperatively. The normal dose was injected the next day (once daily). FPX group: a 2.5 mg dose was injected subcutaneously starting 6 hours postoperatively (once daily). The duration of treatment was 2 weeks. The choice of anticoagulant drugs was decided by the doctor and the patient after the consultation. Inclusion criteria: (1) age ≥18 years; (2) planned initial THA due to end-stage osteoarthritis or femoral head necrosis. (Figure 2 exclusion criteria: (1) revision or bilateral surgery; (2) history of previous ipsilateral hip surgery; (3) contraindications to the use of LMWH and FPX, allergy within 6 months or history of thrombosis; (4) preoperative anemia, hemoglobin (HB) levels, <12 g/dl in women and <13 g/dl in men; (5) body mass index >35 kg/m2; (6) coagulation disorders.
 |
Figure 2 (A) Pre x-ray before right Hip arthroplasty; (B) The x-ray after right Hip arthroplasty. |
Surgical Procedures and Postoperative Rehabilitation
All THAs were performed using a posterolateral approach by a surgical team of 2 senior orthopedic surgeons. General anesthesia and controlled hypotensive anesthesia (BP <100/60 mmHg) were used. Uncemented acetabular prosthesis (Johnson & Johnson Pinnacle acetabular prosthesis) and femoral stem (Johnson & Johnson Corail femoral stem) were used as conventional prostheses.
All patients were routinely given postoperative care and thromboprophylaxis before weight-bearing walking, and walking training and strength training were started on the first postoperative day. On the 1st, 3rd, 5th and 9th postoperative days, the physician in charge of the patient’s incision cleaned with iodine povidone-iodine and observed the recovery of the incision, and if there was any abnormality, it was reported to the physician in time and was treated in a timely manner. On the 7th postoperative day, the patient received ultrasound examination of both lower limbs; the sutures were routinely removed on the 12th postoperative day, but if the patient had complications such as necrosis of the skin edge of the incision or fat liquefaction, the physician in charge had to report to the supervising physician, and the sutures could not be removed until the incision had completely healed. After discharge, patients were told to come to the hospital for regular follow-up of B ultrasound of lower limb blood vessels and coagulation function in 1 or 2 months after the operation; during this period, patients were required to stay in bed strictly, and were not allowed to go down to the ground for weight bearing. Rivaroxaban (Bayeritol, 10 mg, Bayer AG) was administered orally to prevent thrombosis for 15 d. Doppler ultrasound was routinely used to detect deep vein thrombosis at the time of discharge from the hospital, at the 1-month follow-up, or when deep vein thrombosis (DVT) was suspected. If necessary, chest CT-PA was used to detect pulmonary embolism. Blood transfusion protocols were used for patients with hemoglobin levels below 70 g/L, or hemoglobin values of 70–100 g/L accompanied by anemia-related symptoms such as dizziness, palpitations, shortness of breath, or decreased exercise tolerance.
Ending Indicator
The demographic characteristics and medical history of the patients were recorded preoperatively.
Main Outcome Indicators
The main outcome indicators were Platelets, Hemoglobin, Hematocrit, D-dimer, PT activity, INR, Fibrinogen, and estimated blood loss (EBL), overt blood loss, occult blood loss, transfusion rate, transfusion volume, and blood test on the 1st and 5th postoperative days. EBL, apparent blood loss, occult blood loss, transfusion rate, transfusion volume, and blood test. Total blood loss was calculated according to the Gross equation and Nadler equation method: total blood volume=k1×height (m)3+k2×weight (kg)+k3, of which the coefficients for men were k1=0.3669, k2=0.032 19, and k3=0.6041, and those for women were k1=0.3561, k2=0.03308, and k3=0.1833. Total blood loss=blood volume×(height (m)3+k2×weight (kg)+k3). blood loss = blood volume × (preoperative erythrocyte pressure volume - lowest postoperative erythrocyte pressure volume)/mean erythrocyte pressure volume, explicit blood loss was defined as intraoperative blood loss + volume of drainage, and implicit blood loss = total blood loss - explicit blood loss + volume of transfused erythrocytes.
Secondary Outcome Indicators
Postoperative length of stay, duration of surgery, total hospitalization costs and postoperative complications (interosseous vein thrombosis, deep vein thrombosis, pulmonary thrombosis, incisional infections and mortality).
Statistical Analysis
SPSS 26.0 software was used to statistically analyze the data. All results from measured data in this study are presented as mean ± standard deviation, and categorical data are presented as percentages and frequency counts; since no major deviations from normality were detected, t-tests were used to compare continuous variables between the two treatment groups (LMWH and FPX groups), whereas comparisons of categorical variables were made using chi-square tests or Fisher’s exact test.
Patient Demographics
A total of 206 patients (LMWH: 109, FPX: 97) who underwent total hip arthroplasty were collected in this study. The baseline characteristics of the two groups were comparable and are summarized in Table 1
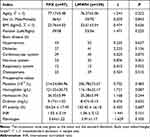 |
Table 1 Comparison of the Preoperative General Data Between the Two Groups |
Comparison of Preoperative Data Between the Two Groups
Preoperative age, gender composition, body mass index, surgical site, hypertension, diabetes mellitus, coronary heart disease, neurological disease, respiratory disease, metabolic disease, as well as platelets, hemoglobin, erythrocyte pressure volume, D-dimer, plasminogen activity (PT), the internationalized standard ratio, and fibrinogen of the patients in the two groups were compared, and the differences were not significant (P>0.05). 0.05), as shown in Table 1
Comparison of Perioperative Bleeding Between the Two Groups
Intraoperative blood loss, Visible blood loss, Hidden blood loss, and Total blood loss were compared between the two groups, and the differences were not significant (P>0.05), as shown in Table 2.
 |
Table 2 Comparison of Perioperative Blood Loss Between the Two Groups |
Comparison of Postoperative Coagulation Indices Between the Two Groups
The PT activity and INR of the LMWH group were significantly lower than those of the FPX group on the 1st and 5th postoperative days, and the differences were significant (P<0.05), See Figures 3 and 4. the differences in the ratios of Platelets, Hemoglobin, Hematocrit, D-dimer, and Fibrinogen on the 1st and 5th postoperative days of the patients in the two groups were not significant (P>0.05). significance (P>0.05). See Table 3 and 4.
 |
Table 3 Comparison of the Coagulation Tests on Day 1 After Surgery |
 |
Table 4 Comparison of the Coagulation Tests on Day 5 After Surgery |
 |
Figure 3 Comparison of the first, postoperative day and fifth postoperative day after PT activity surgery. |
 |
Figure 4 Comparison of the first, postoperative day and fifth postoperative day after INR surgery. |
Comparison of Blood Transfusion Rate and Volume Between the Two Groups
In the FPX group, there were 42 transfusion cases in the perioperative period, with a transfusion rate of 43.3% and a volume of (253.60±340.97) mL; in the LMWH group, there were 38 patients who were transfused, with a transfusion rate of 34.9% and a volume of (203.66±347.45) mL; the difference in the rate of transfusion and the volume of transfusion in these two groups was not significant (χ2 =1.538, χ2 =1.039, pand gt; 0.05). See Table 5.
 |
Table 5 Postoperative Hospital Stay and Complications in the Rate of Transfusion and the Volume of Transfusion in Both Groups |
Comparison of Secondary Outcome Indicators
Total hospitalization costs were significantly lower in the LMWH group than in the FPX group, and the difference was significant (P<0.05);
Compared with the hospitalization time and operation time in the two groups, the difference was not significant (t=0.543, t=0.303, P>0.05). Comparison of the incidence of various postoperative complications between the two groups was not significant (x²=0.134, 0.981, 2.269, 1.129, P>0.05), as shown in Table 6. There were no critical complications such as pulmonary thrombosis, acute renal failure or epilepsy, or death in the postoperative period of the two groups, which indicates that the two drugs are basically the same in terms of their safety for the organism. See Table 6.
 |
Table 6 Postoperative Hospital Stay and Complications in Both Groups with the Hospitalization Time and Operation Time |
Discussion
Total hip arthroplasty (THA) is the primary intervention for the treatment of end-stage hip disease and plays a crucial role in improving the quality of life of elderly patients3,7,8. In hip replacement patients, postoperative lower limb activity is limited and blood flow velocity decreases, leading to venous injury, venous stasis and hypercoagulability of blood3 This leads to frequent occurrence of adverse events such as postoperative DVT and pulmonary embolism, which are the main causes of mortality and morbidity after total hip arthroplasty.9 They are the main causes of mortality and morbidity after total hip arthroplasty. Prophylactic anticoagulation has become essential in the perioperative period of THA and has significantly reduced the overall incidence of postoperative venous thromboembolism (VTE)10. However, despite prophylactic anticoagulation, some patients continue to experience these serious complications during and after hospitalization11.
Clinically, low molecular weight heparin, sodium sulfadiazepoxide, rivaroxaban, warfarin and other drugs are often used for early anticoagulant therapy for patients with hip arthroplasty, and all of them can achieve better results.12,13. Low molecular weight heparin is widely used in perioperative DVT prevention in orthopedic major surgery, belonging to the first-line anticoagulant drugs, which can effectively reduce the biological activity of activated coagulation factors, thus inhibiting platelet aggregation, inducing fibrinolysis, and achieving the purpose of removing venous thrombus embolus, and the drug has a longer half-life, with a good degree of utilization.14 The drug has a long half-life and good utilization. Fondaparinux sodium is a synthetic selective inhibitor of activated factor X. Its pentose structure significantly increases the affinity of antithrombin (AT), which specifically binds to the activation site of antithrombin through its non-covalent bond, resulting in the rapid inhibition of activated coagulation factor X, which in turn reduces the production of prothrombin and fibrin formation.15,16 This results in rapid inhibition of activated factor X, thereby reducing thrombin production and fibrin formation. Unlike UFH and LMWH, sodium sulfadiazepoxide is not expected to bind to platelet factor IV and does not cross-react with plasma from patients with heparin-induced thrombocytopenia.17,18 Sulfohepatidine sodium is not expected to bind to platelet factor IV or cross-react with plasma from patients with heparin-induced thrombocytopenia. Sodium sulfadoxine heparin has unique anticoagulant activity and a longer half-life (10 ~ 15 h) than LMWH. Low molecular weight heparin is a sulfated glycosaminoglycan salt with a molecular weight significantly greater than that of sodium sulfadiazepate19 Sulphated glycosaminoglycan salts. The average molecular weight of sodium sulfated heparin is below 8000 Da, and at least 60% of its molecular weight is distributed below 8000 Da.20,21 The average molecular weight of sulfadoxine sodium is below 8000 Da and at least 60% of the molecular weight is below 8000 Da. Because of its small molecular weight and monotonous action, sulfadoxine does not have many of the important pharmacological properties of pharmaceutical heparin, except for its specific binding to the anti-Xa factor.22 It does not have many of the important pharmacologic properties of pharmaceutical heparin. The present study showed that PT activity and INR indexes were significantly higher in the LMWH group than in the FPX group on postoperative days 1 and 5, (t1day =−3.096, t5day =−2.648, P < 0.05), indicating that the time of plasminogen activation was shortened in the FPX group, which made the formation of thrombus easier. This study also showed that the total cost of hospitalization was lower in the LMWH group than in the FPX group, suggesting that the cost of VTE prevention was lower in the LMWH group and therefore more economical to use.
Some studies have shown that23 DVT is one of the common and major complications of THA. Without any preventive measures, the probability of lower extremity deep vein thrombosis (DVT) after hip arthroplasty is 39%-74%, and the probability of pulmonary artery embolism (PAE), which has a high lethality rate, is 0.5%-2%, and proximal DVT is the main source of pulmonary embolism, which is the most important perioperative cause of orthopedic death.24 Once pulmonary embolism occurs, the disease progresses rapidly, and the current treatment options are very limited and the prognosis is poor.13 In the present study, we found that two patients with pulmonary venous thrombosis (PVT) were found to have a high risk of pulmonary embolism. In this study, we found Intraoperative blood loss, Visible blood loss, Hidden blood loss, Total blood loss in two groups, There was no significant difference between the rates of blood transfusion and thromboembolic events. These results suggest that there is no significant difference in the incidence of DVT after TKA prevention with LMWH and FPX. Some studies have found that25 the incidence of thrombocytopenia caused by LMWH is low. For patients with thrombocytopenia caused by FPX, LMWH can be replaced. Heparin inhibited adrenal aldosterone synthesis, occasionally causing hyperkalemia, and mild transaminase elevation by FPX.
Limitations of the Article
①This trial is a retrospective study, so there may be the possibility of loss of data or failure to record data in time, which may bias the results, but the research team to which the authors belonged strictly and carefully recorded the postoperative outcome indicators of each group to maximize the completeness of the experimental data; ②The sample size of the inclusion of the relatively small, statistically insufficient efficacy of the reporting of bias, and the results of this study need further, multicenter, prospective studies to further elucidate the relationship between clinical outcomes. The results of this study require further multicenter, prospective studies to further elucidate the relationship between clinical outcomes.
Conclusions
In conclusion, this study found that the efficacy and safety of FPX and LMWH in preventing VTE after THA were basically the same, and the total hospitalization cost of the LMWH group was significantly lower than that of the FPX group; however, due to the limited sample size included, high-quality, large-sample, long-term follow-up clinical studies are necessary.
Abbreviations
BMI, Body mass index; DVT, Deep vein thrombosis; Hb, Hemoglobin; Hct, Hematocrit; INR, International normalized ratio; THA, total hip arthroplasty; LMWH, low-molecular-weight heparin; LOH, length of hospital stay.
Data Sharing Statement
Follow-up regarding theEfficacy and safety study of low-molecular-weight heparin and fondaparinux sodium after hip arthroplasty: a retrospective cohort study is not complete, so the dataset analyzed in this study is not publicly available but is available to the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
We confirm that all experiments were performed in accordance with the Declaration of Helsinki. The study was approved by the Ethical Committee of the Xinjiang Medical University Affiliated Sixth Hospital, NO: LFYLLSC20230713-01. Each patient provided written informed consent before participating in the study.
Funding
There is no funding to report.
Disclosure
Abuduwupuer Haibier and Alimujiang Yusufu are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Bülow E, Rolfson O, Cnudde P, et al. Comorbidity does not predict long-term mortality after total Hip arthroplasty. Acta Orthop. 2017;88(5):472–477. doi:10.1080/17453674.2017.1341243
2. Glassou EN, Pedersen AB, Hansen TB. Is decreasing mortality in total Hip and knee arthroplasty patients dependent on patients’ comorbidity?. Acta Orthop. 2017;88(3):288–293. doi:10.1080/17453674.2017.1279496
3. Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S, 2014 to 2030. J Bone Joint Surg Am. 2018;100(17):1455–1460. doi:10.2106/JBJS.17.01617
4. Mclaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with Hip fracture. J Gen Intern Med. 2006;21(3):219–225.
5. Dua A, Desai SS, Lee CJ, et al. National trends in deep vein thrombosis following total knee and total hip replacement in the United States. Ann Vasc Surg. 2017;38:310–314. doi:10.1016/j.avsg.2016.05.110
6. Sun WW, Du XH, Qiu Z, et al. The safety and effect of rivaroxaban and low molecular weight heparin in preventing lower extremity deep vein thrombosis in patients with lower extremity fractures. J Orthop. 2021;24(6):818–821.
7. Kanchanabat B, Stapanavatr W, Meknavin S, et al. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98(10):1356–1364.
8. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis. American College of Chest Physicians.
9. Miyamoto RG, Kaplan KM, Levine BR, et al. Surgical management of Hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16(10):596–607. doi:10.5435/00124635-200810000-00005
10. Franchini M, Mengoli C, Marietta M, et al. Safety of intravenous tranexamic acid in patients undergoing major orthopaedic surgery: a meta-analysis of randomised controlled trials. Blood Transfus. 2018;16(1):36–43.
11. Lieberman JR, Cheng V, Cote MP. Pulmonary embolism rates following total hip arthroplasty with prophylactic anticoagulation: some pulmonary emboli cannot be avoided. J Arthroplasty. 2017;32(3):980–986. doi:10.1016/j.arth.2016.09.006
12. Zheng J, Wang J, Zhang JL. The preventive effect of rivaroxaban combined with low molecular weight heparin sodium on deep vein thrombosis after Hip replacement. Zhejiang Trauma Surgery Department. 2021;26(6):1032–1033.
13. Blitzer RR, Eisenstein S. Venous thromboembolism and pulmonary embolism: strategies for prevention and management. Surg Clin North Am. 2021;101(5):925–938.
14. Chen L, Zhang S, Da J, et al. Clinical observation of low molecular weight heparin calcium combined with dipyridamole on postoperative serum D. Dimer levels and prevention of thrombosis in patients with lower limb fractures. Int J Clin Prac. 2021;18(6):118–121.
15. Fourman MS, Shaw JD, Nwasike CO, et al. Use of fondaparinux following elective lumbar spine surgery is associated with a reduction in symptomatic venous thromboembolism. Glob Spine J. 2020;10(7):844–850. doi:10.1177/2192568219878418
16. Sarhaddi D, Xu K, Wisbeck A, et al. Fondaparinux significantly reduces postoperative venous thromboembolism after body contouring procedures without an increase in bleeding complications. Aesthet Surg J. 2019;39(11):1214–1221. doi:10.1093/asj/sjz184
17. Zhang Y, Zhang M, Tan L, et al. The clinical use of Fondaparinux: a synthetic heparin pentasaccharide. Prog Mol Biol Transl Sci. 2019;163:41–53.
18. Working group of the expert Consensus of Clinical Pharmaceutical Branch of Chinese Medical Association. Expert consensus of pharmaceutical practice of fonda. Herald of Medicine. 2022;41(11):1571–1581.
19. Baytas SN, Varghese SS, Jin W, et al. Preparation of low molecular weight heparin from a remodeled bovine intestinal heparin. J Med Chem. 2021;64(4):2242–2253. doi:10.1021/acs.jmedchem.0c02019
20. John S, Wilkinson M, Ho KM. Monitoring anti-xa levels to optimize low-molecular-weight-heparin thromboprophylaxis in high-risk hospitalized patients: a stratified meta-analysis. Angiology. 2023;2023:33197221150673.
21. Coveney EI, Hutton C, Patel N, et al. Incidence of Symptomatic Venous Thromboembolism (VTE) in 8885 elective total hip arthroplasty patients receiving post-operative aspirin VTE prophylaxis. Cureus. 2023;15(3):e36464.
22. Sun XJ. Innovative Method Investigation for Structural Analysis of Glycosaminoglycan in Bio-Pharmaceuticals. Shandong: Shandong University; 2017.
23. Yen D, Weiss W. Results of adjusted-dose heparin for thromboembolism prophylaxis in knee replacement compared to those found for its use in Hip fracture surgery and elective Hip replacement. Iowa Orthop J. 2007;27:47–51.
24. Mula V, Parikh S, Suresh S, et al. Venous thromboembolism rates after Hip and knee arthroplasty and Hip fractures. BMC Musculoskelet Disord. 2020;21(1):95.
25. Tang X, Du Y, Chen Z, et al. Evaluation of anticoagulant effect of fondaparinux and low molecular weight heparin in continuous renal replacement therapy. Chin Med J. 2023;38(01):51–55. doi:10.1142/S0192415X10007786
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
