Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Efficacy and safety of paliperidone palmitate three-monthly formulation in East Asian patients with schizophrenia: subgroup analysis of a global, randomized, double-blind, Phase III, noninferiority study
Authors Savitz AJ, Xu H , Gopal S , Nuamah I, Ravenstijn P, Hough D, Mathews M, Feng Y, Yu L, Takahashi M , Liu D, Wang G, Yoon J, Chen JJ
Received 9 February 2017
Accepted for publication 15 May 2017
Published 17 August 2017 Volume 2017:13 Pages 2193—2207
DOI https://doi.org/10.2147/NDT.S134287
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Adam J Savitz,1 Haiyan Xu,2 Srihari Gopal,1 Isaac Nuamah,2 Paulien Ravenstijn,3 David Hough,1 Maju Mathews,4 Yu Feng,5 Lu Yu,6 Masayoshi Takahashi,7 Dennis Liu,8 Gang Wang,9 Jin-Sang Yoon,10 Jiahn-Jyh Chen11
1Department of Central Nervous System, 2Department of Clinical Biostatistics, Janssen Research & Development, LLC, Titusville, NJ, USA; 3Department of Clinical Pharmacology, Janssen Research & Development, Beerse, Belgium; 4Global Medical Affairs, Neurosciences, Janssen Research & Development, NY, USA; 5Medical Affairs, Neurosciences, Janssen Pharmaceutical Companies of Johnson and Johnson, Singapore; 6Department of Clinical Development, Janssen Research & Development, Beijing, China; 7Department of Central Nervous System, Janssen Pharmaceutical KK, Tokyo, Japan; 8Playford Community Team, Northern Adelaide Local Health Network, Adelaide, SA, Australia; 9National Clinical Research Center for Mental Disorders, Beijing Anding Hospital, Affiliated Capital University of Medical Science, Beijing, China; 10Department of Psychiatry, Chonnam National University Hospital, Gwangju, South Korea; 11Department of Geriatric Psychiatry, Taoyuan Mental Hospital, Taoyuan, Taiwan
Objective: To demonstrate the efficacy and safety of paliperidone palmitate three-monthly (PP3M) formulation in an East Asian population with schizophrenia by subgroup analysis of a double-blind (DB), multicenter, noninferiority study.
Patients and methods: Of 1,429 patients who entered the open-label (OL) phase, 510 were East Asian (China: 296 [58%], Japan: 175 [34%], South Korea: 19 [4%] and Taiwan: 20 [4%]). In the 17-week OL phase, patients received paliperidone palmitate once-monthly (PP1M) formulation on day 1 (150 mg eq.), day 8 (100 mg eq.) and once-monthly thereafter (50–150 mg eq., flexible). Following the OL phase, patients (n=344 East Asian) entered DB phase and were randomized (1:1) to PP1M (n=174) or PP3M (n=170). Primary efficacy endpoint was the percentage of patients who remained relapse free at the end of the 48-week DB phase, using Kaplan–Meier cumulative survival estimate. Secondary efficacy endpoints included change from DB baseline to endpoint in Positive and Negative Syndrome Scale, Clinical Global Impression Severity, Personal and Social Performance scores and symptomatic remission. Additional assessments included caregiver burden and safety.
Results: A total of 285/344 (83%) randomized East Asian patients completed the DB phase. The percentage of patients who had a relapse event was similar on comparing PP3M (17 [10.2%]) to PP1M (20 [11.8%]), and also for Japan (PP3M: 9 [17.6%], PP1M: 13 [23.2%]) and China (PP3M: 6 [5.9%], PP1M: 7 [6.9%]). Mean change from baseline in secondary efficacy parameters was similar to the global population, regardless of treatment. Symptomatic remission was attained by 50% of the treated patients. Caregiver burden was significantly reduced (P<0.001) following treatment with PP3M/PP1M. Frequency of treatment-emergent adverse events in PP3M group during DB phase was greater in the East Asian subgroup (81%) than the global population (68%) and was higher in Japan (92%) than China (75%).
Conclusion: Results suggest that PP3M is efficacious in the East Asian subgroup. Although treatment-emergent adverse events were slightly higher in the East Asian subgroup versus the global population, no new safety signals were identified.
Keywords: antipsychotic, caregiver burden, depot paliperidone palmitate, East Asia, long-acting injectable, paliperidone palmitate once-monthly, paliperidone palmitate three-monthly, schizophrenia, symptom remission
Introduction
Despite adequate symptom control, nonadherence to treatment is common among patients with schizophrenia undergoing antipsychotic therapy1 and this presents an increased risk of relapse and rehospitalization.2,3 Partial or total nonadherence to treatment generally leads to failure of antipsychotic therapy to adequately control the symptoms of the disease4 or to the increased risk of adverse events associated with the therapy.5 Lack of efficacy as indicated by failure to achieve long-term remission, or by successive relapses during the study, may be a reason as well as a consequence of treatment nonadherence.6 Furthermore, patients achieving symptomatic remission may not necessarily experience improvement in functional outcomes, including quality of life.7 Hence, besides symptom control, physicians face an additional challenge of improving treatment adherence while ensuring long-term symptomatic remission and full functional recovery of the patient.8,9
Frequent dosing requirements of oral antipsychotics often lead to nonadherence among patients.10 The long-acting injectable (LAI) formulations of antipsychotics considerably reduce the dosing frequency due to their sustained delivery and offer increased acceptability and tolerability, thereby improving patient adherence.10–12 Moreover, most LAIs of atypical antipsychotics are aqueous-based formulations, so that injections are comparatively less painful for patients than oil-based LAI preparations of typical antipsychotics.13 Additionally, physicians may also be able to isolate relapses occurring due to nonadherence from relapses due to lack of efficacy, as LAIs are administered only by health care professionals and, thus, adherence is monitored.14
Paliperidone palmitate once-monthly (PP1M; Invega Sustenna®, Titusville, NJ, USA) formulation was the first LAI formulation developed for paliperidone. Following the established efficacy and safety of PP1M formulation in patients with schizophrenia, globally as well as in the Asian population,15–17 a three-monthly (PP3M; Invega Trinza®, Titusville, NJ, USA) formulation with a further sustained exposure and reduced frequency of dosing was developed for patients with schizophrenia previously stabilized on PP1M formulation.
It is well established that the extent and pattern of symptoms of schizophrenia may vary substantially among patients of different ethnicities.18,19 Similarly, sociodemographic differences as well as differences in the practice of medicine have been known to affect treatment outcomes as well as the type and extent of adverse events associated with antipsychotic therapy.20 Previous studies have confirmed that plasma concentrations of paliperidone may be slightly higher in the Asian population owing to their lower body mass index (BMI) compared to Caucasian patients.21 With increased concentrations of PP3M expected in patients from Asia, it becomes imperative to assess the clinical outcomes of schizophrenia associated with PP3M administration in this population. For a large, global, Phase III, randomized, multicenter study, wherein noninferiority of PP3M to PP1M was demonstrated in patients with schizophrenia, a subgroup analysis of the East Asian population was conducted.22
We present here the results of efficacy and safety of PP3M, employing PP1M as a comparator in the East Asian subgroup of patients (including China, Japan, South Korea and Taiwan) enrolled in this multicenter study conducted across 26 countries.
Patients and methods
The methods are described in detail in the primary global study along with the overall efficacy and safety results;22 here we focus only on the East Asia-specific population data from this study.
Patients
Men and women from East Asia, between 18 and 70 years of age, diagnosed with schizophrenia (as per the Diagnostic and Statistical Manual of Mental Disorders, fourth edition) for at least 1 year prior to screening, with Positive and Negative Syndrome Scale (PANSS) total score between 70 and 120 and worsening symptoms were included in this study. Key inclusion criteria were discontinuation of current antipsychotic therapy due to efficacy, safety or tolerability concerns or patient’s preference for injectable medications. Key exclusion criteria were intolerance to risperidone, paliperidone or any excipients used in the formulation; primary, active Diagnostic and Statistical Manual of Mental Disorders, fourth edition Axis I diagnosis other than schizophrenia; active substance dependence within 6 months before screening; attempt to or risk of suicide; and any hematologic, biochemical, cardiovascular or other clinical abnormalities.
Study design and treatment
This was a randomized, double-blind (DB), parallel-group, multicenter study performed to assess the noninferiority of PP3M to PP1M in adult patients with schizophrenia. This study was conducted from April 2012 to March 2015 in 26 countries which included four countries from Asia (Japan: 43 sites; China: 15 sites; South Korea: 4 sites and Taiwan: 4 sites). The study consisted of three phases: screening phase (up to 21 days), open-label (OL) flexible-dose treatment phase (17 weeks) and the DB fixed-dose treatment phase (48 weeks). A follow-up visit was conducted 4 weeks after the end-of-study visit for patients who completed the study without a relapse and for patients who withdrew early during the OL phase. For patients who withdrew early during the DB phase and those who completed the study after they had a relapse in the DB phase, follow-up visit was conducted 12 weeks after the end-of-study visit.
During screening, patients without written source documentation of previous exposure to oral or injectable paliperidone/risperidone were subjected to an oral tolerability test, wherein paliperidone extended-release tablets were administered for four to six consecutive days. Following screening, eligible patients were enrolled into the OL phase to receive PP1M for a 17-week treatment period. The PP1M injection schedule was as follows: day 1 (150 mg eq., deltoid), day 8 (100 mg eq., deltoid), and once-monthly injections thereafter at week 5 and week 9 (flexible dose, 50, 75, 100 or 150 mg eq. in the deltoid or gluteal muscle) and week 13 (same dose as week 9).
For entry into the 48-week DB phase, patients had to additionally satisfy the following conditions: PANSS total score <70 and score of ≤4 on PANSS item scores P1, P2, P3, P6, P7, G8 and G14 at weeks 14 and 17; and decline in Clinical Global Impression Severity (CGI-S) score from OL baseline of ≥1 at weeks 14 and 17. In the DB phase, patients were randomized (1:1) either to PP1M or PP3M treatment groups. Central randomization was carried out by using randomly permuted blocks, stratified on the basis of the study center and executed using an interactive web response system. Patients were randomized via the interactive web response system to receive either PP1M or PP3M. Patients and investigators were blinded to treatment assignment. PP1M and PP3M were supplied in prefilled syringes for administration to patients. Due to the difference in syringe sizes for administration of PP1M and PP3M, patients were not allowed to view the needle or syringe or to observe the injection (administered by the study drug administrator, who was not permitted to communicate patient-related information to the site staff or the investigator). Patients in the PP1M group received the same dose as at week 9 (50, 75, 100 or 150 mg eq.), at four-weekly intervals from week 17 to week 61. Patients in the PP3M group received 3.5-fold multiple of PP1M dose administered at week 9 (175, 263, 350 or 525 mg eq.) at 12-weekly intervals at weeks 17, 29, 41 and 53. To maintain blinding, patients in the PP3M group were administered matching placebo injections (20% intralipid) each month when no PP3M dose was scheduled. Injection site remained the same as that used at the end of OL phase at week 13 (either deltoid or gluteal), with injections administered alternately at the left and the right side during each dose.
Uniformity in diagnosis and assessment was ensured by appointing only qualified raters to administer the PANSS, CGI-S and Personal and Social Performance (PSP) scales. If possible, for a given patient, the same rater administered the scale at all visits. These raters had at least 3 years of experience in evaluating patients with schizophrenia in an inpatient or outpatient setting. Sponsor certified the raters to perform the PANSS and trained them to perform the CGI-S. Timely data reviews, monitoring and comonitoring of sites by the team and routine investigator site audits were conducted globally to confirm data integrity, protocol compliance and safety of the patients based on standard operating procedures for monitoring of clinical studies.
The independent ethics committee or institutional review board at each study site approved the protocol and its amendments (see Supplementary material). The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and was consistent with Good Clinical Practices and applicable regulatory requirements. Written informed consent was obtained from all patients prior to their enrollment in the study.
Allowed and disallowed medication
Patients were allowed to receive oral lorazepam and other short-acting benzodiazepines for the treatment of anxiety or agitation; zolpidem, zopiclone, zaleplon for insomnia; β-blockers (for akathisia); antidepressants; medication for other medical problems and anti-Parkinson therapy. Certain drugs known to interact with paliperidone LAIs, such as drugs with the potential for inducing orthostatic hypotension (eg, α-adrenergics), strong inducers of CYP3A4 and P-gp (eg, carbamazepine, rifampin, St John’s wort), levodopa, dopamine antagonists, other antipsychotics and mood stabilizers, were not allowed during the study.
Study evaluations
Efficacy evaluations
The primary study endpoint was the percentage of patients who remained relapse-free at the end of the 48-week DB treatment phase, calculated based on the Kaplan–Meier 48-week cumulative estimate of survival. For this purpose, relapse was defined as one or more of the following: psychiatric hospitalization, increase in PANSS total score by 25% or 10 points (respective score at randomization >40 or ≤40) or a score of ≥5 or ≥6 (respective score at randomization ≤3 or 4) on PANSS item scores (P1, P2, P3, P6, P7, G8) after randomization for two consecutive assessments separated by 3–7 days, homicidal or suicidal ideation, violent or aggressive behavior causing damage or injury to self or others or property.22
The secondary efficacy endpoints were: change from DB baseline to endpoint in PANSS total scores and CGI-S scores (measured once every 4 weeks during DB), PSP score (collected once every 12 weeks during DB) and symptomatic remission during the DB phase based on Andreasen’s criteria.23 Symptomatic remission was defined as a score of ≤3 on the following PANSS items i.e. P1, P2, P3, N1, N4, N6, G5 and G9 for the last 6 months of DB treatment (no excursion allowed). For patients who maintained both symptomatic and functional remission, symptomatic remission was defined as remission with one excursion allowed. Functional remission was defined as PSP >70 for the last 6 months of the DB treatment, with no excursion allowed.
Exploratory endpoints included the assessment of burden experienced by caregivers of patients treated with PP3M or PP1M formulation, measured using the Involvement Evaluation Questionnaire (IEQ). Out of the 31 items on the IEQ questionnaire, 27 items were summarized into four distinct subscales: tension (9 items), supervision (6 items), worrying (6 items), urging (8 items) and a sum score of the 27 items.
Safety evaluations
Safety assessments included treatment-emergent adverse events (TEAEs), measurement of vital signs, clinical laboratory evaluations, extrapyramidal symptom (EPS) assessment and suicidal ideation and behavior (using Columbia Suicide Severity Rating Scale).
Statistical analysis
Sample size determination
Assuming an expected survival rate (percentage of patients remaining relapse-free) of 70% in the PP1M group, a true difference of 4% between PP1M and PP3M in favor of PP1M and a one-sided significance level of 2.5%, 380 patients were required to demonstrate with 90% power that PP3M was no worse than PP1M by a noninferiority margin of 15% for survival. Overall, ~1,388 patients were planned to be enrolled to the global study to provide 380 patients per treatment group for efficacy evaluation (expecting that only 74% of enrolled patients would be randomized in the DB phase). The study was not powered for individual subgroup analysis.
Patients who were randomly assigned to treatment during the DB phase and received at least one dose of DB study drug and had no major protocol violations that impacted efficacy were included in the per-protocol analysis set, while the modified intent-to-treat (mITT) DB analysis set included all patients who were randomized and received at least one dose of DB study drug and had no errors in the delivery of active treatment due to the manufacturing of the investigational product. The per-protocol analysis set was used for the primary efficacy endpoint assessment, whereas for the analyses of secondary efficacy endpoints, the mITT DB analysis set was used. The primary hypothesis of this study was that PP3M was noninferior to PP1M in the proportion of patients who remained relapse-free over 48 weeks. The hypothesis to be tested using a one-sided α=0.025 level was: H0: p3-p1≤-δ versus H1: p3-p1>-δ, where p1 and p3 were the percentage of patients who remained relapse-free at week 48 in the PP1M and PP3M groups, respectively. Cumulative proportion of survival (percentage of patients remaining relapse-free) was estimated using the Kaplan–Meier method. PP3M was considered as noninferior to PP1M if the lower limit of the two-sided 95% confidence interval (CI) of the difference in relapse-free rates between PP3M and PP1M exceeded −15%.
For the secondary efficacy endpoints, the changes from DB baseline to endpoint (end of 48-week DB phase) in the PANSS total score (and subscale scores), CGI-S and PSP scores were analyzed using an analysis of covariance model with treatment and country as factors and baseline score as a covariate. Treatment effects were estimated using least squares means and 95% CI. The proportion of patients who achieved symptomatic remission was summarized using the point estimate and the two-sided 95% CI for the relative risk using Mantel–Haenszel test with country as a control. Descriptive statistics were provided for summarizing caregiver burden as measured by the IEQ in patients who had a designated caregiver during the study.
For most analyses, the data for South Korea and Taiwan are not presented separately due to the small sample size of patients enrolled. The safety results were summarized descriptively.
Registration
The study is registered at the European (EU) clinical trial registry (EudraCT Number: 2011–004889–15) and ClinicalTrials.gov: NCT01515423.
Results
Patient disposition
A total of 1,429 patients were enrolled in the OL phase of the global study, of which 510 (36%) patients were from East Asia (China: 296 [21%], Japan: 175 [12%], South Korea: 19 [1%] and Taiwan: 20 [1%]). A slightly higher proportion of global patients (1,016/1,429 [71%]) from the OL phase entered the DB phase as compared with East Asian patients (344/510 [67%]; China: 210/296 [71%], Japan: 108/175 [62%], South Korea: 12/19 [63%] and Taiwan: 14/20 [70%]). The proportion of East Asian patients who completed the DB treatment (including relapses) was 285/344 (83%) (China: 174/210 [83%], Japan: 90/108 [83%], South Korea: 7/12 [58%] and Taiwan: 14/14 [100%]), and was similar in both PP3M and PP1M treatment groups and consistent with the global population (842/1,016 [83%]). The primary reasons for withdrawal from the DB phase were consent withdrawal and TEAEs (Figure 1).
Patient demographics and baseline characteristics
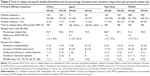
Of the 510 East Asian patients who entered the OL phase of the study, participation of women (53%) was slightly greater than men (47%). The mean (SD) age of these patients (36.4 [12.04] years) was similar to that of the global population (38.4 [11.86] years),22 comparatively higher in Japanese patients (43.5 [11.56] years) than Chinese (32.2 [10.61] years). Patients from China and Japan had similar baseline BMI, and a greater proportion had normal BMI (<25 kg/m2) compared with the global population (China: 64%, Japan: 53% and global: 44%)22 (Table 1).
The mean (SD) age at diagnosis of schizophrenia was 27.1 (9.03) years in the overall East Asian subgroup. The mean (SD) duration of hospitalization due to a psychiatric disorder at study entry was higher in the East Asian population (110.7 [226.00]), particularly in the Japanese subgroup (149.6 [334.85]), compared with the global population (94.2 [221.96]).22 The mean (SD) PANSS total scores at OL baseline were similar for the East Asian subgroup (85.0 [11.39]) and the global population (85.7 [10.73]). Similarly, OL baseline PSP and CGI-S scores were comparable between both the East Asian subgroup and the global population. In patients from East Asia, the DB baseline PANSS score was 57.2 (9.45), PSP was 67.0 (10.88) and CGI-S score was 2.9 (0.64). The improvement from OL baseline to DB baseline in all these scores was consistent with the global population.
Extent of exposure
Extent of exposure to paliperidone palmitate (PP) in terms of dose of drug received throughout the DB phase was similar in the East Asian subgroup (Table S1) and the global population.22 Patients from China (Table S2) were stabilized on lower doses of PP than Japanese patients (Table S3) at the beginning of the DB phase.
Use of prior and concomitant medications
Percentage of patients who had received ≥1 prior psychotropic medication in the month prior to screening was overall comparable between the global and the East Asian populations (90% each), but higher in the Japanese population (100%) as compared with Chinese (84%; Table S4). A higher proportion of Japanese patients (PP3M: 42%, PP1M: 48%) reported concomitant benzodiazepine use as compared with China (PP3M: 16%, PP1M: 14%) and the global population (PP3M: 24%, PP1M: 24%) in the DB phase (Table S5).
Efficacy results
Primary efficacy endpoints
At the end of the 48-week DB treatment phase, the Kaplan–Meier estimate of the difference (95% CI) between the PP3M and PP1M treatment groups in percentages of patients who remained relapse-free (per-protocol analysis set) was similar in the East Asian subgroup (1.6% [-5.7%; 9.0%]), Chinese subgroup (1.1% [-6.1%; 8.3%]) and the global population (1.2% [-2.7%; 5.1%]) and slightly higher in the Japanese subgroup (5.1% [-12.0%; 22.2%]), as shown in Figure 2. Although the study was not powered to show noninferiority in these subgroups, the lower bounds of 95% CI were larger than the global prespecified noninferiority margin of −15%, suggesting noninferiority of PP3M over PP1M, consistent with the global results.
The percentage of patients who experienced a relapse event was comparable in the overall East Asian subgroup (PP3M: 17 [10%], PP1M: 20 [12%]) and the global population (PP3M: 37 [8%], PP1M: 45 [9%]). The proportion was comparatively higher in the Japanese subgroup (PP3M: 9 [18%], PP1M: 13 [23%]) and lower in the Chinese subgroup (PP3M: 6 [6%], PP1M: 7 [7%]). The median time to relapse was not estimated in any of the populations due to low number of relapses (Table 2).
The primary reasons for relapse were similar between the East Asian subgroups and the global population. Most common reasons were increase in the PANSS total score by ≥25% or 10-point increase (China: PP3M: 3 [3%], PP1M: 4 [4%]; Japan: PP3M: 8 [16%], PP1M: 8 [14%]; East Asia: PP3M: 12 [7%], PP1M:12 [7%] and global population: PP3M: 26 [6%], PP1M: 26 [5%]) and psychiatric hospitalization (China: PP3M: 2 [2.0%], PP1M: 4 [4.0%]; Japan: PP3M: 2 [4%], PP1M: 8 [14%]; East Asia: PP3M: 5 [3%], PP1M: 12 [7%] and global population: PP3M: 16 [3%], PP1M: 22 [4%]).
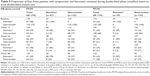
Secondary efficacy endpoints
The mean (SD) change from DB baseline to endpoint in the PANSS total score (mITT DB analysis set) was similar for PP3M and PP1M treatment groups for East Asia (PP3M: −2.8 [11.73], PP1M: −3.3 [12.59]), China (PP3M: −5.8 [8.93], PP1M: −4.5 [9.89]) and global population (PP3M: −3.5 [12.50], PP1M: −4.3 [11.78]). The mean (SD) changes from DB baseline to endpoint in other secondary efficacy parameters were also similar to the global population for 1) CGI-S: East Asia (PP3M: −0.2 [0.89], PP1M: −0.1 [0.80]), China (PP3M: −0.3 [0.83], PP1M: −0.2 [0.78]) and global population (PP3M: −0.1 [0.84], PP1M: −0.1 [0.75]) and 2) PSP: East Asia (PP3M: 0.1 [10.48], PP1M: 0.5 [10.10]), China (PP3M: 1.2 [10.67], PP1M: 1.9 [9.58]) and global population (PP3M: 1.3 [10.22], PP1M: 1.9 [9.21]), as shown in Table 3.
In contrast to the overall East Asian and the Chinese subgroups, PANSS total scores were similar or slightly increased from DB baseline to endpoint in the Japanese subgroup, that is, PP3M: 1.7 (12.86) and PP1M: −0.4 (16.81). Also, a small increase in CGI-S scores (PP3M: 0.2 [0.83], PP1M: 0.2 [0.84]) and decrease in PSP scores (PP3M: −1.8 [10.12], PP1M: −2.4 [11.07]) was observed in both PP3M- and PP1M-treated patients in the Japanese subgroup.
Symptomatic remission during the last 6 months of the DB phase was attained by 50% of the patients from both the PP3M and the PP1M treatment groups of the East Asian subgroup (no excursion allowed), as shown in Table 4A. Percentage of patients who attained both symptomatic and functional remission during the last 6 months of the DB phase was similar between both the treatment groups of the East Asian population (PP3M: 49 [29%]), PP1M: 50 [29%]), as shown in Table 4B. Patients who were symptomatic and functional remitters at DB baseline achieved higher rates of symptomatic and functional remission at week 48 (PP3M: 28 [78%], PP1M: 27 [87%]) than those who were nonremitters at DB baseline (PP3M: 33 [37%], PP1M: 25 [27%]), as show in Table 5.
Exploratory endpoints
In the East Asian patients with schizophrenia treated with oral antipsychotics prior to study entry, a significantly lower caregiving burden (P<0.001) was observed with the use of PP1M and PP3M at the end of the DB phase as compared to OL baseline (mean [SD]: 24.0 [17.03] versus 30.9 [16.73]), as shown in Figure 3.
Safety
Safety results from the global population have been reported previously.22 Incidence of TEAEs in the OL phase (ITT-OL analysis set) was greater in the overall East Asian subgroup (364/510 [71%]) compared with the global population (846/1,429 [59%]). Within the East Asian subgroup, the highest incidence was reported in the Japanese population (132/175 [75%]), followed by Chinese (198/296 [67%]). Similarly, in the DB phase (safety analysis set), incidence of TEAEs was higher in the East Asian subgroup (PP3M: 138/170 [81%], PP1M: 132/174 [76%]) as compared with the global population (PP3M: 342/504 [68%], PP1M: 340/512 [66%]). Within East Asia, frequency of TEAEs in the DB phase was higher in Japan (PP3M: 48/52 [92%], PP1M: 51/56 [91%]) compared with China (PP3M: 78/104 [75%], PP1M: 71/106 [67%]). The most frequently reported TEAE during the DB phase was increased weight, with higher incidence found in the East Asian subgroup (PP3M: 53/170 [31%]; PP1M: 54/174 [31%]) than the global population (PP3M: 105/504 [21%]; PP1M: 109/512 [21%]). Chinese subgroup (PP3M: 38/104 [37%]; PP1M: 37/106 [35%]) also showed a higher incidence of increased weight in the DB phase than Japanese (PP3M: 13/52 [25%]; PP1M: 11/56 [20%]), as presented in Table 6. Most of the TEAEs were mild to moderate in severity. Totally, 6/170 (4%) East Asian patients in the PP3M group and 4/174 (2%) in the PP1M group discontinued the study drug due to a TEAE in the DB phase (safety analysis set).
Incidence of serious TEAEs in the OL phase was comparable between the overall East Asian subgroup (43/510 [8%]), Chinese (20/296 [7%]), Japanese (18/175 [10%]) and the global population (101/1,429 [7%]). Proportion of serious TEAEs in the DB phase was similar between the East Asian subgroup (PP3M: 9/170 [5%], PP1M: 16/174 [9%]) and the global population (PP3M: 26/504 [5%], PP1M: 37/512 [7%]). A slightly lower number of serious TEAEs were observed in the Chinese subgroup (PP3M: 3/104 [3%], PP1M: 5/106 [5%]) than Japanese (PP3M: 5/52 [10%], PP1M: 10/56 [18%]) due to higher rate of relapse of Japanese patients and serious TEAEs related to the primary illness.
Two deaths (one each in the OL and DB phases) were reported in the East Asian subgroup. The death during the OL phase occurred from sudden cardiac arrest and the death during the DB phase occurred as a result of toxicity to various agents.
Incidence of EPS-related TEAEs in the OL phase was higher in the East Asian subgroup (104/510 patients [20%]) versus the global population (180/1,429 [13%]) and in the Chinese subgroup (73/296 patients [25%]) versus the Japanese subgroup (21/175 patients [12%]). The most common EPS-related TEAEs in the DB phase were those grouped under hyperkinesia, Parkinsonism and tremor, with a comparable incidence across both Chinese and Japanese subgroups treated with PP3M and PP1M. Overall, 118/510 (23%) patients from the East Asian subgroup used anti-Parkinson medication in the OL phase (Table S6). In the DB phase, among the East Asian subgroups, anti-Parkinson medication was used by 38/170 (22%) patients in PP3M group and 32/174 (18%) patients in the PP1M group (Table S7).
Mean (SD) change from DB baseline in body weight in the overall East Asian subgroup and in the Chinese and Japanese subgroups in the PP3M- and PP1M-treated patients was <2 kg. Incidence of glucose-related TEAEs was slightly higher in the Japanese subgroup (PP3M: 5/52 [10%], PP1M: 5/56 [9%]) compared with the Chinese subgroup (PP3M: 3/104 [3%], PP1M: 4/106 [4%]), and also in comparison with the overall East Asian population (PP3M: 8/170 [5%], PP1M: 10/174 [6%]) and the global population (PP3M: 13/504 [3%], PP1M: 25/512 [5%]). In the patients from East Asia, potentially prolactin-related TEAEs, such as breast pain (n=2), galactorrhea (n=2) and gynecomastia (n=1), were observed only in the PP3M-treated patients; no increases in blood prolactin levels from DB baseline were noted with either treatment.
For the East Asian patients, TEAE of injection site induration was reported more frequently in the PP3M group (9/170 [5%]) than the PP1M group (4/174 [2%]) in the DB phase; injection site pain was only reported in patients treated with PP3M (n=3). Irrespective of the treatment, the Columbia Suicide Severity Rating Scale indicated that there was no worsening in suicidal ideation or behavior in the DB phase.
Discussion
In this subgroup analysis of the East Asian population stabilized on PP1M, the efficacy of PP3M was consistent with that of the global population.22 Although the study was not powered to demonstrate noninferiority in any subgroup (including the East Asian subgroups), the difference in relapse-free rates for PP3M and PP1M for East Asian population was consistent with the global findings and the lower bound of the 95% CI was ≥-15% (with 15% being the noninferiority margin). Approximately 80% of patients from the Chinese and Japanese subgroups completed the 48-week DB treatment with multiple injections of PP3M.
In the overall East Asian subgroup, demographic characteristics of patients were consistent with the global population and similar across the Chinese and Japanese subgroups, except that the Japanese patients had a higher mean age (43 years) as compared to patients from China (32 years). Baseline disease characteristics were similar between the patients receiving either PP1M or PP3M across East Asia. Number of previous hospitalizations in the past 2 years prior to study entry was similar in the Chinese and Japanese subgroups; however, patients from Japan had a longer duration of prior hospitalization, compared with those from China. This may be attributed to the differences in psychiatric treatment practices in Japan, compared to the rest of the world. The average length of hospital stay for psychiatric inpatients in Japan was higher than in most countries, with a reported approximate duration of 291.9 days in 2014 and 296.1 days in 2011.24–27 In long-stay schizophrenic patients, the average duration of stay has been reported to be 8.5 years, with >71% of the patients likely to stay in hospitals for >1 year.28
Relapse rates observed in this study were consistent with those observed in other studies evaluating PP1M and PP3M.16,29 The Japanese subgroup, however, had higher proportion of patients who experienced a relapse event (PP3M: 17.6%, PP1M: 23.2%) during the study, although the relapse event rate was not higher than that of assumption (30%) prior to the study. This may, in part, have resulted from the nature of patients enrolled. It is well documented that antipsychotic polypharmacy is a relatively common practice associated with schizophrenia treatment in Asia, particularly in Japan.30 As expected, most of the patients in Japan were previously stabilized on multiple antipsychotics possibly due to severity of illness prior to study entry. Discontinuation of these antipsychotics prior to study entry and switching to PP1M or PP3M monotherapy in these patients may have triggered relapse. Additionally, even though the goal was to have patients discharged from the hospital prior to randomization, higher rate of chronic hospitalization in Japan as a result of cultural attitudes and social stigma associated with mental illness may have prolonged hospitalization and unlike in other countries, patients in Japan were allowed to remain voluntarily in the hospital during the DB phase.28,31 This may have allowed additional detection of mild relapses that may not have been necessarily captured in scheduled monthly visits as in other global studies.
Consistent with previous findings,15,17,32,33 an overall improvement from baseline in secondary efficacy parameters (PANSS, CGI-S and PSP scores) was observed in the PP1M- and PP3M-treated patients (after they were stabilized in the OL phase) in the Chinese and overall East Asian subgroups. Patients from Japan did not demonstrate an improvement in symptoms or social performance scales during the DB phase, possibly related to the potential reasons of higher relapse rate in Japan, described previously. A higher rate of concomitant benzodiazepine use in the Japanese subgroup is indicative of low symptom control, compared with the overall East Asian and global populations. Although the BMI ranges were similar in the Chinese and Japanese populations, this difference in efficacy outcomes may perhaps be relevant to the differences in the extent of drug exposure in the Japanese subgroup. In this study, most patients from Japan received lower doses of PP3M compared with the patients in China and overall East Asia subgroups; only 24% of the Japanese patients had received a 525 mg eq. dose of PP3M at week 36, compared to 45% of patients in the global population (mITT DB analysis set). However, in the global study, majority (>50%) of the patients receiving high doses were Caucasian, which could explain the difference in extent of drug exposure due to the differences in BMI.
Besides the relapse rate, remission is another clinically important treatment outcome that determines the success of antipsychotic therapy.34 Overall, half of the total number of patients in the East Asian subgroup (50% each in PP3M and PP1M) of this study achieved symptom remission at the end of the 48-week DB phase. However, it may be worthwhile to note that symptomatic remission does not necessarily translate to full functional recovery in schizophrenic patients.9 As much as alleviation of symptoms is essential, improvement in social functioning remains the ultimate goal of clinicians.35 In this study, the proportion was similar for the patients who remained stable (patients who maintained symptomatic remission with one excursion allowed) and who had functional recovery during the last 6 months before the end of the study for both the treatment groups in the East Asian subgroup (PP3M: 49 [28.8%]; PP1M: 50 [28.7%]).
Symptomatic remission and functional recovery at the end of the 48-week DB phase were more frequently observed in patients who were remitters at DB baseline, compared to those who were nonremitters. Symptomatic remission and functional improvement at the end of the study are thus strongly correlated to the symptom and functional severity at DB baseline. Early response to PP1M, indicated by improvement in symptomatic and functional parameters from OL baseline to DB baseline, may therefore foretell sustained symptomatic remission and functional recovery in patients treated subsequently with either of the LAIs (PP3M or PP1M).
Besides the behavioral traits associated with schizophrenic symptoms, impaired social and cognitive function in patients affects their day-to-day activities and necessitates the support of a caregiver. Outside clinical settings, caregivers are usually the family members or relatives of the patient.36 Studies have reported that caregivers of patients with schizophrenia experience varying degrees of financial, emotional, physical and psychological burden associated with caring, sometimes causing a negative impact on their own work and personal life.37,38 Burden of care can be assessed in terms of objective (effects of caregiving on daily tasks) and subjective (caregivers’ perception of burden) components associated with caregiving.38 The IEQ is an easy-to-administer and reliable multicomponent tool to assess various domains associated with treatment on caregivers.37,39 In this study, reduced IEQ domain scores indicated that treatment with both LAIs (PP3M or PP1M) in the East Asian subgroup significantly reduced the caregiving burden from OL baseline to the end of study.
The overall incidence of TEAEs (OL and DB phase) in general was higher in the East Asian subgroup compared to the global subgroup which could be attributed to racial differences in the population. Despite this, occurrence of serious TEAEs and withdrawal due to TEAEs were low in this population. Frequency of TEAEs was generally similar between East Asian and global populations, except for the TEAE of increased weight, which was higher in the overall East Asian subgroup (PP3M: 31%; PP1M: 31%) than the global population (PP3M: 21%; PP1M: 21%), notably in the Chinese subgroup (PP3M: 37%; PP1M: 35%), compared with Japan (PP3M: 25%; PP1M: 20%). A comparatively higher percentage of patients in the Chinese subgroup (64%) had normal BMI at OL baseline, as compared with the global population (44%), likely leading to higher weight gain in this population.40 The magnitude of weight gain in the East Asian subgroup (<2 kg), however, was similar to the global population (~1.5 kg) and was consistent with the findings reported in previous studies.16,32,41,42 Consistent with previous reports, frequency of glucose-related and potentially prolactin-related TEAEs was low in this study.15–17 There was no significant difference in the frequency of TEAEs in the Japanese patients, except for marginally greater incidence of headache, delusion, dental caries, eczema and diarrhea.
Nevertheless, results of the subgroup analyses should be interpreted with caution, due to the limitation of a relatively small sample size of the East Asian population and also because the study was not powered to detect noninferiority of PP3M over PP1M formulation in the East Asian subgroups. Another limitation was that patient satisfaction with respect to PP3M as compared with PP1M was not explored in this study.
Furthermore, since the study was conducted only in four East Asian countries (China, Japan, South Korea and Taiwan), the findings of the subgroup analyses may not be representative of the entire Asian population.
Conclusion
The findings demonstrate that PP3M was efficacious in East Asian patients with schizophrenia, consistent with the results from the global population. Although TEAEs were slightly higher in the East Asian subgroup compared with the global population, no new safety signals unique to the East Asian population were observed during the study. PP3M can be considered as maintenance therapy for relapse prevention in East Asian patients with schizophrenia following treatment with PP1M.
Acknowledgments
The authors acknowledge Padmini Deshpande and Dr Sonia Philipose (SIRO Clinpharm Pvt. Ltd.) for providing writing assistance and Dr Ellen Baum (Janssen Research & Development, LLC) for providing additional editorial support for the development of this manuscript. Padmini Deshpande developed the first draft of the manuscript under the direction of the authors and the authors reviewed all subsequent drafts for content integrity. Manuscript writing was funded by Janssen Research & Development, LLC, USA.
The authors thank the study participants, without whom the study would never have been accomplished, and also thank the investigators for their participation in the study.
This trial was funded by Janssen Research & Development, LLC, USA. Data were presented at the 30th CINP World Congress of Neuropsychopharmacology, Seoul, South Korea (3–5 July 2016) and the RANZCP Congress, Hong Kong (8–12 May 2016).
Author contributions
AJS, SG and DH were involved in the study design, data collection, analysis and interpretation. HX and IN were the project statisticians and oversaw data analysis and interpretation. PR was involved in pharmacokinetic analysis. MM is the Global Medical Affairs leader and was involved with the development and review of the manuscript. YF, LY and MT were involved in data interpretation and development of the manuscript. DL, GW, JSY and JJC were the study investigators. All authors met the ICMJE criteria and those who fulfilled the criteria are listed as authors. All authors had access to the study data, provided direction and formal review of the manuscript, and made the final decision about where to publish these data. All authors contributed toward drafting and revising the paper and agreed to be accountable for all aspects of the work.
Disclosure
AJS, HX, SG, IN, DH and MM are employees and shareholders of Janssen Research & Development, LLC, USA (parent company Johnson and Johnson). PR is an employee of Janssen Research & Development, Beerse, Belgium. YF is an employee of Janssen Pharmaceutical Companies of Johnson & Johnson, Singapore and LY is an employee of Janssen Research & Development, Beijing, China, while MT is an employee of Janssen Pharmaceutical KK, Tokyo, Japan. The other authors report no conflicts of interest in this work.
References
Nose M, Barbui C, Tansella M. How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychol Med. 2003;33(7):1149–1160. | ||
Lacro JP, Dunn LB, Dolder CR, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. | ||
Bodén R, Brandt L, Kieler H, Andersen M, Reutfors J. Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Res. 2011;133(1–3):36–41. | ||
Liu-Seifert H, Adams DH, Kinon BJ. Discontinuation of treatment of schizophrenic patients is driven by poor symptom response: a pooled post-hoc analysis of four atypical antipsychotic drugs. BMC Med. 2005;3(1):21. | ||
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New Engl J Med. 2005;353(12):1209–1223. | ||
Perkins DO, Gu H, Weiden PJ, McEvoy JP, Hamer RM, Lieberman JA; Comparison of Atypicals in First Episode study group. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry. 2008;69(1):106–113. | ||
Lambert M, Schimmelmann BG, Naber D, et al. Prediction of remission as a combination of symptomatic and functional remission and adequate subjective well-being in 2960 patients with schizophrenia. J Clin Psychiatry. 2006;67(11):1690–1697. | ||
Kane JM. Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007;68 (Suppl 14):27–30. | ||
Barak Y, Aizenberg D. Clinical and psychosocial remission in schizophrenia: correlations with antipsychotic treatment. BMC Psychiatry. 2012;12(1):108. | ||
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S. Oral versus depot antipsychotic drugs for schizophrenia – a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127(1):83–92. | ||
Valenstein M, Copeland LA, Owen R, Blow FC, Visnic S. Adherence assessments and the use of depot antipsychotics in patients with schizophrenia. J Clin Psychiatry. 2001;62(7):545–551. | ||
Carpiniello B, Pinna F. Critical appraisal of 3-monthly paliperidone depot injections in the treatment of schizophrenia. Drug Des Devel Ther. 2016;10:1731–1742. | ||
McEvoy JP. Risks versus benefits of different types of long-acting injectable antipsychotics. J Clin Psychiatry. 2006;67 (Suppl 5):15–18. | ||
Remington GJ, Adams ME. Depot neuroleptic therapy: clinical considerations. Can J Psychiatry. 1995;40(3):S5–S11. | ||
Gopal S, Hough DW, Xu H, et al. Efficacy and safety of paliperidone palmitate in adult patients with acutely symptomatic schizophrenia: a randomized, double-blind, placebo-controlled, dose-response study. Int Clin Psychopharmacol. 2010;25(5):247–256. | ||
Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. | ||
Takahashi N, Takahashi M, Saito T, et al. Randomized, placebo-controlled, doubleblind study assessing the efficacy and safety of paliperidone palmitate in Asian patients with schizophrenia. Neuropsychiatr Dis Treat. 2013;9:1889–1898. | ||
Banerjee A. Cross-cultural variance of schizophrenia in symptoms, diagnosis and treatment. Georget Undergrad J Health Sci. 2012;6(2):18–24. | ||
Bauer SM, Schanda H, Karakula H, et al. Culture and the prevalence of hallucinations in schizophrenia. Compr Psychiatry. 2011;52(3):319–325. | ||
Stauffer VL, Sniadecki JL, Piezer KW, et al. Impact of race on efficacy and safety during treatment with olanzapine in schizophrenia, schizophreniform or schizoaffective disorder. BMC Psychiatry. 2010;10:89. | ||
Coppola D, Liu Y, Gopal S, et al. A one-year prospective study of the safety, tolerability and pharmacokinetics of the highest available dose of paliperidone palmitate in patients with schizophrenia. BMC Psychiatry. 2012;12(1):1–14. | ||
Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority study. Int J Neuropsychopharmacol. 2016;19(7). pii: pyw018. | ||
Andreasen NC, Carpenter Jr WT, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441–449. | ||
Ministry of Health, Labor, and Welfare. The national patient survey 2011. Available from: http://www.mhlw.go.jp/english/database/db-hss/dl/sps_2011_03.pdf. Accessed August 19, 2016. | ||
Ministry of Health, Labor, and Welfare. The national patient survey 2014. Available from: http://www.mhlw.go.jp/english/database/db-hss/dl/sps_2014_03.pdf. Accessed August 19, 2016. | ||
Imai H, Hosomi J, Nakao H, et al. Characteristics of psychiatric hospitals associated with length of stay in Japan. Health Policy. 2005;74(2):115–121. | ||
Nakanishi M, Niimura J, Tanoue M, Yamamura M, Hirata T, Asukai N. Association between length of hospital stay and implementation of discharge planning in acute psychiatric inpatients in Japan. Int J Ment Health Syst. 2015;9:23. | ||
Oshima I, Mino Y, Inomata Y. Institutionalisation and schizophrenia in Japan: social environments and negative symptoms. Br J Psychiatry. 2003;183(1):50–56. | ||
Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830–839. | ||
Sim K, Su A, Fujii S, et al. Antipsychotic polypharmacy in patients with schizophrenia: a multicentre comparative study in East Asia. Br J Clin Pharmacol. 2004;58(2):178–183. | ||
Ando S, Yamaguchi S, Aoki Y, Thornicroft G. Review of mental-health-related stigma in Japan. Psychiatry Clin Neurosci. 2013;67(7):471–482. | ||
Pandina GJ, Lindenmayer JP, Lull J, et al. Randomized, placebo-controlled study to assess the efficacy and safety of three doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharmacol. 2010;30(3):235–244. | ||
Li H, Turkoz I, Zhang F. Efficacy and safety of once-monthly injection of paliperidone palmitate in hospitalized Asian patients with acute exacerbated schizophrenia: an open-label, prospective, noncomparative study. Neuropsychiatr Dis Treat. 2016;12:15–24. | ||
Nasrallah HA, Lasser R. Improving patient outcomes in schizophrenia: achieving remission. J Psychopharmacol. 2006;20 (Suppl 6):57–61. | ||
Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association; Steering Committee on Practice Guidelines. Practice guideline for the treatment of partients with schizophrenia. Am J Psychiatry. 2004;161 (Suppl 2):1–56. | ||
Caqueo-Urízar A, Gutiérrez-Maldonado J, Miranda-Castillo C. Quality of life in caregivers of patients with schizophrenia: a literature review. Health Qual Life Outcomes. 2009;7(1):84. | ||
Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: domains and distress. Schizophr Bull. 1998;24(4):609–618. | ||
Awad AG, Voruganti LN. The burden of schizophrenia on caregivers. Pharmacoeconomics. 2008;26(2):149–162. | ||
van Wijngaarden B, Schene AH, Koeter M, et al. Caregiving in schizophrenia: development, internal consistency and reliability of the Involvement Evaluation Questionnaire – European Version. Br J Psychiatry Suppl. 2000;177(39):s21–s27. | ||
Si T, Zhang K, Tang J, et al. Efficacy and safety of flexibly dosed paliperidone palmitate in Chinese patients with acute schizophrenia: an open-label, single-arm, prospective, interventional study. Neuropsychiatr Dis Treat. 2015;11:1483–1492. | ||
Hough D, Lindenmayer JP, Gopal S, et al. Safety and tolerability of deltoid and gluteal injections of paliperidone palmitate in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(6):1022–1031. | ||
Kramer M, Litman R, Hough D, et al. Paliperidone palmitate, a potential long-acting treatment for patients with schizophrenia. Results of a randomized, double-blind, placebo-controlled efficacy and safety study. Int J Neuropsychopharmacol. 2010;13(5):635–647. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.