Back to Journals » Journal of Pain Research » Volume 16
Efficacy and Safety of Naloxegol in Patients with Chronic Non-Cancer Pain Who Experience Opioid-Induced Constipation: A Pooled Analysis of Two Global, Randomized Controlled Studies
Authors Chey WD, Brenner DM, Cash BD, Hale M, Adler J, Jamindar MS, Rockett CB, Almenoff JS , Bortey E, Gudin J
Received 9 May 2023
Accepted for publication 18 August 2023
Published 28 August 2023 Volume 2023:16 Pages 2943—2953
DOI https://doi.org/10.2147/JPR.S417045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amitabh Gulati
William D Chey,1 Darren M Brenner,2 Brooks D Cash,3 Martin Hale,4 Jeremy Adler,5 Mansi S Jamindar,6 Carol B Rockett,6 June S Almenoff,6 Enoch Bortey,7 Jeffrey Gudin8
1Department of Internal Medicine, Division of Gastroenterology and Hepatology, Michigan Medicine, Ann Arbor, MI, USA; 2Departments of Medicine and Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA; 3Division of Gastroenterology, Hepatology, and Nutrition at the University of Texas Health Science Center at Houston, Houston, TX, USA; 4Gold Coast Research, L.L.C, Miami, FL, USA; 5Pacific Pain Medicine Consultants, Encinitas, CA, USA; 6Medical Affairs, RedHill Biopharma, Inc, Raleigh, NC, USA; 7Pharmaceutical Development Strategies, L.L.C, Chapel Hill, NC, USA; 8Department of Anesthesiology and Pain Management, University of Miami, Miami, FL, USA
Correspondence: June S Almenoff, Email [email protected]
Objective: This study evaluates the onset, magnitude, and consistency of improvement of opioid-induced constipation (OIC) symptoms with naloxegol treatment.
Methods: This was a pooled analysis of two Phase 3, double-blind, randomized, placebo-controlled studies (KODIAC-04/05, NCT01309841/NCT01323790) in patients with chronic non-cancer pain and OIC treated with naloxegol 25mg or 12.5mg daily. This analysis assessed improvements in response rates, frequency of spontaneous bowel movement (SBM) and complete SBMs (CSBM), OIC constipation symptoms (straining, stool consistency), time to first post-dose SBM and CSBM, and onset of adverse events over the 12-week period.
Subjects: The population of 1337 subjects had a mean age of 52 years and mean duration of opioid use of 3.6 years at baseline. Mean SBM frequency was 1.4/week.
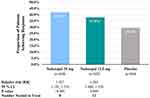
Results: Naloxegol 25mg and 12.5mg demonstrated significantly higher response rates vs placebo (PBO) [41.9% (P < 0.001), 37.8% (P = 0.008), 29.4% respectively]. Rapid (within 1 week) and sustained (over 12 weeks) symptom improvement was significantly greater for naloxegol vs PBO (P < 0.05). Both doses showed statistically significant and clinically meaningful improvements in straining, stool consistency, number of SBMs and CSBMs/wk. Significantly shorter times to first post-dose SBM and CSBM were observed with naloxegol vs PBO (SBM HR: 25mg = 1.90, 12.5mg= 1.60; CSBM HR: 25mg = 1.42, 12.5mg = 1.36; P < 0.001 for each regimen). Adverse events occurred more frequently in the naloxegol 25mg group and were most frequently reported during the first week.
Conclusion: In patients with chronic non-cancer pain, naloxegol 25mg and 12.5mg demonstrated significantly higher response rates and rapid and sustained improvements in OIC symptoms compared with PBO.
Keywords: opioid-induced constipation, naloxegol, clinical trials
Introduction
The Centers for Disease Control and Prevention (CDC) estimate that 50.2 million US adults experience chronic pain,1 and systematic reviews reveal that 23–36% of these individuals consume opioids.2–6 Opioid-induced constipation (OIC) is a common and bothersome side effect of chronic opioid use and is estimated to occur in 40–80% of patients.7–9 OIC results from the binding of opioids to μ-opioid receptors located in the enteric nervous system leading to decreased gastrointestinal motility, reduced intestinal fluid and electrolyte secretion and increased reabsorption, and sphincter dysfunction.10–12 OIC commonly persists with chronic opioid use, whereas other adverse effects such as nausea and vomiting lessen over time.13–15 Gastrointestinal symptoms associated with OIC include decreased stool frequency, straining, hard stools, and a sense of incomplete evacuation.7 The presence of OIC negatively impacts patients’ health-related quality of life (HR-QOL), ability to perform daily activities and work productivity, and results in significant patient burden.16 In a recent survey of 447 patients with non-cancer pain, over 50% reported modifying their opioid regimen due to constipation.17
The 2019 American Gastroenterological Association Guideline on the medical management of OIC recommends the use of laxatives as first-line agents for the treatment of OIC.9 Similar recommendations had been made in the European expert consensus statement.18 However, 93% of patients experience inadequate response to laxatives and 26% meet criteria for having an inadequate response to two laxatives.14 Given these high rates of inadequate response and the persistent and significant symptom burden of OIC, targeted pharmacological treatments are needed to provide more effective relief. Naloxegol (Movantik®) is a peripherally acting mu-opioid receptor antagonist (PAMORA) specifically designed to antagonize opioid binding at μ-opioid receptors in the GI tract. This reduces the constipating effects of opioids while having negligible central nervous system (CNS) penetration, thus limiting potential interference with analgesia. Naloxegol has demonstrated a rapid and predictable onset of relief of OIC symptoms in subjects treated with opioids for chronic non-cancer pain in two phase 3 trials (KODIAC-04/-05[N = 1337]; NCT01309841/NCT01323790).19,20 In the US, naloxegol is indicated for use in adult patients with OIC with chronic non-cancer pain, including patients with chronic pain related to prior cancer or its treatment who do not require frequent (eg, weekly) opioid dosage escalation (Movantik, US prescribing information). In Europe, it is indicated for adult patients with OIC who have an inadequate response to laxatives (LIR) (Moventig EU SMPC). A previous pooled analysis (KODIAC-04/-05) of the inadequate response to laxatives (LIR) subpopulation showed favorable outcomes.21 In the US, naloxegol is indicated for adult patients with chronic non-cancer OIC (Movantik, US prescribing information), irrespective of laxative use. Here, we present a pooled analysis of the total ITT population, which includes both LIR and patients with OIC who were not classified as LIR.
Given the high symptom burden of OIC and the importance of prompt and long-term relief to patients and providers, this analysis aims to assess the efficacy and safety of naloxegol in the full, pooled population of patients included in phase 3 studies of naloxegol for OIC.
Methods
Data Source
This study is a pooled analysis of two identical phase 3, double-blind, randomized, placebo-controlled studies (KODIAC 4/5; NCT01309841/NCT01323790) in patients with chronic non-cancer pain and OIC treated with naloxegol 25 mg or 12.5 mg daily. The studies were conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonisation. An ethics committee or institutional review board at each study site approved the final study protocol and informed-consent form. All patients provided written informed consent at screening, before any study procedures were performed. Patients who subsequently underwent randomization recorded their symptoms in electronic diaries (eDiaries) throughout the treatment period. The primary endpoint for KODIAC 4/5 was the response rate during the 12-week treatment period. Response was defined as three or more SBM/week and an increase of one or more SBM/week over baseline for at least 9 of 12 treatment weeks and at least 3 of the final 4 treatment weeks. The use of laxatives (except for prespecified rescue laxatives) was not permitted during the 12-week treatment period. OIC symptoms including frequency of spontaneous bowel movements (SBM), complete SBM (CSBM), straining, and stool consistency were recorded. A sense of complete evacuation was documented for each SBM. The degree of straining was measured on a scale of 1, not at all, to 5, an extreme amount. Stool consistency was assessed with the Bristol Stool Scale (BSS) (1–7 ranging from hard to watery stools).
Statistical Analyses
The results of two identically designed studies were pooled to investigate the effect of treatment with respect to efficacy and safety outcomes. It is important to note that the sample size and power considerations for each study were based solely on the primary endpoint of those studies. Thus, the potential treatment effect on endpoints other than the primary endpoint needs to be investigated by pooling the data. For efficacy outcomes, inferential statistics were provided by p-values, and for safety outcomes, the data were summarized descriptively. Response rate was analyzed by relative risk, interpreted as the likelihood of treatment achieving the endpoint compared with PBO (treatment response). P-values shown in these analyses are considered nominal and not adjusted for multiplicity.
The time to first post-dose SBM and CSBM (without rescue medication) for each naloxegol dose vs PBO was analyzed via the Cox proportional hazard model; treatment effect was analyzed via the hazard ratio (HR). The median time to first post-dose SBM & CSBM was derived via the Kaplan–Meier (KM) method. Onset of action was summarized descriptively by the proportion of patients with SBM and CSBM from 4 hours to 48 hours post first dose, which reflects a clinically relevant timeframe.20
Patient-reported symptom data were analyzed by mixed-model repeated-measures models with fixed effects for baseline-dependent variables, baseline laxative response, treatment, treatment-time interaction, and random effects for study center.
Safety analyses were conducted for subjects in the intent-to-treat (ITT) population who had received one or more doses of study drug. Pooled safety data were evaluated from the two phase 3 studies.
Results
Patients
A total of 1337 patients receiving naloxegol (12.5 mg, n = 445; 25 mg, n = 446) or PBO (n = 446) were included in the ITT analysis of the KODIAC-04 and −05 studies. Baseline characteristics were balanced across the study groups and were similar between the two studies (Table 1). Key demographics included mean age (52 years), ≥65 years of age (11%), female (62.4%), White (79%), and Black (18.6%). Back pain was the most common reason for pain (56.5%) followed by arthritis (9.8%). Enrolled patients had been consuming opioids for an average of 3.6 years. The mean baseline opioid morphine equivalent daily dosage was 137.7 mg. The majority of patients had taken a laxative in the 2 weeks before enrollment (71%); the most commonly used laxatives were stimulants (61.9% and 52.9%) and stool softeners (28.9% and 31.9%) across treatment groups in KODIAC-04 and KODIAC-05 respectively. More than 50% of patients in the studies were classified as having an inadequate laxative response. Baseline OIC symptoms were balanced across the treatment groups (25 mg and 12.5 mg) and PBO (Table 1). There was high symptom burden at baseline with low frequencies of SBM (1.3–1.6 SBM/week) and CSBM (0.4–0.5 CSBM/week), and a moderate amount of straining (score ~3) (Table 1).
 |
Table 1 Baseline Demographics and Clinical Characteristics; KODIAC-04 and KODIAC-05 Pooled IIT Population |
Response Rates
Overall response rates to naloxegol 25 mg and 12.5 mg were significantly greater than PBO (41.9%, 37.8%, 29.4% respectively) Figure 1 yielding numbers needed to treat (NNT) for naloxegol 25 mg and 12.5 mg of approximately 8 and 12, respectively (Figure 1). Patients treated with naloxegol 25 mg or 12.5 mg were 42.7% (RR: 1.427; 95% CI: 1.192–1.710; p < 0.001) and 28.5% (RR: 1.285; 95% CI: 1.066–1.550; p = 0.008) more likely to achieve response than patients treated with PBO (Supplementary Table 1). Persistently significant improvements in response rates and similar NNTs were observed across the entire study period for both naloxegol doses vs PBO (Supplementary Table 1).
Change from Baseline in OIC Symptoms Over 12 Weeks
Significantly greater OIC-related symptom improvements were observed for both naloxegol doses compared to PBO over the 12-week study period for degree of straining, stool consistency, and numbers of SBM and CSBM/week (p ≤ 0.01 for all comparisons (naloxegol 25 mg and 12.5 mg vs PBO) (Supplementary Table 2). Rapid improvements in straining and stool consistency were demonstrated as early as week 1 and were sustained through week 12 for both naloxegol doses vs PBO (Figure 2a and b).
Naloxegol demonstrated rapid and sustained significant improvements in stool frequency and numbers of SBM/week and CSBM/week over the 12-week study period vs PBO (p < 0.01). Significant improvements in SBM/week and CSBM/week were seen within 1 week and were sustained through 12 weeks for both naloxegol doses vs PBO (Figure 3a and b). Mean numbers of SBM/week nearly doubled from baseline to 12 weeks with naloxegol 25 mg (1.48 to 3.10) and naloxegol 12.5 mg (1.42 to 2.60 SBM/week). Mean numbers of CSBM/week increased over five-fold from baseline to 12 weeks with naloxegol 25 mg (0.4 to 2.12) and increased over three-fold for naloxegol 12.5 mg (0.5 to 1.69) (Supplementary Table 2).
Time to First Post-Dose OIC Symptom Improvement
Significantly reduced times to first SBM and CSBM were observed after first dose of naloxegol vs PBO. There was nearly a 5-fold reduction in median time to first post-dose SBM for naloxegol 25 mg vs PBO (25 mg: 7.8 hrs; 12.5 mg: 19.9 hrs; vs PBO: 36.4 hrs) (Figure 4a). The majority of patients treated with either naloxegol dose experienced an SBM within 24 hours of the first dose (25 mg: 65.5%; 12.5 mg: 58.4%; vs PBO: 36.5%). Time to first CSBM was nearly 3-fold faster with naloxegol 25 mg and twice as fast with naloxegol 12.5 mg vs PBO (median time to first post-dose CSBM: 53.4 hrs for naloxegol 25 mg, 71.2 hrs for naloxegol 12.5 mg vs 152 hours for PBO) (Figure 4b). Kaplan–Meir curves for time to first post-dose SBM and CSBM demonstrate clear separation. Patients treated with naloxegol achieved a first post-dose SBM 60–90% faster, and a CSBM 36–42% faster than placebo. (SBM HR: 25mg = 1.90; 12.5 mg = 1.60. CSBM HR: 25 mg = 1.42; 12.5 mg = 1.36. p < 0.001 for each regimen) (Figure 4a and b).
Safety
Most adverse events (AEs) were mild to moderate in severity and were most frequent in patients receiving naloxegol 25 mg. The most commonly observed AEs (≥5%) observed at a higher rate in the naloxegol groups vs placebo were abdominal pain, diarrhea, nausea and flatulence. The majority of AEs were non-serious (Table 2). The incidence of serious AEs was similar across treatment groups (25 mg [3.4%], 12.5 mg [5.7%], and PBO [5.2%]). The proportion of patients with AEs leading to discontinuation across treatment groups were: naloxegol 25mg (10.3%), naloxegol 12.5mg (4.8%), and PBO (5.4%). The most common GI AEs leading to discontinuation were abdominal pain (4%, 0.9%, 0.2%, respectively), diarrhea (3.1%, 0.9%, 0.7%, respectively), and nausea (1.1%, 1.1%, 0.2%, respectively). The onset of GI AEs was highest within the first week of therapy (Figure 5).
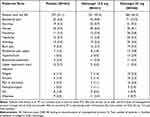 |
Table 2 Number (%) of Patients with the Most Common (≤2% Incidence in Any Treatment Group) AEs During the Treatment Period (KODIAC-04 and KODIAC-05 Pooled IIT Population) |
 |
Figure 5 Onset of gastrointestinal related adverse events associated with naloxegol; KODIAC-04 and KODIAC-05 Pooled IIT population. |
Discussion
Although treatment recommendations are evolving to limit the use of chronic opioids in non-cancer pain, there is nonetheless an important role for their use in appropriately selected patients.22 The efficacy of naloxegol for improving OIC symptoms in opioid using patients with chronic non-cancer pain was previously established in two phase 3 studies. Significant treatment responses were observed in KODIAC-04 for the 12.5 mg (p = 0.03) and 25 mg (p = 0.002) doses of naloxegol and in KODIAC-05 for the 25-mg dose (p = 0.01), which corresponded to increased response rates of 14–20% compared to PBO. Numerical improvement in response was shown for naloxegol 12.5 mg vs PBO in KODIAC-05.19 The current pooled analysis with a larger patient population confirms the efficacy and safety of both naloxegol doses, 25 mg and 12.5 mg, given once daily. The response rate over 12 weeks significantly increased by 8.4% (naloxegol 12.5 mg) and 12.5% (naloxegol 25 mg) over PBO and patients treated with naloxegol were 29–43% more likely to be treatment responders. This improvement is clinically relevant as the treatment response criteria were highly stringent, requiring three or more SBM/week plus an increase of one or more SBM/week over baseline for at least 9 of 12 treatment weeks, including at least 3 of the final 4 treatment weeks. Patients in this pooled analysis had high baseline symptom burden and on average had only 1.3–1.5 SBM/week. Consequently, the assigned treatment response criteria required, at a minimum, an approximate doubling of the number of SBM/week over the study period.
Consistent with the individual studies, this pooled analysis demonstrated naloxegol’s ability to provide significant, rapid, and sustained improvements in both stool frequency and OIC related GI symptoms. Both naloxegol doses demonstrated significantly reduced times to first SBM and CSBM compared with PBO. Time to first post-dose SBM was nearly 5-fold faster with naloxegol 25 vs PBO with 50% of patients achieving a bowel movement within 8 hours after the first dose and 66% achieving an SBM within the first day. Similarly, time to first post-dose CSBM was nearly 3-fold faster with naloxegol 25 mg vs PBO with 50% of patients achieving a CSBM within 53 hours. This is clinically relevant as at baseline, patients averaged one CSBM every 15 days.
Improvement in stool frequency and OIC symptoms at 12 weeks was demonstrated in the individual phase 3 studies of naloxegol,19 however the larger sample size of this pooled analysis demonstrates significant, rapid improvement in OIC symptoms as early as week 1 sustained through week 12 for both naloxegol doses vs placebo. The increase in SBM and CSBM frequency significantly improved within the first week and was maintained through week 12 for both naloxegol doses vs PBO. Both naloxegol doses also demonstrated rapid and significant improvement of OIC-related GI symptoms including straining and stool consistency as early as week 1 and through 12 weeks.
Previous work published by Tack et al21 analyzed the pivotal trial endpoints in a subpopulation of 720 subjects who were laxative inadequate responders prior to enrolling in the pivotal trials (KODIAC-04 and -05). This population constituted a key secondary endpoint in the pivotal trial and consisted of 54.6% in KODIAC-04 and 53.2% in KODIAC-05.
In this current analysis, we have evaluated the full ITT population, in order to increase the power of the analysis and to evaluate naloxegol-dose response in all 1337 patients who participated in the studies. It is noteworthy that in the EU, naloxegol is approved for the LIR population, whereas in the US, the product is approved for patients with chronic OIC, irrespective of laxative response status. Therefore, the current ITT analysis is highly relevant to all patients, as opposed to LIR patients only. Also, among the differences, we look at proportions of patients with complete spontaneous bowel movements (CSBM) as well as spontaneous bowel movements (SBM) over the first 48 hours. Complete SBMs are believed to be an important contributor to overall patient. Complete SBMs are believed to be an important contributor to overall patient satisfaction, and these were evaluated in greater detail in this analysis. We also ascertained the predictability and reliability of dose response for both the 12.5 and 25 mg doses in the ITT population, which supports potential dosing flexibility in the broader OIC population.
Importantly, the work shows a Kaplan–Meier analysis of time to first dose complete SBM, demonstrating rapid onset of action (Figure 4b), which are consistent with therapeutic effects of naloxegol for SBM (Figure 4a) for both doses.
The AE profile was consistent with the known profile of naloxegol, and no new safety signals were identified. The most common AEs observed were abdominal pain, diarrhea, and nausea and AEs were more frequently observed with the 25 mg dose. This analysis demonstrated that GI-related AEs most frequently occur within the first week of treatment, although they infrequently led to discontinuation of therapy. We hypothesize that these early GI AEs relate to the mobilization and wakening of the quiescent gut due to lessening of the GI side effects of opioids. Abdominal pain is likely associated with the restoration of peristalsis in a bowel full of stool, and the perception of diarrhea may be contributed to by the normalization of bowel function after a period of limited activity due to OIC. These are important counseling points to help establish patient expectations around the effects of naloxegol therapy for OIC.
The naloxegol FDA label recommends initiating therapy with 25 mg once daily in the morning and to reduce the dosage to 12.5 mg once daily if patients are unable to tolerate the higher dose. This may in part explain the results of KODAIC-05 in which naloxegol 12.5 mg did not demonstrate significant improvement in treatment response. However, this pooled analysis with a larger sample size, reinforces the efficacy and safety of both naloxegol doses in providing consistent treatment responses and rapid and sustained improvements in stool frequency and OIC related GI symptoms. This result is likely due to the higher statistical power of the considerably larger sample size of the pooled analysis vs the individual studies.
The key strengths of this analysis include the larger sample size from pooling the two identical phase 3 studies allowing for higher statistical power for subgroup analyses. The individual studies have a highly rigorous study design and include patients with high unmet medical burden. A key limitation is that the study protocol did not include an assessment of exact time to resolution of adverse events, so it precludes drawing conclusions regarding the duration of these AEs. A potential limitation of the work is that this pooled analysis is retrospective and that it is based on only two studies. However, for each study, the treatment effect was consistent across the endpoints evaluated, and the studies were pooled to allow for evaluation of overall treatment effect with regard to the endpoints indicated for naloxegol treatment.
Conclusion
This pooled analysis demonstrates the consistent efficacy and safety of two doses of naloxegol 25 mg and 12.5 mg. These benefits occur early and are sustained over time. The outcomes of this study suggest that both naloxegol doses are effective treatment options for patients with chronic non-cancer pain who are experiencing OIC.
Acknowledgments
The authors acknowledge Phil Yeung (Medical Affairs 360, LLC.) for his contributions to the study concepts.
Funding
Funding support for this research was provided by RedHill Biopharma Inc.
Disclosure
William Chey consulted for AbbVie, Biomerica, Comvita, Gemelli, Ironwood, Isothrive, QOL Medical, Nestle, Phathom Pharmaceuticals, Progenity, Quest, Redhill Biopharma, Salix, Urovant, and Vibrant and stock options in Coprata, Dieta, Gastro Girl, Kiwi Bioscience, Isothrive, and Modify Health. In addition, Dr William D Chey has a patent Rectal Expulsion Device issued. Darren Brenner is Consultant Advisor and/or Speaker for the following: Anji, Ardelyx, AbbVie, Salix, Ironwood, Takeda, Bayer, Alnylam, Arena, Gemelli Laborie, Vibrant, RedHill Biopharma Inc, and Mahana Therapeutics. Brooks Cash is a consultant: RedHill, Salix, Phathom, AbbVie, Takeda, Medtronic and a speaker for Salix, QOL, Anylam, AbbVie, Takeda. Martin Hale has no conflicts to report. Jeremy Adler is a speaker for Averitas, Redhill, California Academy of PAs and a Consultant for AppliedVR and AbbVie.
Mansi S. Jamindar and Carol B. Rockett are previous employees and stockholders of RedHill Biopharma Inc. and June S. Almenoff is a current employee and stockholder of RedHill Biopharma Inc. Enoch Bortey has no conflicts to report. Jeffrey Gudin is a consultant to Collegium, Hisamitsu, Redhill- Quest Diagnostics, Sanofi, and principal and on the Boards of Virpax and Optimus Health. No authors were compensated for work performed on this paper, except for RedHill Employees.
References
1. Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among U.S. Adults, 2019. NCHS Data Brief. 2020;2020:1–8.
2. Dahlhamer JM, Connor EM, Bose J, Lucas JL, Zelaya CE. Prescription opioid use among adults with chronic pain: United States, 2019. Natl Health Stat Report. 2021;2021:1–9.
3. De Sola H, Duenas M, Salazar A, Ortega-Jimenez P, Failde I. Prevalence of therapeutic use of opioids in chronic non-cancer pain patients and associated factors: a systematic review and meta-analysis. Front Pharmacol. 2020;11:564412. doi:10.3389/fphar.2020.564412
4. Mathieson S, Wertheimer G, Maher CG, et al. What proportion of patients with chronic noncancer pain are prescribed an opioid medicine? Systematic review and meta-regression of observational studies. J Intern Med. 2020;287(5):458–474. doi:10.1111/joim.13026
5. Wertheimer G, Mathieson S, Maher CG, et al. The prevalence of opioid analgesic use in people with chronic noncancer pain: systematic review and meta-analysis of observational studies. Pain Med. 2021;22(2):506–517. doi:10.1093/pm/pnaa322
6. Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. Pain. 2022;163(2):e328–e332. doi:10.1097/j.pain.0000000000002291
7. Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European patient survey (PROBE 1). Pain Med. 2009;10(1):35–42. doi:10.1111/j.1526-4637.2008.00495.x
8. Tuteja AK, Biskupiak J, Stoddard GJ, Lipman AG. Opioid-induced bowel disorders and narcotic bowel syndrome in patients with chronic non-cancer pain. Neurogastroenterol Motil. 2010;22(4):424–30, e96. doi:10.1111/j.1365-2982.2009.01458.x
9. Crockett SD, Greer KB, Heidelbaugh JJ, et al. American gastroenterological association institute guideline on the medical management of opioid-induced constipation. Gastroenterology. 2019;156(1):218–226. doi:10.1053/j.gastro.2018.07.016
10. Camilleri M. Opioid-induced constipation: challenges and therapeutic opportunities. Am J Gastroenterol. 2011;106(5):835–842. doi:10.1038/ajg.2011.30
11. Nojkov B, Baker J, Menees S, et al. Is dyssynergic defecation an unrecognized cause of chronic constipation in patients using opioids? Am J Gastroenterol. 2019;114(11):1772–1777. doi:10.14309/ajg.0000000000000413
12. Rachinger-Adam B, Conzen P, Azad SC. Pharmacology of peripheral opioid receptors. Curr Opin Anaesthesiol. 2011;24(4):408–413. doi:10.1097/ACO.0b013e32834873e5
13. Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26(10):1386–1395. doi:10.1111/nmo.12417
14. Coyne KS, Margolis MK, Yeomans K, et al. Opioid-induced constipation among patients with chronic noncancer pain in the United States, Canada, Germany, and the United Kingdom: laxative use, response, and symptom burden over time. Pain Med. 2015;16(8):1551–1565. doi:10.1111/pme.12724
15. Panchal SJ, Muller-Schwefe P, Wurzelmann JI. Opioid-induced bowel dysfunction: prevalence, pathophysiology and burden. Int J Clin Pract. 2007;61(7):1181–1187. doi:10.1111/j.1742-1241.2007.01415.x
16. Argoff CE. Opioid-induced constipation: a review of health-related quality of life, patient burden, practical clinical considerations, and the impact of peripherally acting mu-opioid receptor antagonists. Clin J Pain. 2020;36(9):716–722. doi:10.1097/AJP.0000000000000852
17. Varrassi G, Banerji V, Gianni W, Marinangeli F, Pinto C. Impact and consequences of opioid-induced constipation: a survey of patients. Pain Ther. 2021;10(2):1139–1153. doi:10.1007/s40122-021-00271-y
18. Farmer AD, Drewes AM, Chiarioni G, et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United European Gastroenterol J. 2019;7(1):7–20. doi:10.1177/2050640618818305
19. Chey WD, Webster L, Sostek M, Lappalainen J, Barker PN, Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014;370(25):2387–2396. doi:10.1056/NEJMoa1310246
20. Chey WR, Bortey E, Almenoff J. Rapid onset of time to first Spontaneous Bowel Movement (SBM) and predictable efficacy of Naloxegol.
21. Tack J, Lappalainen J, Diva U, Tummala R, Sostek M. Efficacy and safety of naloxegol in patients with opioid-induced constipation and laxative-inadequate response. United European Gastroenterol J. 2015;3(5):471–480. doi:10.1177/2050640615604543
22. CDC. 71 CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. CDC; 2022:1–95.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.