Back to Journals » Nature and Science of Sleep » Volume 14
Efficacy and Safety of Lower-Sodium Oxybate in an Open-Label Titration Period of a Phase 3 Clinical Study in Adults with Idiopathic Hypersomnia
Authors Thorpy MJ, Arnulf I, Foldvary-Schaefer N, Morse AM , Šonka K , Chandler P, Hickey L , Chen A, Black J, Sterkel A, Chen D, Bogan RK , Dauvilliers Y
Received 8 April 2022
Accepted for publication 9 October 2022
Published 26 October 2022 Volume 2022:14 Pages 1901—1917
DOI https://doi.org/10.2147/NSS.S369122
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Video abstract presented by Michael J Thorpy.
Views: 366
Michael J Thorpy,1 Isabelle Arnulf,2 Nancy Foldvary-Schaefer,3 Anne Marie Morse,4 Karel Šonka,5 Patricia Chandler,6 Luke Hickey,7 Abby Chen,6 Jed Black,6,8 Amanda Sterkel,6 Dan Chen,9 Richard K Bogan,10 Yves Dauvilliers11,12
1Albert Einstein College of Medicine, Bronx, NY, USA; 2Sleep Disorder Unit, Pitié-Salpêtrière Hospital and Sorbonne University, Paris, France; 3Cleveland Clinic Sleep Disorders Center, Department of Neurology, Lerner College of Medicine, Cleveland, OH, USA; 4Janet Weis Children’s Hospital, Geisinger, Danville, PA, USA; 5Department of Neurology, First Faculty of Medicine, Charles University and General University Hospital, Prague, Czech Republic; 6Jazz Pharmaceuticals, Palo Alto, CA, USA; 7Jazz Pharmaceuticals, Philadelphia, PA, USA; 8Stanford University Center for Sleep Sciences and Medicine, Palo Alto, CA, USA; 9Formerly Jazz Pharmaceuticals, Palo Alto, CA, USA; 10University of South Carolina School of Medicine, Columbia, SC, USA; 11Sleep and Wake Disorders Centre, Department of Neurology, Gui de Chauliac Hospital, Montpellier, France; 12University of Montpellier, INSERM Institute Neuroscience Montpellier (INM), Montpellier, France
Correspondence: Michael J Thorpy, Albert Einstein College of Medicine, 1300 Morris Park Avenue, Bronx, NY, 10461, USA, Tel +1 718 920-4841, Fax +1 718 798-4352, Email [email protected]
Purpose: To report the efficacy and safety of lower-sodium oxybate (LXB; Xywav®) during the open-label titration and optimization period (OLT) and stable-dose period (SDP) in a clinical study for the treatment of idiopathic hypersomnia.
Patients and Methods: Data were collected during treatment titration and optimization in a phase 3 randomized withdrawal trial in adults (18– 75 years of age) with idiopathic hypersomnia who took LXB treatment (once, twice, or thrice nightly, administered orally) in the OLT (10– 14 weeks), followed by the 2-week, open-label SDP. Endpoints included the Epworth Sleepiness Scale (ESS), Idiopathic Hypersomnia Severity Scale (IHSS), Patient Global Impression of Change, Clinical Global Impression of Change, Functional Outcomes of Sleep Questionnaire (FOSQ)-10, and Work Productivity and Activity Impairment Questionnaire: Specific Health Problem (WPAI:SHP).
Results: The safety population included 154 participants; the modified intent-to-treat population comprised 115 participants. During open-label treatment, mean (SD) ESS scores improved (decreased) from 15.7 (3.8) at baseline to 6.1 (4.0) at end of SDP, and IHSS scores improved (decreased) from 31.6 (8.3) to 15.3 (8.5). Improvements were also observed during OLT in each individual IHSS item and in FOSQ-10 and WPAI:SHP scores. Thirty-five (22.7%) participants discontinued during OLT and SDP, 22 (14.3%) due to treatment-emergent adverse events (TEAEs) during OLT and SDP. The most frequent TEAEs in the first 4 weeks were nausea, headache, dizziness, and dry mouth; TEAE incidence decreased throughout OLT and SDP (weeks 1– 4, n = 87 [56.5%]; weeks 13– 16, n = 39 [31.7%]).
Conclusion: During open-label treatment with LXB, participants showed clinically meaningful improvements in idiopathic hypersomnia symptoms and in quality of life and functional measures. TEAE incidence declined over LXB titration and optimization.
Keywords: excessive daytime sleepiness, hypersomnolence, quality of life, pharmacotherapy
Plain Language Summary
Idiopathic hypersomnia is a sleep disorder that causes daytime sleepiness. Many patients also have difficulty awakening, long sleep time at night, long and unrefreshing naps, and problems thinking clearly. Lower-sodium oxybate is a medicine used to treat symptoms of idiopathic hypersomnia.
This research was done to understand how lower-sodium oxybate affected idiopathic hypersomnia symptoms in participants beginning treatment in the first 2 parts of a clinical trial (NCT03533114; EUDRACT: 2018-001311-79). First, participants adjusted to lower-sodium oxybate until they found a best dose (for 10–14 weeks). Next, they took the same best dose for 2 weeks (stable-dose period). Participants knew they were taking lower-sodium oxybate during this time. Participants’ idiopathic hypersomnia symptoms, quality of life, functioning, working ability, sleep time, and side effects were measured.
Lower-sodium oxybate improved their sleepiness and other symptoms of idiopathic hypersomnia. Participants reported that their quality of life improved and they were better able to function and work. About 20% of participants left the trial early, and in total, 14% left because of side effects. The most common side effects in the first 4 weeks were nausea, headache, dizziness, and dry mouth. Side effects happened less often as the trial went on.
These results show that lower-sodium oxybate improved symptoms of idiopathic hypersomnia and improved participants’ quality of life, day-to-day functioning, and ability to work. The results also show that side effects decreased with continued treatment.
Introduction
Idiopathic hypersomnia is a debilitating neurologic sleep disorder characterized by chronic excessive daytime sleepiness (EDS), with many patients also experiencing severe sleep inertia (prolonged difficulty waking, often with frequent reentries into sleep, confusion, and irritability), as well as prolonged nighttime sleep, cognitive impairment, and long and unrefreshing naps.1–3 The cardinal symptom, EDS, is characterized by the inability to stay awake and alert during the day, resulting in the irrepressible need to sleep or unplanned lapses into sleep or drowsiness.3–5 Despite requiring objective evidence of hypersomnolence for diagnosing idiopathic hypersomnia,3 the diagnosis remains difficult because other causes of hypersomnolence must be ruled out.4,6 The burden of idiopathic hypersomnia symptoms leads to poor health-related quality of life (QoL) and impaired functioning across multiple domains, including self-care, employment, and driving.7–10 In particular, patients with idiopathic hypersomnia have reported that cognitive difficulty is the most bothersome functional impairment caused by idiopathic hypersomnia and the most important to improve.8
Calcium, magnesium, potassium, and sodium oxybates (lower-sodium oxybate [LXB]; Xywav®) is an oxybate medication with the same active moiety at the same concentration as sodium oxybate (SXB) and a unique composition of cations resulting in 92% less sodium.11 LXB was approved in the US in 2021 for the treatment of idiopathic hypersomnia in adults, following its approval in 2020 for the treatment of cataplexy or EDS in patients ≥7 years of age with narcolepsy.12 In the treatment of narcolepsy, LXB was deemed by the US Food and Drug Administration (FDA) to be clinically superior to SXB, by means of greater safety, given its significant reduction in chronic sodium burden compared with SXB and the associated implications for cardiovascular morbidity.13 The FDA approval for LXB treatment of idiopathic hypersomnia was granted based on the results of a double-blind randomized withdrawal study; the primary results of this study have been published.14 LXB had a clinically meaningful impact on EDS and overall idiopathic hypersomnia symptom severity,14 as evidenced by worsening of Epworth Sleepiness Scale (ESS) and Idiopathic Hypersomnia Severity Scale (IHSS) scores during randomization to placebo when compared with the maintenance of effect for those randomized to LXB. The safety profile of LXB in idiopathic hypersomnia was similar to that observed in narcolepsy.11 The primary objective of the present analysis was to report data evaluating the efficacy and safety of LXB treatment during the open-label titration and optimization period (OLT) and stable-dose period (SDP) of this study. These additional efficacy and safety data from the titration and optimization period may guide clinicians and their patients in anticipating and evaluating treatment success. It can also provide a better understanding of baseline disease severity, the impact of concurrent treatments and the long sleep time (LST) phenotype, and the effect of LXB on various symptoms of idiopathic hypersomnia measured by the novel IHSS instrument.15,16
Methods
Study Design
The study (NCT03533114; EUDRACT: 2018-001311-79) included a screening period of ≤30 days, an OLT (10–14 weeks), an SDP (2 weeks), a double-blind randomized withdrawal period (DBRWP; 2 weeks), an open-label safety extension period (OLE; 24 weeks), and a safety follow-up period (2 weeks). Enrollment began November 27, 2018 and ended March 6, 2020; these analyses used final data, after all participants had completed the OLE. The current analysis includes open-label efficacy data during the OLT and SDP only; as noted, results of the main safety and efficacy analyses from the DBRWP have been published elsewhere,14 and results of the OLE will be reported separately.
Participants
Eligible participants were 18–75 years of age with a primary diagnosis of idiopathic hypersomnia according to International Classification of Sleep Disorders, 2nd or 3rd edition (ICSD-2 or ICSD-3) criteria3,17 and an average nocturnal total sleep time ≥7 hours. The presence of the LST phenotype was identified clinically by investigators according to ICSD-2 or ICSD-3 criteria. Participants were treatment naive or taking medications to manage idiopathic hypersomnia symptoms, including SXB and/or alerting agents (traditional stimulants or wake-promoting agents); all participants were required to have an ESS score ≥11 at screening and baseline, except for participants taking SXB at study entry, who were instead required to have had prior clinical improvement of EDS with SXB treatment per the investigator’s clinical judgment. Participants treated with alerting agents were required to have been on a stable dose and regimen for at least 2 months prior to screening, and to take the same dose during the study.
Key exclusion criteria were a hypersomnolence disorder due to another medical, behavioral, or physical disorder or evidence of untreated or inadequately treated sleep-disordered breathing. Participants were also ineligible if their job required shiftwork or they had a usual bedtime later than 1:00
Procedures
Participants who were taking a stable dose of SXB at study entry entered OLT and switched from SXB to the same dosing regimen of LXB. Participants who were not taking SXB at study entry entered OLT and initiated LXB treatment on a once-nightly or twice-nightly dosing regimen, at the discretion of the investigator. The regimen (ie, once nightly, twice nightly) and dose amount could be changed during the OLT to optimize efficacy and tolerability. The protocol included guidance to investigators that participants should be considered for once-nightly dosing if they reported difficulty awakening at night to take the second dose, and that participants should be considered for twice-nightly dosing if they reported disrupted nighttime sleep or difficulty with sleep maintenance. Additionally, investigators could change the regimen to thrice-nightly dosing after initiation at once- or twice-nightly dosing. Maximum starting doses were 3 g/night for participants taking LXB once nightly and 4.5 g/night for participants taking LXB twice nightly. Doses could be titrated in increments of 1.5 g/night per week, up to a maximum nightly dose of 6 g for once-nightly dosing, or 9 g for twice-nightly or thrice-nightly dosing. Individual doses up to 6 g were also allowed as part of a twice- or thrice-nightly regimen as long as the maximum nightly total dose was 9 g/night. For twice- and thrice-nightly regimens, doses were divided equally or unequally, with the first dose administered at bedtime and the second and third (when applicable) doses administered at 2.5- to 4-hour intervals from each other.
During SDP, participants remained on their individually optimized stable LXB dose for 2 weeks. Participants who met randomization criteria were then randomized 1:1 to take LXB (at the same dose and regimen as in SDP) or placebo (at a volume and regimen equivalent to the stable LXB dose) as double-blind treatment for 2 weeks during DBRWP. Upon completing DBRWP, participants entered the 24-week OLE period.
This article reports efficacy and safety results from OLT and SDP. Scheduled clinic visits relevant to the present analysis occurred at screening; day 1 of OLT (baseline); OLT weeks 1, 4, and 8; end of OLT/start of SDP; and end of SDP. Adverse events are reported through end of SDP; serious adverse events (SAEs) and discontinuations due to TEAEs are reported for the entire study duration.
Assessments and Outcomes
The ESS and IHSS were assessed at every clinic visit during those periods. The ESS is an 8-item scale that assesses daytime sleepiness, with responses ranging from 0 to 3; total scores range from 0 to 24, with values >10 indicating pathologic sleepiness.18 The IHSS is a recently developed, 14-item self-report questionnaire that evaluates the severity of symptoms of idiopathic hypersomnia and their functional consequences; total scores range from 0 to 50, with a value of 22 distinguishing individuals with untreated idiopathic hypersomnia from healthy controls.16,19 The Patient Global Impression of Change (PGIc) and Clinical Global Impression of Change (CGIc) were assessed at every clinic visit starting at OLT week 1. PGIc and CGIc ratings are relative to baseline for all clinic visits; the proportion of participants reporting symptoms as improved (minimally, much, or very much) was summarized. Functional Outcomes of Sleep Questionnaire (FOSQ)-10 was assessed at the baseline and end of SDP visits (total scores range from 5 to 20; scores ≥17.8 indicate normal functioning, and scores <17.8 indicate impaired functioning).20 The Work Productivity and Activity Impairment Questionnaire: Specific Health Problem (WPAI:SHP), a self-reported, 6-item questionnaire that measures percentage (0% to 100%) of work time missed and activity impairment due to idiopathic hypersomnia (in this study) over the last week, was assessed at the baseline and end of SDP visits.
Statistical Analyses
The modified intent-to-treat (mITT) population included all participants who were randomized to LXB or placebo, took at least 1 dose of study medication during DBRWP, and had at least 1 set of post-randomization assessments for ESS or IHSS, or PGIc at the end of DBRWP. The safety population included all participants who took at least 1 dose of study medication. Descriptive analyses were conducted post hoc for efficacy endpoints from baseline through end of SDP in the mITT population (and safety population, for individual IHSS item scores). Selected efficacy endpoints were subsequently analyzed post hoc in participant subgroups defined by treatment at study entry, idiopathic hypersomnia phenotype (with and without LST), and LXB dosing regimen (maintained on once nightly, maintained on twice nightly, or switched between once and twice nightly). Differences in ESS and IHSS scores were assessed between dosing regimens at each timepoint using a linear mixed model with ESS or IHSS as response variables, with baseline ESS or IHSS, dose regimen group, and interaction between visit and dose regimen as fixed effects, and visit as a random effect; participants who were on twice-nightly dosing or switched between regimens were compared against those who remained on once-nightly dosing. The number of LXB dose adjustments required to reach a stable dose and time to stable dose (days) during OLT were examined in the population who completed the SDP and entered DBRWP, and in subgroups stratified by baseline medication (SXB with or without alerting agents, alerting agents only, and treatment naive). The overall incidence of treatment-emergent adverse events (TEAEs) and TEAEs in ≥5% of participants were examined in 4-week periods during the OLT and SDP (ie, weeks 1–4, 5–8, 9–12, and 13–16). SAEs and study discontinuations due to TEAEs, with information on timing of occurrence, are reported for the entire study period.
Results
Study Population
The safety population comprised 154 participants who were enrolled and treated; 115 participants were included in the mITT population (LXB, n = 56; placebo, n = 59). Participants in the safety population had a mean (SD) age of 40.3 (13.7) years, 68.2% were female, and 20.1% had idiopathic hypersomnia with LST (Table 1). At study entry, 6 participants were taking SXB (SXB only, n = 2; SXB + alerting agent, n = 4), 82 were taking alerting agents only, and 66 were treatment naive. Twenty-nine (18.8%) participants discontinued during OLT, 2 (1.3%) completed the OLT but discontinued before the SDP, and 4 (2.6%) discontinued during SDP. Reasons for discontinuation were adverse events (n = 22), lack of efficacy (n = 6), withdrawal by the participant (n = 4), protocol deviations (n = 1), loss to follow-up (n = 1), and noncompliance with the study medication (n = 1). An additional 23 (14.9%) participants discontinued after completing the SDP; 3 participants discontinued after SDP but before DBRWP. In the DBRWP, 1 participant discontinued 2 days after randomization due to a TEAE of limb injury (stubbed toe) and was not included in the mITT population. Additional demographics and baseline characteristics, as well as detailed disposition of the study population, are reported in the primary paper.14
 |
Table 1 Demographic and Baseline Disease Characteristics |
Dosing Regimen and Titration
Among the participants who completed the SDP and entered the DBRWP (n = 116), the median number of LXB dose adjustments required by participants differed slightly by treatment at study entry (Table 2). Participants who were taking alerting agents only at baseline required a median (first quartile [Q1], third quartile [Q3]) of 4 (3, 6) LXB dose adjustments during OLT. Participants who were treatment naive at baseline required a median (Q1, Q3) of 3 (2, 5) dose adjustments during OLT. Four of the 6 participants who entered the study taking SXB (with or without alerting agents) required no LXB dose adjustments (median [Q1, Q3] number of LXB adjustments = 0 [0, 2]).
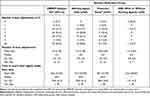 |
Table 2 Number of LXB Dose Adjustments and Time to Reach Total Nightly Stable Dose of LXB During OLT |
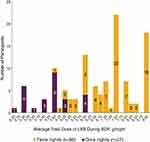
Within the protocol-specified maximum dose adjustment rate of 1.5 g/week, the median (range) number of days required to reach a stable dose was 48.5 (1–97) overall, 46 (9–92) in participants taking alerting agents only at baseline, and 56 (1–90) in participants who were treatment naive; among participants taking SXB (with or without alerting agents) at baseline, the median (range) number of days required to reach a stable dose was 1 (1–97). During SDP, the total nightly dose of LXB varied widely, with higher total doses in the twice-nightly group (Figure 1). Median total nightly dose of LXB was 7 g/night (range, 2.5–9.0) for all participants, 4.5 g/night (range, 2.5−6.0) for participants taking once-nightly LXB, and 7.5 g/night (range, 4.5−9.0) for participants taking twice-nightly LXB. Of participants who were initially on a once-nightly regimen, 21/40 (52.5%) stayed on their original regimen and 19/40 (47.5%) switched at least once during OLT. Of participants who were initially on a twice-nightly regimen, 93/114 (81.6%) stayed on their original regimen and 21/114 (18.4%) switched at least once. Few participants (10/154 [6.5%]) switched regimens more than once. Dosing during SDP was once, twice, and thrice nightly in 29 (23.6%), 93 (75.6%), and 1 (0.8%) of the 123 participants, respectively. As only 1 participant entered SDP on thrice-nightly dosing, this participant was excluded from further analyses by dosing regimen.
Efficacy
As reported previously,14 ESS scores in the mITT population declined (improved) with open-label LXB treatment during OLT and SDP. ESS scores followed a similar pattern between participants who were treatment naive at study entry and those who entered taking alerting agents, whereas participants who entered the study taking SXB (with or without alerting agents) maintained mean ESS scores in the normal range (≤10)18 during titration and stable dosing with LXB (Figure 2A). Overall, mean (SD) ESS scores at baseline (OLT day 1), OLT week 1, OLT week 4, OLT week 8, end of OLT, and end of SDP were 15.7 (3.8), 13.5 (4.7), 9.8 (4.5), 7.9 (4.6), 6.7 (4.4), and 6.1 (4.0), respectively.
As reported previously,14 mean (SD) IHSS total scores in the mITT population declined (improved) with open-label LXB treatment during OLT and SDP. IHSS scores followed a similar pattern between participants who were treatment naive at study entry and those who entered taking alerting agents, whereas participants who entered the study taking SXB (with or without alerting agents) maintained mean IHSS scores in the normal range (<22)19 during titration and stable dosing with LXB (Figure 2B). Overall, mean (SD) IHSS scores at baseline (OLT day 1), OLT week 1, OLT week 4, OLT week 8, end of OLT, and end of SDP were 31.6 (8.3), 27.3 (9.1), 20.9 (8.9), 18.8 (9.2), 16.9 (8.8), and 15.3 (8.5), respectively.
Idiopathic hypersomnia symptom severity and impairment varied across domains at baseline, as assessed by individual IHSS items (Figure 3). In particular, severe impairment was seen at baseline on items 2, 10, and 11. At baseline, 76.0% of participants reported often or always having a feeling of not having slept enough (item 2), 87.7% of participants reported that hypersomnolence had a significant, or very significant, impact on general health (item 10), and 74.7% of participants reported that hypersomnolence had a significant, or very significant, impact on intellectual functioning (item 11 in Figure 3). During open-label LXB treatment, scores decreased on all individual items through OLT and SDP, and this reduction was generally consistent with overall IHSS total scores. At the end of SDP, 70.7% of participants reported never or sometimes having a feeling of not having slept enough, 56.1% of participants reported that hypersomnolence was no problem in terms of, or had a minor impact on, general health, and 54.5% reported that hypersomnolence was no problem in terms of, or had a minor impact on, intellectual functioning. Of note, on item 14 (hypersomnolence is a problem for driving), 8/154 (5.2%) and 10/123 (8.1%) participants indicated that they do not drive at baseline (OLT day 1) and end of SDP, respectively, and were categorized as “no problem” for the analysis, per the IHSS protocol.19
On the PGIc, the proportion of participants in the mITT population rating their idiopathic hypersomnia symptoms as improved (minimally, much, or very much) relative to baseline (OLT day 1) was 52.6%, 87.0%, 94.6%, 94.7%, and 95.7% at OLT week 1, OLT week 4, OLT week 8, end of OLT, and end of SDP, respectively (Figure 4). The percentage of participants rating their symptoms as very much improved as compared with minimally improved also increased substantially at the end of SDP compared with OLT week 1. The pattern of improvement observed on the CGIc was similar to that observed on the PGIc. On the CGIc, the proportion of participants (mITT population) whose idiopathic hypersomnia symptoms were rated by clinicians as improved (minimally, much, or very much) relative to baseline (OLT day 1) was 55.8%, 86.8%, 93.8%, 95.7%, and 94.8% at OLT week 1, OLT week 4, OLT week 8, end of OLT, and end of SDP, respectively.
Measures of QoL and functional impairment also showed improvement with LXB treatment (Figure 5). Mean (SD) FOSQ-10 scores increased (improved) from baseline (11.9 [3.4]) to end of SDP (16.9 [2.8]). WPAI:SHP percent work time missed (absenteeism), percent impairment while working (presenteeism), percent overall work impairment (absenteeism + presenteeism), and percent activity impairment due to idiopathic hypersomnia all decreased (improved) from baseline to end of SDP. Mean (SD) change from baseline in absenteeism, presenteeism, absenteeism + presenteeism, and activity impairment was −4.4% (10.5), −33.1% (24.7), −34.1% (26.0), and −38.4% (25.5), respectively.
Subgroup Analyses by Dosing Regimen and in Participants with and without LST
The patterns of efficacy during OLT and SDP were similar among subgroups with and without LST for ESS and IHSS scores (Figure 6), as well as for the PGIc, and consistent with efficacy in the overall population. Mirroring improvements seen on the PGIc, the percentage of participants rated by investigators on the CGIc as improved increased from 41.7% and 59.6% at OLT week 1 to 91.7% and 95.6% at end of SDP, in participants with or without LST, respectively. Improvements on the FOSQ-10 and WPAI:SHP were also consistent between LST subgroups and with the overall population (Table 3). The patterns of efficacy (ESS and IHSS) during OLT and SDP were also similar among subgroups defined by dosing regimen and consistent with efficacy in the overall population (nominal P>0.05 across subgroups at all timepoints).
 |
Table 3 FOSQ-10 and WPAI:SHP Scores During OLT and SDP in Participants with and without LSTa |
Treatment-Emergent Adverse Events
The incidence of TEAEs decreased over the duration of the OLT and SDP (weeks 1–4, n = 87 [56.5%]; weeks 5–8, n = 65 [46.1%]; weeks 9–12, n = 47 [35.3%]; weeks 13–16, n = 39 [31.7%]). Nausea, headache, dizziness, and dry mouth were the most common TEAEs, occurring in ≥5% of participants in the safety population during at least 1 of the 4-week study periods (Table 4).
 |
Table 4 TEAEs During the First 16 Weeks of LXB Exposure in OLT and SDPa |
Serious Adverse Events and Study Discontinuations Due to TEAEs
As previously reported14 and briefly described here, in all study periods, excluding placebo data, 9 SAEs occurred in 4 participants (2.6%): 4 during OLT, 1 during safety follow-up, and 4 during OLE. This included non-cardiac chest pain (n = 1; 1 event), rhabdomyolysis (n = 1; 1 event), syncope (n = 1; 1 event), and nephrolithiasis and pyelonephritis (n = 1; 6 events); none of the SAEs were deemed related to the study medication. Twenty-six participants experienced TEAEs leading to discontinuation (16.9%; excluding placebo data) in all study periods. Most discontinuations due to TEAEs occurred during the OLT (OLT, n = 20 [weeks 1–4, n = 9; weeks 5–8, n = 5; weeks 9–12, n = 6]; SDP, n = 2 [weeks 9–12, n = 1; week 14 onwards, n = 1]; DBRWP, n = 1; OLE, n = 3). During DBRWP, 1 participant randomized to placebo discontinued due to a TEAE of insomnia. TEAEs leading to discontinuation in more than 1 participant were anxiety (n = 4), insomnia (n = 3), nausea (n = 3), and confusion (n = 2). Psychiatric disorders were the most prominent TEAEs leading to discontinuation (n = 13).
Discussion
Double-blind results are important for describing the effects of treatment compared with placebo. However, because this study had a randomized withdrawal design, important treatment effects were seen in the open-label dose titration and treatment optimization period, which is the focus of this separate paper. The current open-label results show strong improvement not only in ESS, IHSS, and PGIc, but also in HRQoL endpoints (ie, the FOSQ-10 and WPAI:SHP). Furthermore, the novel data included on baseline values and treatment effects for individual IHSS items aid understanding about the symptoms and functional impact of idiopathic hypersomnia, as well as the impact of treatment. In the OLT and SDP sections of this double-blind randomized withdrawal study of LXB in adults with idiopathic hypersomnia, improvements were seen within the first 4 weeks across the ESS, IHSS, PGIc, and CGIc endpoints, and these improvements were maintained through the SDP. At week 1, the mean ESS and IHSS scores decreased from baseline by 2.3 and 4.4 points, respectively, which is consistent with the established thresholds for a minimum within-person change (≥2 points for ESS [based on narcolepsy] and 4 points for IHSS [IH specific]).16,21 Improvements in scores of the QoL measures FOSQ-10 and WPAI:SHP were also observed at the end of stable-dose treatment. Participants reached a stable dose of LXB in a median of 48.5 days; the median dose was 7 g/night, and the majority of participants were stable on a twice-nightly dosing regimen. Subgroup analyses confirmed that the beneficial effects of LXB treatment were independent of dosing regimen or the presence of long sleep time. The incidence of TEAEs with LXB treatment decreased over the duration of the study.
The median time to reach a stable dose of LXB and number of dose adjustments required were generally similar in participants who were treatment naive and participants who entered the study taking alerting agents only for idiopathic hypersomnia. Participants who entered the study taking SXB reached a stable dose quickly and with few dose adjustments; 4 out of 6 of them required no dose adjustments. Investigators could initiate participants on a once- or twice-nightly regimen at their discretion and were free to change the regimen throughout the titration period. Majorities, however, stayed on their initial regimen (74.0%) during OLT, and were stable on twice-nightly dosing (75.6%), with a minority stable on once-nightly dosing (23.6%); thus, extensive switching among LXB regimens in the present study was uncommon and therefore unlikely to have led to longer titration times. A spectrum of optimized doses was seen during SDP, suggesting that individualized titration was important for clinicians and their patients. The efficacy seen in participants taking once-nightly LXB is noteworthy, as participants were able to receive the benefits of LXB therapy with a dosing regimen that was optimized based on their clinical response. The median time of 48.5 days required to reach a stable dose of LXB among participants with idiopathic hypersomnia was longer than the median of 29 days seen in all participants in the clinical study of LXB for participants with narcolepsy.11 This could be because clinicians took a cautious approach when titrating LXB in participants with idiopathic hypersomnia. Even physicians who may have experience using SXB or LXB in patients with narcolepsy likely had less familiarity with treatments for idiopathic hypersomnia, as there were no FDA-approved therapies for idiopathic hypersomnia at the time of the study.22,23 Finally, it has been demonstrated previously that while many participants with narcolepsy showed a clinically meaningful response to SXB within 2 months, on average, a period of over 3 months is required to reach the maximum therapeutic response to SXB in terms of EDS.24
Both ESS and IHSS total scores decreased with open-label LXB treatment during OLT and SDP, whether participants entered the study taking alerting agents or were treatment naive (the 6 participants who entered taking SXB maintained scores in the published range for healthy controls),18,19 and improvements seen on the IHSS mirrored those observed on the FOSQ-10 and WPAI:SHP. This agreement between instruments is consistent with a previous study showing a correlation between IHSS and ESS scores in untreated and treated participants with idiopathic hypersomnia.19 The PGIc and CGIc also showed high agreement, indicating that both participants and clinicians similarly perceived participants’ idiopathic hypersomnia symptom severity improvement over time during OLT and SDP. Consistency between the IHSS and the PGIc and CGIc (which measure global changes in overall condition) indicates that responses on the IHSS assess multiple symptoms and symptom impacts. Mean ESS scores were within the normal range at the end of SDP, when participants were taking an optimized dose of LXB. The large magnitude of decrease in ESS scores with LXB treatment in this idiopathic hypersomnia population was notable, and compared favorably with the wake-promoting agent modafinil. Of 2 prior randomized, double-blind, placebo-controlled studies of modafinil for idiopathic hypersomnia, 1 reported a median reduction in ESS scores of 6.0, while the other reported a least squares mean reduction in Japanese ESS scores of 7.1;25,26 the median and mean reductions in ESS score at the end of SDP in the present study were 10.0 and 9.7, respectively.
Symptom severity and impairment, as measured by individual IHSS items, varied at baseline, as previously reported in idiopathic hypersomnia.16 Despite this heterogeneity, IHSS responses indicated a consistent improvement across all items, indicative of a beneficial effect of LXB treatment during OLT and SDP across all symptoms and functional domains. In particular, severe impairment was seen at baseline on items 2, 10, and 11, relating to feelings of not having slept enough, and the impact of hypersomnolence on general health and intellectual functioning. At the end of SDP, scores on these 3 items reflected a strong improvement. This may be particularly important in terms of intellectual functioning, given that this last IHSS item corresponds to the domain of impairment reported as most bothersome, and important to treat, in another study of QoL in participants with idiopathic hypersomnia.8
In addition to changes in symptom severity, improvements were seen on QoL measures. Changes on the FOSQ-10 and WPAI:SHP are consistent with those reported in the primary efficacy analysis,14 and reflect a reduced impact of idiopathic hypersomnia symptoms on daily activities and work productivity. Absenteeism, as assessed by the WPAI:SHP in the current analyses, was far higher at baseline than has been previously reported for the general population (7.1% compared with 1.3%).27 Presenteeism also was high, indicating that participants were physically present at work but productivity was low. At the end of SDP, absenteeism was reduced to 1.9% and presenteeism was reduced by over 30%, reflecting large increases in the ability of participants to be at work and perform effectively. Altogether, these improvements may have afforded participants more time to participate in daily activities.
Further subgroup analyses found that the beneficial effects of LXB treatment were observed in participants both with and without long sleep time. The prevalence of prolonged sleep (defined as ≥11 hours of ad libitum sleep during extended monitoring) may be underestimated and difficult to diagnose, as most sleep centers cannot perform extended polysomnography (>24 hours), and patients’ responsibilities may prevent them from sleeping for the required duration.3,5,28–30 Furthermore, government and private payers may not provide insurance reimbursement for long sleep protocols, especially in the US.31 Accordingly, although the present study reports long sleep time in approximately 20% of participants, 2 recent studies reported long sleep in approximately 49% and 69% of participants.32,33 This is important given the recent suggestions that idiopathic hypersomnia may be a heterogeneous disorder with important phenotypic differences between patients who have an increased need for sleep and those who do not.30,34,35 Despite this heterogeneity, in the current study, improvements were similar in both timing and magnitude between participants with or without LST across all outcomes measured, as previously reported with SXB in a small case series.36
The safety profile of LXB in idiopathic hypersomnia was generally consistent with its profile in narcolepsy11 and the known safety profile of SXB.37–41 Twenty-three percent of all participants discontinued the trial during the open-label treatment periods (OLT and SDP), 14% due to TEAEs. These rates of discontinuation are similar to those in the same periods of a phase 3 study of LXB in a narcolepsy population, where 32% of participants discontinued overall and 10% discontinued due to TEAEs. In the present study, psychiatric disorders, such as anxiety and insomnia, were the most prominent type of TEAE leading to discontinuation. Nausea, headache, and dizziness were the most common TEAEs in the first 4 weeks. The incidence of TEAEs occurred mainly in the early phase of initiation and titration and declined over time, similar to what has been reported with SXB and LXB in narcolepsy.42,43
Strengths of this study include the use of multiple outcome measures over time, which allowed for the robust assessment of overall idiopathic hypersomnia symptoms and impact on function and QoL in these open-label treatment periods. Also, the design of this study included individually optimized LXB dosing, which may more closely reflect real-world practice than forced titration or fixed dosing. Limitations of this study to be acknowledged are, first, that the requirement for participants entering the study taking SXB to have shown documented clinical improvement of EDS with SXB treatment may have introduced selection bias; however, only 6 participants were taking SXB at study entry, so such a bias would have minimal impact. Second, due to the open-label nature of the titration and stable-dosing periods, both participants and clinicians were aware that participants were receiving an active study drug, which could have biased their responses on subjective measures of symptoms severity, QoL, and tolerability during the OLT and SDP.44 LST was determined by the investigator, and this study did not include polysomnography or objective measures of LST. Furthermore, it is unclear whether titration of LXB could be affected by LST phenotype.
Based on the primary efficacy and safety analysis performed as part of this clinical study, LXB is now the first FDA-approved treatment for idiopathic hypersomnia in adults.12,14 In clinical practice prior to the approval of LXB for the treatment of idiopathic hypersomnia in the United States, patients with idiopathic hypersomnia may have taken more than 1 off-label medication to manage their idiopathic hypersomnia symptoms,45 or cycled through multiple off-label treatments sequentially due to lack of efficacy.22,23 In the present study, similar efficacy was seen between participants entering and maintaining concomitant treatment with alerting agents (traditional stimulants or wake-promoting agents) and participants who were treatment naive, indicating that LXB may be useful as first-line therapy as a single agent, or in combination with alerting agents.
Conclusion
In conclusion, in this study of adults with idiopathic hypersomnia, open-label administration of LXB led to clinically meaningful improvements in idiopathic hypersomnia symptoms and QoL measures, observed from as early as week 1. These changes were maintained or continued to improve through the duration of the titration and optimization period and during the 2 weeks of stable dosing. The mean ESS scores were within the normal range at the end of stable dosing, when participants were taking an optimized dose of LXB. Nearly 25% of patients only required once-nightly dosing. Participants who entered on SXB maintained efficacy after switching to LXB. The safety profile of LXB in the population of adults with idiopathic hypersomnia was similar to its profile in the narcolepsy study population, as well as to the profile of SXB. TEAE incidence declined over time as participants titrated to their stable dose.
Abbreviations
CGIc, Clinical Global Impression of Change; DBRWP, double-blind randomized withdrawal period; EDS, excessive daytime sleepiness; ESS, Epworth Sleepiness Scale; FDA, US Food and Drug Administration; FOSQ-10, Functional Outcomes of Sleep Questionnaire-10; ICSD-2, International Classification of Sleep Disorders, 2nd edition; ICSD-3 International Classification of Sleep Disorders, 3rd edition; IHSS, Idiopathic Hypersomnia Severity Scale; LST, long sleep time; LXB, lower-sodium oxybate; mITT, modified intent-to-treat; OLE, open-label safety extension period; OLT, open-label titration and optimization period; PGIc, Patient Global Impression of Change; Q1, first quartile; Q3, third quartile; QoL, quality of life; SAE, serious adverse event; SDP, stable-dose period; SXB, sodium oxybate; TEAE, treatment-emergent adverse event; WPAI:SHP, Work Productivity and Activity Impairment Questionnaire: Specific Health Problem.
Data Sharing Statement
All relevant data are provided within the manuscript and supporting files. Jazz has established a process to review requests from qualified external researchers for data from Jazz-sponsored clinical trials in a responsible manner that includes protecting patient privacy, assurance of data security and integrity, and furthering scientific and medical innovation. Additional details on Jazz Pharmaceuticals data sharing criteria and process for requesting access can be found at: https://www.jazzpharma.com/science/clinical-trial-data-sharing/.
Acknowledgments
The authors would like to thank the participants, study investigators, and study staff for their contributions to this research. This study was sponsored by Jazz Pharmaceuticals. Under the direction of the authors, Sean Anderson, PhD and Karyn Liu, PhD of Peloton Advantage, LLC, an OPEN Health company, provided medical writing and editorial support, which was funded by Jazz Pharmaceuticals.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; have drafted or written, or substantially revised or critically reviewed the article; have agreed on the journal to which the article will be submitted; reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage; and agree to take responsibility and be accountable for the contents of the article.
Funding
This study was funded by Jazz Pharmaceuticals.
Disclosure
MJT has received research/grant support and consultancy fees from Jazz Pharmaceuticals, Harmony Biosciences, Balance Therapeutics, Axsome Therapeutics, NLS Pharmaceuticals, XW Pharma, Suven Life Sciences, Takeda Pharmaceutical, Idorsia Pharmaceuticals, Eisai Pharmaceuticals, and Flamel/Avadel Pharmaceuticals. IA has participated in an advisory board for Idorsia and received compensation for participating in a speaker bureau for UCB Pharma. N F-S has served on an advisory committee for Jazz Pharmaceuticals and participated in clinical trials supported by Jazz Pharmaceuticals, Suven, Harmony, and Takeda. AMM has received research funding from the National Institutes of Health, Geisinger Health Plan, and the Klarman foundation; has been a site PI for Avadel Pharmaceuticals and Jazz Pharmaceuticals; and has served on an advisory board/speakers bureau for Jazz Pharmaceuticals and advisory boards for Avadel Pharmaceuticals and Harmony Biosciences; he is also a medical advisor for Neura. KŠ has served on the speakers’ bureau for Sanofi, Angelini, and Stada and as a consultant for AOP Orphan, and participated in advisory boards for UCB and in clinical trials for Jazz Pharmaceuticals, Flamel-Avadel, and Luitpold Pharmaceuticals. PC, LH, AC, and AS are full-time employees of Jazz Pharmaceuticals who, in the course of this employment, have received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals, plc. JB is a part-time employee of Jazz Pharmaceuticals and shareholder of Jazz Pharmaceuticals plc. DC is a former full-time employee of Jazz Pharmaceuticals who, in the course of this employment, received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals, plc. RKB has served as a consultant for Jazz Pharmaceuticals, Harmony Biosciences, Balance Therapeutics, Avadel Pharmaceuticals, Takeda, and Oventus, and on the speakers’ bureau for Jazz Pharmaceuticals, Harmony Biosciences, and Eisai. He also reports grants for industry-funded research from Avadel, BresoTec, Idorsia, Suven, Jazz, Balance, Vanda, Merck, Eisai, Philips, Fresca, Takeda, Liva Nova, Roche, Sommetrics, NLS, Sanofi, and Apnimed. He is a shareholder of WaterMark Medical. YD is a consultant for and has participated in advisory boards for Jazz Pharmaceuticals, Orexia, UCB Pharma, Avadel, Idorsia, Takeda, Theranexus, and Bioprojet. The authors report no other conflicts of interest in this work.
References
1. Billiard M, Sonka K. Idiopathic hypersomnia. Sleep Med Rev. 2016;29:23–33. doi:10.1016/j.smrv.2015.08.007
2. Trotti LM. Idiopathic hypersomnia. Sleep Med Clin. 2017;12(3):331–344. doi:10.1016/j.jsmc.2017.03.009
3. American Academy of Sleep Medicine. Idiopathic hypersomnia. In: International Classification of Sleep Disorders.
4. Vernet C, Leu-Semenescu S, Buzare MA, Arnulf I. Subjective symptoms in idiopathic hypersomnia: beyond excessive sleepiness. J Sleep Res. 2010;19(4):525–534. doi:10.1111/j.1365-2869.2010.00824.x
5. Arnulf I, Leu-Semenescu S, Dodet P. Precision medicine for idiopathic hypersomnia. Sleep Med Clin. 2019;14(3):333–350. doi:10.1016/j.jsmc.2019.05.007
6. Evangelista E, Rassu AL, Barateau L, et al. Characteristics associated with hypersomnia and excessive daytime sleepiness identified by extended polysomnography recording. Sleep. 2021;44(5):zsaa264. doi:10.1093/sleep/zsaa264
7. Ozaki A, Inoue Y, Nakajima T, et al. Health-related quality of life among drug-naive patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep time. J Clin Sleep Med. 2008;4(6):572–578. doi:10.5664/jcsm.27352
8. Srivastava B, Morris S, Banderas B, Lowe C, Dauvilliers Y. Patient-reported symptoms and health-related quality of life impacts of idiopathic hypersomnia [abstract].
9. Pizza F, Jaussent I, Lopez R, et al. Car crashes and central disorders of hypersomnolence: a French study. PLoS One. 2015;10(6):e0129386. doi:10.1371/journal.pone.0129386
10. Dauvilliers Y, Paquereau J, Bastuji H, Drouot X, Weil JS, Viot-Blanc V. Psychological health in central hypersomnias: the French Harmony study. J Neurol Neurosurg Psychiatry. 2009;80(6):636–641. doi:10.1136/jnnp.2008.161588
11. Bogan RK, Thorpy MJ, Dauvilliers Y, et al. Efficacy and safety of calcium, magnesium, potassium, and sodium oxybates (lower-sodium oxybate [LXB]; JZP-258) in a placebo-controlled, double-blind, randomized withdrawal study in adults with narcolepsy with cataplexy. Sleep. 2021;44(3):zsaa206. doi:10.1093/sleep/zsaa206
12. Xywav® (calcium, magnesium, potassium, and sodium oxybates) oral solution, CIII [prescribing information]. Palo Alto, CA: Jazz Pharmaceuticals, Inc.; 2021.
13. US Food and Drug Administration. Clinical superiority findings; 2021. Available from: https://www.fda.gov/industry/designating-orphan-product-drugs-and-biological-products/clinical-superiority-findings.
14. Dauvilliers Y, Arnulf I, Foldvary-Schaefer N, et al. Safety and efficacy of lower-sodium oxybate in adults with idiopathic hypersomnia: a phase 3, placebo-controlled, double-blind, randomised withdrawal study. Lancet Neurol. 2022;21(1):53–65. doi:10.1016/S1474-4422(21)00368-9
15. Dauvilliers Y, Arnulf I, Foldvary-Schaefer N, et al. Correlation of the Idiopathic Hypersomnia Severity Scale (IHSS) score with other measures of sleep parameters in a phase 3 trial [poster 500].
16. Rassu AL, Evangelista E, Barateau L, et al. Idiopathic Hypersomnia Severity Scale to better quantify symptoms severity and their consequences in idiopathic hypersomnia. J Clin Sleep Med. 2022;18(2):617–629. doi:10.5664/jcsm.9682
17. American Academy of Sleep Medicine. Idiopathic hypersomnia with long sleep time. In: International Classification of Sleep Disorders: Diagnostic and Coding Manual.
18. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
19. Dauvilliers Y, Evangelista E, Barateau L, et al. Measurement of symptoms in idiopathic hypersomnia: the Idiopathic Hypersomnia Severity Scale. Neurology. 2019;92(15):e1754–e1762. doi:10.1212/WNL.0000000000007264
20. Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the Functional Outcomes of Sleep Questionnaire. Sleep. 2009;32(7):915–919. doi:10.1093/sleep/32.7.915
21. Maski K, Trotti LM, Kotagal S, et al. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2021;17(9):1895–1945. doi:10.5664/jcsm.9326
22. Evangelista E, Lopez R, Dauvilliers Y. Update on treatment for idiopathic hypersomnia. Expert Opin Investig Drugs. 2018;27(2):187–192. doi:10.1080/13543784.2018.1417385
23. Schinkelshoek MS, Fronczek R, Lammers GJ. Update on the treatment of idiopathic hypersomnia. Curr Sleep Med Rep. 2019;5(4):207–214. doi:10.1007/s40675-019-00158-7
24. Bogan RK, Roth T, Schwartz J, Miloslavsky M. Time to response with sodium oxybate for the treatment of excessive daytime sleepiness and cataplexy in patients with narcolepsy. J Clin Sleep Med. 2015;11(4):427–432. doi:10.5664/jcsm.4598
25. Mayer G, Benes H, Young P, Bitterlich M, Rodenbeck A. Modafinil in the treatment of idiopathic hypersomnia without long sleep time–a randomized, double-blind, placebo-controlled study. J Sleep Res. 2015;24(1):74–81. doi:10.1111/jsr.12201
26. Inoue Y, Tabata T, Tsukimori N. Efficacy and safety of modafinil in patients with idiopathic hypersomnia without long sleep time: a multicenter, randomized, double-blind, placebo-controlled, parallel-group comparison study. Sleep Med. 2021;80:315–321. doi:10.1016/j.sleep.2021.01.018
27. US Bureau of Labor Statistics. Household data annual averages. 47. Absences from work of employed full-time wage and salary workers by occupation and industry; 2022. Available from: https://www.bls.gov/cps/cpsaat47.htm.
28. Trotti LM, Ong JC, Plante DT, Friederich Murray C, King R, Bliwise DL. Disease symptomatology and response to treatment in people with idiopathic hypersomnia: initial data from the Hypersomnia Foundation registry. Sleep Med. 2020;75:343–349. doi:10.1016/j.sleep.2020.08.034
29. Šonka K, Šusta M, Billiard M. Narcolepsy with and without cataplexy, idiopathic hypersomnia with and without long sleep time: a cluster analysis. Sleep Med. 2015;16(2):225–231. doi:10.1016/j.sleep.2014.09.016
30. Vernet C, Arnulf I. Idiopathic hypersomnia with and without long sleep time: a controlled series of 75 patients. Sleep. 2009;32(6):753–759. doi:10.1093/sleep/32.6.753
31. Wickwire EM, Verma T. Value and payment in sleep medicine. J Clin Sleep Med. 2018;14(5):881–884. doi:10.5664/jcsm.7130
32. Schneider L, Stevens J, Husain A, Ito D, Fuller DS, Macfadden W. Characteristics and disease burden of patients with idiopathic hypersomnia with and without long sleep time: the Real-World Idiopathic Hypersomnia Outcomes Study (ARISE) [abstract].
33. Saad R, Ben-Joseph R, Prince P, Stack C, Bujanover S, Taylor B. Utilization of diagnostic sleep testing prior to idiopathic hypersomnia diagnosis among US adults: a real-world claims analysis [abstract 499]. Sleep. 2021;44(suppl2):A197. doi:10.1093/sleep/zsab072.498
34. Lammers GJ, Bassetti CLA, Dolenc-Groselj L, et al. Diagnosis of central disorders of hypersomnolence: a reappraisal by European experts. Sleep Med Rev. 2020;52:101306. doi:10.1016/j.smrv.2020.101306
35. Nevsimalova S, Susta M, Prihodova I, Maurovich Horvat E, Milata M, Sonka K. Idiopathic hypersomnia: a homogeneous or heterogeneous disease? Sleep Med. 2021;80:86–91. doi:10.1016/j.sleep.2021.01.031
36. Leu-Semenescu S, Louis P, Arnulf I. Benefits and risk of sodium oxybate in idiopathic hypersomnia versus narcolepsy type 1: a chart review. Sleep Med. 2016;17:38–44. doi:10.1016/j.sleep.2015.10.005
37. Xyrem® (sodium oxybate) oral solution, CIII [prescribing information]. Palo Alto, CA: Jazz Pharmaceuticals, Inc.; 2020.
38. U.S. Xyrem Multicenter Study Group. A randomized, double blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25(1):42–49.
39. U.S. Xyrem Multicenter Study Group. Sodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsy. Sleep Med. 2004;5(2):119–123. doi:10.1016/j.sleep.2003.11.002
40. Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006;29(7):939–946. doi:10.1093/sleep/29.7.939
41. Xyrem International Study Group. A double-blind, placebo-controlled study demonstrates sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsy. J Clin Sleep Med. 2005;1(4):391–397. doi:10.5664/jcsm.26368
42. Husain AM, Bujanover S, Ryan R, Scheckner B, Black J, Profant J. Incidence and duration of common, early-onset adverse events occurring during 2 randomized, placebo-controlled, phase 3 studies of sodium oxybate in participants with narcolepsy. J Clin Sleep Med. 2020;16(9):1469–1474. doi:10.5664/jcsm.8530
43. Bogan RK, Foldvary-Schaefer N, Skowronski R, Chen A, Thorpy MJ. Timing and duration of treatment-emergent adverse events in a clinical trial of lower-sodium oxybate in participants with narcolepsy with cataplexy [poster 486].
44. Finniss DG, Kaptchuk TJ, Miller F, Benedetti F. Biological, clinical, and ethical advances of placebo effects. Lancet. 2010;375(9715):686–695. doi:10.1016/S0140-6736(09)61706-2
45. Pascoe M, Bena J, Foldvary-Schaefer N. Effects of pharmacotherapy treatment on patient-reported outcomes in a narcolepsy and idiopathic hypersomnia cohort. J Clin Sleep Med. 2019;15(12):1799–1806. doi:10.5664/jcsm.8088
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.