Back to Journals » Journal of Pain Research » Volume 17
Efficacy and Safety of Ketamine Compared with Placebo and Other Medications for Preventing Propofol Injection Pain in Adults: A Systematic Review and Meta-Analysis
Authors Wu Q , Xu F , Wang J , Jiang M
Received 5 October 2023
Accepted for publication 19 January 2024
Published 1 February 2024 Volume 2024:17 Pages 459—476
DOI https://doi.org/10.2147/JPR.S440250
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jinlei Li
Quantong Wu,1 Fuchao Xu,2 Jie Wang,3 Ming Jiang2
1Department of Anesthesiology, Nanjing Drum Tower Hospital Clinical College, Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China; 2Emergency Department, Nanjing Drum Tower Hospital Clinical College, Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China; 3Neurosurgery department, Nanjing Drum Tower Hospital Clinical College, Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China
Correspondence: Ming Jiang, Department of Anesthesiology, Nanjing Drum Tower Hospital Clinical College, Nanjing Medical University, Gulou District, Nanjing, Jiangsu, People’s Republic of China, Email [email protected]
Purpose: To systematically evaluate the effectiveness and safety of ketamine in preventing propofol injection pain (PIP).
Patients and Methods: The electronic databases including PubMed, Embase, Web of Science, and Cochrane Library were searched from their inception until 2 August 2023. Randomized controlled trials (RCT) comparing ketamine with placebo or other interventions to alleviate PIP in adults were included. Fixed-effects or random-effects models were used to calculate pooled risk ratios (RR) and corresponding 95% confidence intervals (CI) based on the heterogeneity of the studies included.
Results: Thirteen RCTs involving 2105 patients were included. In terms of reducing the incidence of PIP, ketamine is more effective than placebo (RR = 0.43, 95% CI = [0.34, 0.55], P < 0.00001), lidocaine (RR = 0.70, 95% CI = [0.55, 0.90], P = 0.005), dexmedetomidine (RR = 0.52, 95% CI = [0.40, 0.66], P < 0.00001), and thiopental (RR = 0.25, 95% CI = [0.08, 0.83], P = 0.02). In reducing the incidence of severe PIP, ketamine is superior to placebo (RR = 0.12, 95% CI = [0.08, 0.19], P < 0.00001), and lidocaine (RR = 0.34, 95% CI = [0.21, 0.56], P < 0.0001), except dexmedetomidine (RR = 0.20, 95% CI = [0.04, 1.13], P = 0.07), and thiopental (RR = 0.33, 95% CI = [0.04, 3.10], P = 0.33). Compared with mixed injection, separate injection of ketamine and propofol showed no significant difference in the incidence of PIP (RR = 0.96, 95% CI = [0.31, 3.00], P = 0.95) and severe PIP (RR = 1.19, 95% CI = [0.07, 21.29], P = 0.90). Based solely on the reports from the studies included, subanesthetic doses of ketamine are generally safe in preventing PIP.
Conclusion: A subanesthetic dose of ketamine can effectively and safely reduce the incidence of PIP and severe PIP in adults, and is more effective than lidocaine, dexmedetomidine, and thiopental.
Registration: PROSPERO CRD42023455093.
Keywords: ketamine, pain, injection, propofol, meta-analysis
Introduction
Propofol is currently the most commonly used intravenous anesthetic worldwide and has many advantages, including fast onset, quick metabolism, smooth induction, and rapid recovery, making it widely used in general anesthesia and procedural sedation.1 However, injection pain is one of the most common side effects of propofol, causing patients painful experiences, unnecessary body movements, and even cardiovascular adverse events during the induction process, and has become the seventh problem that American anesthetists most want to solve.2 The incidence of propofol injection pain (PIP) during induction has been reported to be 28–90% in adults, 28–85% in children,3 and 70% on average.4
Medications that have been reported to prevent PIP include lidocaine,5,6 thiopental,7 opioids,8,9 dexmedetomidine,10 non-steroidal anti-inflammatory drugs (NSAIDs),11 metoclopramide,12 magnesium sulfate,13 ephedrine,14 ondansetron,15 etc. Techniques include the use of a larger antecubital vein,16 venous occlusion combined with drug pretreatment,17 alterations of the concentration and pH of propofol,18 and transcutaneous electrical acupoint stimulation.19 However, to date, no method has been found that completely or almost completely prevents the occurrence of PIP.
A fast-acting intravenous anesthetic introduced in 1970, ketamine produces sedative, hypnotic, amnestic, and potent analgesic effects, primarily through non-competitive antagonism of the N-methyl-D-aspartate (NMDA) receptor.20 Moreover, research has revealed that ketamine also has local anesthetic effects by blocking voltage-gated sodium channels.21 In recent years, numerous studies have disclosed the impact of ketamine pre-treatment or being combined with propofol to prevent PIP. Nevertheless, the efficacy and superiority of this treatment over alternative pharmacological solutions are still contentious. To date, there has been no systematic review or meta-analysis conducted to individually assess the effectiveness and safety of this medication. This systematic review and meta-analysis aimed to assess the effectiveness and safety of ketamine in preventing PIP in adults. The evaluation involved comparing the efficacy of ketamine with both placebo (saline) and other medications in terms of reducing the incidence of PIP and severe PIP. Additionally, the review sought to analyze the potential side effects associated with ketamine treatment.
Materials and Methods
The review was conducted following the methods recommended by the Cochrane Collaboration and written following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement.22 The protocol has been registered on the PROSPERO website (ID: CRD42023455093).
Eligibility Criteria
Studies meeting the following criteria were included: (1) Participants: Adult patients classified as American Society of Anesthesiologists (ASA) class I or II underwent sedation or anesthesia with propofol. (2) Interventions: Patients received racemic ketamine pretreatment before propofol injection through the same vein or a mixed injection of racemic ketamine and propofol. (3) Controls: Use of placebo or alternative medications to substitute for ketamine. (4) Primary outcomes: The incidence and severity of PIP. (5) Study design: Randomized controlled trials (RCT) published in English.
Studies meeting any of the following criteria were excluded: (1) Use of other analgesics before or at the same time as propofol injection, other than the experimental and control medications. (2) Trial registration for which outcome data were not available. (3) The incidence or severity of PIP was not the primary outcome. (4) Unavailable or non-credible data.
Search Strategy
The electronic databases including PubMed, Embase, Web of Science, and Cochrane Library were searched from their inception until 2 August 2023. Search terms such as “ketamine” and “propofol injection pain” were utilized, with limitations concerning species and article types. While conducting the search in the Cochrane Library, trial registries were also explored to identify unpublished data. The complete search strategy for each database is provided in the Supplementary Materials. Additionally, citations from the included articles and relevant research were manually retrieved to identify potential qualified studies.
Selection Process
Two reviewers (QW and FX) carried out the search independently, removed duplicate articles through automated procedures and manual intervention, screened the remaining articles by reading titles and abstracts, and read the full text of the remaining articles to determine the final selection of articles for inclusion. Any disagreements that arose during the screening process were resolved through discussion to reach a consensus; otherwise, the decision would be left to another author (MJ).
Data Extraction
Data from the included articles were extracted by two reviewers (QW and FX) independently and logged within a spreadsheet crafted for this purpose. If any crucial data were not present in an article that fulfilled the criteria for inclusion, the reviewers would get in touch with the authors via email to request the data. Discussions were held to reach a consensus on any disagreements during the data extraction. The following information was extracted from each selected article: first author, year of publication, country or region, study design, grouping and intervention strategies, sample size, demographics, procedure, anesthesia regimen, pain rating scale, primary and secondary outcomes, and its data.
Outcome Measures
The objective of this study was to assess the effectiveness and safety of ketamine in treating PIP in adults. Effectiveness was gauged by comparing the incidence of PIP and severe PIP across various treatments. In all included studies, any level of pain detected by a pain scale following propofol injection was categorized as PIP, while severe PIP was defined as a 3-point scale score of 2, a Verbal Rating Scale (VRS) score of 3, or a Visual Analogue Scale (VAS) score of 7–10. Safety evaluation involved analyzing the incidence of complications related to ketamine administration.
Risk of Bias Assessment
The revised Cochrane risk of bias tool for randomized trials (RoB 2), last updated on 22 August 2019,23 was used by two independent reviewers (QW and FX) to assess the quality of the included RCTs. The quality of each RCT was evaluated by answering signaling questions from five domains: randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. The tool automatically calculated the risk for each domain based on the answers to the signaling questions, and the result was either low risk, some concerns, or high risk. The overall bias rating would align with the worst domain. Any discrepancies were discussed to reach a consensus. The results of the assessment were presented graphically using the Review Manager software (Version 5.4. The Cochrane Collaboration, 2020).
Data Synthesis and Analysis
Data synthesis and analysis were performed using Stata 17 software (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC). The data extracted from the RCTs included in this review were dichotomous variables, therefore, the risk ratios (RR) were applied as effect size and expressed with 95% confidence intervals (CI). If the 95% CI of RR included 1, there would not be any statistically significant difference. The heterogeneity was evaluated using the Cochrane Q test and the I² test. A mild heterogeneity was indicated if I² < 50%, and the data would be pooled using a fixed-effects model and the Mantel-Haenszel method. Otherwise, a significant heterogeneity would be considered, and a random-effects model and the Dersimonian-Laird method would be employed. Sources of heterogeneity were explored using meta-regression analysis and served as the basis for setting subgroups. Sensitivity analyses were performed to validate the reliability and stability of the results. The results of the statistical analysis were summarized and presented in the forest plots. For publication bias, the funnel plot was used for qualitative detection, the Egger test was used for quantitative detection, and the trim-and-fill procedure was used to evaluate the results adjusted for publication bias.
Results
Search results
A total of 455 relevant records were initially retrieved from the designated databases, and 155 duplicate records were removed by automation tools and humans. Of the 300 remaining records, 266 were eliminated after reading their titles and abstracts. A further 21 were excluded after reading the full-text articles. Reasons for exclusion included: not a Randomized Controlled Trial (n = 2), pilot studies (n = 4), conference articles (n = 2), ineligible interventions (n = 3), not racemic ketamine (n = 2), not primary outcome (n = 1), not adults (n = 4), and unavailable data (n = 3). The selection process is depicted in Figure 1.
 |
Figure 1 The flow diagram of the selection process. |
Study Characteristics
After meticulous screening, a total of 13 RCTs involving 2105 patients from eight countries were included in the review.24–36 The baseline characteristics of each RCT are presented in Table 1. Of the studies included, eight used 1% propofol, one used 2% propofol, and the rest did not report. Eleven studies administered separate injections of the test drugs and propofol, and two studies administered both separate and mixed injections and compared their effects. Four studies performed venous occlusion for over 30 seconds during injection of the test drugs, while the remaining studies did not. Only one study omitted the injection site information, while others reported injecting drugs through the dorsal vein of the hand or wrist. Eleven studies evaluated the injection pain with the VRS, whereas one study employed the 3-point scale, and one study utilized the VAS.
 |
Table 1 Characteristics of Included RCTs |
Risk of Bias
Assessments of the risk of bias are presented in Figure 2. Regarding the randomization process, nine studies25,27,29–35 provided detailed information on random sequence generation, allocation concealment, and similar demographics, and were assessed as low risk, while the remaining studies24,26,28,36 were rated as having some concerns due to insufficient information. All studies were assessed as low risk concerning deviations from the intended interventions and missing outcome data. With regard to the measurement of outcome, one study24 was assessed as high risk because the outcome assessors were not blinded. In terms of the selection of the reported result, except for two studies,24,25 the rest26–36 did not provide detailed information about trial registration and were assessed as having some concerns. The overall bias rating equals that of the worst domain.
 |
Figure 2 The risk of bias of the included studies; (a) risk of bias for each study; (b) risk of bias summary. |
Meta-Analysis
Incidence of Propofol Injection Pain
Ketamine versus Saline
Among the included studies, eight RCTs25,26,28–30,32,33,36 compared the effects of ketamine with saline. To address the high heterogeneity after direct pooling (I2 = 87%), we conducted a meta-regression analysis before subgroup analysis. Our findings showed that the dose of ketamine was the primary source of heterogeneity (P = 0.001, 95% CI = [−0.54, −0.13]), thus prompting us to apply subgroup analysis based on the ketamine dose. The forest plot is presented in Figure 3. The results showed statistically significant differences between the ketamine and saline groups in the incidence of PIP (44.23% versus 87.37%, RR = 0.43, 95% CI = [0.34, 0.55], P < 0.00001).
 |
Figure 3 The incidence of propofol injection pain in the ketamine group compared with the saline group. |
Ketamine versus Lidocaine
Seven RCTs25,26,29–32,36 involving 1041 patients compared the use of ketamine and lidocaine. As a result of significant heterogeneity (I2 = 64.90%), the data were combined utilizing the random-effects model and the DerSimonian-Laird method. Subgroup analysis by ketamine dose was not performed again because the seven studies had similar ketamine doses. Compared with the lidocaine group, the ketamine group had a lower incidence of PIP (45.83% versus 55.59%, RR = 0.70, 95% CI = [0.55, 0.90], P = 0.005) (Figure 4).
 |
Figure 4 The incidence of propofol injection pain in the ketamine group compared with the lidocaine group. |
Ketamine versus Dexmedetomidine
Two RCTs34,35 compared the incidence of PIP in the ketamine and dexmedetomidine groups. Meta-analysis using a fixed-effects model and Mantel-Haenszel method revealed a significantly lower incidence of PIP in the ketamine group as compared with the dexmedetomidine group (41.35% versus 79.81%, RR = 0.52, 95% CI = [0.40, 0.66], P < 0.00001) (Figure 5).
 |
Figure 5 The incidence of propofol injection pain in the ketamine group compared with the dexmedetomidine group. |
Ketamine versus Thiopental
Two RCTs24,32 compared the use of ketamine and thiopental for preventing PIP. After pooling the data using the fixed-effects model and Mantel-Haenszel method, previously non-significant results became statistically significant and showed that ketamine was more effective (12.00% versus 24.00%, RR = 0.25, 95% CI = [0.08, 0.83], P = 0.02) (Figure 6). Such an alteration could be attributed to the growth in sample size after the pooling.
 |
Figure 6 The incidence of propofol injection pain in the ketamine group compared with the thiopental group. |
Separate Injection versus Mixed Injection
Two RCTs27,30 compared the ketamine-propofol mixture with ketamine pretreatment. However, the results of the two RCTs were diametrically opposite (I2 = 94.15%), and the results pooled through the random-effects model and DerSimonian-Laird method lack statistical significance (50.00% versus 43.55%, RR = 0.96, 95% CI = [0.31, 3.00], P = 0.95) (Figure 7).
 |
Figure 7 The incidence of propofol injection pain in the separate injection group compared with the mixed injection group. |
Incidence of Severe Propofol Injection Pain
Ketamine versus Saline
The PIP scores were reported in eight RCTs25,26,28–30,32,33,36 for both the ketamine and saline groups. Only one33 of these studies used the 3-point scale, while the remaining studies utilized the Verbal Rating Scale (VRS). According to consensus, a 3-point scale score of 2 and a VRS score of 3 are considered severe pain. Eight RCTs were divided into three subgroups based on the dosage of ketamine, as previously stated. After pooling the data using the fixed-effects model and Mantel-Haenszel method (I2 = 42.21%), the meta-analysis results are shown in Figure 8. The ketamine group exhibited a significantly lower incidence of severe PIP compared with the saline group (2.37% versus 24.25%, RR = 0.12, 95% CI = [0.08, 0.19], P < 0.00001).
 |
Figure 8 The incidence of severe propofol injection pain in the ketamine group compared with the saline group. |
Ketamine versus Lidocaine
The PIP scores in the ketamine group and the lidocaine group were reported by seven RCTs.25,26,29–32,36 Only one31 of these studies used the Visual Analogue Scale (VAS), while the remaining six all used the VRS. According to consensus, a VAS score of 7–10 and a VRS score of 3 are considered severe pain. After pooling the data using the fixed-effects model and Mantel-Haenszel method (I2 = 0.00%), the meta-analysis results are shown in Figure 9. The incidence of severe PIP was significantly lower in the ketamine group compared with the lidocaine group (2.78% versus 12.85%, RR = 0.34, 95% CI = [0.21, 0.56], P < 0.0001).
 |
Figure 9 The incidence of severe propofol injection pain in the ketamine group compared with the lidocaine group. |
Ketamine versus Dexmedetomidine
Two studies34,35 evaluated the PIP scores of the ketamine and dexmedetomidine groups using the VRS. The results of the meta-analysis are presented in Figure 10. Although there was a lower incidence of severe PIP in the ketamine group compared with the dexmedetomidine group, this difference did not reach statistical significance (0.96% versus 6.73%, RR = 0.20, 95% CI = [0.04, 1.13], P = 0.07).
 |
Figure 10 The incidence of severe propofol injection pain in the ketamine group compared with the dexmedetomidine group. |
Ketamine versus Thiopental
Two RCTs24,32 compared the efficacy of ketamine and thiopental in preventing severe PIP, and the pooled results are shown in Figure 11. The pooled data indicates that ketamine has comparable efficacy to thiopental in preventing severe PIP (0.00% versus 4.00%, RR = 0.33, 95% CI = [0.04, 3.10], P = 0.33).
 |
Figure 11 The incidence of severe propofol injection pain in the ketamine group compared with the thiopental group. |
Separate Injection versus Mixed Injection
Two RCTs27,30 compared the incidence of severe PIP between the two methods of ketamine administration. Due to the high heterogeneity between the two studies (I2 = 67.25%), the random-effects model and DerSimonian-Laird method were employed to pool the data. The results, as depicted in Figure 12, indicated no statistically significant difference in efficacy between the two administration methods for preventing severe PIP (6.45% versus 3.23%, RR = 1.19, 95% CI = [0.07, 21.29], P = 0.90).
 |
Figure 12 The incidence of severe propofol injection pain in the separate injection group compared with the mixed injection group. |
Safety Assessment
Ten studies described the safety evidence of ketamine for treating PIP, which is both sporadic and diverse. Regarding the heart rate post-administration, five studies25,30,32,33,36 reported that ketamine did not cause more changes in heart rate compared to the saline group, while one study35 reported more occurrences of tachycardia in the ketamine group compared with the dexmedetomidine group. Four studies25,30,33,36 reported similarity in blood pressure changes after ketamine administration compared to the saline group, while one study32 found that ketamine administration prevented blood pressure from dropping after the induction. Only two studies28,33 reported on oxygenation, and both claimed that ketamine administration did not have a significant impact on oxygenation, despite the potential for increased airway secretions. As for the psychiatric side effects of ketamine that concern most anesthesiologists, only one study29 reported abnormal behavioral responses in 5 out of 96 patients that did not require active intervention; the other five studies27,28,30,33,36 found no such effects. We could not conduct a quantitative meta-analysis for these outcomes due to the varying disease definitions and measures utilized in the included studies.
Sensitivity Analysis
For a meta-analysis that was highly heterogeneous and included more than two studies, we performed a sensitivity analysis. The sensitivity analysis was conducted by systematically excluding individual studies to assess the stability of the meta-analysis findings. The results of these meta-analyses are reliable and stable as shown in Figures 13 and 14.
 |
Figure 13 Sensitivity analysis for meta-analysis comparing the incidence of PIP in the ketamine group and the saline group. |
 |
Figure 14 Sensitivity analysis for meta-analysis comparing the incidence of PIP in the ketamine group and the lidocaine group. |
Publication Bias
We assessed publication bias for the meta-analyses with the most included studies, which compared the incidence of PIP and severe PIP of the ketamine group versus the saline group. Publication bias was found in both the meta-analyses by funnel plots and Egger tests. The trim-and-fill procedure was applied to evaluate the results corrected for publication bias, and the processed funnel plots are shown in Figures 15 and 16. After processing, the statistical results remain significant, suggesting that the outcomes of 1.1 and 2.1 are unaffected despite the potential for publication bias. Table 2 provides the results of the Egger tests and trim-and-fill procedure.
 |
Table 2 Results of Egger Tests and Trim-and-Fill Procedure |
 |
Figure 15 The funnel plot for the meta-analysis 1.1 processed by the trim-and-fill method. |
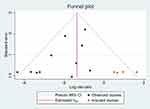 |
Figure 16 The funnel plot for the meta-analysis 2.1 processed by the trim-and-fill method. |
Discussion
Propofol is undoubtedly the most commonly used intravenous anesthetic and has been employed in over one billion surgeries performed on humans since its introduction into clinical practice.1 However, the pain caused by propofol injections is a recurring issue for patients and a challenge for anesthesiologists who encounter it daily, yet it remains a difficult problem to fully resolve. Propofol injection pain (PIP) may occur either immediately or 10–20 seconds following injection.3 Prompt pain may result from direct stimulation of the vein, whereas postponed pain may be attributed to the kinin cascade.37 Ketamine is a rapid-acting intravenous anesthetic providing potent local and central analgesic effects. This meta-analysis compared the efficacy of ketamine with placebo and some reported drugs for preventing PIP.
Similar to the partial results of the meta-analysis conducted by Jalota et al,38 our meta-analysis, including recently published studies from the past decade but excluding non-English language literature, confirms the effectiveness of ketamine in reducing the incidence of PIP. In addition, our results indicated that ketamine can effectively reduce the severity of PIP as well. The mechanism through which ketamine prevents PIP is still unclear, and research on related mechanisms is deficient. Some scholars speculate that the local anesthetic effect may play a significant role, rather than its central analgesic effect.33
Lidocaine was previously the drug of choice for preventing PIP,37 and was also recommended by the manufacturer of propofol.3 The results of this meta-analysis indicated that ketamine is more effective than lidocaine in preventing the occurrence and severity of PIP in adults. However, the meta-analysis conducted by Lang et al suggested that the two drugs have similar effects on children.39 Such a discrepancy may stem from differences in the populations and sample sizes that were included, and it is worth noting that our meta-analysis comprised a larger number of adult patients.
In recent years, studies have employed dexmedetomidine as a means to prevent PIP and have demonstrated both its efficacy and safety.10,40,41 Compared with dexmedetomidine, our findings indicate that ketamine is more effective in reducing the incidence of PIP. This aligns with the partial conclusions drawn by Ji et al.42 But in terms of safety and availability, dexmedetomidine has fewer contraindications, is safer to use, and is less likely to cause psychiatric side effects.43 However, coadministration of dexmedetomidine and propofol could heighten the incidence of bradycardia and hypotension,44 while ketamine diminishes this incidence.45 Moreover, ketamine can provide more comprehensive analgesic effects for surgeries than dexmedetomidine.
Compared with thiopental, our results suggest that ketamine is more effective in reducing the incidence, but not the severity, of PIP. Before this, the results of individual studies included in this review indicated no statistically significant difference in efficacy between the two drugs. Nevertheless, upon pooling the data, the results became statistically significant. This alteration might have resulted from the enlarged sample size after pooling.
We also compared the ketamine-propofol mixture with ketamine pretreatment. However, as the included studies were fewer and heterogeneous, we obtained statistically insignificant and unstable results. More high-quality randomized controlled trials comparing the effects of the two injection methods are needed in the future. Regarding safety, a quantitative analysis could not be conducted. Based solely on the reports from the studies included, subanesthetic doses of ketamine (≤ 1.0 mg/kg) appear to be generally safe for preventing PIP. Although the studies cited above involved ketamine to some extent, this study is, to our knowledge, the first to systematically review and analyze the effectiveness and safety of ketamine in preventing PIP.
Limitations
Although we employed scientific methods for our systematic review and meta-analysis, there are still certain limitations present. In terms of the quality of the evidence, although only one of the included studies was rated as high risk, several studies were rated as some concerns in the “selection of the reported result” domain attributed to the absence of trial registration. In addition, the generalizability of our findings to various age groups is restricted due to the exclusion of research involving children. In terms of methodology, certain outcomes in the meta-analysis displayed high heterogeneity due to the included studies using various drug doses and dosing regimens. Although the major source of heterogeneity was identified through meta-regression, subgroup analyses remained highly heterogeneous. Fortunately, the sensitivity analysis indicates that the results are stable This review excluded articles written in languages other than English, which may have contributed to the presence of publication bias. Fortunately, the trim-and-fill procedure indicated that the stability of these results was not affected by publication bias. Last but not least, as an additional outcome, the safety of ketamine in preventing PIP was not evaluated through a quantitative meta-analysis as the included studies used various definitions and measures of complications.
Conclusion
In conclusion, ketamine proves to be a potent drug in preventing propofol injection pain (PIP), leading to a marked reduction in its incidence and severity, and surpasses lidocaine, dexmedetomidine, and thiopental in efficacy. Although its safety has been questioned, our findings indicate that subanesthetic doses of ketamine are generally safe for the prevention of PIP. The future exploration of ketamine’s specific mechanism in preventing PIP and the further study of esketamine’s efficacy and safety in preventing PIP are necessary.
Data Sharing Statement
The corresponding author of this study can provide the data upon request.
Funding
No external funding was received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ct W. Propofol: milk of Amnesia. Cell. 2018;175(1):10–13. doi:10.1016/j.cell.2018.08.031
2. Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg. 1999;88(5):1085–1091. doi:10.1097/00000539-199905000-00023
3. Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia. 1998;53(5):468–476. doi:10.1046/j.1365-2044.1998.00405.x
4. Picard P, Tramer MR. Prevention of pain on injection with propofol: a quantitative systematic review. Anesth Analg. 2000;90(4):963–969. doi:10.1097/00000539-200004000-00035
5. Euasobhon P, Dej-Arkom S, Siriussawakul A, et al. Lidocaine for reducing propofol-induced pain on induction of anaesthesia in adults. Cochrane Database Syst Rev. 2016;2(2):CD007874. doi:10.1002/14651858.CD007874.pub2
6. Kam E, Abdul-Latif MS, McCluskey A. Comparison of propofol-lipuro with propofol mixed with lidocaine 10 mg on propofol injection pain. Anaesthesia. 2004;59(12):1167–1169. doi:10.1111/j.1365-2044.2004.03964.x
7. Agarwal A, Ansari MF, Gupta D, et al. Pretreatment with thiopental for prevention of pain associated with propofol injection. Anesth Analg. 2004;98(3):683–686. doi:10.1213/01.ANE.0000103266.73568.18
8. Gao W, Sha B, Zhao Y, Fan Z, Liu L, Shen X. Comparison of simultaneous and sequential administration of fentanyl-propofol for surgical abortion: a randomized single-blinded controlled trial. Artif Cells Nanomed Biotechnol. 2017;45(5):1045–1050. doi:10.1080/21691401.2016.1239106
9. Zhou C, Yang Y, Zhu Y, Ruan L. Effects of dezocine on prevention of propofol injection pain: a meta-analysis. J Pain Res. 2017;10:1369–1375. doi:10.2147/JPR.S128889
10. He L, Xu JM, He T, Liu L, Zhu R. Dexmedetomidine pretreatment alleviates propofol injection pain. Ups J Med Sci. 2014;119(4):338–342. doi:10.3109/03009734.2014.941049
11. Zhang L. Efficacy and safety of flurbiprofen axetil in the prevention of pain on propofol injection: a systematic review and meta-analysis. Med Sci Monit. 2014;20:995–1002. doi:10.12659/MSM.890102
12. Ganta R, Fee JP. Pain on injection of propofol: comparison of lignocaine with metoclopramide. Br J Anaesth. 1992;69(3):316–317. doi:10.1093/bja/69.3.316
13. Agarwal A, Dhiraj S, Raza M, et al. Vein pretreatment with magnesium sulfate to prevent pain on injection of propofol is not justified. Can J Anaesth. 2004;51(2):130–133. doi:10.1007/BF03018771
14. Gilani MT, Bameshki A, Razavi M. Efficacy of ephedrine in the prevention of vascular pain associated with different infusion rates of propofol. Anesth Essays Res. 2014;8(3):345–348. doi:10.4103/0259-1162.143137
15. Pei S, Zhou C, Zhu Y, Huang B. Efficacy of ondansetron for the prevention of propofol injection pain: a meta-analysis. J Pain Res. 2017;10:445–450. doi:10.2147/JPR.S128992
16. Bachmann-Mennenga B, Ohlmer A, Heesen M. Incidence of pain after intravenous injection of a medium-/long-chain triglyceride emulsion of propofol. An observational study in 1375 patients. Arzneimittelforschung. 2003;53(9):621–626.
17. Canbay O, Celebi N, Arun O, Karagoz AH, Saricaoglu F, Ozgen S. Efficacy of intravenous acetaminophen and lidocaine on propofol injection pain. Br J Anaesth. 2008;100(1):95–98. doi:10.1093/bja/aem301
18. Sim JY, Lee SH, Park DY, et al. Pain on injection with microemulsion propofol. Br J Clin Pharmacol. 2009;67(3):316–325. doi:10.1111/j.1365-2125.2008.03358.x
19. Jin D, Pan Y, Jin W, Yan Y, Huang L, Wang J. Clinical study on the combination of transcutaneous electrical acupoint stimulation and lidocaine for preventing propofol injection pain. J Pain Res. 2022;15:745–755. doi:10.2147/JPR.S356150
20. Zanos P, Moaddel R, Morris PJ, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70(3):621–660. doi:10.1124/pr.117.015198
21. Zhou ZS, Zhao ZQ. Ketamine blockage of both tetrodotoxin (TTX)-sensitive and TTX-resistant sodium channels of rat dorsal root ganglion neurons. Brain Res Bull. 2000;52(5):427–433. doi:10.1016/S0361-9230(00)00283-5
22. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
23. Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi:10.1136/bmj.l4898
24. Akbari H, Nasiri E, Nikkhah A, Ardehali SH. Analgesic effects of ketamine, magnesium sulfate, and sodium-thiopental on propofol injection pain: a single-blind randomized clinical trial. Tanaffos. 2018;17(1):22–29.
25. Ayatollahi V, Behdad S, Kargar S, Yavari T. Comparison of effects of ephedrine, lidocaine and ketamine with placebo on injection pain, hypotension and bradycardia due to propofol injection: a randomized placebo controlled clinical trial. Acta Med Iran. 2012;50(9):609–614.
26. Batra YK, Al Qattan AR, Marzouk HM, Smilka M, Agzamov A. Ketamine pretreatment with venous occlusion attenuates pain on injection with propofol. Eur J Anaesthe. 2005;22(1):69–70. doi:10.1097/00003643-200501000-00015
27. Hwang J, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Preventing pain on injection of propofol: a comparison between peripheral ketamine pre-treatment and ketamine added to propofol. Anaesth Int Care. 2009;37(4):584–587. doi:10.1177/0310057X0903700404
28. Iwata M, Inoue S, Kawaguchi M, et al. Ketamine eliminates propofol pain but does not affect hemodynamics during induction with double-lumen tubes. J Anesthesia. 2010;24(1):31–37. doi:10.1007/s00540-009-0833-5
29. Jayaprakash R, Prathibha VK, Gopakumar G, Thomas M. Effect of small-dose ketamine in the prevention of pain on propofol injection: a prospective randomized controlled study. National J Phy Pharm. 2020;10(5):437–441.
30. Koo SW, Cho SJ, Kim YK, Ham KD, Hwang JH. Small-dose ketamine reduces the pain of propofol injection. Anesthesia Analg. 2006;103(6):1444–1447. doi:10.1213/01.ane.0000243334.83816.53
31. Naz U, Wadood F, Aurangzeb I, Ullah M, Bangash AS. Effectiveness of low dose ketamine and lignocaine in prevention of propofol induced pain. J Med Sci. 2020;28(1):16–20.
32. Saadawy I, Ertok E, Boker A. Painless injection of propofol: pretreatment with ketamine vs thiopental, meperidine, and lidocaine. Middle East j Anaesthe. 2007;19(3):631–644.
33. Tan CH, Onsiong MK, Kua SW. The effect of ketamine pretreatment on propofol injection pain in 100 women. Anaesthesia. 1998;53(3):302–305. doi:10.1046/j.1365-2044.1998.00287.x
34. Thukral S, Gupta P, Lakra A, Gupta M. Dexmedetomidine versus ketamine infusion to alleviate propofol injection pain: a prospective randomized and double-blind study. Indian J Anaes. 2015;59(8):488–492. doi:10.4103/0019-5049.162987
35. Wani MA, Wani S, Dogra S, Jitendra M. Comparison of injection dexmedetomidine with injection ketamine in alleviation of propofol injection pain. JK Sci. 2018;20(1):30–33.
36. Zahedi H, Nikooseresht M, Seifrabie M. Prevention of propofol injection pain with small-dose ketamine. Middle East j Anaesthe. 2009;20(3):401–404.
37. Desousa KA. Pain on propofol injection: causes and remedies. Indian J Pharmacol. 2016;48(6):617–623. doi:10.4103/0253-7613.194845
38. Jalota L, Kalira V, George E, et al. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ. 2011;342:d1110.
39. Lang BC, Yang CS, Zhang LL, Zhang WS, Fu YZ. Efficacy of lidocaine on preventing incidence and severity of pain associated with propofol using in pediatric patients: a PRISMA-compliant meta-analysis of randomized controlled trials. Medicine. 2017;96(11):e6320. doi:10.1097/MD.0000000000006320
40. Yu J, Zhang Y, Lu Y, Dong C. Preemptive dexmedetomidine to prevent propofol injection pain in children. Ir J Med Sci. 2015;184(2):375–378. doi:10.1007/s11845-014-1122-3
41. Li X, Chen CJ, Tan F, et al. Effect of dexmedetomidine for attenuation of propofol injection pain in electroconvulsive therapy: a randomized controlled study. J Anesthesia. 2018;32(1):70–76. doi:10.1007/s00540-017-2430-3
42. Ji L, Sun W, Lan Y, et al. Dexmedetomidine for prevention of propofol injection pain upon induction of anesthesia: a meta-analysis. Eur J Clin Pharmacol. 2020;76(8):1103–1110. doi:10.1007/s00228-020-02889-x
43. Keating GM. Dexmedetomidine: a review of its use for sedation in the intensive care setting. Drugs. 2015;75(10):1119–1130. doi:10.1007/s40265-015-0419-5
44. Lewis K, Alshamsi F, Carayannopoulos KL, et al. Dexmedetomidine vs other sedatives in critically ill mechanically ventilated adults: a systematic review and meta-analysis of randomized trials. Intensive Care Med. 2022;48(7):811–840. doi:10.1007/s00134-022-06712-2
45. Guit JB, Koning HM, Coster ML, Niemeijer RP, Mackie DP. Ketamine as analgesic for total intravenous anaesthesia with propofol. Anaesthesia. 1991;46(1):24–27. doi:10.1111/j.1365-2044.1991.tb09308.x
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
