Back to Journals » Drug Design, Development and Therapy » Volume 17
Efficacy and Safety of Ciprofol for Sedation/Anesthesia in Patients Undergoing Hysteroscopy: A Randomized, Parallel-Group, Controlled Trial
Authors Lan H, Shan W, Wu Y, Xu Q , Dong X, Mei P, Duan G , You M, Jin L, Wu J
Received 25 March 2023
Accepted for publication 2 June 2023
Published 11 June 2023 Volume 2023:17 Pages 1707—1717
DOI https://doi.org/10.2147/DDDT.S414243
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Haiyan Lan, Weifeng Shan, Yini Wu, Qiaomin Xu, Xiaoli Dong, Peiyi Mei, Gongchen Duan, Minji You, Linfei Jin, Jimin Wu
Department of Anesthesiology, Lishui City People’s Hospital, The Sixth Affiliated Hospital of Wenzhou Medical University, Lishui, People’s Republic of China
Correspondence: Jimin Wu, Department of Anesthesiology, Lishui City People’s Hospital, The Sixth Affiliated Hospital of Wenzhou Medical University, No. 15, Dazhong Street, Lishui, Zhejiang Province, 323000, People’s Republic of China, Email [email protected]
Objective: To compare the efficacy and safety of ciprofol and propofol for sedation during hysteroscopy.
Methods: A total of 149 patients undergoing hysteroscopy were randomly assigned to a ciprofol (Group C) or propofol group (Group P). All cases received intravenous sufentanil 0.1 μg/kg for analgesic preconditioning. Group C received an induction dose of ciprofol 0.4 mg/kg and a maintenance dosage of 0.6– 1.2 mg/kg/h to maintain BIS value between 40– 60. In Group P, propofol was started at 2.0 mg/kg and then maintained at 3.0– 6.0 mg/kg/h. The primary outcome was the successful rate of hysteroscopy. Secondary outcomes included the change of hemodynamic, respiratory adverse events, injection pain, body movement, recovery time, anesthetist’s satisfaction, time of disappearance of the eyelash reflex and the incidence of nausea and vomiting.
Results: The success rate of hysteroscopy in each group was 100%. After drug administration, the incidence of hypotension in Group C was much lower than that in Group P (P< 0.05). The incidence of respiratory adverse events in Group C (4.0%) was much lower than that in Group P (31.1%) (P< 0.05). The incidence of injection pain and body movement in Group C was significantly lower than that in Group P (P< 0.05). The mean eyelash reflex disappearance time was less than 3 minutes in both groups. There was no statistically significant difference between the two groups in awakening times, anesthetist’s satisfaction and the incidence of nausea and vomiting. No serious adverse events occurred in any patients.
Conclusion: Ciprofol proved to be a safer alternative to propofol for anesthesia during hysteroscopy. In comparison to propofol, ciprofol does not cause injection pain, exerts less impact on hemodynamics, and results in less respiratory depression.
Keywords: ciprofol, propofol, sedation, anesthesia, hysteroscopy
Introduction
Hysteroscopy is the most common procedure in minimally invasive gynecological techniques for the diagnosis and treatment of endometrial and other intrauterine diseases.1 Despite the short duration of surgery, the intense pain associated with cervical dilation and endometrial curettage is excruciating,2–4 and patients’ fear and anxiety about pain require anesthetic intervention in most cases.5,6 General anesthesia, paracervical block, and local anesthesia can be used for hysteroscopy.7 Among these techniques, propofol combined with opioid intravenous anesthesia is used most commonly for hysteroscopic surgery.8 This approach provides good sedation and analgesic effects for patients and also greatly reduces patients’ anxiety and improves their comfort.
Propofol has a rapid onset of action and short duration, and is associated with complete awakening and high patient comfort, making it suitable for outpatient surgery;9,10 therefore, propofol has become the first choice for hysteroscopic procedures. However, propofol also has disadvantages, such as marked hemodynamic effects, respiratory depression, and painful intravenous administration.11 Therefore, identification of the ideal sedative drug in hysteroscopic surgery remains crucial.
Ciprofol (HSK 3486) is a novel 2,6 disubstituted phenol derivative that binds more tightly to the γ-aminobutyric acid type A receptor compared with propofol.12 A Phase I study involving healthy Chinese participants showed that 0.4–0.9 mg/kg of ciprofol was well tolerated, with rapid onset of action and fast recovery.13 The results of a Phase II clinical trial that investigated the efficacy and safety of ciprofol in colonoscopy showed that ciprofol was administered at a dose of only one-quarter to one-fifth that of propofol. Additionally, ciprofol had minimal residual effects and did not cause significant pain at the injection site.14 Another trial of ciprofol in mechanically ventilated patients in the intensive care unit (ICU) determined the sedative effects and safety of ciprofol for this patient group.15
The current trial was designed to confirm the efficacy and safety of ciprofol versus propofol during hysteroscopy, in the hope of providing a new safe and effective sedative drug for hysteroscopy.
Methods
Ethics and Registration
This trial was performed in accordance with the Declaration of Helsinki and the Chinese Clinical Trial Specifications, and the study is registered in the Chinese Clinical Trial Registry in 29/11/2021 (www.chictr.org.cn; registration number: ChiCTR2100053768). The study was approved by the Medical Ethics Committee of Lishui People’s Hospital (approval No. LLW-FO-401), and all enrolled patients provided signed informed consent.
Patient Inclusion and Exclusion Criteria
The participants in this prospective study were 150 women scheduled to undergo hysteroscopic examination and therapeutic surgery under total intravenous anesthesia from December 2021 to May 2022. The inclusion criteria were as follows: patients aged 18–70 years, American Society of Anesthesiologists (ASA)16 physical status I or II, and body mass index of 18–30 kg/m2. Patients with a history of allergy to study anesthetic drugs, renal or liver diseases or other systemic complications before the operation, mental disorders, communication difficulties, respiratory difficulties, or recent respiratory infections were excluded. A patient was excluded if the procedure lasted more than 60 min or if anesthesia was escalated to tracheal intubation and general inhalational anesthesia.
Randomization and Masking
Patients were randomized at a 1:1 ratio to be assigned to the ciprofol group (Group C) or the propofol group (Group P) by an independent anesthesiologist who was involved only in randomization, using a computer-generated random number table by SPSS 25.0 software (IBM Corp., Armonk, NY). Randomized results were sealed in sequentially numbered envelopes until the end of the study.
Allocation concealment was ensured by the participation of an independent nurse who was not involved in data collection or analysis. Both ciprofol and propofol are white emulsions and are coded with a number, therefore, the patients and the investigator who was responsible for postoperative follow-up and data processing, did not know the group assignment throughout the study period.
Technique
All patients were routinely fasted for more than 8 h and were not allowed to drink water for at least 2 h before the surgery. No medications were taken before the operation. Upper extremity venous access was achieved in the preoperative preparation room. Upon arrival in the operating room, the Bene View T15 monitor (Mindray Biomedical Electronics Co., Shenzhen, China) was connected to monitor the electrocardiogram, noninvasive blood pressure (including systolic blood pressure (SBP) and diastolic blood pressure (DBP)), peripheral oxygen saturation (SpO2), and heart rate (HR). Prophylactic oxygen (4 L/min) was provided using a suitable face mask during the operation. Patients were also monitored with a bispectral index (BIS) sensor (ConView YY-106, Pearlcare, Zhejiang, China) positioned on the forehead. BIS values between 40 and 60 reflect adequate hypnotic effects of general anesthesia, with reasonably rapid recovery of consciousness.
All anesthesia was administered by a board-certified anesthesiologist and all procedures were performed by the same group of experienced gynecologists.
The following evaluation time points were used:
After surgery, the patients were transferred to the post-anesthesia care unit for close monitoring until their discharge; standard monitoring comprised mean arterial pressure (MAP), HR, and SpO2 values. Patients were discharged to the general ward when their Aldrete score was at least 9.17
Grouping and Intervention
Both groups received sufentanil citrate (Yichang Humanwell Pharmaceutical Co., Ltd., Yichang, China) at 0.1 μg/kg intravenously for analgesia before the start of hysteroscopy. All patients in Group C received an induction dose of 0.4 mg/kg ciprofol (Haisco Pharmaceutical Group Co., Ltd., Liaoning, China) over a time period of 30s and a maintenance dosage of 0.6–1.2 mg/kg/h by continuous intravenous infusion to maintain BIS value between 40–60 until the end of surgery. All patients in Group P received an induction dose of 2.0 mg/kg propofol (Fresenius Kabi AG, Graz, Austria) over a time period of 30s. The propofol infusion rate was maintained at a dosage of 3.0–6.0 mg/kg/h18 to keep the sedation. When the BIS value was < 60 and the eyelash reflex was completely lost, hysteroscopy was started.
In the case of body movement that affected the operation, propofol 0.5 mg/kg/time was added in Group P and ciprofol 0.1 mg/kg/time was added in Group C. If the depth of sedation was insufficient (BIS value > 60), the patients received intravenous injection of propofol 0.5mg/kg/time in group P and ciprofol 0.1 mg/kg/time in group C until the BIS value was maintained at 40–60.
When adverse hemodynamic events, namely, hypotension (SBP < 90 mmHg, DBP < 50 mmHg, or mean arterial pressure (MAP) decrease of ≥ 20% below baseline.) or bradycardia (HR < 50 beats per minute or a decrease in HR of ≥ 20% from the baseline value) occurred during the procedure, ephedrine or atropine was administered for treatment. If respiratory depression occurred, as indicated by an Sp02 value < 90% or respiratory rate < 8 breaths/min for more than 1 min, or airway obstruction or apnea, mandibular elevation or mechanical ventilation was performed.
Outcomes
Primary Outcome
The primary outcome was the success rate of hysteroscopy, defined by the following criteria:
- Completion of hysteroscopy;
- BIS ≤ 60 after administration of a study drug (up to five top-up doses); and
- No need to change sedatives.
Secondary outcomes
The secondary outcomes included the change of hemodynamic, respiratory adverse events, injection pain, body movement, recovery time, anesthetist’s satisfaction, time of disappearance of the eyelash reflex and the incidence of nausea and vomiting. Injection pain referred to the pain reported verbally by patients after the first injection. Body movement was defined as visible limbs bending or head movement during the hysteroscopy. Recovery time referred to the time from the last drug administration to awakening.
A respiratory adverse event was defined as desaturation (SpO2 < 95%) or requiring airway intervention; airway intervention comprised chin-lift/jaw-thrust maneuvers, increased O2 flow, and assisted ventilation.
Changes in blood pressure (SBP, DBP, MAP (MAP = (SBP + 2 × DBP)/3)), HR, SPO2, and BIS values were continuously monitored from the start of administration of a study drug to the end of surgery. Hypotension was defined as follows: SBP < 90 mmHg, DBP < 50 mmHg, or mean arterial pressure (MAP) decrease of ≥ 20% below baseline. Hypertension was defined as follows: SBP > 180 mmHg, DBP > 110 mmHg, or a MAP increase of ≥ 20% compared with the baseline value. Bradycardia was defined as follows: HR < 50 beats per minute or a decrease in HR of ≥ 20% from the baseline value. Tachycardia was defined as follows: HR > 100 beats per minute or an increase in HR of ≥ 20% of the baseline value.
Sample Size and Statistical Analysis
The sample size was assessed using NCSS-PASS software version 15.0. According to previous literature, the success rate of colonoscopy in the 2.0mg/kg propofol was 97% and 100% in the ciprofol 0.4–0.5mg/kg.14 We assumed that the success rates of hysteroscopy in 0.4mg/kg ciprofol would be 97%. The noninferiority cut-off value was 10%, a one-sided type I error rate of 2.5%, a power of 90%, and considering possible losses of 20%, each group comprised a cohort of 75 patients.
Statistical analysis was performed using SPSS Statistics 25.0 (IBM Corp., Armonk, NY). The Shapiro–Wilk test was applied to determine whether continuous variables were normally distributed. Normally distributed continuous variables were expressed as the mean ± standard deviation, and these data were analyzed using Student’s t-test. The Mann–Whitney U-test was used to analyze non-normally distributed continuous variables. Hemodynamic parameters were compared by repeated measures analysis of variance. Categorical variables were expressed as frequency (percentage) and analyzed using Pearson’s chi-square test. The Wilcoxon signed-rank test was used to compare continuous variables. Significance was set at p< 0.05.
Results
A total of 150 patients were assessed for eligibility. One patient in the propofol group was excluded because the operation time exceeded 60 min. Therefore, data for 75 patients in Group C and 74 patients in Group P were analyzed (Figure 1).
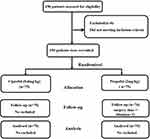 |
Figure 1 Flow diagram representing patient enrollment, group assignment, and analysis. |
Demographic Data and Surgical Characteristics
The demographic and surgical characteristics of the patients are shown in Table 1. The characteristics of the patients in the two groups were similar, and age, height, weight, body mass index, and ASA physical status were statistically similar between the groups (P> 0.05). There were no significant differences in the duration of the procedure, awakening time and anesthesiologists’ satisfaction between the groups. The disappearance time of the eyelash reflex in Group C (1.4 ± 0.9 min) was significantly longer than that of Group P (1.2 ± 0.5 min) (p< 0.05).
 |
Table 1 Demographic Characteristics and Clinical Data for Each Group |
Primary Efficacy Outcome for the Study Drug
The success rate of hysteroscopy in both groups was 100% (Table 2). Successful hysteroscopy was performed in all patients without the use of alternative sedative drugs. Changes in BIS values were recorded to evaluate the objective level of sedation (Figure 2). Generally, the pattern of sedation level changes elicited by ciprofol was comparable to that with propofol. The BIS values of the ciprofol and propofol groups decreased rapidly after drug administration. This result indicated that 0.4mg/kg doses of ciprofol were non-inferior to 2.0mg/kg doses of propofol for successful sedation/anesthesia.
 |
Table 2 Sedation-Related Outcomes |
 |
Figure 2 BIS values at different time intervals. |
Changes in Circulation
SBP, DBP, MAP, and HR values at each time point are shown in Figure 3. Baseline blood pressure and HR were comparable between the groups. After sedative administration, SBP, DBP, MAP, and HR in both groups decreased significantly compared with the baseline values (P< 0.05). However, SBP, DBP, and MAP values in Group P were significantly lower than those in Group C at T2, T3, and T4, whereas HR in both groups was comparable at all time points. Generally, blood pressure reached a nadir 2 min after administration (T2), followed by a small increase in SBP, DBP, and MAP, in both groups. Both groups showed the same change in trends for SBP, DBP, MAP, and HR during the monitoring.
Respiratory Events
During the surgical process, three patients in group C had respiratory adverse events, two of whom required airway intervention and two of whom had decreased oxygen saturation (SpO2 <95%). In group P, 23 patients experienced respiratory adverse events, 17 of whom required airway intervention and 10 of whom experienced a decrease in oxygen saturation (p< 0.05). Nonetheless, no patients required tracheal intubation or a change in the anesthesia plan. Compared with Group P, Group C patients experienced less respiratory depression.
Adverse Events
There were no serious adverse events or deaths in either group (Table 3). Injection pain was the most common adverse event in Group P (27.0%), but this adverse event did not occur in Group C (p< 0.05). The incidence of body movements in Group P was much higher than that in Group C (59.5% vs 33.3%, respectively; p< 0.05), and movements manifested as slight body movements, such as visible limb bending or head movement. However, these movements did not affect the operation.
 |
Table 3 Adverse Events |
Discussion
This trial demonstrated that ciprofol 0.4 mg/kg was non-inferior to 2.0 mg/kg propofol in the success rate of hysteroscopy. The incidence of injection pain in the ciprofol group was significantly reduced, and there were fewer incidents of respiratory problems compared to propofol group. Additionally, the hemodynamics were more stable in the ciprofol group. Our results indicate that ciprofol is a promising sedative with advantages in hysteroscopy.
Propofol has been the commonly used intravenous anesthetic drug for the induction and maintenance of anesthesia and sedation of patients, due to its fast onset, fast clearance, and rapid patient recovery. However, there are some unavoidable limitations to propofol, such as injection pain, suppression of circulatory function, and respiratory depression. Ciprofol is a close analog of propofol which binds more tightly to the γ-aminobutyric acid type A receptor. Previous Phase I–III clinical trials have reported that the potency of ciprofol is approximately five times that of propofol which means only 20% of a ciprofol dose was needed to achieve the same anesthetic effect as propofol.13,14,19 In the phase IIb trial, the success rate of colonoscopy in the ciprofol 0.4 mg/kg was 100% and 96.8% in the propofol 2.0 mg/kg group.14 Thus, this trial used 2.0mg/kg propofol and 0.4mg/kg ciprofol during induction. In this study, the objective index, the BIS value, was selected to monitor the depth of anesthesia. In accordance with a phase I clinical study, the change trend of the Richmond Agitation-Sedation Scale was consistent with the BIS values.19 We chose to maintain the BIS value at < 60 intraoperatively to ensure that the patient was at the appropriate depth of sedation during hysteroscopy. A previous multicenter Phase III clinical trial in China showed that the pattern of sedation level changes elicited by ciprofol was comparable to that of the propofol group, which is consistent with our findings.20 All patients in two groups were successfully sedated, and no remedial drugs were used. The average eyelash reflex disappearance time in group C was longer than that in group P, with statistical significance (1.4 ± 0.9 vs 1.2 ± 0.5 min; P= 0.024), but both groups had an eyelash reflex disappearance time of less than 3 minutes. Therefore, we believe that this difference has no significant clinical significance. Our study reconfirmed that ciprofol can rapidly provide sufficient depth of sedation and rapid patient recovery and can become a good choice for hysteroscopic procedures.13,14,20–22
A previous phase I–III clinic study both demonstrated that ciprofol resulted in slightly less respiratory depression compared with propofol.13–15,19,21,23 Based on this study, it was found that ciprofol was associated with less respiratory depression and a lower proportion of airway interventions and desaturation during sedation, compared to propofol. The anesthesiologists took appropriate airway intervention measures, such as chin lift/jaw thrust, increased O2 flow, and assisted ventilation, when they observed significant airway obstruction or respiratory arrest during surgery. As a result, 10 patients in the propofol group developed hypoxia, but 17 patients required airway intervention. It is worth noting that neither group required mechanical ventilation or tracheal intubation. Since respiratory depression is a critical issue during sedation anesthesia, the lower incidence of respiratory depression associated with ciprofol makes it a potentially safer option than propofol for hysteroscopic procedures.
In this study, the incidence of hypotension was lower in the ciprofol group compared to the propofol group, and the decrease in blood pressure was also significantly smaller in the ciprofol group, indicating that ciprofol has a smaller impact on blood pressure compared to propofol, resulting in a more stable hemodynamic profile throughout the anesthesia process. Patients in the ciprofol group had a certain degree of decrease in heart rate during hysteroscopy, but the changes were relatively stable and did not require special treatment. In contrast, patients in the propofol group had a relatively higher heart rate, which may be related to changes in blood pressure between the two groups, as patients in the propofol group exhibited a more significant decrease in blood pressure, which could reflexively cause an increase in heart rate. Considering all factors, ciprofol may be a better choice than propofol as an anaesthetic, due to its minimal impact on blood pressure, with a more stable hemodynamic changes during anesthesia.
Injection pain is one of the most common adverse effects of propofol administration. This pain is related to the aqueous concentration of propofol, which causes discomfort, increased patient distress and anxiety, and leads to body movements that can prevent smooth completion of hysteroscopy.24–26 The reported incidence of propofol injection pain varies widely, ranging from 30% to 70%.24 In the present study, we found that the incidence of injection pain in the propofol group was much higher than that in the ciprofol group (27.0% vs 0.0%, respectively; p< 0.001), which is consistent with the results of a previous multicenter phase II clinical trial in China.14 This difference may be because of the lower concentration in the aqueous phase that is provided by the higher potency of ciprofol compared with propofol. Furthermore, in our study, no injection pain was observed in the ciprofol, which is a lower incidence than that reported in the literature, probably mainly due to the preoperative use of sufentanil in our study.
There were obvious limb bending or head movements in both groups during the operation, which were more common in group P than group C, but these movements did not hinder the operation. Inadequate intraoperative analgesia and pain caused by surgical stimulation may cause involuntary movement. The study used a single intravenous injection of sufentanil for intraoperative analgesia, but its effect decreased over time, and no additional doses were administered during the operation. In previous studies, continuous intravenous infusion of remifentanil was used for pain control.27 Therefore, depending on the intraoperative body movements, it may be more suitable for hysteroscopic analgesia with intravenous infusion. The lower incidence of involuntary movement of ciprofol compared with propofol may be due to the fact that ciprofol provides deeper sedation than propofol during maintenance.
Our study first confirmed the effectiveness and safety of ciprofol for sedation in hysteroscopy. But the following limitations still need to be considered in our study. Firstly, we included only low‐risk patients (ASA class I and II) in this study. Secondly, our patient observation was limited to the period from sedation administration to the recovery room, with no long-term postoperative follow-up observation. Thirdly, maintaining the BIS value at 40–60 may result in excessive sedation during hysteroscopic surgery. In Western countries, moderate sedation is the target level of sedation for hysteroscopy patients, while most sedation procedures are performed under deep sedation in China. Finally, this is a single-center study with a small sample size.
Therefore, there is still a need for large multicenter trials to substantiate our findings and further investigate the efficacy, safety, and applicability of ciprofol in high-risk populations.
Conclusions
In this study, it has been shown that Ciprofol is a safer alternative to propofol for anesthesia during hysteroscopy. Compared with propofol, Ciprofol does not cause injection pain, has less impact on hemodynamics, and leads to less respiratory depression.
Data Sharing Statement
The original data analyzed in this study are included in the article; further inquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This trial was performed in accordance with the Declaration of Helsinki and the Chinese Clinical Trial Specifications. The study was approved by the Medical Ethics Committee of Lishui People’s Hospital (approval No. LLW-FO-401), and was registered in the Chinese Clinical Trial Registry in 29/11/2021 (www.chictr.org.cn; registration number: ChiCTR2100053768). Written informed consent was obtained from all participants. The study protocol followed the CONSORT guidelines. The study protocol was performed in the relevant guidelines.
Acknowledgments
We thank the patients who participated in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Beijing Health Alliance Charitable Foundation (S100).
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Sutton C. Hysteroscopic surgery. Best practice & research. Clin Obstetr Gynaecol. 2006;20(1):105–137.
2. Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17(6):703–708. doi:10.1016/j.jmig.2010.07.003
3. Carta G, Palermo P, Marinangeli F, et al. Waiting time and pain during office hysteroscopy. J Minim Invasive Gynecol. 2012;19(3):360–364. doi:10.1016/j.jmig.2012.01.017
4. Amer-Cuenca JJ, Marín-Buck A, Vitale SG, et al. Non-pharmacological pain control in outpatient hysteroscopies.. Minim Invasive Ther Allied Technol. 2020;29(1):10–19. doi:10.1080/13645706.2019.1576054
5. Gupta JK, Clark TJ, More S, et al. Patient anxiety and experiences associated with an outpatient “one-stop” “see and treat” hysteroscopy clinic. Surg Endosc. 2004;18(7):1099–1104. doi:10.1007/s00464-003-9144-3
6. Vitale SG, Caruso S, Ciebiera M, et al. Management of anxiety and pain perception in women undergoing office hysteroscopy: a systematic review. Arch Gynecol Obstet. 2020;301(4):885–894. doi:10.1007/s00404-020-05460-2
7. Hassan L, Gannon MJ. Anaesthesia and analgesia for ambulatory hysteroscopic surgery. Best practice & research. Clin Obstetr Gynaecol. 2005;19(5):681–691.
8. Yu J, Xiang B, Song Y, et al. ED50 of propofol in combination with low-dose sufentanil for intravenous anaesthesia in hysteroscopy. Basic Clin Pharmacol Toxicol. 2019;125(5):460–465. doi:10.1111/bcpt.13280
9. Avramov MN, White PF. Use of alfentanil and propofol for outpatient monitored anesthesia care: determining the optimal dosing regimen. Anesth Analg. 1997;85(3):566–572. doi:10.1213/00000539-199709000-00015
10. Bingol Tanriverdi T, Koceroglu I, Devrim S, et al. Comparison of sedation with dexmedetomidine vs propofol during hysteroscopic surgery: single-centre randomized controlled trial. J Clin Pharm Ther. 2019;44(2):312–317. doi:10.1111/jcpt.12793
11. Marik PE. Propofol: therapeutic indications and side-effects. Curr Pharm Des. 2004;10(29):3639–3649. doi:10.2174/1381612043382846
12. Qin L, Ren L, Wan S, et al. Design, synthesis, and evaluation of novel 2,6-disubstituted phenol derivatives as general anesthetics. J Med Chem. 2017;60(9):3606–3617. doi:10.1021/acs.jmedchem.7b00254
13. Teng Y, Ou MC, Wang X, et al. Pharmacokinetic and pharmacodynamic properties of ciprofol emulsion in Chinese subjects: a single center, open-label, single-arm dose-escalation Phase 1 study. Am J Transl Res. 2021;13(12):13791–13802.
14. Teng Y, Ou M, Wang X, et al. Efficacy and safety of ciprofol for the sedation/anesthesia in patients undergoing colonoscopy: phase IIa and IIb multi-center clinical trials. Eur J Pharma Sci. 2021;164:105904. doi:10.1016/j.ejps.2021.105904
15. Liu Y, Chen C, Liu N, et al. Efficacy and safety of ciprofol sedation in ICU patients with mechanical ventilation: a clinical trial study protocol. Adv Ther. 2021;38(10):5412–5423. doi:10.1007/s12325-021-01877-6
16. Doyle DJ, Goyal A, Garmon EH. American society of anesthesiologists classification. In: StatPearls. Treasure Island (FL): StatPearls PublishingCopyright © 2022, StatPearls Publishing LLC; 2022.
17. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49(6):924–934. doi:10.1213/00000539-197011000-00020
18. Zhang S, Wang J, Ran R, et al. Efficacy and safety of remimazolam tosylate in hysteroscopy: a randomized, single-blind, parallel controlled trial. J Clin Pharm Ther. 2022;47(1):55–60. doi:10.1111/jcpt.13525
19. Hu C, Ou X, Teng Y, et al. Sedation effects produced by a ciprofol initial infusion or bolus dose followed by continuous maintenance infusion in healthy subjects: a Phase 1 trial. Adv Ther. 2021;38(11):5484–5500. doi:10.1007/s12325-021-01914-4
20. Wang X, Wang X, Liu J, et al. Effects of ciprofol for the induction of general anesthesia in patients scheduled for elective surgery compared to propofol: a Phase 3, multicenter, randomized, double-blind, comparative study. Eur Rev Med Pharmacol Sci. 2022;26(5):1607–1617. doi:10.26355/eurrev_202203_28228
21. Wu B, Zhu W, Wang Q, et al. Efficacy and safety of ciprofol-remifentanil versus propofol-remifentanil during fiberoptic bronchoscopy: a prospective, randomized, double-blind, non-inferiority trial. Front Pharmacol. 2022;13:1091579. doi:10.3389/fphar.2022.1091579
22. Zeng Y, Wang DX, Lin ZM, et al. Efficacy and safety of HSK3486 for the induction and maintenance of general anesthesia in elective surgical patients: a multicenter, randomized, open-label, propofol-controlled Phase 2 clinical trial. Eur Rev Med Pharmacol Sci. 2022;26(4):1114–1124. doi:10.26355/eurrev_202202_28101
23. Liu Y, Yu X, Zhu D, et al. Safety and efficacy of ciprofol vs propofol for sedation in intensive care unit patients with mechanical ventilation: a multi-center, open label, randomized, phase 2 trial. Chin Med J. 2021;135(9):1043–1051.
24. Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia. 1998;53(5):468–476. doi:10.1046/j.1365-2044.1998.00405.x
25. Doenicke AW, Roizen MF, Rau J, et al. Reducing pain during propofol injection: the role of the solvent. Anesth Analg. 1996;82(3):472–474. doi:10.1097/00000539-199603000-00007
26. Klement W, Arndt JO. Pain on injection of propofol: effects of concentration and diluent. Br J Anaesth. 1991;67(3):281–284. doi:10.1093/bja/67.3.281
27. Zhang X, Li S, Liu J. Efficacy and safety of remimazolam besylate versus propofol during hysteroscopy: single-centre randomized controlled trial. BMC Anesthesiol. 2021;21(1):156. doi:10.1186/s12871-021-01373-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

