Back to Journals » Drug Design, Development and Therapy » Volume 17
Efficacy and Prognostic Factors of Regorafenib in the Treatment of BCLC Stage C Hepatocellular Carcinoma After Failure of the First-Line Therapy
Authors Xu B, Lu D, Liu K , Lv W, Xiao J, Zhang X, Zhang Z, Chai J, Wang L
Received 7 December 2022
Accepted for publication 4 February 2023
Published 16 February 2023 Volume 2023:17 Pages 507—518
DOI https://doi.org/10.2147/DDDT.S400533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Beibei Xu,1 Dong Lu,1,2 Kaicai Liu,3 Weifu Lv,2 Jingkun Xiao,2 Xingming Zhang,2 Zhengfeng Zhang,2 Jie Chai,2 Lijun Wang2
1School of Graduate, Bengbu Medical College, Bengbu, 233030, People’s Republic of China; 2Department of Interventional Radiology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, 230001, People’s Republic of China; 3Infection Hospital, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, 230000, People’s Republic of China
Correspondence: Dong Lu, Department of Interventional Radiology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, No. 17, Lujiang Road, Hefei, Anhui, 230001, People’s Republic of China, Tel +86 18056000897, Email [email protected]
Purpose: Regorafenib is a standard second-line treatment for hepatocellular carcinoma (HCC). This study aimed to evaluate the efficacy and safety of regorafenib in the treatment of patients with Barcelona clinic liver cancer (BCLC) stage C HCC after failure of the first-line therapy and to analyze factors affecting the efficacy of regorafenib as the second-line treatment.
Methods: A retrospective analysis was conducted on 103 BCLC stage C HCC patients who received regorafenib as the second-line treatment. Among them, 51 patients received regorafenib plus transarterial chemoembolization (TACE) and 52 patients received regorafenib alone. Progression-free survival (PFS), overall survival (OS), and adverse events were compared between the two groups, and factors influencing the efficacy of regorafenib were analyzed.
Results: In patients with BCLC stage C HCC after failure of the first-line therapy, there was no statistically significant difference in median PFS between regorafenib plus TACE group and regorafenib group (5.3 vs 4.0 months, P=0.432). The median OS was significantly longer in the regorafenib plus TACE group than that in the regorafenib group (11.3 vs 8.2 months, P=0.034). Patients in both groups experienced adverse events at rates of 78.43% and 75%, respectively. Rates of grade III–IV serious adverse events were 19.61% and 13.46%, respectively. Hand-foot skin reactions, fatigue, abdominal pain, and hypertension were common side effects of regorafenib. The number of tumors was noted as an independent prognostic factor for PFS in the univariate and multivariate Cox regression analyses, while Eastern Cooperative Oncology Group (ECOG) performance status (ECOG-PS) score, tumor size, the number of tumors, and combined local therapy were independent prognostic factors for OS. Regorafenib combined with TACE treatment improved OS for patients with ECOG-PS scores of 0– 1, tumor size < 5 cm, and the number of tumors ≥ 3 compared with regorafenib alone.
Conclusion: Regorafenib exhibited to be a safe and effective sequential therapy for patients with BCLC stage C HCC after failure of the first-line treatment, and its combination with TACE could achieve a higher efficacy. ECOG-PS score, tumor size, the number of tumors, and combined local therapy were noted as prognostic factors affecting patients with BCLC stage C HCC who were treated with regorafenib.
Keywords: regorafenib, hepatocellular carcinoma, TACE, efficacy, prognostic factors
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer, the third leading cause of cancer-related deaths worldwide, and the second leading cause of deaths in China.1,2 Due to the insidious onset and inconspicuous early symptoms, the majority of patients are diagnosed at the intermediate-to-late stage. In addition, patients with early-stage HCC have a high recurrence rate after surgical resection and are prone to metastasis.3 However, the prognosis of patients with advanced liver cancer is poor, and it is particularly important to select the appropriate treatment to improve the prognosis.
Transarterial chemoembolization (TACE) plays an important role in the clinical treatment of advanced HCC.4,5 TACE can block the blood supply arteries of tumor tissue, increase the concentration of local chemotherapeutic drugs, and induce ischemic necrosis, thereby controlling the local growth of the tumor tissue. However, tumor necrosis and hypoxia also promote intra-tumor angiogenesis, which may drive tumor growth, recurrence, and metastasis.6 In recent years, the emergence of anti-angiogenic drugs for HCC is advantageous for patients with inoperable HCC. Tyrosine kinase inhibitors (TKIs), such as sorafenib, lenvatinib, and donafenib have improved the clinical efficacy of HCC and prolonged the survival time of patients with advanced HCC.7–10 Meanwhile, TACE combined with these anti-angiogenic drugs can reduce the expression level of vascular endothelial growth factor (VEGF), reduce the incidence of tumor recurrence and metastasis, and improve the efficacy of TACE.11
Regorafenib is an oral multi-kinase inhibitor that blocks a variety of protein kinases related to tumor angiogenesis, cell proliferation, tumor metastasis, and immunity.12 It has stronger anti-angiogenic and anti-tumor proliferative activities than sorafenib, and it was approved as a standard second-line treatment for HCC.13 The majority of patients with HCC are ultimately unable to respond to first-line treatment due to tumor progression or intolerable adverse reactions, thus, safer and more effective second-line drugs are recommended to control disease progression. At present, it is suggested to provide more data related to the modality and efficacy of subsequent treatment for patients who failed in the first-line treatment. The present study aimed to evaluate the efficacy and safety of regorafenib in patients with Barcelona clinic liver cancer (BCLC) stage C HCC after failure of the first-line treatment.
Materials and Methods
Patients
A retrospective analysis was conducted on patients with BCLC stage C HCC who received regorafenib as a second-line therapy at the First Affiliated Hospital of the University of Science and Technology of China (Hefei, China) from August 2019 to May 2022. Inclusion criteria were as follows: (1) patients who aged ≥18 years old and were diagnosed with primary HCC according to the criteria of American Association for the Study of Liver Diseases;14 (2) patients who received first-line targeted therapy ≥20 days, while experienced failure of the therapy due to disease progression or intolerable side effects; (3) patients with BCLC stage C HCC; (4) patients with Child-Pugh class A or B; (5) Eastern Cooperative Oncology Group (ECOG) performance status (PS) score of 0–2; (6) patients undergoing at least one cycle of regorafenib therapy; and (7) patients with at least one measurable lesion according to the modified Response Evaluation Criteria in Solid Tumors (mRECIST).15 Exclusion criteria were as follows: (1) incomplete clinical date; (2) complication with other serious cardiovascular or hepatic or renal diseases; (3) patients with other concurrent malignancies; and (4) patients receiving local treatment of the liver other than TACE after starting regorafenib therapy; (5) Patients who cannot tolerate sorafenib treatment (serious adverse events ≥ grade 3). Totally, 103 patients were enrolled, of whom 52 patients were treated with regorafenib alone and 51 patients were treated with TACE plus regorafenib therapy (Figure 1).
 |
Figure 1 Flow diagram illustrating the treatment process. |
Ethics Approval
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China (Approval No. 2022-RE-351). The study was conducted in accordance with the Declaration of Helsinki. All treatments were initiated with patients’ consent. As this was a retrospective study, the research content was scientific and the subjects’ risks and benefits were reasonable, the Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China waived the requirement to obtain written informed consent from patients. All patient information is confidential.
Treatment
All patients received regorafenib (Bayer AG, Leverkusen, Germany) during second-line treatment. Patients received 160 mg (4 tablets of 40 mg) regorafenib orally daily for the first three weeks of each 4-week cycle until tumor progression, and patient death or serious adverse events (AEs) were recorded. The dose could be reduced (120 or 80 mg daily) or interrupted according to the physicians’ prescription when the side effects were intolerable. All patients received at least one course of regorafenib.
Patients in the regorafenib plus TACE group were treated with TACE as required within one week prior to or during oral regorafenib after failure of the first-line therapy. TACE was performed using the modified Seldinger technique. First, patients underwent abdominal and superior mesenteric arteriography to identify the location of the tumor and its feeding arteries. A microcatheter (ProgreatTM, Terumo, Tokyo, Japan) was used to perform superselective cannulation of segmental or subsegmental hepatic artery branches feeding the tumor, and then, iodinated oil emulsion loaded with doxorubicin or platinum-based chemotherapeutic agents was injected. Depending on the abundance of tumor blood supply, granular embolic agents, such as polyvinyl alcohol (PVA) or gelatin sponges were used to embolize the tumor supply arteries if necessary. The frequency and interval of TACE were determined by the imaging tumor evaluation and the patient’s liver functional status.
Data Collection
The primary endpoint was overall survival (OS), which was defined as the time from initiation of regorafenib treatment to death from any cause or to the last follow-up visit. The secondary endpoint was progression-free survival (PFS), which was defined as the time from initiation of regorafenib to the first progression or death from any cause before disease progression. The severity of AEs was graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0.16 Factors potentially associated with survival time included treatment modality, ECOG-PS score, alpha-fetoprotein (AFP) level, Child-Pugh class, albumin-bilirubin (ALBI) grade, tumor status, vascular invasion, and extrahepatic metastasis. Fever, abdominal pain, nausea, and vomiting occurring within 2 weeks of TACE were considered as post-embolization syndrome and were not recorded as regorafenib-related AEs. All data were obtained through outpatient visits, medical record systems, and telephone follow-up. The follow-up deadline was September 30, 2022.
Statistical Analysis
SPSS 22.0 software (IBM, Armonk, NY, USA) was used to perform statistical analysis. The Shapiro-wilk test was used to test the normality of the data distribution. Continuous variables conforming to normal distribution were expressed as mean ± standard deviation (SD), abnormally distributed data were expressed as median (range), and categorical variables were presented as frequency and proportion. Two groups of data were compared using the independent-samples t-test, Mann–Whitney U-test, χ2 test or Fisher’s exact test. Kaplan-Meier curve was used for survival analysis, and Log rank test was used for making comparison. To assess prognostic factors affecting PFS and OS, univariate and multivariate logistic regression analyses were performed using Cox proportional-hazards models. All statistical tests were two-sided, and P<0.05 was statistically significant.
Results
Patients’ Characteristics
A total of 103 patients with BCLC stage C HCC were enrolled in this study. Table 1 summarizes patients’ baseline data before regorafenib treatment. There were no significant differences between the two groups in terms of age, gender, ECOG-PS score, AFP level, Child-Pugh score, ALBI grade, vascular invasion, tumor size, number of tumors, extrahepatic metastasis, and first-line targeted immunotherapy (P > 0.05). In the regorafenib plus TACE group, 14 patients were combined with Camrelizumab, 2 with Tislelizumab, 2 with Toripalimab, and 2 with Pembrolizumab. In the regorafenib group, 19 patients were combined with Camrelizumab, 2 with Tislelizumab, 3 with Toripalimab, and 1 with Pembrolizumab. The number of patients receiving TACE in the regorafenib plus TACE group was slightly higher than that in the regorafenib group (94.12% vs 78.85%, P=0.024), and the number of pre-second-line TACE treatments was also different between the two groups (P=0.014). During second-line treatment, patients in the regorafenib plus TACE group received 1–5 courses of TACE as needed, with an average of 1.63 times. Median treatment time was 5.5 months in the regorafenib plus TACE group and 5.0 months in the regorafenib group, and there was no difference in the duration of regorafenib treatment between the two groups (P=0.191).
 |
Table 1 Baseline Characteristics of Patients Treated with Regorafenib |
Treatment Efficacy
The median second-line PFS was 4.3 months (95% confidence interval (CI): 3.5–5.1), and the median second-line OS was 9.8 months (95% CI: 7.8–11.8) for all patients. The median second-line PFS was 5.3 months (95% CI: 4.4–6.2) in the regorafenib plus TACE group and 4.0 months (95% CI: 3.8–4.2) in the regorafenib group (P=0.432, Figure 2A). Second-line OS was 11.3 months (95% CI: 9.1–13.5) in the regorafenib plus TACE group and 8.2 months (95% CI: 6.3–10.1) in the regorafenib group (P=0.034, Figure 2B).
 |
Figure 2 Kaplan–Meier curve of (A) progression-free survival (PFS), and (B) overall survival (OS). |
Prognostic Factors Affecting PFS and OS
In univariate analysis, age and the number of tumors were influential factors for PFS. The multivariate Cox regression analysis showed that the number of tumors was independently associated with PFS, as shown in Table 2. For OS, the univariate analysis revealed that ECOG-PS score, Child-Pugh class, ALBI grade, portal vein tumor thrombosis (PVTT), tumor size, number of tumors, and combined local therapy therapy might influence it, and the multivariate analysis demonstrated that ECOG-PS score, tumor size, the number of tumors, and combined local therapy were independent prognostic factors (Table 3).
 |
Table 2 Univariate and Multivariate Cox Regression Analyses of PFS |
 |
Table 3 Univariate and Multivariate Cox Regression Analyses of OS |
Subgroup Analysis of OS
Based on the results of multivariate regression analysis of OS, subgroup analysis of OS was performed on the physical status, tumor size, and number of tumors at the start of second-line treatment in both groups (Figures 3A–F). The results showed that the efficacy of regorafenib combined with TACE was significantly better than that of regorafenib alone in patients with ECOG-PS scores of 0–1, tumor size < 5 cm, and number of tumors ≥ 3 (P < 0.05). For patients with tumor size ≥ 5 cm or number of tumors < 3, the median OS of regorafenib combined with TACE was higher than that of regorafenib alone, while there was no statistically significant difference (P > 0.05). For patients with ECOG-PS score of 2, the effects of regorafenib plus TACE therapy were comparable to regorafenib alone (7 months).
AEs
The AEs associated with regorafenib treatment are shown in Table 4. In the regorafenib plus TACE group, 32 (62.75%) patients developed post-embolization syndrome, which was basically relieved within 1–2 weeks after the procedure by supportive nursing. During the observation period, AEs with varying degrees of severity were observed in 40 (78.43%) and 39 (75%) patients in each of the two groups, with 10 (19.61%) and 7 (13.46%) patients who experienced grade ≥ 3 serious AEs. Common AEs associated with regorafenib included hand-foot skin reactions, fatigue, abdominal pain, and hypertension. A total of 7 patients were identified to permanently discontinue regorafenib due to serious AEs, including 3 patients in the regorafenib plus TACE group and 4 patients in the regorafenib group.
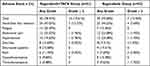 |
Table 4 Comparison of Adverse Events Related to Regorafenib Between the Two Groups |
At the end of follow-up, 34 cases were still alive. Besides, 32 (31.07%) patients were identified who discontinued regorafenib due to disease progression or AEs. In the regorafenib plus TACE group, 6 patients received lenvatinib, 4 received apatinib, 2 received donafenib, and 1 received bevacizumab in combination with immune checkpoint inhibitors (ICIs). In the regorafenib group, 12 cases received lenvatinib, 2 received apatinib, 1 received donafenib, and 4 received bevacizumab combined with ICIs.
Discussion
Advanced HCC patients with vascular invasion or extrahepatic metastases have a poor prognosis, and systemic therapies were recommended by guidelines. Sorafenib, a small molecule-targeted drug, was approved for the treatment of advanced liver cancer in 2007 and extended median survival to within 3 months (10.7 months vs 7.9 months), which revolutionized treatment for advanced HCC.7 In recent years, systemic therapies, including ICIs and TKIs have promoted the treatment of HCC and made substantial progress.17 The newly reported combination of atezolizumab (anti-programmed death-ligand 1 (PD-L1) antibody) and bevacizumab (anti-VEGF antibody) is the first regimen to improve OS in patients with unresectable HCC, achieving a PFS of 6.8 months and a median OS of 19.2 months.18 This may result in longer and more qualitative life in patients with advanced HCC.
Although there are several drugs and combination regimens for the systemic treatment of advanced HCC, studies are mainly limited to first-line therapy and drug resistance in first-line treatment is not uncommon.19 Patients who progress after first-line drug resistance and experience intolerable side effects need to change drugs or combine with other treatments to control disease progression and prolong survival. To date, the options and efficacy of second-line treatment for HCC have not been well studied, and it has still remained elusive whether combination of targeted drugs with local therapy is more effective. Considering the late stage of patients at the time of second-line treatment, the present retrospective study aimed to evaluate the efficacy and AEs of regorafenib in BCLC stage C HCC patients and to analyze the prognostic factors affecting PFS and OS.
Regorafenib is an oral multi-targeted TKI with a structure similar to sorafenib. It not only targets VEGF receptor-1, −2 and −3 (VEGFR1-3), platelet-derived growth factor receptor-β (PDGFR-β), fibroblast growth factor receptor (FGFR), tunica interna endothelial cell kinase 2 (TIE2), and the oncogenic kinases (KIT, RET, and B-RAF) to inhibit tumor angiogenesis and cell proliferation, but also acts on the tumor microenvironment and immunosuppression by modulating macrophages and CD8+ T cells.12,20,21 The RESORCE trial reported that regorafenib increased median survival from 7.8 to 10.6 months in patients who received sorafenib, significantly improving disease control rate and survival time in HCC patients after failure of the first-line therapy.22
In the present study, the median OS of HCC patients treated with regorafenib after first-line failure was 8.2 months, which was lower than 10.6 months in the RESORCE trial. This could be related to the fact that patients were all BCLC stage C in the present study, the proportions of vascular invasion and extrahepatic metastases were significantly higher than those in the RESORCE trial, and patients’ basal status was slightly worse. A longer OS was found in the regorafenib plus TACE group than that in the regorafenib group (11.3 vs 8.2 months, P=0.034), indicating that the combination of regorafenib and TACE could result in a longer survival after failure of the first-line therapy. Previous studies have shown that local TACE can control the progression of intrahepatic lesions, and the combination of targeted agents has been advocated in the treatment of intermediate stage HCC.23,24 This is because TACE can enhance tumor angiogenesis, while causing tumor necrosis and hypoxia, and the combination of these targeted drugs may inhibit the reconstruction of tumor blood circulation. Although TACE was not recommended to the majority of patients with advanced HCC,24 several recent studies have shown that TACE combined with targeted therapy could improve the survival rate of patients with advanced HCC.25–27 This may be related to the fact that TACE enhances the toxic effects of TKIs on tumor cells.28 Although local treatment of primary lesions is not the standard treatment for patients with metastatic cancer, the control of intrahepatic lesions by TACE cannot be denied, and treatment of intrahepatic tumors may also appropriately improve the prognosis of some patients.29 In addition, some studies have reported the efficacy of TACE in patients with PVTT, and pulmonary and mediastinal metastases from HCC when the role of targeted therapy is limited.30,31 In the present study, the majority of patients received TACE in the first-line treatment, while drug resistance or side effects led to weakening of the synergy and failure of the first-line therapy. At this point, the administration of regorafenib could inhibit the growth of tumor cells and blood vessels with a broader targeting effect. The median PFS and OS of patients in this study were prolonged in the regorafenib plus TACE group compared with those in the regorafenib group, while there was no statistically significant difference in PFS between the two groups, which could be related to differences in the time and number of courses of TACE or patients’ selection.
The present study revealed that the independent influential factor of PFS was the number of tumors, while the dependent influential factors of OS were ECOG-PS score, tumor size, number of tumors, and combined local treatment. The size and number of tumors are important for staging and play a key role in prognosis. Previous studies have shown that tumor size and the number of tumors are associated with long-term survival in patients with liver cancer.32,33 In addition, the patient’s physical status may be correlated with drug tolerance, and patients with good basal status may receive local treatment.
Subgroup analysis indicated that regorafenib combined with TACE treatment was more effective than regorafenib alone in patients with good physical status, tumor size <5 cm, and number of tumors ≥ 3. For patients with tumor size ≥ 5 cm or number of tumors <3, combination therapy was also resulted in a longer OS, while there was no statistically significant difference. Some studies have shown that smaller tumors can benefit more from TACE treatment and larger tumors are associated with an increased risk of death in TACE.33 The larger tumors are associated with a higher difficulty of completely inhibiting tumor growth, and patients may need to undergo multiple cycles of TACE. Repeated TACE can impair patients’ liver function, which is very detrimental to the prognosis of patients with advanced liver cancer. The mean number of TACE courses in the regorafenib plus TACE group was 1.63 in the present study. The combination of regorafenib could reduce the frequency of TACE to protect patients’ liver function and improve patients’ quality of life in patients with advanced HCC.
The greater the number of tumors, the worse the patient’s prognosis mainly is. The present study showed that regorafenib combined with TACE was significantly more effective than regorafenib alone in treating patients with multiple lesions, which was similar to the results that the combination of TACE and sorafenib might provide survival benefits for patients with a large number of HCC nodules.34 In patients with ECOG-PS score of 2, the effects of regorafenib plus TACE therapy were found comparable to that of regorafenib alone, while for patients with good physical status, combination therapy significantly prolonged patients’ survival. This may be because the efficacy and tolerability of TACE are related to patients’ physical status, and patients in good physical condition are more likely to benefit from combination therapy. To some extent, this may indicate which patients would benefit from combination therapy, although these results need to be validated.
Common AEs associated with regorafenib in this study included hand-foot skin reactions, fatigue, abdominal pain, and hypertension, while they were mainly < grade 3, and no treatment-related deaths were recorded. No more serious AEs were found in the regorafenib plus TACE group than in the regorafenib group, except for the common post-embolization syndrome. Of course, the higher proportion and frequency of pre-TACE may have increased the toxic effects in the regorafenib plus TACE group, resulting in a bias in the safety evaluation of the two groups.
There were some limitations in the present study. Firstly, this was a single-centre retrospective study lacking randomized controls, and larger multi-centre prospective studies are required to validate the results in the future. Secondly, TACE treatment may be influenced by multiple factors. It is more recommended for patients with a better liver function, and there might be subjective biases in TACE technique and number of sessions. Third, the various remedial treatments following discontinuation of regorafenib may confuse the interpretation of regorafenib’s efficacy, safety and potential prognostic factors. Finally, the data related to AEs might be insufficient and would not reflect the actual conditions.
Conclusion
Regorafenib is an alternative sequential therapy for BCLC stage C HCC patients after failure of the first-line therapy, and it is expected to achieve a greater efficacy in combination with TACE. Further studies are needed to confirm the results of the present study. The patient’s ECOG-PS score, tumor size, number of tumors, and combined local therapy are factors influencing the prognosis of patients undergoing second-line therapy.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent to Publish
This manuscript does not include images that may indicate patients enrolled in this study.
Funding
This study was supported by Scientific Research Program for Department of Education of Anhui Province (2022AH040192).
Disclosure
The authors declare that there is no conflict of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. 2021;134(7):783–791. doi:10.1097/CM9.0000000000001474
3. Liu D, Song T. Changes in and challenges regarding the surgical treatment of hepatocellular carcinoma in China. Biosci Trends. 2021;15(3):142–147. doi:10.5582/bst.2021.01083
4. Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: a systematic review of efficacy and safety data. Hepatology. 2016;64(1):106–116. doi:10.1002/hep.28453
5. Kong JY, Li SM, Fan HY, Zhang L, Zhao HJ, Li SM. Transarterial chemoembolization extends long-term survival in patients with unresectable hepatocellular carcinoma. Medicine. 2018;97(33):e11872. doi:10.1097/MD.0000000000011872
6. Sergio A, Cristofori C, Cardin R, et al. Transcatheter arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): the role of angiogenesis and invasiveness. Am J Gastroenterol. 2008;103(4):914–921. doi:10.1111/j.1572-0241.2007.01712.x
7. Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi:10.1056/NEJMoa0708857
8. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised Phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–1173. doi:10.1016/S0140-6736(18)30207-1
9. Qin S, Bi F, Gu S, et al. Donafenib versus sorafenib in first-line treatment of unresectable or metastatic hepatocellular carcinoma: a randomized, open-label, parallel-controlled phase II-III trial. J Clin Oncol. 2021;39(27):3002–3011. doi:10.1200/JCO.21.00163
10. Laface C, Fedele P, Maselli FM, et al. Targeted therapy for hepatocellular carcinoma: old and new opportunities. Cancers. 2022;14(16):4028. doi:10.3390/cancers14164028
11. Liu KC, Hao YH, Lv WF, et al. transarterial chemoembolization combined with sorafenib in patients with BCLC stage C hepatocellular carcinoma. Drug Des Devel Ther. 2020;14:3461–3468. doi:10.2147/DDDT.S248850
12. Wilhelm SM, Dumas J, Adnane L, et al. Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer. 2011;129(1):245–255. doi:10.1002/ijc.25864
13. Rimassa L, Pressiani T, Personeni N, Santoro A. Regorafenib for the treatment of unresectable hepatocellular carcinoma. Expert Rev Anticancer Ther. 2017;17(7):567–576. doi:10.1080/14737140.2017.1338955
14. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. doi:10.1002/hep.24199
15. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60. doi:10.1055/s-0030-1247132
16. Freites-Martinez A, Santana N, Arias-Santiago S, Viera A. Using the common terminology criteria for adverse events (CTCAE - version 5.0) to evaluate the severity of adverse events of anticancer therapies. Actas Dermosifiliogr. 2021;112(1):90–92. doi:10.1016/j.ad.2019.05.009
17. Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7(1):6. doi:10.1038/s41572-020-00240-3
18. Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi:10.1056/NEJMoa1915745
19. Cabral LKD, Tiribelli C, Sukowati CHC. Sorafenib resistance in hepatocellular carcinoma: the relevance of genetic heterogeneity. Cancers. 2020;12(6):1576. doi:10.3390/cancers12061576
20. Abou-Elkacem L, Arns S, Brix G, et al. Regorafenib inhibits growth, angiogenesis, and metastasis in a highly aggressive, orthotopic colon cancer model. Mol Cancer Ther. 2013;12(7):1322–1331. doi:10.1158/1535-7163.MCT-12-1162
21. Granito A, Forgione A, Marinelli S, et al. Experience with regorafenib in the treatment of hepatocellular carcinoma. Therap Adv Gastroenterol. 2021;14:17562848211016959. doi:10.1177/17562848211016959
22. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56–66. doi:10.1016/S0140-6736(16)32453-9
23. Kudo M, Ueshima K, Ikeda M, et al. Randomised, multicentre prospective trial of transarterial chemoembolisation (TACE) plus sorafenib as compared with TACE alone in patients with hepatocellular carcinoma: TACTICS trial. Gut. 2020;69(8):1492–1501. doi:10.1136/gutjnl-2019-318934
24. Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T. Updated use of TACE for hepatocellular carcinoma treatment: how and when to use it based on clinical evidence. Cancer Treat Rev. 2019;72:28–36. doi:10.1016/j.ctrv.2018.11.002
25. Cheng Z, He L, Guo Y, Song Y, Song S, Zhang L. The combination therapy of transarterial chemoembolisation and sorafenib is the preferred palliative treatment for advanced hepatocellular carcinoma patients: a meta-analysis. World J Surg Oncol. 2020;18(1):243. doi:10.1186/s12957-020-02017-0
26. Patidar Y, Chandel K, Condati NK, Srinivasan SV, Mukund A, Sarin SK. Transarterial chemoembolization (TACE) combined with sorafenib versus TACE in patients with BCLC stage C hepatocellular carcinoma - A retrospective study. J Clin Exp Hepatol. 2022;12(3):745–754. doi:10.1016/j.jceh.2021.12.009
27. Kim N, You MW. Hepatocellular carcinoma and macrovascular tumor thrombosis: treatment outcomes and prognostic factors for survival. Jpn J Radiol. 2019;37(11):781–792. doi:10.1007/s11604-019-00868-6
28. Wang H, Xiao W, Han Y, et al. Study on safety and efficacy of regorafenib combined with transcatheter arterial chemoembolization in the treatment of advanced hepatocellular carcinoma after first-line targeted therapy. J Gastrointest Oncol. 2022;13(3):1248–1254. doi:10.21037/jgo-22-395
29. Han Y, Cao G, Sun B, et al. Regorafenib combined with transarterial chemoembolization for unresectable hepatocellular carcinoma: a real-world study. BMC Gastroenterol. 2021;21(1):393. doi:10.1186/s12876-021-01967-3
30. Leng JJ, Xu YZ, Dong JH. Efficacy of transarterial chemoembolization for hepatocellular carcinoma with portal vein thrombosis: a meta-analysis. ANZ J Surg. 2016;86(10):816–820. doi:10.1111/ans.12803
31. Hori A, Ohira R, Nakamura T, et al. Transarterial chemoembolization for pulmonary or mediastinal metastases from hepatocellular carcinoma. Br J Radiol. 2020;93(1110):20190407. doi:10.1259/bjr.20190407
32. Chen KL, Gao J. Factors influencing the short-term and long-term survival of hepatocellular carcinoma patients with portal vein tumor thrombosis who underwent chemoembolization. World J Gastroenterol. 2021;27(13):1330–1340. doi:10.3748/wjg.v27.i13.1330
33. Jeliazkova P, Umgelter A, Braren R, Kaissis G, Mustafa M, Einwächter H. Prognostic factors in hepatocellular carcinoma patients undergoing transarterial chemoembolization and radioembolization: a retrospective study. Eur J Gastroenterol Hepatol. 2020;32(8):1036–1041. doi:10.1097/MEG.0000000000001625
34. Abe Y, Ohkawa K, Sakakibara M, et al. Prognostic factors for patients with a large number of hepatocellular carcinoma nodules. J Clin Med Res. 2020;12(1):26–35. doi:10.14740/jocmr4032
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

