Back to Journals » International Journal of Women's Health » Volume 15
Efficacy and Adverse Effects After Single-Incision Slings for Women with Stress Urinary Incontinence: A 12-Year Follow-Up
Authors Barba M , Cola A, Costa C, Liberatore A, Frigerio M
Received 1 March 2023
Accepted for publication 11 July 2023
Published 18 July 2023 Volume 2023:15 Pages 1077—1082
DOI https://doi.org/10.2147/IJWH.S410539
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Marta Barba,1 Alice Cola,2 Clarissa Costa,1 Antonio Liberatore,3 Matteo Frigerio2
1Obstetric and Gynecology Department - University of Milano-Bicocca, Monza, Italy; 2Gynecology Department, Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy; 3School of Medicine, University of Milano-Bicocca, Monza, Italy
Correspondence: Marta Barba, University of Milano-Bicocca, Via Pergolesi, 33, Monza, Italy, Tel +39 233 9434, Email [email protected]
Objective: Single-incision slings (SISs) are not considered the first surgical choice for stress urinary incontinence due to few data about long-term results. Our aim was to evaluate the outcomes of SISs 12 years after implantation and to search for consequences such as deterioration after a certain amount of time.
Methods: We included women with stress urinary incontinence both clinically and urodynamically proven who underwent SISs procedure. Objective and subjective cure rates were compared to short-term outcomes to detect possible deterioration over time.
Results: A total of 85 patients were analysed with a median follow-up of 12.0 (IQR 10.4– 12.8) years. Objective and subjective cure rates were 81.0% and 82.1%, respectively. Median (IQR) PGI-I scores and ICIQ-SF, respectively, were 1 (1– 2) and 0 (0– 6.8). No significant deterioration of outcomes over time was shown after comparison between short-term and long-term follow-ups (objective cure rate 84.5% vs 81.0%, p=0.684; subjective cure rates 92.9% vs 82.1%, p=0.060). Also, voiding symptoms and overactive bladder did not differ over time (20.2% vs 21.4%, p=1.000; 20.2% vs 33.3%, p=0.080, respectively).
Conclusion: SISs were shown to be a procedure with a great efficacy and safety profile at very long-term follow-up.
Keywords: complications, functional outcomes, long-term follow-up, quality of life, single-incision sling, stress urinary incontinence
Introduction
Stress urinary incontinence (SUI) is a frequent condition described as the involuntary leakage of urine associated with actions like sneezing, laughing, and coughing.1 This condition negatively affects social, occupational, domestic, and psychophysical well-being.2 Conservative measures involve pelvic floor muscle training, electrical stimulation, magnetic stimulation, and vaginal laser.3 Surgery is considered in case of conservative management failure. Different kinds of surgery have been proposed in the last years, such as repair of anterior vaginal wall, autologous sling, suspension of bladder neck, urethral bulking agents, stem cells injection, and use of mesh tapes.4,5 As of today, positioning of standard suburethral slings is validated as the first-line therapy due to high long-term efficacy percentage.6 Various surgical approaches have been developed for suburethral slings, and each one involves some drawbacks. Retropubic tapes have been related with visceral injuries, especially bladder damage such as perforation.7 Transobturator slings may be related with vascular injuries and obturator nerve damage, involving thigh pain and neurological deficiency.8 Single-incision slings (SISs) are characterised by shorter tape length and consequently a limited intracorporeal dissection and lack of full passage of the introducers through the obturator foramen, adductor tendons, and skin. This involves a lower risk of complications including visceral injury, major bleeding, infection, and neurological pain, shorter recovery time, and a negligible learning curve.9,10 While excellent short-term efficacy rates unaffected by age, BMI, obstetrical history, and proper bilateral anchoring on obturator membranes have been demonstrated, long-term data are scarce.11–13
The aim of this study was to determine the long-term effects of treatment for urinary incontinence after single-incision sling implantation. We considered a 12-year follow-up, and we considered functional complications, subjective and objective cure rates, and patient satisfaction. Moreover, we aimed to compare the short-term and long-term outcomes in the same cohort of patients to search for possible deterioration of efficacy after a certain time frame.
Materials and Methods
We conducted a retrospective study at San Gerardo Hospital, University of Milano Bicocca, Monza, Italy. The study was approved by the local Institutional Review Board. Informed consent was not necessary due to the retrospective nature of the study. It was conducted in accordance with the 1964 Helsinki Declaration. We included all women with stress urinary incontinence both clinically and urodynamically proven who underwent SISs procedure in the time frame between October 2008 and June 2013. In the period of interest, SISs implantation was our standard procedure for women eligible for surgery. Preoperative assessment included clinical history collection, pelvic examination with prolapse staging, and urine examinations. Every woman was evaluated through preoperative urodynamics such as filling cystometry, uroflowmetry, and pressure/flow study by a trained urogynaecologist.14 Q-tip test result >30° defined urethral hypermobility. The Good Urodynamic Practice Guidelines of the International Continence Society were followed to define procedures and definitions.15 Exclusion criteria were: OAB symptoms/detrusor overactivity, positive postvoid residual volume (>100 mL), concomitant vaginal prolapse >stage 1 according to the POP-Q system, previous pelvic surgery, and neurological disorders. To assess women’s preoperative quality of life, the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) was submitted to all patients.16
Procedure used in the time frame was the MiniArc single-incision sling (American Medical Systems, Minnetonka, MN, USA). MiniArc is a 1 cm tape made by polypropylene 8.5 with self-fixating tips to bilaterally anchor it on the obturator muscles fascia. Every surgical procedure was executed according to manufacturer recommendations, as previously described.17 A 1–1.5 cm anterior colpotomy was made at the mid-urethra level, and paraurethral spaces were bilaterally exposed. The sling was then positioned, and the tips were fixed to the obturator muscles fascia. At the end of the procedure, exclusion of bladder/urethra injuries was made through intraoperative cystoscopy.
Postoperative visit was performed at one month, followed by an evaluation at 12 months, then yearly. During the examination, urogenital symptoms, voiding diary, and questionnaires were firstly collected, then clinical examination with a stress test was performed. The objective outcome was determined by a 300 mL stress test. Objective failure was defined if a positive stress test was found or the patient required a second surgical procedure for urinary incontinence. To evaluate the subjective cure rate, patients were asked to complete the Patient Global Impression of Improvement (PGI-I) questionnaire.18 The PGI-I questionnaire includes a seven-point scale, with responses ranging from 1 (“very much improved”) to 7 (“very much worse”), evaluating patients’ satisfaction. Success was defined by a PGI-I score ≤2. ICIQ-SF questionnaires were submitted to assess the urinary incontinence severity. The occurrence of de novo overactive bladder symptoms was identified during the clinical interviews or by specific domain in ICIQ-SF (“leak before you can get to the toilet”). Also voiding difficulty was evaluated through the voiding diary or during the clinical interview. If the patients did not undergo the follow-up visit within the last year, they were telephoned and asked to come to our outpatient setting for evaluation.
Database was completed by one author with a secondary double-check by another author. JMP software version 9 (SAS Institute, USA) was used for statistical analysis. Outcomes were defined as absolute (relative) frequency for non-continuous variables and as median (interquartile range) for continuous variables. To evaluate possible outcome deterioration over time, a previous database was used to compare short-term and long-term outcomes for the same patients, in terms of cure rates and functional outcomes. The Fisher test for non-continuous data was used to test the differences. Statistical significance was set with a p-value <0.05.
Results
In the period of interest, 102 consecutive records were collected. Seventeen (16.7%) patients were considered lost at follow-up: 4 patients had died, and 13 patients had wrong phone numbers. As a consequence, 85 patients completed the follow-up evaluation, with a median time of 12.0 (IQR 10.4–12.8) years. Table 1 reports population characteristics before surgery. No surgical postoperative complications were observed. Cure rates and functional outcomes at 12-year follow-up are reported in Table 2. Objective cure rate was 81.0%, while subjective cure rate was 82.1%. Median (IQR) PGI-I and ICIQ-SF scores were 1 (1–2) and 0 (0–6.8), respectively. Outcomes were compared to those available for the same patients in a previous series, 24 (15–41) months after the procedures. As shown in Figure 1, comparison between short-term and long-term follow-up did not show a significant difference of outcome over time. More specifically, objective and subjective cure rates were similar (84.5% vs 81.0%, p=0.684; 92.9% vs 82.1%, p=0.060, respectively). Also, voiding symptoms and overactive bladder did not differ over time (20.2% vs 21.4%, p=1.000; 20.2% vs 33.3%, p=0.080 respectively).
 |
Table 1 Population Characteristics Before Surgery. Data Reported as Median (Interquartile Range) for Continuous Variables and as the Absolute (Relative) Frequency for Non-Continuous Variables |
 |
Table 2 Long-Term Outcomes. Data Reported as Median (Interquartile Range) for Continuous Variables and as the Absolute (Relative) Frequency for Non-Continuous Variables |
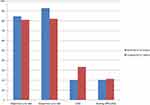 |
Figure 1 Comparison between short-term (2.6 ± 1.4 y) and long-term (10.3 ± 0.7 y) follow-up in terms of main outcomes in percentage (%). Abbreviation: OAB, overactive bladder syndrome. |
Discussion
Currently, midurethral sling implantation is under observation for the risk of graft-related complications, like chronic pelvic pain. The 2018 English ban on midurethral slings represents the direct consequence of these concerns.19 As previously happened with transvaginal mesh for prolapse repair, this warning brought anti-incontinence tape manufacturers to discontinue the production. Specifically, transobturator tapes are three times more prone to lead to neurological symptoms compared to retropubic tapes, and this is estimated to occur in up to 21% of women.20,21 As a consequence, the Australian Commission on Quality and Safety in Health Care and other guidelines recommend anti-incontinence procedures that avoid the trocar’s passage into the obturator space to reduce pain-related complications. Although SIS devices have this characteristic, they are still not recommended due to the lack of adequate scientific data.22 In fact, despite short-term evidence demonstrating comparable efficacy and less pain for SISs compared to conventional tapes, data about long-term outcomes are scarce.9,23
Our study focused on the efficacy at very long-term follow-up and on the complication rate of SISs implantation. We found that the procedure maintains excellent efficacy and safety 12 years after SISs implantation, without significant deterioration over time. In contrast, alternative anti-incontinence procedures present either low efficacy or significant intraoperative complications.24 Moreover, to date there is a paucity of studies evaluating SISs at long-term follow-up (>5 years). For example, 31 TVT-O patients versus 33 SISs (TVT Secur) were evaluated by Sun et al, 10 years after surgery.25 Transobturator tape resulted in superior objective and subjective cure rate, and its efficacy tends to decrease less after 10 years. Moreover, at medium-term follow-up (4.5 years), TVT Secur was confirmed to have poor results, demonstrating a 31% success rate.26 However, TVT Secur may not be considered representative of the SISs category for its mediocre performance, which led to its withdrawal from the market.27 Another study by Mira Gon et al prospectively analysed, after 8 years of follow-up, 20 naive patients with Ophira implanted as first anti-incontinence procedure compared to 20 women undergoing the procedure as secondary anti-incontinence surgery.28 The authors found that repeated surgery had a long-term cure rate decrease, while the subgroup of naive patients did not show any complications or functional disorder occurrence, nor any deterioration of cure rates over time, compared to short-term follow-up. Nienke et al retrospectively evaluated, with a mean follow-up time of 4.5 years, the long-term cure rates in a cohort of 397 patients after SISs (Ajust or Altis) implantation. They reported subjective improvement in 75% of patients, a lower rate if compared to those reported at 1-year follow-up after Ajust implantation and 2-year follow-up after Altis surgery. Sling failure was reported in 10% of patients, with 76% of these appearing in the first 2 years post-surgery.29 More reassuring data were reported by Frigerio et al who retrospectively evaluated long-term outcomes (with a mean follow-up of 10.3 ± 0.7 years) in 51 patients after MiniArc positioning. Objective cure rate was 86.3%, and subjective cure was 88.2%, with no long-term complications.23
A major strength of our study is the evaluation of SISs outcomes at long-term follow-up (12 years) with a limited loss of patients. Another strength can be identified in the homogeneous naive population with pure SUI. The discontinued surgical kit analysed and the retrospective design represent the study’s limitations. This study highlights the necessity of randomized prospective clinical trials to investigate SISs long-term outcomes, since they have the potential to become, similarly to standard tapes, a first-line treatment for SUI.
Conclusions
Single-incision sling procedures showed a safety profile and a great efficacy at very long-term follow-up. Compared to short-term results, cure rates and functional outcomes did not have any deterioration over time.
Data Sharing Statement
Data generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Ethics Approval
The study was approved by the Institutional Review Board of San Gerardo Hospital in Monza, Italy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bo K, Frawley HC, Haylen BT, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn. 2017;36:
2. Frigerio M, Barba M, Cola A, et al. Quality of life, psychological wellbeing, and sexuality in women with urinary incontinence-where are we now: a narrative review. Medicina. 2022;58(4):525. doi:10.3390/medicina58040525
3. Ruffolo AF, Braga A, Torella M, et al. Vaginal laser therapy for female stress urinary incontinence: new solutions for a well-known issue-A concise review. Medicina. 2022;58(4):512. doi:10.3390/medicina58040512
4. Manodoro S, Frigerio M, Barba M, Bosio S, de Vitis LA, Marconi AM. Stem cells in clinical trials for pelvic floor disorders: a systematic literature review. Reprod Sci. 2022;29(6):1710–1720. doi:10.1007/s43032-021-00745-6
5. Serati M, Braga A, Salvatore S, et al. Up-to-date procedures in female stress urinary incontinence surgery: a concise review on bulking agents procedures. Medicina. 2022;58(6):775. doi:10.3390/medicina58060775
6. Braga A, Castronovo F, Ottone A, et al. Medium term outcomes of TVT-abbrevo for the treatment of stress urinary incontinence: efficacy and safety at 5-year follow-up. Medicina. 2022;58(10):1412. doi:10.3390/medicina58101412
7. Milani R, Manodoro S, Cola A, Palmieri S, Frigerio M. Management of unrecognized bladder perforation following suburethral tape procedure. Int J Gynaecol Obstet. 2018;142(1):118–119. doi:10.1002/ijgo.12493
8. Milani R, Barba M, Manodoro S, Locatelli L, Palmieri S, Frigerio M. Inability to walk and persistent thigh pain after transobturator tape procedure for stress urinary incontinence: surgical management. Int Urogynecol J. 2021;32(5):1317–1319. doi:10.1007/s00192-020-04666-x
9. Mostafa A, Lim CP, Hopper L, Madhuvrata P, Abdel-Fattah M. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: an updated systematic review and meta-analysis of effectiveness and complications. Eur Urol. 2014;65(2):402–427. doi:10.1016/j.eururo.2013.08.032
10. Spelzini F, Frigerio M, Regini C, Palmieri S, Manodoro S, Milani R. Learning curve for the single-incision suburethral sling procedure for female stress urinary incontinence. Int J Gynaecol Obstet. 2017;139(3):363–367. doi:10.1002/ijgo.12317
11. Palmieri S, Frigerio M, Spelzini F, Manodoro S, Milani R. Risk factors for stress urinary incontinence recurrence after single-incision sling. Neurourol Urodyn. 2018;37(5):1711–1716. doi:10.1002/nau.23487
12. Frigerio M, Regini C, Manodoro S, Spelzini F, Milani R. Mini-sling efficacy in obese versus non-obese patients for treatment of stress urinary incontinence. Minerva Ginecol. 2017;69(6):533–537. doi:10.23736/S0026-4784.17.04081-3
13. Spelzini F, Cesana MC, Verri D, Polizzi S, Frigerio M, Milani R. Three-dimensional ultrasound assessment and middle term efficacy of a single-incision sling. Int Urogynecol J. 2013;24(8):1391–1397. doi:10.1007/s00192-012-2031-5
14. Manodoro S, Spelzini F, Frigerio M, Nicoli E, Verri D, Milani R. Is occult stress urinary incontinence a reliable predictive marker? Female Pelvic Med Reconstr Surg. 2016;22(4):280–282. doi:10.1097/SPV.0000000000000272
15. Schäfer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21(3):261–274. doi:10.1002/nau.10066
16. Tubaro A, Zattoni F, Prezioso D, et al. Italian validation of the international consultation on incontinence questionnaires. BJU Int. 2006;97(1):101–108. doi:10.1111/j.1464-410X.2006.05885.x
17. Spelzini F, Manodoro S, Cola A, Palmieri S, Roselli F, Frigerio M. Single-incision sling for stress urinary incontinence: a video tutorial. Eur J Obstet Gynecol Reprod Biol. 2019;237:216–217. doi:10.1016/j.ejogrb.2019.04.037
18. Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–528. doi:10.1007/s00192-009-1069-5
19. UK Parliament. Update on the independent medicines and medical devices safety review: written statement—HCWS841. Available from: https://www.parliament.uk/business/publications/written-questions-answers-statements/written-statement/Commons/2018-07-10/HCWS841.
20. Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7. doi:10.1002/14651858.CD006375.pub4
21. Seklehner S, Laudano MA, Xie D, Chughtai B, Lee RK. A metaanalysis of the performance of retropubic mid urethral slings versus transobturator mid urethral slings. J Urol. 2015;193:909–915. doi:10.1016/j.juro.2014.09.104
22. ACQSHC. Care Pathway for the Management of Stress Urinary Incontinence. ACQSHC; 2018.
23. Frigerio M, Milani R, Barba M, et al. Single-incision slings for the treatment of stress urinary incontinence: efficacy and adverse effects at 10-year follow-up. Int Urogynecol J. 2021;32(1):187–191. PMID: 32902762. doi:10.1007/s00192-020-04499-8
24. Haylen BT, Lee JKS, Sivagnanam V, Cross A. What if there were no tapes? Neurourol Urodyn. 2018;37(6):2026–2034. doi:10.1002/nau.23741
25. Sun Z, Wang X, Lang J, et al. Comparison of outcomes between single-incision sling and transobturator sling for treating stress urinary incontinence: a 10-year prospective study. Neurourol Urodyn. 2019;38(7):1852–1858. doi:10.1002/nau.24078
26. Cornu JN, Lizée D, Sèbe P, et al. TVT SECUR single-incision sling after 5 years of follow-up: the promises made and the promises broken. Eur Urol. 2012;62(4):
27. Luca MG, Bedretdinova D, Bosch JL, et al. European Association of Urology (EAU) guidelines. Guidelines Urinary Incont. 2015;60(6):1118–1129.
28. Mira Gon L, Zanettini Riccetto CL, Citatini de Campos CC, Iamashita Voris BR, Reis LO, Rodrigues Palma PC. Mini-sling Ophira at 8 years follow-up: does it sustain results? Urol Int. 2019;102(3):
29. Osse NJE, Engberts MK, Koopman LS, van Eijndhoven HWF. Evaluation of the long-term effect and complication rate of single-incision slings for female stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2021;267:1–5. PMID: 34688183. doi:10.1016/j.ejogrb.2021.10.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
