Back to Journals » International Journal of General Medicine » Volume 16
Effects of Three-Hour Wearing Personal Protective Equipment on Heart Rate Variability in Healthcare Workers for the Treatment of COVID-19 Patients
Authors Thi Ngoc Le H , Xuan Nguyen K , Duy Nguyen T , Quang La H, Thanh Nguyen X , Tien Le D, Quoc Pham H, Xuan Nguyen K, Hoang Nguyen H, Van Pham V, Van Pham C, Pho DC , Nhu Do B, Viet Tran T, Tien Nguyen S , Dinh Le T , Cong Luong T
Received 25 March 2023
Accepted for publication 13 June 2023
Published 16 June 2023 Volume 2023:16 Pages 2531—2539
DOI https://doi.org/10.2147/IJGM.S413626
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Han Thi Ngoc Le,1,* Kien Xuan Nguyen,2,* Toan Duy Nguyen,1 Ho Quang La,3 Xuan Thanh Nguyen,4 Dung Tien Le,5 Huy Quoc Pham,5 Khai Xuan Nguyen,6 Hiep Hoang Nguyen,7 Viet Van Pham,6 Cong Van Pham,5 Dinh Cong Pho,8 Binh Nhu Do,8 Tien Viet Tran,9 Son Tien Nguyen,10 Tuan Dinh Le,10,* Thuc Cong Luong1
1Cardiovascular Center, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 2Department of Military Medical Command and Organization, Vietnam Medical Military University, Hanoi, 10000, Vietnam; 3Hospital Quality Control Division, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 4Senior Officer Department, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 5Intensive Care, Emergency and Poison Control Center, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 6Interventional Radiology Department, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 7Field Internal Medicine Center, Military Hospital 103, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 8Department of Military Science, Vietnam Military Medical University, Hanoi, 10000, Vietnam; 9Department of Infectious Diseases, Military Hospital 103, Vietnam Medical Military University, Hanoi, 10000, Vietnam; 10Department of Rheumatology and Endocrinology, Vietnam Military Hospital 103, Medical Military University, Hanoi, 10000, Vietnam
*These authors contributed equally to this work
Correspondence: Thuc Cong Luong, Cardiovascular Center, Military Hospital 103, Vietnam Military Medical University, 160 Phung Hung Street, Phuc La Ward, Ha Dong District, Hanoi, Vietnam, Email [email protected]
Background: Personal protective equipment (PPE), an essential shield to protect healthcare workers (HCWs) during the COVID-19 pandemic, has been reported to affect their heart rate variability (HRV).
Objective: To investigate the changes of very short-term heart rate variability in HCWs after three hours of wearing PPE to treat COVID-19 patients at different working times and intensities, and related factors.
Methods: Sixty-five healthy HCWs were enrolled at the Number 2 Infectious Field Hospital (formed by Military Hospital 103), Vietnam. Two-minute 12-lead electrocardiograms were recorded before wearing and after removing PPE.
Results: After three hours of wearing PPE, the mean heart rate of HCWs increased (p = 0.048) meanwhile, the oxygen saturation decreased significantly (p = 0.035). Standard deviation of all normal to normal intervals (SDNN), mean intervals RR (mean NN), and root mean square successive difference (rMSSD) after wearing PPE was also reduced significantly. SDNN, Mean NN, and rMSSD decreased as the working intensity increased (as in mild, moderate, and severe patient departments). In univariate regression analysis, logSDNN, logmean NN and logrMSSD were positively correlated with SpO2 and QT interval (r = 0.14, r = 0.31, r = 0.25; r = 0.39, r = 0.77, r = 0.73, respectively) and were negatively correlated with ambient temperature inside PPE (r = − 0.41, r = − 0.405, r = − 0.25, respectively) while logmean NN and log rMSSD were negatively correlated with diastolic blood pressure (r = − 0.43, r = − 0.39, respectively). In multivariable regression analysis, logSDNN and logmean NN were negatively correlated to ambient temperature inside PPE (r = − 0.34, r = − 0.18, respectively).
Conclusion: Time-domain heart rate variability decreased after wearing PPE. Time-domain HRV parameters were related to ambient temperature inside PPE, diastolic blood pressure, QT interval, and SpO2.
Keywords: cardiovascular disorders, cardiovascular change, heart rate variability, personal protective equipment, healthcare workers, COVID-19
Introduction
In December 2019, COVID-19 outbroke in Wuhan, China, and quickly spread around the world.1 On 11th March 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic.2 Over the past two years, COVID-19 has claimed millions of lives. Although the COVID-19 pandemic is subsiding, emerging and re-emerging infectious diseases are still a global health threat. Personal protective equipment (PPE) remains paramount to protecting healthcare workers from viruses. The set of PPE includes a hair cover, goggles, N95 mask, fluid-resistant gown, gloves, and boots.3,4 PPE is crucial in preventing SARS-CoV-2 infection in HCWs but also causes some symptoms and adverse reactions. Previous studies have shown that after wearing PPE, HCWs often experienced respiratory symptoms or pressure-related lesions, skin lesions, eye damage, and stress disorders after wearing PPE.5–8 The stress and discomfort experienced when using PPE negatively contribute to the burden on HCWs and hinder their work.5,9
Stress causes activation of the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis, which initiates the release of catecholamines (adrenaline and noradrenaline) and cortisol into circulation.10 Simultaneously, the parasympathetic nervous system blocks those responses through the vagus nerve and returns the body to equilibrium.10 HCWs in the setting of stressful conditions are subject to harmful physiological adaptations related to the overactivity of the sympathetic nervous system.11 Heart rate variability (HRV) is the temporal variation between intervals of consecutive heartbeats. HRV reflects the balance of the sympathetic and parasympathetic nervous systems.12 The decrease in HRV over time is reportedly associated with events and survival prognosis in patients with cardiovascular diseases.13,14 Recent studies showed that wearing PPE in a short time increased heart rate and decreased heart rate variability.9,15 However, the effects of wearing PPE for long hours and working time and intensity on HRV have not been elucidated. We aimed to investigate the changes in very short-term HRV and related factors in healthcare workers after wearing PPE at different working shifts and intensities in a COVID-19 field hospital.
Methods
Study Population
A descriptive and cross-sectional study was conducted on 65 healthy HCWs (doctors and nurses) with a mean age of 35.1±5.0 (years) who worked at the Infectious Disease Field Hospital No.2, Military Hospital 103, Vietnam Military Medical University, in Bac Giang Province, Vietnam from May 2021 to July 2021. Of whom 96.9% were male, and 3.1% were female. Sixty-five HCWs were assigned to three departments based on the severity of the COVID-19 patients: 19 (29.2%) in severe patient department, 21 (32.3%) in moderate patient department, and 25 (38.5%) in mild patient department.
All HCWs who had cardiovascular or respiratory comorbidities did not finish a 3-hour shift at least, or did not consent to participate in the study were excluded.
Medical staff worked in shifts, each shift lasted three hours (namely, 0:00–3:00, 3:00–6:00, 6:00–9:00, 9:00–12:00, 12:00–15:00, 15:00–18:00, 18:00–21:00, 21:00–0:00). Day shifts were defined as shifts from 6:00 to 18:00, and night shifts were from 18:00 to 6:00. Healthcare workers were advised to have a light meal and drink enough water before their shift. The set of personal protective equipment, including hair cover, goggles, N95 mask, fluid-resistant gown, gloves, and boots, was worn by all health workers before the start of the shift and removed after the end of the shift. Health workers are also instructed to leave before expected work time if there is discomfort or any malfunction of personal protective equipment.
Before and after the shift (before putting on and after removing personal protective equipment), the temperature inside PPE, and clinical parameters (weight, body temperature, blood pressure, pulse rate, and SpO2) were measured, and a two-minute 12-lead electrocardiogram was recorded. The ambient temperature inside PPE was measured with a continuous electronic thermometer put in healthcare worker scrubs’ pocket, and data from this thermometer was taken and read on a computer. Healthcare workers’ weight was measured using a standard electronic weight scale. Body temperature was measured using a mercury thermometer. Blood pressure was measured with an electronic sphygmomanometer. Pulse rate and SpO2 were measured using a handheld fingertip oximeter. ECG was recorded at 50 mm/s speed using a Nihon Kohden Cardiofax M ECG machine (Nihon Kohden Co., Japan). Heart rate and QT interval on ECG were measured manually and averaged from 5 consecutive beats on lead II. R-R intervals were measured from the whole 2-minute tracing on lead II by two doctors trained to analyze electrocardiograms. Time-domain heart rate variability parameters, including mean NN (mean intervals RR), SDNN (standard deviation of all normal to normal intervals), and rMSSD (the square root of the mean of the squared difference between adjacent normal to normal R-R intervals) were calculated as described elsewhere.12,16
Stepwise procedure to manually measure SDNN, Mean NN, and rMSSD: The RR intervals in lead II of a 2-minute ECG were measured in millimeters. SDNN is computed in Excel using the STDEV function and converted to milliseconds. Calculate mean NN: (total duration of RR intervals)/(number of RR intervals). rMSSD is calculated by summing the squares of differences between RR intervals, averaging the sum of squares, and then taking the square root of the average using the SQRT function in Excel.
Ethical Statement
All participants provided written informed consent and agreed to join our study. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Review Committee of Military Hospital 103 (Reference No.189/2021/HĐĐĐ).
Statistical Analysis
Data were presented as mean±standard deviation or percentage or interquartile range. Comparison of continuous variables before and after the shift was performed with paired t-test or Wilcoxon test. Comparison of qualitative variables was done using the χ2 test. The univariate and multivariable regression analysis were performed with variables after the shift. A value of p <0.05 was considered statistically significant. Data were analyzed using the SPSS version 22 (IBM Inc, USA).
Results
After the shift, the mean weight of healthcare workers was lower than before the shift (p = 0.005). The pulse rate of healthcare workers after the shift was higher than before the shift (p = 0.032, respectively). The oxygen saturation decreased significantly as compared to before the shift (p = 0.035). Twelve-lead electrocardiograms analysis showed that the mean heart rate of healthcare workers after the shift increased significantly compared to before the shift (p = 0.048) while QT interval, SDNN, mean NN and rMSSD after the shift were significantly reduced compared to before the shift (p = 0.012, p = 0.031, p = 0.008 and p = 0.009, respectively). There were no differences in body temperature, systolic and diastolic blood pressures before and after the shift (Table 1). The mean temperature inside PPE during the working time was 29.7±1.9°C (min: 26.8°C and max: 32.8°C) (Table 1).
 |
Table 1 Healthcare Workers’ Characteristics and Time-Domain HRV Indices Before and After the Shift |
SDNN, Mean NN and rMSSD after the night shift were significantly lower than the day shift (p = 0.006, p = 0.027 and p = 0.03, respectively) (Table 2).
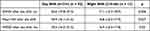 |
Table 2 Association of Heart Rate Variability Indices and Working Time |
Time domain HRV indices (SDNN, Mean NN, rMSSD) after the shift of HCWs working in severe COVID-19 patients department were significantly lower than those working in moderate and mild patient departments (Table 3).
 |
Table 3 Association of Heart Rate Variability Indices and Working Intensity |
In univariate regression analysis, the SDNN index had a statistically significant negative correlation with pulse rate, heart rate, and temperature inside PPE (r = −0.31, r = −0.42, r = −0.41, respectively); but positively correlated with QT interval and SpO2 (r = 0.39, r = 0.14, respectively). Mean NN strongly negatively correlated with pulse rate and heart rate (r = −0.67, r = −0.82, respectively); moderately correlated with diastolic BP and temperature inside PPE (r = −0.43, r = −0.405, respectively), but positively correlated with QT interval and SpO2 (r = 0.77, r = 0.31, respectively). The rMSSD index had a very high negative correlation with statistical significance of pulse rate and heart rate (r = −0.65 and r = −0.74, respectively); moderately correlated with diastolic BP and temperature inside PPE (r = −0.39, r = −0.29, respectively), but positively correlated with QT interval and SpO2 (r = 0.73, r = 0.25, respectively) (Table 4).
 |
Table 4 Correlation Between Heart Rate Variability Indices and Healthcare Workers’ Characteristics After the Shift |
In multivariable regression analysis, SDNN index was statistically significantly related to temperature inside PPE (beta coefficient = −0.34, p = 0.01). The mean NN was significantly related to heart rate, QT interval, and temperature inside PPE (beta coefficients and p-value of −0.41, 0.009 and 0.32, 0.026 and −0.18, 0.021, respectively). The rMSSD index was significantly associated with QT interval with beta and p coefficients of 0.41, 0.02 (Table 5).
 |
Table 5 Multivariate Regression Analysis of Heart Rate Variability Indices and Healthcare Workers’ Characteristics After the Shift |
Discussion
PPE is crucial in preventing the risk of infection with SARS-CoV-2. However, this protective measure also has certain adverse physiological consequences for HCWs.5,17 Our results showed a significant increase in the pulse rate of HCWs after three hours of wearing PPE (87.6±17.1 vs 84.1±13.1 beats per minute, p = 0.032). Choudhury et al, when observing HCWs working in the COVID-19 ICU, also found a significant difference in HCWs’ heart rates after removing PPE compared with baseline (not wearing protective equipment).9 Kim et al found that using an N95 mask for one hour increased heart rate from 5.7 to 10.6 beats per minute.18 When analyzing the 12-lead electrocardiogram, we found that the mean heart rate of HCWs after the shift increased significantly compared to before the shift (78.6±13.6 vs 75.9±11.0 beats per minute, p = 0.048). This suggests physiological responses to hypoxia and increased CO2 when wearing protective gear. The dead space of an N95 respirator without a valve can lead to a build-up of CO2.17 A decrease in O2 and an increase in CO2 can lead to increased heart rate and blood pressure. Airway resistance seems to increase in HCWs wearing an N95 respirator without a valve, which can further overload the heart and increase heart rate.9 The increase in heart rate when wearing PPE is also related to the time wearing protective equipment, workload, physicality, and anxiety of HCWs.
We found that the change in oxygen saturation before and after the shift was <1%. Other authors have recognized this in the process of qualitatively testing the suitability of users for N95 masks without valves.19 In our study, the oxygen saturation of HCWs decreased from 97.7(0.9%) to 97.4(0.8%) after the shift. The difference was statistically significant with p = 0.035, although not clinically significant (ie, HCWs did not feel any problems with this change). Our result aligned with Choudhury et al.9 Gaikwad et al also found that oxygen saturation decreased significantly when using an N95 mask.20 The decrease in oxygen saturation after wearing PPE can be explained by the high temperature and humidity of the micro-environment inside the valveless type N95 respirator as well as PPE leading to a higher impedance during breathing through a valveless respirator and thus reduced oxygen saturation.9,21
HRV is the number of consecutive heart rate fluctuations around the mean heart rate and reflects the complex interplay between the sympathetic and parasympathetic nervous systems.12 HRV is the change in the R-R intervals on the electrocardiogram, which is the change in the interval between a cardiac cycle and the next one. HRV was obtained from the electrocardiogram, including the time and frequency domain parameters. The easiest and fastest way to represent changes in HRV are time-domain variables.22,23 According to the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, the most important time-domain HRV parameters are SDNN and rMSSD.12 The time-varying rhythm indices show the function of sympathetic and parasympathetic nerves, but the degree of parasympathetic tone is more reflected. Normally, these indicators also fluctuate in a range of values, when there is a cardiovascular autonomic disorder, it will fluctuate in two directions of increase or decrease. Increased values are significant in the prognosis of survival and events in patients with cardiovascular disease, and decreased values play a role in assessing autonomic dysfunction.12 In field conditions, our study was conducted to collect parameters of heart rate variability (Mean NN, SDNNN, rMSSD) from RR intervals in two-minute 12-lead electrocardiogram of the medical staff. We found that SDNN mean NN and rMSSD after the shift were significantly reduced compared to before the shift. The stress and discomfort that health workers experience when using personal protective equipment cause the sympathetic nervous system to be overactive, leading to an imbalance of the sympathetic and parasympathetic nervous systems, manifesting itself by the dynamic variation of heart rate variability, which explained the decrease in SDNN, Mean NN, rMSSD after wearing personal protective equipment in our study. A study by Korean authors on 20 healthy people who were monitored for HRV, specifically SDNN when wearing a KF94 mask for 5 minutes and when not wearing a mask showed that wearing a mask made the SDNN of the research subjects decreased. One possible reason is that wearing a mask increases airway resistance leading to difficulty breathing and not getting enough oxygen, thereby affecting the regulation of the autonomic nervous system, ultimately leading to a decrease in variability of heart rate.15 This is just a test result when wearing a KF94 mask for 5 minutes. The authors believed that the longer the mask is worn, the more severe the hypoxia, and the more severe the body’s response to hypoxia. And therefore, the decrease in heart rate variability value would be greater.15 The health workers in our study wore personal protective equipment and worked each shift lasting three h, and the difference in time-domain heart rate variability index (SDNN, Mean NN, and rMSSD) before and after the shift was statistically significant (p = 0.031, p = 0.008 and p = 0.009, respectively). Our results are similar to the study of Pakanati et al. SDNN decreased significantly after wearing the N95 mask for one hour (40.93±19.11 ms) compared with before wearing the mask (42.68±19.11 ms), HRV indices representing parasympathetic components rMSSD and HF (High-Frequency power) significantly decreased when using N95 mask (from 41.79±24.43 ms to 38.66±21.01 ms and from 45.22±16.59 to 40.32±17.67, respectively). Meanwhile, LF (Low-Frequency power) represents sympathetic nerve activity, and the LF/HF ratio (A ratio of Low Frequency to High Frequency) increased significantly when using N95 masks (from 27.94±11.20 to 30.61±11.37 and from 0.71±0.73 to 1.07±1.08, respectively).24
There was a significant difference in the SDNN index in the group of HCWs on the night shift compared with the group on the day shift (17.1 vs 26.6, p = 0.006). Mean NN and rMSSD on the night shift were significantly reduced compared to the day shift (p = 0.027 and 0.03, respectively). This is consistent with the diurnal rhythm of HRV in normal individuals, which is lower at night than during the day. The indices of HRV over the time spectrum (ie, SDNN, Mean NN, rMSSD) after the shift in the group working in the severe patient department were significantly lower than those working with moderate and mild patients (p = 0.014, p = 0.031, p = 0.012, respectively). This reflects the influence of workload on HRV. The medical staff all worked in 3-hour shifts, but the staff working in the severe patient department had a larger workload than others. A greater workload meant more stress. Previous studies have shown that acute or chronic stress leads to reduced HRV.25,26 While stress makes the sympathetic nervous system overactive, the parasympathetic nervous system is underactive, which leads to an imbalance of the sympathetic and parasympathetic nervous systems, reducing the variables heart rate.27–29 A study in India on 1.373 HCWs working during the COVID-19 pandemic found that rMSSD, SDNN, and pNNi50 (NN50 count divided by the total number of the all normal to normal intervals) were significantly lower in the group of HCW with exhaustion/stress compared with the group of HCW who are not exhausted/stressed.
In our study, when analyzing univariate regression, logSDNN index had significantly negative correlation with pulse rate (r = −0.31) and heart rate (r = −0.42); log mean NN had a strong negative correlation with pulse rate (r = −0.67) and heart rate (r = −0.82); log rMSSD index had a strong negative correlation with pulse rate (r = −0.65) and heart rate (r = −0.74). In multivariate regression analysis, logmean NN was significantly related to heart rate (beta and p coefficients of −0.41, 0.009). This is easily explained by wearing protective equipment; as mentioned above, the sympathetic nervous system is overactive, causing an increase in pulse and heart rates and at the same time an imbalance of the nervous system. These sympathetic and parasympathetic activations reduce HRV over time (ie, SDNN, Mean NN, rMSSD).
In univariate regression analysis, logmean NN and log rMSSD were negatively correlated with diastolic blood pressure (r = −0.43, r = −0.39, respectively). These results are consistent with previous findings, which confirmed the inverse association between HRV and blood pressure.30,31 Mori et al also found a significant inverse association of HRV with diastolic blood pressure, although there was no significant association of HRV with systolic blood pressure.32 The autonomic nervous system regulates blood pressure by three mechanisms: direct action on the heart to increase stroke volume, output, and heart rate; direct action on peripheral arterial resistance; and by increasing renin level and activity. Sympathetic nerve endings release noradrenaline, which increases cardiac output by increasing heart rate and cardiac muscle automaticity and vascular resistance in peripheral blood vessels. Therefore, autonomic imbalance involving active sympathetic function and hypoactive parasympathetic function partially contribute to blood pressure elevation.
In analyzing univariate regression, the time-domain heart rate variability index (logSDNN, logMean NN and logrMSSD) positively correlated with SpO2 (r = 0.14, r = 0.31, r = 0.25, respectively). A decrease in O2 and an increase in CO2 when wearing PPE leads to decreased oxygen saturation and activated sympathetic nervous, causing decreased time domain HRV.
We found that logSDNN was positively correlated with QT interval (r = 0.39) in analyzing univariate regression, and logmean NN, logrMSSD were positively correlated with QT interval in analyzing univariate and multivariate regression (r = 0.77, r = 0.73, r = 0.32, r = 0.41, respectively). The QT interval represents the time from the onset of ventricular depolarization to the completion of repolarization. Previous animal studies showed that the dispersion of ventricular repolarization was increased by sympathetic stimulation.33 Recent human studies showed that the QT interval was associated positively with sympathetic activity and negatively with parasympathetic activity, reflecting physiologic homeostasis in cardiac autonomic modulations.34,35
In addition to the influence of day/night shifts and workload on HRV, the temperature inside PPE must also be considered. In our study, the temperature inside PPE of HCWs was correlated with time-domain HRV indices in regression analysis. In analyzing univariate regression, logSDNN, logmean NN, and logrMSSD index was negatively correlated with the temperature inside PPE (r = −0.41, p = 0.001; r = −0.405, p = 0.001 and r = −0.29, p = 0.016, respectively). In analyzing multivariable regression, logSDNN and logmean NN were significantly related to the temperature inside PPE (beta and p coefficients of −0.34,0.01 and −0.18,0.021, respectively). The insulative properties of PPE lead to elevated temperature and humidity inside PPE.36 In our study, the peak temperature inside PPE during the working time was 32.8°C. Several previous studies have shown that ambient temperature inside PPE becomes higher and contains more water vapor relative to the surrounded air leading to thermoregulatory challenges.37,38 In COVID-19 practice, HCWs wearing PPE reporting thermal discomfort, high sweat rates and soaked clothing, making working conditions uncomfortable.39,40 The higher the temperature inside PPE, the more pressure, discomfort, and stress medical staff have when working with PPE, leading to dynamic HRV changes. Temperature variability was associated with decreased HRV has been recognized by other authors.41,42 Yamamoto et al43 and Ren et al44 found that high temperature was inversely associated with all HRV measures. HRV parameters are very important showing the current health status of patients. These parameters can change in a short time with a healthy lifestyle.45 COVID-19 can also change the HRV parameters. Increased tonus of parasympathetic parameters is very interesting following COVID-19 infection.46
Conclusion
Wearing PPE for long hours results in a decrease in time domain HRV. The change in time domain HRV parameters is related to ambient temperature inside PPE, oxygen saturation, working intensity, and working time. The decrease in oxygen saturation, the increase in ambient temperature inside PPE, the higher working intensity and night shift lead to the reduction in time domain HRV parameters. This reflects bad effects of working stress when wearing PPE for long hours on healthcare workers’ cardiovascular health in treating COVID-19 patients.
Abbreviations
PPE, personal protective equipment; HCWs, healthcare workers; HRV, heart rate variability; SDNN, standard deviation of all normal to normal intervals; mean NN, mean intervals RR; rMSSD, root mean square successive difference; SBP, systolic blood pressure; DBP, diastolic blood pressure; SpO2, saturation pulse oxygen; bpm, beats per minute.
Acknowledgments
We thank the staff in Military Hospital 103 for collecting the samples and supporting the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The author(s) received no financial support for this article’s research, authorship, and/or publication.
Disclosure
The authors declared no potential conflicts of interest to this article’s research, authorship, and/or publication.
References
1. Guo Y-R, Cao Q-D, Hong Z-S, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Med Res. 2020;7(1):11. doi:10.1186/s40779-020-00240-0
2. WHO. WHO Director-General’s opening remarks at the media briefing on COVID- 19: 11 March 2020; 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-.
3. World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages: Interim Guidance; 2020.
4. Tabah A, Ramanan M, Laupland KB, et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): an international survey. Research Support, Non-U.S. Gov’t. J Crit Care. 2020;59:70–75. doi:10.1016/j.jcrc.2020.06.005
5. Battista RA, Ferraro M, Piccioni LO, Malzanni GE, Bussi M. Personal Protective Equipment (PPE) in COVID 19 Pandemic: related Symptoms and Adverse Reactions in Healthcare Workers and General Population. Observational Study. J Occupational Environ Med. 2021;63(2):e80–e85. doi:10.1097/JOM.0000000000002100
6. Lin P, Zhu S, Huang Y, et al. Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak: a survey in Wuhan and its surrounding regions. Letter. Br J Dermatol. 2020;183(1):190–192. doi:10.1111/bjd.19089
7. Jiang Q, Liu Y, Wei W, et al. The prevalence, characteristics, and related factors of pressure injury in medical staff wearing personal protective equipment against COVID-19 in China: a multicentre cross-sectional survey. Multicenter Study. Int Wound J. 2020;17(5):1300–1309. doi:10.1111/iwj.13391
8. Gefen A, Ousey K. Update to device-related pressure ulcers: SECURE prevention. COVID-19, face masks and skin damage. J Wound Care. 2020;29(5):245–259. doi:10.12968/jowc.2020.29.5.245
9. Choudhury A, Singh M, Khurana DK, et al. Physiological Effects of N95 FFP and PPE in Healthcare Workers in COVID Intensive Care Unit: a Prospective Cohort Study. Indian j Critical Care Med. 2020;24(12):1169–1173. doi:10.5005/jp-journals-10071-23671
10. Godoy LD, Rossignoli MT, Delfino-Pereira P, Garcia-Cairasco N, de Lima Umeoka EH. A Comprehensive Overview on Stress Neurobiology: basic Concepts and Clinical Implications. Review. Front Behav Neurosci. 2018;12:127. doi:10.3389/fnbeh.2018.00127
11. Aristizabal JP, Navegantes R, Melo E, Pereira A. Use of Heart Rate Variability Biofeedback to Reduce the Psychological Burden of Frontline Healthcare Professionals Against COVID-19. Front Psychol. 2020;11:572191. doi:10.3389/fpsyg.2020.572191
12. Naspe ESC. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Guideline Practice Guideline. Circulation. 1996;93(5):1043–1065.
13. Perkiomaki JS, Huikuri HV, Koistinen JM, Makikallio T, Castellanos A, Myerburg RJ. Heart rate variability and dispersion of QT interval in patients with vulnerability to ventricular tachycardia and ventricular fibrillation after previous myocardial infarction. Research Support, Non-U.S. Gov’t. J Am Coll Cardiol. 1997;30(5):1331–1338. doi:10.1016/s0735-1097(97)00301-x
14. Melillo P, Izzo R, De Luca N, Pecchia L. Heart rate variability and target organ damage in hypertensive patients. Research Support, Non-U.S. Gov’t. BMC Cardiovasc Disord. 2012;12:105. doi:10.1186/1471-2261-12-105
15. Tian Z, Bong-Young K, Myung-Jin B. A Study on the Effect of Wearing Masks on Stress Response. Int J Eng Res Technol. 2020;13:807–813.
16. Billman GE. Heart rate variability - a historical perspective. Front Physiol. 2011;2:86. doi:10.3389/fphys.2011.00086
17. Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Comparative Study. Respir Care. 2010;55(5):569–577.
18. Kim JH, Benson SM, Roberge RJ. Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am J Infect Control. 2013;41(1):24–27. doi:10.1016/j.ajic.2012.02.037
19. Laferty EA, McKay RT. Physiologic effects and measurement of carbon dioxide and oxygen levels during qualitative respirator fit testing. J Chem Health Safe. 2006;13:22–28. doi:10.1021/acs.chas.8b13507
20. Gaikwad RP, Banodkar AB, Nandgaonkar VP. Respiratory consequences of N95 mask during Covid-19 pandemic- an observational study. Int J Health Sci Res. 2021;11(4):55–61. doi:10.52403/ijhsr.20210407
21. Li Y, Tokura H, Guo YP, et al. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Comparative Study. Int Arch Occup Environ Health. 2005;78(6):501–509. doi:10.1007/s00420-004-0584-4
22. Shaffer F, Ginsberg JP. An Overview of Heart Rate Variability Metrics and Norms. Front Public Health. 2017;5:258. doi:10.3389/fpubh.2017.00258
23. Penttila J, Helminen A, Jartti T, et al. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: effects of various respiratory patterns. Clin Physiol. 2001;21(3):365–376. doi:10.1046/j.1365-2281.2001.00337.x
24. Pakanati S, Venkata MG, Prabhakara R. Heart rate variability related to N95 respirator use in interns during COVID-19 pandemic. Int J Sci Res. 2021;10(10):69–70. doi:10.36106/ijsr
25. Delaney JP, Brodie DA. Effects of short-term psychological stress on the time and frequency domains of heart-rate variability. Percept Mot Skills. 2000;91(2):515–524. doi:10.2466/pms.2000.91.2.515
26. Lucini D, Di Fede G, Parati G, Pagani M. Impact of chronic psychosocial stress on autonomic cardiovascular regulation in otherwise healthy subjects. Research Support, Non-U.S. Gov’t. Hypertension. 2005;46(5):1201–1206. doi:10.1161/01.HYP.0000185147.32385.4b
27. Schwartz AR, Gerin W, Davidson KW, et al. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 2003;65(1):22–35. doi:10.1097/01.psy.0000046075.79922.61
28. Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH. Stress and Heart Rate Variability: a Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018;15(3):235–245. doi:10.30773/pi.2017.08.17
29. Lennartsson AK, Jonsdottir I, Sjors A. Low heart rate variability in patients with clinical burnout. Int J Psychophysiol. 2016;110:171–178. doi:10.1016/j.ijpsycho.2016.08.005
30. Schroeder EB, Liao D, Chambless LE, Prineas RJ, Evans GW, Heiss G. Hypertension, blood pressure, and heart rate variability: the Atherosclerosis Risk in Communities (ARIC) study. Hypertension. 2003;42(6):1106–1111. doi:10.1161/01.HYP.0000100444.71069.73
31. Singh JP, Larson MG, Tsuji H, Evans JC, O’Donnell CJ, Levy D. Reduced heart rate variability and new-onset hypertension: insights into pathogenesis of hypertension: the Framingham Heart Study. Hypertension. 1998;32(2):293–297. doi:10.1161/01.hyp.32.2.293
32. Mori H, Saito I, Eguchi E, Maruyama K, Kato T, Tanigawa T. Heart rate variability and blood pressure among Japanese men and women: a community-based cross-sectional study. Hypertens Res. 2014;37(8):779–784. doi:10.1038/hr.2014.73
33. Ishida S, Nakagawa M, Fujino T, Yonemochi H, Saikawa T, Ito M. Circadian variation of QT interval dispersion: correlation with heart rate variability. J Electrocardiol. 1997;30(3):205–210. doi:10.1016/s0022-0736(97)80005-2
34. Arai K, Nakagawa Y, Iwata T, Horiguchi H, Murata K. Relationships between QT interval and heart rate variability at rest and the covariates in healthy young adults. Auton Neurosci. 2013;173(1–2):53–57. doi:10.1016/j.autneu.2012.11.006
35. Ishii N, Dakeishi M, Sasaki M, Iwata T, Murata K. Cardiac autonomic imbalance in female nurses with shift work. Auton Neurosci. 2005;122(1–2):94–99. doi:10.1016/j.autneu.2005.08.010
36. McLellan TM, Daanen HA, Cheung SS. Encapsulated environment. Compr Physiol. 2013;3(3):1363–1391. doi:10.1002/cphy.c130002
37. White MK, Vercruyssen M, Hodous TK. Work tolerance and subjective responses to wearing protective clothing and respirators during physical work. Ergonomics. 1989;32(9):1111–1123. doi:10.1080/00140138908966878
38. de Korte JQ, Bongers C, Catoire M, Kingma BRM, Eijsvogels TMH. Cooling vests alleviate perceptual heat strain perceived by COVID-19 nurses. Temperature. 2022;9(1):103–113. doi:10.1080/23328940.2020.1868386
39. Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Global Health. 2020;8(6):e790–e798. doi:10.1016/S2214-109X(20)30204-7
40. Davey SL, Lee BJ, Robbins T, Randeva H, Thake CD. Heat stress and PPE during COVID-19: impact on healthcare workers’ performance, safety and well-being in NHS settings. J Hosp Infect. 2021;108:185–188. doi:10.1016/j.jhin.2020.11.027
41. Tang M, He Y, Zhang X, et al. The acute effects of temperature variability on heart rate variability: a repeated-measure study. Environ Res. 2021;194:110655. doi:10.1016/j.envres.2020.110655
42. Bruce-Low SS, Cotterrell D, Jones GE. Heart rate variability during high ambient heat exposure. Aviat Space Environ Med. 2006;77(9):915–920.
43. Yamamoto S, Iwamoto M, Inoue M, Harada N. Evaluation of the effect of heat exposure on the autonomic nervous system by heart rate variability and urinary catecholamines. Evaluation Study. J Occup Health. 2007;49(3):199–204. doi:10.1539/joh.49.199
44. Ren C, O’Neill MS, Park SK, Sparrow D, Vokonas P, Schwartz J. Ambient temperature, air pollution, and heart rate variability in an aging population. Am J Epidemiol. 2011;173(9):1013–1021. doi:10.1093/aje/kwq477
45. Hayıroğlu M, Çinier G, Yüksel G, et al. Effect of a mobile application and smart devices on heart rate variability in diabetic patients with high cardiovascular risk: a sub-study of the LIGHT randomized clinical trial. Kardiol Pol. 2021;79(11):1239–1244. doi:10.33963/KP.a2021.0112
46. Asarcikli LD, Hayiroglu M, Osken A, Keskin K, Kolak Z, Aksu T. Heart rate variability and cardiac autonomic functions in post-COVID period. J Interv Card Electrophysiol. 2022;63(3):715–721. doi:10.1007/s10840-022-01138-8
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
