Back to Journals » Infection and Drug Resistance » Volume 14
Effects of Regulation on Carbapenem Prescription in a Large Teaching Hospital in China: An Interrupted Time Series Analysis, 2016–2018
Authors Xie L, Du Y, Wang X, Zhang X , Liu C, Liu J, Peng X, Guo X
Received 3 June 2021
Accepted for publication 14 July 2021
Published 11 August 2021 Volume 2021:14 Pages 3099—3108
DOI https://doi.org/10.2147/IDR.S322938
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Lewei Xie,1 Yaling Du,1 Xuemei Wang,1 Xinping Zhang,1 Chenxi Liu,1 Junjie Liu,2 Xi Peng,3 Xinhong Guo3
1School of Medicine and Health Management, Tongji Medical School, Huazhong University of Science and Technology, Wuhan, Hubei, People’s Republic of China; 2School of Statistics and Mathematics, Central University of Finance and Economics, Beijing, People’s Republic of China; 3First Affiliated Hospital, School of Medicine, Shihezi University, Xinjiang, Shihezi, People’s Republic of China
Correspondence: Xinping Zhang; Yaling Du
School of Medicine and Health Management, Tongji Medical School, Huazhong University of Science and Technology, Wuhan, Hubei, People’s Republic of China
Tel +86 133 4995 0095
; +86 180 0993 8932
Email [email protected]; [email protected]; [email protected]
Purpose: Carbapenem resistance due to the overuse of carbapenems has become a public health problem worldwide, particularly in low- and middle-income countries (LMICs). However, there are few policies guiding carbapenem prescription, and their effectiveness is still unclear. A regulation targeting carbapenem prescription was implemented in March 2017 in China. This study aimed to assess the effects of the regulation for providing evidence on the prudent use of carbapenems.
Patients and Methods: This was an interventional, retrospective study started in January 2017. The intervention covered establishing performance appraisal indicators, special authorisation, strict prescribing restrictions, and dedicated supervision, particularly in the intensive care unit (ICU). Data on adult inpatients who received at least one carbapenems were extracted from January 2016 to December 2018. Segmented regression analysis was performed to evaluate the effect of the regulation.
Results: A total of 2005 inpatients received carbapenems. Segmented regression models showed an immediate decline in the intensity of antibiotic consumption (IAC) of carbapenems (coefficient = − 9.65, p < 0.001), particularly imipenem (coefficient = − 6.82, p = 0.002), and the antibiotic consumption of carbapenems (coefficient = − 133.60, p = 0.003) in the ICU. And there is a decreasing trend in the IAC of meropenem (coefficient = − 0.03, p = 0.008) in all departments. Furthermore, the IAC of carbapenems and imipenem (coefficient = − 0.36, p = 0.035; coefficient = − 0.49, p = 0.025, respectively), and the average length of stay (ALoS) (coefficient = − 0.73, p < 0.001) showed downward trends in the ICU.
Conclusion: The intervention effectively reduced the IAC of carbapenems and imipenem, carbapenem consumption and the ALoS in the ICU, and the IAC of meropenem in all departments. The effects of the intervention were significant in the ICU, which indicated an urgent need for stronger regulations focusing on critical departments in the future.
Keywords: carbapenem prescription, ICU, multifaceted intervention, antimicrobial stewardship, effects assessment, segmented regression
Introduction
Carbapenem resistance occurs mainly in Gram-negative bacilli such as Enterobacteriaceae.1 From 2015 to 2019, carbapenem-resistant Enterobacteriaceae (CRE) showed a significant growth trend, especially carbapenem-resistant Klebsiella pneumoniae (CR-Kp).2 The increase in carbapenem-resistant Gram-negative bacilli (CR-GNB) is a critical threat to global public health.1,3 Infections caused by CR-GNB have few effective treatment options and a high mortality rate due to co-resistance to multiple antibiotic groups, signifying a challenge for clinicians and healthcare systems.4–6 The increasing number of CR-GNB has increased the pressure on dosing options to combat bacterial resistance7,8 and reduced compliance with infection prevention and control strategies.9 Multiple studies confirm that carbapenem consumption is strongly associated with the spread and development of CR-GNB.10–13 Studies from several tertiary hospitals in China have confirmed that carbapenem resistance is related to the intensity of use.14,15 This shows that carbapenem abuse is an inescapable cause of carbapenem resistance and that curbing the misuse of carbapenem antibiotics is an urgent necessity.
In recent years, low- and middle-income countries (LMICs) have recorded a significant increase in carbapenem consumption, exposing health systems to the high burden of diseases and mortality of carbapenem-resistant infections in the near future.16,17 Carbapenems were most frequently prescribed in Latin America and Asia.18 However, effective interventions for carbapenem prescription are significantly inadequate in LMICs countries, especially in Asia.19,20 Although international guidelines and studies provide a wealth of evidence-based recommendations for regulating the prescription of carbapenems, these recommendations are often incompatible with the practice and infrastructure of many hospitals in Asia.21–23 In addition, carbapenem use in the ICU needs more attention and effective intervention related to high consumption, the severity of the disease, and the complexity of the infecting bacteria.
There are currently five central international strategies to manage antibiotic use: education and guidelines, formulary and restriction, review and feedback, computer assistance, and antibiotic cycling.24 A regulation for managing carbapenem prescribing was introduced in China in March 2017, including prescribing restrictions and review with feedback strategies. The regulation outlines specific requirements for the prescription of carbapenems with dedicated personnel to collect, collate and report information on carbapenem prescription. In contrast to the previous policies on managing all types of antibiotics, this features a clear focus on a single kind of antibiotic, carbapenems, and tighter control in departments with high carbapenem use, such as the ICU.
To evaluate the effectiveness of the regulation and improve carbapenem prescribing in LMICs of Asia, we implemented a multimodal intervention for carbapenems in a large teaching hospital in China based on this policy. We evaluated its effectiveness using segmented regression analysis of interrupted time series (ITS). The results of this study will fill the gaps in the literature and add comparable evidence for a dedicated stewardship system for carbapenems in Asia to further promote the prudent use of carbapenems.
Patients and Methods
Study Setting and Data Sources
This study was conducted at a sizeable 1500-bed teaching hospital in Xinjiang, Western China. A total of 2005 inpatients who used at least one carbapenem were selected for the study. Data on the primary diagnosis and carbapenem antimicrobial prescriptions were extracted from the inpatient information system, masking the patients’ personal data (patient name, ID number, telephone number, home address). Data over 36 months (from Jan 1, 2016 to Dec 31, 2018) were collected. The intervention started in July 2017. The data were divided into 18 months pre-intervention and 18 months post-intervention, including demographic information, primary disease diagnosis, and carbapenem prescriptions (name, dose, duration of use, type, etc.).
Intervention Design and Implementation
In March 2017, a new regulation for the carbapenem prescription was issued by the National Health Commission of China.25 A team including physicians, pharmacists, microbiologists, and infectious disease specialists designed the intervention model based on this regulation. Starting in July 2017, the multifaceted intervention was gradually implemented at the teaching hospital. The intervention included the following strategies: (1) Establishing performance appraisal indicators: the delivery rate of prescribing carbapenems was added to the hospital performance appraisal indicators. The specific requirement of the indicator is that prescriptions containing carbapenems must be supported by a drug sensitivity test (with a delivery rate of no less than 80%).
(2) Special authorisation: specify that physicians qualified as associate chief physicians or above and are trained and authorised to prescribe antibiotic drugs can prescribe carbapenems. (3) Strict prescribing restrictions: firstly, prescriptions must be issued after multidisciplinary consultation and agreement between the department, the disease-related department, and the pharmacist. Secondly, prescriptions may only be given by a physician with the special prescribing authority. Finally, when it is necessary to overstep the prescribing jurisdiction in an emergency, the prescription should not exceed one day’s dosage, and the relevant medical records should be preserved. (4) Dedicated supervision: each clinical department was required to complete the Information Form of Carbapenem Prescription (IFCP) after using carbapenems, which included drug name, patient information, and medication information (primary diagnosis, drug usage, prescribing physician, prescription-checking pharmacists, drug sensitivity test results, etc.). We designated a dedicated person in the pharmacy department who collected and summarised the IFCP daily and checked each IFCP feedback and explanation of the inappropriate prescriptions was conducted with the physician. Each month, the prescription of carbapenems was published within the hospital. (5) Strengthen the management of critical departments: we selected the ICU as the critical department, collected and reviewed IFCPs from the ICU as a priority, and provided weekly feedback to the ICU director.
Outcomes
Three indicators were used to describe the use and clinical outcomes of carbapenems in this study. The intensity of antibiotic consumption (IAC) is expressed as the average number of defined daily doses (DDD) of antibiotics per 100 patient days of hospitalisation for the same period (DDD/100 patient-days).26 DDDs equivalent is the usage amount multiplied by the package size divided by the DDD, DDDs = (usage amount × package size/DDD).27 The antibiotic consumption (Cumulative DDDs) is defined as the sum of the DDDs every month. The average length of stay (ALoS) = total number of days in the hospital for inpatients treated with carbapenem antibiotics/number of inpatients treated with carbapenem antibiotics in the same period. There are two kinds of carbapenems in the hospital: meropenem, imipenem. The criteria for diagnosing diseases are based on the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) developed by the WHO.28
Statistical Analysis
Interrupted time series analysis is a simple but powerful tool for assessing the impact of a policy change or quality improvement programme on a particular outcome in a defined population. A significant advantage of ITS in observational data evaluating the impact of quality improvement efforts is that the method controls the effects of long-term trends in the time series of outcome measures.29 In this study, monthly carbapenem antibiotic use and the ALoS from Jan 1, 2016 to Dec 31, 2018 was applied as the unit of analysis, with Jan 1, 2016 to June 30, 2017 as the pre-intervention evaluation period and July 1, 2017 to Dec 31, 2018 as the post-intervention evaluation period.
To evaluate the effect of the intervention on carbapenem prescription and the ALoS, the following segmented linear regression model was applied:
Y = β0 + β1*time + β2*intervention + β3*time*intervention + ε
Y represents the IAC, cumulative DDDs, or ALoS. The coefficient β0 represents the baseline level in January 2016; β1 represents the change that occurred in each month before the intervention (baseline trend/slope); β2 and β3 represent the change in the level and trend of the outcome indicators (compared to β0 and β1) since the start of the intervention, indicating the short-term and long-term effects of the intervention, respectively. Time is the value of the time variable (in months), Jan 2016 = 1, Feb 2016 = 2, Mar 2016 = 3 … Intervention is a binary variable used to distinguish the period before and after the intervention. The term ε is residual error. This study used residual analysis to test for serial autocorrelation and assessed autocorrelation through the Durbin-Watson statistic. The generalised least-squares method was used to adjust the model to avoid autocorrelation. We used t-tests to assess continuous variables and Chi-squared tests or Fisher’s exact tests to evaluate categorical variables. All statistical analyses were completed using STATA version 12.0, and differences of P < 0.05 were considered statistically significant.
Results
Patient Characteristics
Table 1 presents the characteristics of inpatients who received at least one carbapenem antibiotic. There were 1054 and 951 inpatients who had received carbapenem antibiotics in the pre- and post-intervention period, respectively. The mean age of the inpatients before and after the intervention was 61.99 years and 60.76 years, respectively. The top five principal diagnoses were chronic obstructive pneumonia, pneumonia, pulmonary infections, sepsis, and infectious fever.
 |
Table 1 Characteristics of Inpatients During the Pre- and Post-Intervention Periods |
There were no significant differences between the pre- and post-intervention samples in age, gender, the number of top five diagnoses, and the main department of the inpatient admitted.
Carbapenem Consumption and Average Length of Stay During 2016–2018
Figure 1 shows the monthly values for IAC in all departments. The IAC of meropenem showed a fluctuating downward trend after the intervention, but the IAC of imipenem showed an upward trend. The IAC of carbapenems showed a slowly decreasing trend after the intervention. Figure 2 shows the monthly values for IAC in the ICU. The IAC of carbapenems and imipenem showed a significant downward trend after the intervention. The IAC of meropenem showed a transient decrease after the intervention, followed by a fluctuating upward trend. Figure 3 shows the monthly values for ALoS. No significant trend change in ALoS was observed in all departments after the intervention, with the ICU showing a significant downward trend in ALoS.
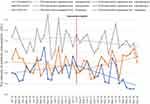 |
Figure 1 The change in the IAC of carbapenems per month pre- and post-intervention in all departments. |
 |
Figure 2 The change in the IAC of carbapenems per month pre- and post-intervention in the ICU. |
 |
Figure 3 The change in the ALoS per month pre- and post-intervention. |
Effects of the Intervention Targeting Carbapenem Prescriptions
Table 2 presents the detailed results of changes in levels and trends in each outcome indicator before and after the intervention. Figures 1–3 show that carbapenem consumption and the ALos peaked in certain seasons. Therefore the regression model took into account seasonality to control confounding factors. In addition, the results of the residual analysis showed no effect of auto-correlation in the four models.
 |
Table 2 Results of the Segmented Regression Analysis of IAC, Cumulative DDDs and ALoS |
The IAC of meropenem and imipenem per month showed a steady trend (coefficient = 0.01, p = 0.319; coefficient = 0.01, p = 0.553, respectively) before the intervention. After the intervention, there was a decreasing trend in the IAC of meropenem (coefficient = −0.03, p = 0.008) but an increasing trend for imipenem (coefficient = −0.02, p = 0.019). There was no significant difference in the level of change in IAC between meropenem and imipenem in all departments before and after the intervention. Cumulative DDDs (coefficient = −8.54, p = 0.087) and ALoS (coefficient =0.02, p = 0.551) showed a stable trend even after the intervention.
After the intervention, the IAC of carbapenems and imipenem in the ICU per month showed slight downward trends (coefficient = −0.36, p = 0.035; coefficient = −0.49, p = 0.025, respectively) and significantly reduced levels (coefficient = −9.65, p <0.001; coefficient = −6.82, p = 0.002, respectively). The level of cumulative DDDs in the ICU showed a significant decrease (coefficient = −133.60, p = 0.003) after the intervention, but the downward trend was not significant in the long term (coefficient = −7.62, p = 0.087). A declining trend (coefficient = −0.73, p < 0.001) in the ALoS was observed in the ICU each month after the intervention, but there was a non-significant increase (coefficient = 2.30, p = 0.089) in the level of change.
Discussion
The results of this study showed no significant benefits of the intervention in all departments during the 18-month post-intervention study period. However, we saw a significant downward trend in the IAC of meropenem (coefficient = −0.03, p = 0.008) in all departments, the IAC of imipenem showed an upward trend (coefficient = 0.02, p = 0.019). Interestingly, the effect of the intervention was evident in the ICU, with a significant downward trend in the IAC of carbapenem and imipenem (coefficient = −0.36, p = 0.035; coefficient = −0.49, p = 0.025, respectively) and the ALoS (coefficient = −0.73, p < 0.001). While confirming a considerable change in the IAC and the antibiotic consumption of carbapenems and the ALoS in all departments after the intervention, the interrupted time series analysis did not show a significant change in trend for the three study outcomes, which requires more attention and discussion.
Our study confirmed that the intervention was associated with a reduction in the IAC of meropenem, suggesting that the intervention, while not having a significant effect on overall prescription of carbapenem across all departments, had some effect on limiting the use of meropenem, in line with previous studies.30,31 Prescription restriction and audit were the core strategies of this intervention. Some studies have shown that prescription restrictions, particularly for single antibiotic classes, have proven to reduce antibiotic use, reduce mortality and shorten the ALoS.32–34 Auditing, with its components of intense communication and feedback, renders antibiotic stewardship programmes(ASP) effective.35,36 It is worth noting that previous antibiotic policies in China have targeted all antibiotics and lacked regulation of specific antibiotics, with limited intervention effects on the use of carbapenems.37,38 In many Asian hospitals, carbapenem-focused interventions for prevalent carbapenem-resistant A. baumannii may be more practical than widespread prescription restrictions.21 Therefore, compared to previous antibiotic stewardship policies, the interventions in this study are more targeted and represent a solid attempt to manage a single type of antibiotic.
However, in implementing the intervention, medical institutions also face several practical difficulties. For example, doctors with carbapenem prescribing authority must be highly motivated, willing to cooperate with the intervention and trust and accept pharmacists’ advice. A study conducted by the University of Pennsylvania showed that antimicrobial stewardship teams based on close collaboration between pharmacists and physicians had significantly higher recommendation appropriateness (87% vs 47%, respectively; p < 0.001) and clinical cure rates (64% vs 42%, respectively; p = 0.007) than non-team collaborating physicians.39 Nevertheless, collaborative efforts between physicians and pharmacists when prescribing and providing feedback is often inadequate, particularly in developing countries in Asia.40,41 In addition, filling the IFCP increases the workload of physicians resulting in omissions, errors or refills after prescribing. Although an employee is designated to collect, collate and provide feedback on the IFCP, it may still affect the effectiveness of interventions on carbapenem consumption and ALoS to some extent. In a follow-up study, we will consider simplifying the process of completing the IFCP and adding a carbapenem panel to the hospital’s infection control system to facilitate accessibility to the intervention.
In this study, the Interrupted Time-Series (ITS) results and the post-intervention regression line trends showed a significant decrease in IAC levels of carbapenems and imipenem in the ICU at the intervention transient, with both carbapenems and imipenem having much lower IAC than pre-intervention during the 18 months after the intervention. Therefore, we believe that the intervention achieved good effects in the ICU, suggesting that setting up a critical department and strengthening its management in interventions targeting carbapenems can improve prescription regulation and reduce carbapenem consumption.19 In the Asia-Pacific region, limited human and fiscal resources and the lack of information technology are regarded as the main barriers to effective ASPs.20 Hence, in ASP designs that focus on limited resources in departments with more severe antibiotic misuse, prioritising interventions for them may achieve more desirable outcomes. In this study, after selecting the ICU as the critical department, we placed it ahead of other departments in the collection, feedback and reporting process of the IFCP and provided regular feedback to the ICU director. While it is true that the better effect of the intervention in the ICU is inseparable from the ICU’s superior staffing and medical resource allocation, the effectiveness of the strategy of setting a critical department should not be overlooked.
To our knowledge, this is the first study to attempt to use ITS techniques to assess the impact of regulation on carbapenem use in China and to compare the variability of the effects of regulation between the entire department and the ICU.42 Firstly, our study used retrospective data and did not include details of treatments and interventions, such as medication appropriateness. Therefore, we were unable to evaluate the specifics of the national policy on physician guidance, which will be the goal of our future study. Secondly, a simultaneous control group was not included in this study because hospitals have only one ICU for the same condition. It is difficult to control for consistency of ICU interventions across hospitals. Therefore, we only carried out a before-and-after comparison analysis. Finally, it is well known that when one class of antibiotics is regulated, the use of other classes of antibiotics increases (the so-called “squeeze the antibiotic balloon”). Therefore, our subsequent studies should take into account how the use of other antibiotics changes as a result of carbapenem restrictions.
Conclusion
This study showed that regulation targeting carbapenem prescribing, although effective in reducing IAC for meropenem, was not significantly effective overall in reducing carbapenem prescribing in all departments. In the ICU, which is a critical department, the intervention reduced the IAC and ALoS of carbapenems, imipenem and achieved sound effects. This suggests that more targeted regulations should be introduced in future ASP for carbapenems, and that controls in the critical department with high and problematic carbapenem use should be strengthened.
Ethics Statement
The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China. As the study used anonymous, pooled, and retrospective data, the Ethics Committee waived the need for participants to provide written informed consent. The study complies with the Declaration of Helsinki.
Acknowledgments
The authors would like to sincerely thank the members involved in this paper for their help and support. Thanks to Janelle for editing this paper in English.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017;215:S28–S36. doi:10.1093/infdis/jiw282
2. ECDC. Antimicrobial resistance in the EU/EEA (EARS-Net)—AER for 2019. Available from: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019. Accessed July 04, 2021.
3. Stewardson A, Marimuthu K, Sengupta S, et al. Effect of carbapenem resistance on outcomes of bloodstream infection caused by Enterobacteriaceae in low-income and middle-income countries (PANORAMA): a multinational prospective cohort study. Lancet Infect Dis. 2019;19(6):601–610. doi:10.1016/S1473-3099(18)30792-8
4. Tumbarello M, Trecarichi EM, De Rosa FG, et al. Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrobial Chemotherapy. 2015;70(7):2133–2143. doi:10.1093/jac/dkv086
5. Cassini A, Högberg LD, Plachouras D, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66. doi:10.1016/S1473-3099(18)30605-4
6. Martin A, Fahrbach K, Zhao Q, Lodise T. Association between carbapenem resistance and mortality among adult, hospitalised patients with serious infections due to enterobacteriaceae: results of a systematic literature review and meta-analysis. Open Forum Infect Dis. 2018;5(7):ofy150. doi:10.1093/ofid/ofy150
7. Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014;20(9):821–830. doi:10.1111/1469-0691.12719
8. Arepyeva MA, Kolbin AS, Sidorenko SV, et al. A mathematical model for predicting the development of bacterial resistance based on the relationship between the level of antimicrobial resistance and the volume of antibiotic consumption. J Global Antimicrobial Resist. 2017;8:148–156. doi:10.1016/j.jgar.2016.11.010
9. Valencia C, Hammami N, Agodi A, et al. Poor adherence to guidelines for preventing central line-associated bloodstream infections (CLABSI): results of a worldwide survey. Antimicrob Resist Infect Control. 2016;5:49. doi:10.1186/s13756-016-0139-y
10. Goel N, Wattal C, Oberoi JK, Raveendran R, Datta S, Prasad KJ. Trend analysis of antimicrobial consumption and development of resistance in non-fermenters in a tertiary care hospital in Delhi, India. J Antimicrobial Chemotherapy. 2011;66(7):1625–1630. doi:10.1093/jac/dkr167
11. Meyer E, Gastmeier P, Deja M, Schwab F. Antibiotic consumption and resistance: data from Europe and Germany. Int J Med Microbiol. 2013;303(6–7):388–395. doi:10.1016/j.ijmm.2013.04.004
12. McLaughlin M, Advincula MR, Malczynski M, Qi C, Bolon M, Scheetz MH. Correlations of Antibiotic Use and Carbapenem Resistance in Enterobacteriaceae. Antimicrob Agents Chemother. 2013;57(10):5131–5133. doi:10.1128/AAC.00607-13
13. Wong D, Spellberg B. Leveraging antimicrobial stewardship into improving rates of carbapenem-resistant Enterobacteriaceae. Virulence. 2017;8(4):383–390. doi:10.1080/21505594.2016.1188234
14. Zou YM, Ma Y, Liu JH, et al. Trends and correlation of antibacterial usage and bacterial resistance: time series analysis for antibacterial stewardship in a Chinese teaching hospital (2009–2013). Eur J Clin Microbiol Infect Dis. 2015;34(4):795–803. doi:10.1007/s10096-014-2293-6
15. Xu J, Sun Z, Li Y, Zhou Q. Surveillance and correlation of antibiotic consumption and resistance of acinetobacter baumannii complex in a tertiary care hospital in Northeast China, 2003–2011. Int J Environ Res Public Health. 2013;10(4):1462–1473. doi:10.3390/ijerph10041462
16. Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci USA. 2018;115(15):E3463–E3470. doi:10.1073/pnas.1717295115
17. Lim C, Takahashi E, Hongsuwan M, et al. Epidemiology and burden of multidrug-resistant bacterial infection in a developing country. eLife. 2016;5:e18082. doi:10.7554/eLife.18082
18. Versporten A, Zarb P, Caniaux I, et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Health. 2018;6(6):E619–E629. doi:10.1016/S2214-109X(18)30186-4
19. Karanika S, Paudel S, Grigoras C, Kalbasi A, Mylonakis E. Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital-based antimicrobial stewardship programs. Antimicrob Agents Chemother. 2016;60(8):4840. doi:10.1128/AAC.00825-16
20. Honda H, Ohmagari N, Tokuda Y, Mattar C, Warren DK. Antimicrobial stewardship in inpatient settings in the asia pacific region: a systematic review and meta-analysis. Clin Infect Dis. 2017;64(suppl_2):S119–S126. doi:10.1093/cid/cix017
21. Apisarnthanarak A, Kwa AL-H, Chiu C-H, et al. Antimicrobial stewardship for acute-care hospitals: an Asian perspective. Infect Control Hospital Epidemiol. 2018;39(10):1237–1245. doi:10.1017/ice.2018.188
22. Hsu L-Y, Apisarnthanarak A, Khan E, Suwantarat N, Ghafur A, Tambyah PA. Carbapenem-resistant acinetobacter baumannii and enterobacteriaceae in South and Southeast Asia. Clin Microbiol Rev. 2017;30(1):1–22. doi:10.1128/CMR.00042-16
23. Apisarnthanarak A, Lapcharoen P, Vanichkul P, Srisaeng-Ngoen T, Mundy LM. Design and analysis of a pharmacist-enhanced antimicrobial stewardship program in Thailand. Am J Infect Control. 2015;43(9):956–959. doi:10.1016/j.ajic.2015.05.011
24. Macdougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638–656. doi:10.1128/CMR.18.4.638-656.2005
25. National Health Commission. Notice from the General Office of the National Health and Family Planning Commission on Further Strengthening the Management of Clinical Application of Antibacterial Drugs to Curb Bacterial Drug Resistance. National Health Commission of the People’s Republic of China; 2017.
26. World Health Organization. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD). World Health Organization; 2003.
27. Tang Y, Liu C, Zhang Z, Zhang X. Effects of prescription restrictive interventions on antibiotic procurement in primary care settings: a controlled interrupted time series study in China. Cost Effectiveness Resource Allocation. 2018;16:1. doi:10.1186/s12962-018-0086-y
28. World Health Organization. International Statistical Classification of Diseases and Related Health Problems.
29. Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6):S38–S44. doi:10.1016/j.acap.2013.08.002
30. Garcia-Rodriguez JF, Bardan-Garcia B, Pena-Rodriguez MF, Alvarez-Diaz H, Marino-Callejo A. Meropenem antimicrobial stewardship program: clinical, economic, and antibiotic resistance impact. Eur J Clin Microbiol Infect Dis. 2019;38(1):161–170. doi:10.1007/s10096-018-3408-2
31. Mani NS, Lan KF, Jain R, et al. Post-prescription review with threat of infectious disease consultation and sustained reduction in meropenem use over four years. Clin Infect Dis. 2020;1:5. doi:10.1093/cid/ciaa1279
32. Yusef D, Hayajneh WA, Bani Issa A, et al. Impact of an antimicrobial stewardship programme on reducing broad-spectrum antibiotic use and its effect on carbapenem-resistant Acinetobacter baumannii (CRAb) in hospitals in Jordan. J Antimicrobial Chemotherapy. 2021;76(2):516–523. doi:10.1093/jac/dkaa464
33. Davey P, Marwick CA, Scott CL, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Sys Rev. 2017;2(2):CD003543. doi:10.1002/14651858.CD003543.pub4
34. Li Z, Cheng B, Zhang K, et al. Pharmacist-driven antimicrobial stewardship in intensive care units in East China: a multicenter prospective cohort study. Am J Infect Control. 2017;45(9):983–989. doi:10.1016/j.ajic.2017.02.021
35. Yeo C-L, Chan DS-G, Earnest A, et al. Prospective audit and feedback on antibiotic prescription in an adult hematology-oncology unit in Singapore. Eur J Clin Microbiol Infect Dis. 2012;31(4):583–590. doi:10.1007/s10096-011-1351-6
36. Baur D, Gladstone BP, Burkert F, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17(9):990–1001. doi:10.1016/S1473-3099(17)30325-0
37. Wang X, Tang Y, Liu C, Liu J, Cui Y, Zhang X. Effects of restrictive-prescribing stewardship on antibiotic consumption in primary care in China: an interrupted time series analysis, 2012–2017. Antimicrob Resist Infect Control. 2020;9(1):159. doi:10.1186/s13756-020-00821-7
38. Chrysou K, Zarkotou O, Kalofolia S, et al. First-year results of an antibiotic stewardship program in a Greek tertiary care hospital. Eur J Clin Microbiol Infect Dis. 2018;37(2):333–337. doi:10.1007/s10096-017-3137-y
39. Gross R, Morgan AS, Kinky DE, Weiner M, Gibson GA, Fishman NO. Impact of a hospital-based antimicrobial management program on clinical and economic outcomes. Clin Infect Dis. 2001;33(3):289–295. doi:10.1086/321880
40. Sakeena MHF, Bennett AA, McLachlan AJ. Enhancing pharmacists’ role in developing countries to overcome the challenge of antimicrobial resistance: a narrative review. Antimicrob Resist Infect Control. 2018;7(1):63. doi:10.1186/s13756-018-0351-z
41. Davey P, Marwick C, Scott C, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Sys Rev. 2017;2:576. doi:10.1002/14651858.CD003543.pub4
42. Sun J. Systematic review of interventions on antibiotic prophylaxis in surgery in Chinese hospitals during 2000–2012. J Evid Based Med. 2013;6(3):126–135. doi:10.1111/jebm.12048
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
