Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Effects of Psychiatric Disease Severity and Clinical Characteristics on Duration of High Violence Risk: A Perspective on Violence Prevention in the Psychiatric Ward
Authors Chang PY , Chen JH , Cheng HW, Wang YC
Received 2 January 2023
Accepted for publication 16 March 2023
Published 27 March 2023 Volume 2023:19 Pages 663—671
DOI https://doi.org/10.2147/NDT.S403388
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Ping-Ying Chang,1,2 Jian-Hong Chen,1– 3 Hui-Wen Cheng,1 Yen-Chin Wang4
1Department of Psychiatry, Chang-Gung Medical Foundation Keelung Chang-Gung Memorial Hospital, Keelung, Taiwan, Republic of China; 2School of Medicine, Chang Gung University, Taoyuan, Taiwan, Republic of China; 3Doctoral Program for Transnational Sport Management and Innovation, National Taiwan Sport University, Taoyuan, Taiwan, Republic of China; 4Department of Psychiatry, National Taiwan University Hospital, Hsin-Chu Branch, Hsinchu, Taiwan, Republic of China
Correspondence: Jian-Hong Chen, Email [email protected]
Objective: Prevention, de-escalation, and management of violence in the acute psychiatric ward is essential. Few studies have focused on differences in the duration of high-violence risk between different profiles of high-violence risk. This study aimed to analyze the data of high-violence patients and duration of high-violence risk to provide a new perspective on violence prevention, de-escalation and management.
Methods: This retrospective observational cohort study included 171 patients who were treated in the acute psychiatric ward of Keelung Chang Gung Memorial Hospital between January 2016 and June 2020, and who were assessed daily as having high violence risk. All patient data were collected from electronic hospital records (eg, age, gender, diagnosis, violence history, self-harm history, and admission condition (involuntary admission, discharged against medical advice). Between-group differences in disease severity, use of antipsychotics and benzodiazepine, and duration of high violence risk were analyzed using regression analysis.
Results: Only patients’ age was significantly associated with duration of high-violence risk (P = 0.028), making it predictive of longer duration of high-violence risk. In patients with schizophrenia spectrum disorder or bipolar disorder, higher severity was significantly associated with longer duration of high-violence risk (P = 0.007, P = 0.001, respectively).
Conclusion: Only age is a predictor of longer duration of violence risk in psychiatric patients, although higher severity is associated with higher violence risk. Study results may help management and healthcare staff better understand how quickly or slowly violence risk will decrease and may improve efficient use of healthcare resources and individualized patient-centered care.
Keywords: acute psychiatric ward, predictor, risk assessment, severity, violence risk
Plain Language Summary
High violence risk causes tremendous physical and mental burden on both patients and healthcare staff in the acute psychiatric ward. The long duration of high violence risk makes this condition a constant battle. Therefore, we sought to determine if there were any predictors of the duration of high violence risk or any interventions that may be effective. This study found that only age is a predictor of the duration of high violence risk among patients in the acute psychiatric ward, while patients with more severe schizophrenia or bipolar disorder have a longer high-risk period. Intramuscular injections of antipsychotics and benzodiazepines can temporarily reduce symptoms, but not the duration of high violence risk. For cases at high risk of violence, adequate treatment of the major psychiatric disorder is recommended. By understanding these factors, healthcare staff may be better equipped to prevent violent incidents, provide individualized care, and intervene more effectively.
Introduction
Violence behavior is frequent among psychiatric inpatients and exposes healthcare staff to significant physical and psychological burdens as well as significant social impact.1 Regardless of direct or vicarious exposure to aggression, the possible impact of healthcare workplace aggression may encompass adverse effects on quality, safety, and accessibility of care.2,3 Violence in the psychiatric ward is common and widespread, and prevention, de-escalation, and management of violence risk are important issues.4,5 Based on literature review, most previous studies focused on assessing the incidence of violence over time.
Although few risk factors actually predict future occurrence of violence accurately, and underlying mechanisms of violence are not well understood,6 certain statistical risk factors of violence have been identified, including male gender, diagnosis of major mental illness, history of violence, involuntary hospital admission, drug or alcohol abuse, antisocial personality disorder, and intellectual disability.7–14 Violence evaluation check lists, including the Brøset Violence Checklist and the Historical, Clinical and Risk Management-20 (HCR-20) instrument, show violence risk predictors as young age, relationship instability, employment problems, impulsivity, criminal history and so on. Also, current violence risk assessment tools have been developed for heterogeneous and non-psychopathic populations.15 However, the clinical use of violence risk assessment tools is not widely adopted, especially in Asia.16 Different violence risk assessment tools have significant differences in their predictive rates, and the same tool may have different predictive rates for violence in different regions.17 These factors make it difficult to integrate various studies.
Based on the statistics of our acute psychiatric ward, the total patient-days of hospitalization included in this study from 2016 to 2020 were 25,548 person-days. In addition, the total person-days of high violence risk were 1669 person-days, and there were a total of 20 incidents of physical aggression. According to some research,18,19 individualized nursing management based on the conditions of different patients can reduce the incidence of violence among patients. Our ward also provides relevant nursing management according to the degree of violence risk of different patients (see the Appendix). Specifically, for patients with a higher risk of violence, the nurses will visit the patients more intensively and conduct stricter safety checks. At the same time, they will be more careful to keep distance and avoid being alone when contacting patients. From the above data combined with the nursing management mentioned above, it can be seen that the person-days of high violence risk have caused a tremendous physical and mental burden on the healthcare staff in the ward. Furthermore, from 2016 to 2020, there were 380 incidents of involuntary restraint and 842 incidents of involuntary isolation in this ward. Although not all of these incidents were related to violent events, they to some extent reflect the suffering of patients and the level of tension in the ward.
While education and training about preventing and minimizing workplace aggression toward healthcare workers may increase personal knowledge and positive attitudes among healthcare staff, the combination of education and training may not affect actual workplace aggression against healthcare workers.20 Preventing individuals with severe mental illness from committing violence may provide huge benefits in reducing the risk of violence, as well as protecting the victims of violence.1 In clinical practice, understanding the predictors of violence risk may provide healthcare staff with expectations of how quickly or slowly violence risk may decrease in clinical practice.
While numerous studies7–13,21 have described predicting the incidence of violence over a period of time, only a few have focused on differences in the duration of high violence risk between different profiles of high violence risk cases. This study aimed to analyze the data of high violence patients and their duration of high violence risk to provide a new perspective on violence prevention,14,22 de-escalation and management. The use of antipsychotic and benzodiazepine intramuscular (IM) injections was also analyzed to determine whether or not these medications decreased the duration of high violence risk. Results of these research objectives may be useful to help management personnel and clinicians arrange staffing of the ward, implement nursing principles for acute psychiatric care, and improve the efficient use of healthcare resources and individualized patient-centered care.
Methods
Study Design and Sample
This retrospective observational cohort study enrolled 171 patients treated in the acute psychiatric ward of Keelung Chang Gung Memorial Hospital between January 2016 and June 2020, and who were assessed daily by psychiatrists as having high risk of violence based on the ward-routine checklist of violence risk. Patients’ background data were collected from their electronic hospital records (including age, gender, diagnosis, education level, occupation, etc.), violence history, self-harm history, admission condition (involuntary admission, discharged against medical advice, etc.). Duration of high violence risk was defined as duration from the day a patient’s violence risk was evaluated as high, to the day the patient’s violence risk was de-escalated to moderate.
After data collection, 13 patients were excluded from analyses because of high risk of violence at discharge (discharge against medical advice or transfer to another ward or hospital), resulting in a final sample size of 158 patients. Subjects’ background information, medical history, and admission condition were analyzed to find possible predictive factors to predict duration of high risk of violence.
Ethical Considerations
The study protocol was approved by the Institutional Review Board (IRB) of the Keelung Chang Gung Memorial Hospital (IRB No.: 202201395B0). The study met the standards of the Helsinki Declaration. Because the study used retrospective deidentified data, signed informed consent from patients was waived.
Subgroup Analysis
Subgroup analysis was also performed because the diagnoses of schizophrenia spectrum disorder and bipolar disorder represented the majority of the patient population. In subgroup analysis, subjects were grouped according to different diagnoses, disease severity, and whether or not they received IM injections of antipsychotics or benzodiazepine during high violence risk duration. Cases of schizophrenia spectrum disorder were further separated into four groups based on severity scores of the Brief Psychiatry Rating Scale (BPRS), which assesses 18 symptoms, with scores for each ranging from 1 to 7 based on severity. The total score of all symptoms ranges from 0 to 70 as follows: Ill > 25, Moderately ill ≥ 35, Markedly ill ≥ 50, Severely ill ≥ 70).23 Cases of bipolar disorder were separated into five groups according to severity scores of the Young Mania Rating Scale (YMRS) based on mania symptoms, for which the total score ranges from 0 to 70, with higher scores indicating higher severity (Ill > 12, Minimal symptoms ≥ 13, Mild mania ≥ 20, Moderate mania ≥ 26, Severe mania ≥ 38).24
Differences Between Subjects with Different Disease Severity Levels
Further analysis was done to determine differences, as follows: (1) whether differences were found in the duration of high-violence risk by groups of different severity levels evaluated at admission; (2) whether differences existed in whether or not subjects receive IM injections during the period of high violence risk by groups of different severity levels evaluated at admission, and (3) whether differences were noted in the duration of high-violence risk by groups receiving IM injections or not during the period of high violence risk. Through these analyses, associations between the different severity groups were explored, including the administration of antipsychotic and benzodiazepine IM injections, and the duration of high risk of violence in patients with schizophrenia or bipolar disorder.
Measurements
All included patients were evaluated by psychiatrists for violence risk using the Ward-routine Violent Behavior Evaluation Scale. This checklist was developed by psychiatrists in the acute psychiatric ward of the study hospital. The scale includes 15 evaluation items, including violence history, physical signs, verbal signs, emotional signs, substance abuse, active suicidal behavior, etc. (See the Appendix). The scale has three grades of violence risk—mild, moderate, and high— which are determined based on final scores of the above items. Mild violence risk was assigned to subjects with fewer than 5 evaluated items, moderate violence risk was assigned to subjects with 5–10 evaluated items, and high violence risk was assigned to subjects with 10 or more evaluation items.
Statistical Analysis
The duration of high violence risk as a continuous variable was collected using natural logarithm convergence to conform to the normal distribution test. Univariate analysis for each variable was performed. Backward selection method was used to avoid false positives and overfitting problems. Univariable and multivariable regression analyses were performed to compare groups and to determine meaningful predictors. Associations between the different degrees of disease severity, the administration of antipsychotic and benzodiazepine IM injections, and the duration of high risk of violence in patients with schizophrenia or bipolar disorder were also evaluated by regression analysis to determine differences between disease severity and duration of high violence risk. The independent sample t-test was used to determine differences in high violence risk duration between groups with or without injections. Chi-square test was used to determine differences in disease severity between groups receiving IM injections or not. All statistical analysis was performed using SPSS software (SPSS, Chicago, IL, USA). P < 0.05 was established as statistical significance.
Results
Subjects’ baseline demographic and clinical data are displayed in Table 1. Overall, 158 patients were included, with ages ranging from 17 to 89 (42.3 ± 14.5) and 62.0% males. Diagnoses included schizophrenia spectrum disorder (59.5%), bipolar disorder (21.5%), alcohol/substance use disorder (10.8%), autistic spectrum disorder (3.1%), and intellectual disability (10.8%). Other demographic data (lifestyle, education) can be found in Table 1. Patients’ admission conditions during hospitalization included involuntary admission (5.7%), discharge against medical advice (9.6%), and admission for more than 30 days. History of violence was 84.2%, self-harm 31.0%. Mean duration of high violence risk was 9.3± 8.0 days.
 |
Table 1 Descriptive Statistics of Subjects’ Demographic and Clinical Characteristics |
Univariate analysis of potential predictors of high violence risk duration revealed that associated variables were significantly associated with duration of high violence risk (Table 2), including age (B = −0.009, P = 0.036), BMI (B = −0.016, P = 0.153), self-harm history (B = 0.227, P = 0.079), history of discharge against medical advice (B = 0.371, P = 0.068), and history of admission for more than 30 days (B = 0.170, P = 0.176). However, backward selection of potential predictors of high-violence risk duration showed that only age (B = −0.009, P = 0.028) was significantly associated with duration of high violence risk (Table 3).
 |
Table 2 Univariate Analysis of Potential Predictors of High-Violence-Risk Duration_ln |
 |
Table 3 Backward Selection of Potential Predictors of High-Violence-Risk Duration_ln |
In patients with schizophrenia spectrum disorder or bipolar disorder, those with higher severity levels had longer duration of high violence risk (Table 4). Schizophrenia patients who were markedly ill (P = 0.007) and severely ill (P = 0.001) had longer duration of high-violence risk than those who were mildly ill. In cases of bipolar disorder, those with severe mania had longer duration of high violence risk than those with mild mania (P = 0.040).
 |
Table 4 Differences Between Disease Severity and High-Violence-Risk Duration_ln |
Patients who received IM injections of antipsychotics and benzodiazepine had longer duration of high violence risk than those who did not (Table 5). Among patients diagnosed as schizophrenia spectrum disorder, the group receiving antipsychotics and benzodiazepine IM injections during high violence risk had longer durations of high violence risk than the non-injection group (P = 0.001). Among patients diagnosed as bipolar disorder, those who received antipsychotics and benzodiazepine IM injections during high violence risk duration had longer duration of high violence risk than those who did not (P = 0.01).
 |
Table 5 Differences in High-Violence-Risk Duration_ln Between Groups with or without IM Injection of Antipsychotics or Benzodiazepine |
No differences were found among high violence risk patients with schizophrenia spectrum disorder and bipolar disorder who had higher and lower disease severity whether or not they received antipsychotic and benzodiazepine IM injections (Table 6). Among patients diagnosed with schizophrenia spectrum disorder, no differences were found between those receiving IM injections and those who did not between groups with different disease severity levels (P = 0.514). Also, among patients diagnosed with bipolar disorder, no differences were found between those receiving IM injections or not between groups with different disease severity levels (P = 0.056).
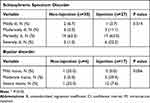 |
Table 6 Differences in IM Injection of Antipsychotics or Benzodiazepine or Not Between Subjects with Different Disease Severity |
Discussion
In the present study, age was the only statistically significant positive predictor of duration of high violence risk. In addition, the data of high violence risk patients with schizophrenia spectrum disorder and bipolar disorder revealed that higher severity was associated with longer duration of high violence risk, and antipsychotics and benzodiazepine IM injections during hospitalization were also associated with longer duration of high-violence risk than those who did not receive injections. Also, no significant differences were found in the severity of illness and the administration of IM injections of antipsychotic and benzodiazepine or not during periods of high violence risk. It can be inferred that high violence risk patients diagnosed with schizophrenia spectrum disorder and bipolar disorder require active treatment of the disease first. Although antipsychotics and benzodiazepines can temporarily calm patients, they do not contribute significant benefit to the long-term course of the disease or reductions in the duration of high-violence risk.25
Although multiple studies have shown associations between predicted risk of violence and diagnosis of major mental illness7,9,12 and violence history,11,13 these predictors were not significantly associated with duration of high violence risk in the present study. Therefore, as stated in previous studies,13,14,26 the causes of violence risk and its duration are complex, and it is difficult to predict the probability of violence behavior and the duration of high risk using simple variables.
In the present study, in patients with schizophrenia spectrum disorder or bipolar disorder, subjects with higher disease severity had longer duration of high violence risk. A previous study reported high scores on the Positive and Negative Syndrome Scale (PANSS) or BPRS that appear to increase risk of aggression.21 Another study also found that persistent physical aggression before and during hospitalization was associated with higher overall BPRS scores.22
The most commonly used interventions in the management of violent patients are physical restraint, seclusion, and medication.27 Physical restraint and seclusion are shown to have no therapeutic value and may even contribute to post-traumatic stress, serious physical injury, and higher morbidity and mortality.28,29 In the present study, among patients with schizophrenia spectrum disorder or bipolar disorder who had high violence risk, those who received antipsychotics and benzodiazepine IM injections had longer duration of high violence risk than those who did not. The effects of IM injections on incident risk appear to be primarily short-term, and the risk never falls significantly below baseline risk.25
In high violence risk patients in the present study who had schizophrenia spectrum disorder and bipolar disorder, no significant differences were noted between higher severity and lower severity levels, whether or not patients received antipsychotic and benzodiazepine IM injections. This observation suggests that IM injections of these agents may achieve effective sedation for a short period of time to help protect patients and staff from physical injury and to promote the management of acute psychiatric wards. However, in order to reduce the duration of the high risk of violence, treating the major mental illness itself is the most important thing.
Psychiatric ward management varies corresponding to between-patient differences in violence risk. For patients with mild violence risk, nursing management principles recommend observing patients according to the principles of ward routines, conducting weekly security checks and implementing general nursing care principles. For patients with moderate violence risk, nursing management principles require managing not only mild violence risk but also conducting daily security checks, keeping a proper distance from the patient, using padded rooms, physical restraint or medication if needed, among other management methods. For patients with high violence risk, nursing management principles advise monitoring patients every 15 minutes, security checks every 8 hours, and to avoid approaching these patients alone. Overall, management of high violence risk involves much time, human costs, and psychological stress of the healthcare staff. Thus, determining the predictors of the duration of violence risk and developing possible strategies to de-escalate the violence risk to a lower grade are immediate and necessary.
The present study has several limitations. First, this study was retrospective and cross‐sectional in nature, which limit inferences of causality and generalization to other populations. Because of the limitations of medical records (such as between-patient differences in length of hospital stay and in comorbidities or medications), the variables in this study also have limitations, many of which are dichotomous variables, while more detailed polytomous variables are lacking. Also, data collection was only limited to the acute psychiatric ward of a single regional hospital, and the patient population was limited to patients with psychiatric diagnoses, so the data may not be applicable to other ethnicities and regions. Further, although this study discovered that higher severity levels may have longer duration of high violence risk in patients with schizophrenia spectrum disorder and bipolar disorder, patients with higher severity levels and patients receiving antipsychotic and benzodiazepine IM injections may have longer duration of high violence risk; however, this study only found differences between groups, but not in associations between these variables or how they work. Future studies should consider the dynamic factors, such as patient’s current state and the context, and explore the potential for associations between different factors and duration of high violence risk. Another potential limitation is that the patients included in this study all had reductions in violence risk from high to moderate, which may lead to selection bias. Results of this study cannot be interpreted as a process from moderate to low risk of violence and from low risk of violence to release.
The other limitation of present study is that the ward-routine scale used to assess high-violence risk in this study was developed by the hospital psychiatrists themselves, and its reliability has not yet been tested. In fact, different violence risk assessment tools have significant differences in their predictive rates, and the same tool may have different predictive rates for violence in different regions.17 Little evidence is available to support the use of existing violence risk assessment tools for people with mental illness in China.30 Clinical use of violence risk assessment tools is lower in Asia than in Europe and North America.16 Therefore, developing a simpler, more accurate and appropriate scale of violence risk assessments for Asians is a top priority. The present study focused mainly on predictors of high violence risk based on patients’ conditions and did not include healthcare staff factors and environment of the psychiatric ward in the analyses. Violence behavior in the psychiatric ward has been linked to interpersonal styles of individual healthcare staff, a lower sense of fairness, and less involvement in the outside world.31 Although no strong causal relationships were found between design of the psychiatric ward and clinical outcomes, private spaces and intimate surroundings may contribute to patients’ health status.32 Therefore, these factors will likely be given more prominence and incorporated in future research of violence.
Conclusions
Results of the present study identified that only age is a predictor of duration of high violence risk among psychiatric patients. Other factors such as patients’ gender, diagnosis, education level, occupation, violence or self-harm history, and admission condition (involuntary admission, discharge against medical advice) were not associated with duration of high violence risk. For cases at high risk of violence, adequate treatment of the major psychiatric disorder is recommended. IM injections of antipsychotics and benzodiazepine may temporarily reduce symptoms, but not the duration of high risk of violence. In clinical practice, these findings support more efficient use of healthcare resources and more appropriate planning for different case characteristics, including de-escalation techniques, regular security checks, IM or oral forms of medications, restraint, isolation, and more. Finally, the causes of violence are complex, and more research is needed to complete causal and theoretical constructions. Future directions for further research include developing a simpler, more accurate and appropriate scale of violence risk assessment for Asians, and possibly analyzing more factors of the healthcare staff and psychiatric ward environment in relation to the duration of high violence risk. Other intervention variables, including physical restraint, de-escalation techniques and separate room isolation, could also be analyzed in the further research.
Acknowledgments
The authors would like to thank Ching-Yen Chen, M.D. Professor (Chang Gung University, Taiwan), and National Science Council of Taiwan (NMRPG2M0051) for writing/editorial assistance with this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Senior M, Tsiachristas A, Fazel S. The economic impact of violence perpetration in severe mental illness: a retrospective, prevalence-based analysis in England and Wales. Lancet Public Health. 2020;5(2):e99–e106. doi:10.1016/S2468-2667(19)30245-2
2. Hills D, Joyce CM. Workplace aggression in clinical medical practice: associations with job satisfaction, life satisfaction and self-rated health. Med J Aust. 2014;201(9):535–540. doi:10.5694/mja13.00152
3. Dupré KE, Dawe KA, Barling J. Harm to those who serve: effects of direct and vicarious customer-initiated workplace aggression. J Interpers Violence. 2014;29(13):2355–2377. doi:10.1177/0886260513518841
4. Roca RP, Charen B, Boronow J. Ensuring staff safety when treating potentially violent patients. JAMA. 2016;316(24):2669–2670. doi:10.1001/jama.2016.18260
5. Odes R, Chapman S, Harrison R, et al. Frequency of violence towards healthcare workers in the United States’ inpatient psychiatric hospitals: a systematic review of literature. Int J Ment Health Nurs. 2021;30(1):27–46. doi:10.1111/inm.12812
6. Volavka J. The neurobiology of violence: an update. J Neuropsychiatry Clin Neurosci. 1999;11(3):307–314. doi:10.1176/jnp.11.3.307
7. Fazel S, Smith EN, Chang Z, et al. Risk factors for interpersonal violence: an umbrella review of meta-analyses. Br J Psychiatry. 2018;213(4):609–614. doi:10.1192/bjp.2018.145
8. Moberg T, Stenbacka M, Tengström A, et al. Psychiatric and neurological disorders in late adolescence and risk of convictions for violent crime in men. BMC Psychiatry. 2015;15:299. doi:10.1186/s12888-015-0683-7
9. Sariaslan A, Larsson H, Fazel S. Genetic and environmental determinants of violence risk in psychotic disorders: a multivariate quantitative genetic study of 1.8 million Swedish twins and siblings. Mol Psychiatry. 2016;21(9):1251–1256. doi:10.1038/mp.2015.184
10. Fazel S, Gulati G, Linsell L, et al. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8):e1000120. doi:10.1371/journal.pmed.1000120
11. Large MM, Nielssen O. Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2011;125(2–3):209–220. doi:10.1016/j.schres.2010.11.026
12. Cornaggia CM, Beghi M, Pavone F, et al. Aggression in psychiatry wards: a systematic review. Psychiatry Res. 2011;189(1):10–20. doi:10.1016/j.psychres.2010.12.024
13. Wolf A, Fanshawe TR, Sariaslan A, et al. Prediction of violent crime on discharge from secure psychiatric hospitals: a clinical prediction rule (FoVOx). Eur Psychiatry. 2018;47:88–93. doi:10.1016/j.eurpsy.2017.07.011
14. Dack C, Ross J, Papadopoulos C, et al. A review and meta-analysis of the patient factors associated with psychiatric in-patient aggression. Acta Psychiatr Scand. 2013;127(4):255–268. doi:10.1111/acps.12053
15. Fazel S. The scientific validity of current approaches to violence and criminal risk assessment. In: de Keijser JW, Roberts JV, Ryberg J, editors. Predictive Sentencing: Normative and Empirical Perspectives. Oxford: Hart Publishing; 2019:197–212.
16. Singh JP, Desmarais SL, Hurducas C, et al. International perspectives on the practical application of violence risk assessment: a global survey of 44 countries. Int J Forensic Ment Health. 2014;13(3):193–206. doi:10.1080/14999013.2014.922141
17. Ramesh T, Igoumenou A, Vazquez Montes M, et al. Use of risk assessment instruments to predict violence in forensic psychiatric hospitals: a systematic review and meta-analysis. Eur Psychiatry. 2018;52:47–53. doi:10.1016/j.eurpsy.2018.02.007
18. Urheim R, Palmstierna T, Rypdal K, et al. Violence rate dropped during a shift to individualized patient-oriented care in a high security forensic psychiatric ward. BMC Psychiatry. 2020;20(1):200. doi:10.1186/s12888-020-02524-0
19. Gaynes BN, Brown CL, Lux LJ, et al. Preventing and de-escalating aggressive behavior among adult psychiatric patients: a systematic review of the evidence. Psychiatr Serv. 2017;68(8):819–831. doi:10.1176/appi.ps.201600314
20. Geoffrion S, Hills DJ, Ross HM, et al. Education and training for preventing and minimizing workplace aggression directed toward healthcare workers. Cochrane Database Syst Rev. 2020;9(9):Cd011860. doi:10.1002/14651858.CD011860.pub2
21. Weltens I, Bak M, Verhagen S, et al. Aggression on the psychiatric ward: prevalence and risk factors. A systematic review of the literature. PLoS One. 2021;16(10):e0258346. doi:10.1371/journal.pone.0258346
22. Amore M, Menchetti M, Tonti C, et al. Predictors of violent behavior among acute psychiatric patients: clinical study. Psychiatry Clin Neurosci. 2008;62(3):247–255. doi:10.1111/j.1440-1819.2008.01790.x
23. Leucht S, Engel RR, Davis JM, et al. Equipercentile linking of the brief psychiatric rating scale and the clinical global impression scale in a catchment area. Eur Neuropsychopharmacol. 2012;22(7):501–505. doi:10.1016/j.euroneuro.2011.11.007
24. Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi:10.1192/bjp.133.5.429
25. Gao YN, Oberhardt M, Vawdrey D, et al. Medication use and physical assaults in the psychiatric emergency department. J Clin Psychiatry. 2021;83(1). doi:10.4088/JCP.21m13970
26. Large M, Nielssen O. Assessing risk of suicide and aggression in hospitals: same but different. Acta Psychiatr Scand. 2013;128(1):101. doi:10.1111/acps.12127
27. Cowman S, Björkdahl A, Clarke E, et al. A descriptive survey study of violence management and priorities among psychiatric staff in mental health services, across seventeen european countries. BMC Health Serv Res. 2017;17(1):59. doi:10.1186/s12913-017-1988-7
28. Steinert T, Birk M, Flammer E, et al. Subjective distress after seclusion or mechanical restraint: one-year follow-up of a randomized controlled study. Psychiatr Serv. 2013;64(10):1012–1017. doi:10.1176/appi.ps.201200315
29. Sailas E, Fenton M. Seclusion and restraint for people with serious mental illnesses. Cochrane Database Syst Rev. 2000;2000(2):Cd001163. doi:10.1002/14651858.CD001163
30. Gaynes BN, Brown C, Lux LJ, et al. AHRQ comparative effectiveness reviews. In: Strategies to De-Escalate Aggressive Behavior in Psychiatric Patients. Agency for Healthcare Research and Quality (US): Rockville (MD); 2016.
31. Ireland CA, Ireland JL, Jones NS, et al. Predicting security incidents in high secure male psychiatric care. Int J Law Psychiatry. 2019;64:40–52. doi:10.1016/j.ijlp.2019.01.004
32. Papoulias C, Csipke E, Rose D, et al. The psychiatric ward as a therapeutic space: systematic review. Br J Psychiatry. 2014;205(3):171–176. doi:10.1192/bjp.bp.114.144873
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
