Back to Journals » Drug Design, Development and Therapy » Volume 17
Effects of Combined Use of Salbutamol/Budesonide in Thoracic Surgery on Postoperative Myocardial Injury (MINS) – A Prospective Randomized Clinical Trial
Authors Lin S , Zhang Y, Huang X , Zhang X, Cheng E, Zhou Z, Liu J
Received 24 January 2023
Accepted for publication 24 March 2023
Published 1 April 2023 Volume 2023:17 Pages 1025—1036
DOI https://doi.org/10.2147/DDDT.S403638
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Shuchi Lin,1,* Ying Zhang,1,* Xiaofan Huang,1,* Xiaohan Zhang,1 Erhong Cheng,1 Zhaoyun Zhou,2 Jindong Liu1,3– 5
1Department of Anesthesiology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, Jiangsu, People’s Republic of China; 2Department of Anesthesiology, The Affiliated Taian City Central Hospital of Qingdao University, Taian, Shandong, People’s Republic of China; 3Jiangsu Province Key Laboratory of Anesthesiology, Xuzhou Medical University, Xuzhou, Jiangsu, People’s Republic of China; 4Jiangsu Province Key Laboratory of Anesthesia and Analgesia Application Technology, Xuzhou Medical University, Xuzhou, Jiangsu, People’s Republic of China; 5NMPA Key Laboratory for Research and Evaluation of Narcotic and Psychotropic Drugs, Xuzhou Medical University, Xuzhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jindong Liu, Department of Anesthesiology, The Affiliated Hospital of Xuzhou Medical University, Huaihai Road West, Quanshan District, Xuzhou, Jiangsu, People’s Republic of China, Tel +86-13951355136, Email [email protected]
Purpose: This study aims to investigate whether the administration of salbutamol/budesonide reduced the incidence of myocardial injury in thoracic surgery.
Methods: The randomized controlled trial included 298 patients over 45 and at high-risk for cardiovascular complications after lobectomy. Patients in the experimental group were treated with salbutamol/budesonide after anesthesia induction with fiberoptic bronchoscope. The primary outcome was the incidence rates of myocardial injury, assessed before and three days after the operation. The secondary outcome was respiratory function at each time point during the operation, including lung compliance and arterial partial pressure of oxygen, postoperative pulmonary and cardiovascular complications, hospital stay, pain score, and analgesic dosage.
Results: In the control group, the incidence of myocardial injury was 57/150 (38%), while that in the experimental group was 33/148 (22%); compared between the two groups, the difference in the incidence of myocardial injury was statistically significant. The dynamic compliance and static compliance at half an hour after the start of surgery in the experimental group were significantly improved. Before leaving the operating room, the difference in arterial oxygen partial pressure between the two groups was statistically significant.
Conclusion: Intraoperative administration of salbutamol/budesonide reduced the incidence of myocardial injury after thoracic surgery, improved lung function, and reduced the incidence of postoperative pulmonary complications.
Keywords: salbutamol/budesonide, myocardial injury, thoracic surgery, cardiovascular risk, hsTnT, prediction model
Introduction
Myocardial injury after non-cardiac surgery (MINS) based on elevated troponin has been identified as the most common perioperative cardiac complication. MINS was the leading reason for increased postoperative complications, prolonged hospitalization, and major adverse cardiovascular events 30 days after operation.1 Among all patients over 45 who accepted in-hospital non-cardiac surgery, approximately 8% of people had significant cardiovascular complications.2,3 Adverse cardiovascular events include myocardial infarction and asymptomatic myocardial injury within 30 days after non-cardiac surgery.4 The largest cohort study of cardiovascular events (VISION) in non-cardiac patients (over 40,000 patients) showed the incidence rate of MINS after thoracic surgery was 19.8%.5
The mismatch of oxygen supply and demand is considered a potential mechanism of MINS.6 A previous study of coronary angiography in patients with perioperative MINS showed that coronary artery demand ischemia was the leading cause, caused by the disequilibrium of myocardial oxygen supply and the increase of oxygen demand during the perioperative period.7,8 Surgery increases the release of catecholamine, which increases heart rate and has a negative impact on myocardial oxygenation. During one-lung ventilation after thoracotomy (OLV), hypoxic pulmonary vasoconstriction, pulmonary collapse, and intraoperative pulmonary artery clamping will lead to right ventricular dilatation and dysfunction, increase the right ventricular end-diastolic volume, and even cause supraventricular arrhythmia.5 Increased pulmonary vascular resistance may give rise to acute cardiovascular changes that may trigger excessive myocardial contraction, thereby increasing troponin.9
Salbutamol can bind to β2-adrenergic receptors in airway smooth muscle or directly couple with Gs protein activated by receptor and CA2+-activated potassium channel, resulting in cell hyperpolarization to relax airway smooth muscle, thereby dilating bronchi and improving lung ventilation. Salbutamol at therapeutic serum concentration has an anti-inflammatory effect.10,11 Budesonide can inhibit the release of multiple chemical mediators (such as prostaglandins or histamine) to achieve a comprehensive anti-inflammatory effect.12 The combination of salbutamol and budesonide can reduce intracellular CA2+ levels to weaken the secretion of elastase, synergistically inhibit the release of IL-8 of smooth muscle cells, rapidly reduce airway mucosal edema, enhance bronchiectasis, and regulate immune cell activity.13 Budesonide is hydrophilic and therefore more soluble in airway mucus and more quickly absorbed by airway tissue and systemic circulation.
Patients with severe cardiovascular complications may profit from improving oxygen supply. A review of cardiovascular pathophysiology of patients undergoing lobectomy during perioperative period has shown that intraoperative and postoperative inflammation of the heart muscle, and injury of right ventricular function in patients undergoing thoracotomy are associated with postoperative troponin elevations.5 Therefore, we infer that the combined use of salbutamol/budesonide may improve myocardial oxygen supply through its anti-inflammatory effect and improved lung ventilation, which may reduce the risk of myocardial oxygen demand and supply mismatch and reduce the release of biomarkers such as postoperative troponin, which may improve early postoperative myocardial injury. An observational study of postoperative myocardial injury in high-risk thoracic surgery found that only smoking and type of surgery were independent risk factors for myocardial injury. How to predict the myocardial injury after thoracic surgery is unclear.9 In this article, we examined the primary hypothesis that the administration of salbutamol/budesonide reduced the incidence of postoperative myocardial injury in patients with high risk of cardiovascular complications who underwent lobectomy. In addition, we examined the secondary hypothesis that the application of salbutamol/budesonide could improve lung function and reduce the occurrence of postoperative pulmonary and cardiovascular complications and the total postoperative hospital stay. We also evaluated the effect of salbutamol/budesonide administration on mortality, pain scores, and analgesic dosage, explored the independent risk factors that cause MINS, and established a risk prediction model.
Materials and Methods
This prospective, single-blind, single-center, randomized controlled trial was implemented at the Affiliated Hospital of Xuzhou Medical University from May 2022 to October 2022. The trial complies with the Declaration of Helsinki, was ratified by the Clinical Trials Ethics Committee of the Affiliated Hospital of Xuzhou Medical University (XYFY2022-KL126-01), and was registered at the Chinese Clinical Trial (ChiCTR2200059926).
Participants
One day before surgery, researchers evaluated patients who plan to undergo elective thoracoscopic lobectomy, and screened qualified patients. All participants got written informed consent before study commencement and give their consent to this study. Eligible patients were over 45 and must satisfy at least one of the following criteria: 1. Coronary artery disease; 2. Peripheral arterial disease; 3. Stroke OR 4. Any two of the following seven conditions (a-g): a). Over 70 years old; b). History of congestive heart failure; c). Cerebrovascular diseases; d). Hypertension; e). Diabetes and currently taking oral hypoglycemic drugs or insulin; f). smoking; g). Preoperative creatinine >2.0 mg/dl. Patients who meet one of the following criteria were excluded: 1. Sepsis; 2. Using inotropic drugs; 3. Severe heart failure; 4. History of asthma; 5. History of long-term use of hormone drugs. Patients who met one of the following criteria were eliminated from the trial: 1. Voluntary withdrawal; 2. Operation cancelled; 3. Myocardial injury is caused by non-ischemic causes such as pulmonary embolism and myocarditis. 4. Biomarker is not measured once after the operation.
Randomization and Masking
We used stratified randomization and stratified patients according to age factors (45–69 years old, ≧70 years old) and smoking or not. Patients were randomly assigned to the experimental group (EG) and the control group (CG) at a ratio of 1:1 by using a random sequence in each layer. The random allocation sequence was generated by a randomized website (https://www.medbox.top/dynamicRand). The block length was 6, and the random sequence was placed in a sealed opaque envelope. Researchers in charge of randomization did not participate in postoperative blood collection and outcome evaluation. Other researchers took blood samples 1 to 3 days after the operation and followed up by telephone 30 days after the operation.
Definition
MINS was defined as postoperative troponin elevation due to myocardial ischemia within 30 days after the operation and did not require clinical manifestations of myocardial ischemia.14 Based on this definition, the measured increase of hsTnT after the operation is defined as >20 to <65 ng/L, and the absolute change is at least 5 ng/L or hsTnT level of at least 65 ng/L.15,16 According to VISION, 78% of MINS occur either on the day of surgery or the first day after surgery, 94% on the second day after surgery, and only 0.6% of MINS can be diagnosed after the third day after surgery.17
Intervention and Observational Index
Details of a standardized anesthetic protocol and intraoperative management can be found in Appendices A–C. When salbutamol is used as a preventive medicine, the recommended dose of inhalation is 0.1–0.2 mg, and the dosage of budesonide is 0.5–1 mg. Considering that this study included high-risk cardiovascular patients and referring to the professional advice of respiratory department and thoracic surgery. We decided that the dosage of the drug was: salbutamol 100 μg + budesonide 1 mg. No drug-related adverse reactions were observed in preliminary experiments. After induction, during bilateral lung ventilation, the experimental group injected salbutamol 100 μg + budesonide 1 mg through the airway with a fiberoptic bronchoscope, while the control group did not receive intervention. We collected demographic data and perioperative variables. We also measured blood gas analysis preoperatively (S0) and before the patient left the operating room (S5), dynamic lung compliance (Cd), and static lung compliance (Cs) after anesthesia induction (S1) and at the end of operation (S4), blood gas analysis and compliance after administration of intervention (S2), and half an hour after the start of surgery (S3). The hsTnT, pulmonary complication score, pain score, analgesic dosage, drainage tube withdrawal time, and hospitalization time three days after the operation were recorded.
Primary and Secondary Outcomes
The primary outcome was the incidence of MINS. We measured hsTnT on postoperative days 1~3, and the highest postoperative measurement allowed the diagnosis of MINS, which was considered to be the occurrence of MINS. MINS is not considered to have occurred if the hsTnT increase was due to a number of non-ischemic causes, including congestive heart failure, pulmonary embolism, aortic valve disease, and sepsis. Our secondary outcomes were respiratory function at each time point during the operation, including lung compliance and arterial partial pressure of oxygen, postoperative pulmonary complications and hospital stay, pain score, and analgesic dosage. Our exploratory results included reoperation, unplanned ICU admission, and postoperative cardiovascular complications, including heart failure, heart infarction, new-onset arrhythmias, massive bleeding, respiratory failure, and mortality at 30 days after the operation. Blinded investigators evaluated exploratory results during hospitalization, and postoperative complications after discharge were further documented with telephone follow-up on the 30th postoperative day. The definitions of outcomes can be found in Appendices D–E.
Statistical Analysis and Sample Size Calculation
The patients were analyzed by intention-to-treat analysis. Missing data were treated with multiple imputations. The Kolmogorov–Smirnov test was used to test whether continuous variables conform to normal distribution. The Levene test was used to test whether the population variance is the same. Continuous variables subject to normal distribution were presented as mean ± SD. Skewed data were presented as median (IQR). Classification variables were expressed as absolute and per cent values. A Student’s t-test was used for data conforming to normal distribution and homogeneity of variance, and the non-normal distribution data were tested by Mann–Whitney U-test. The incidence rate of postoperative myocardial injury was the Pearson Chi-Square test. Repeated measures of ANOVA was used for other repeated measures data such as Cd, Cs.
We also performed a univariate logistic regression to select the risk factors associated with MINS. For all significant variables (P<0.05) in the univariate logistic regression model as the independent variable, MINS as the dependent variable, multiple regression was performed to determine independent risk factors for MINS in patients. Conduct collinearity diagnostic evaluation on all risk factors. The Hosmer-Lemeshow good of fit test assessed the calibration of the logistic regression model. We utilized the area under the receiver operating characteristic curve (AUC) to evaluate the model’s discriminative performance and capacity for prediction. According to the β-value calculated by the logistic model, the value of risk factors was assigned, and the risk prediction model of MINS was established. Potential confounders were included in logistic regression analysis as covariates. For our exploratory outcomes, we performed Fisher’s exact test. We furthermore performed a sensitivity analysis to evaluate the influence of the baseline covariates on the incidence of postoperative myocardial injury. We used SPSS26.0 for data analysis. For all analyses, α=0.05, P-values <0.05 were considered to be statistically significant.
According to our preliminary experiment, the incidence of MINS in lobectomy at the Affiliated Hospital of Xuzhou Medical University during the past six months was 24.7%. Given that the majority of patients measure hsTnT only on the first postoperative day, the incidence of 24.7% may be low, and the sample size was calculated using 27% of the results from the previous studies.9 The reduction of 50% was expected to be considered as effective intervention. According to the 80% power of the test and 5% significance level, the sample size was calculated according to 1:1 using PASS software, and 136 cases were required for each group. Considering the dropping of samples, the increase of 10% for each group resulted in 152 cases.
Results
We recruited 308 patients over 45 years old with high-risk of cardiovascular complications who underwent elective thoracoscopic lobectomy. A total of 153 patients were randomly assigned to the control group, and 155 patients were randomly assigned to the experimental group. In the control group, two patients refused to undergo surgery before surgery, and one patient with recurrent cerebral infarction before surgery was excluded from the study. In the experimental group, four patients refused before surgery, two patients changed to thoracotomy, and one patient was excluded from the study due to delayed surgery (Figure 1). Thus, 298 patients were involved in the final analysis.
 |
Figure 1 CONSORT flowchart showing the number of patients at each phase of the study. |
Demographic data, ASA physical status, comorbidities, RCRI, preoperative laboratory parameters, and types of surgery between the two groups were similar (Table 1). Analogously, intraoperative features and postoperative features, including duration of surgery and one-lung ventilation time, fluid and electrolyte management, anesthesia management, vasoactive drug consumption, arterial blood gas analysis, hospital stay, and drainage tube withdrawal time were similar (Table 2). Two groups of patients showed differences in preoperative hemoglobin (Figure F4).
 |
Table 1 Patient Baseline Characteristics |
 |
Table 2 Perioperative Variables |
The incidence rate of MINS in the control group was 57/150 (38%), while that in the experimental group was 33/148 (22%). There was a significant difference in the incidence of MINS between the two groups (P=0.03) (Table 3). There was no significant difference in preoperative troponin concentration between the EG and CG (P=0.417), and the median maximum postoperative troponin was 11.45 ng/L. The difference in troponin on the first postoperative day was statistically significant between the EG and CG (P=0.019; Figure F3). During hospitalization, no patient died in the first three days after surgery, and no patient developed troponin elevations due to non-ischemic causes.
 |
Table 3 Primary Outcomes |
The results of repeated measures analysis of variance show that the main effect between the two groups is significant (P<0.01). Compared with S1, the Cd and Cs at S3 in the experimental group were significantly improved (P<0.01), and the Cd and Cs at S2 were significantly decreased (P<0.05) (Figure 2). The difference in arterial partial pressure of oxygen at S5 was significant between the two groups (P<0.01) (Figure F5). Hospitalization (P=0.334) and drainage tube withdrawal time (P=0.397) were similar between the two groups. Postoperative pulmonary complication scores were mostly within the range of 2~4 points.14,15 The score of postoperative pulmonary complications in the experimental group was lower than that in the control group, and the difference was statistically significant (P<0.05). The analgesic consumption and VAS score of the control group after surgery were more than those of the experimental group (P<0.05) (Table 2).
Age, BMI, smoking, and ACCI were significant in univariate logistic regression between the two groups (Table F1). Combined with clinical features, preoperative hemoglobin and ASA physical status were decided to be included. The variance inflation factor (VIF) between variables was less than 10 after the multi-collinearity test, and no collinearity was found for several factors, so all of them were included in the multiple logistic regression with MINS as the dependent variable.
Multiple logistic regression showed that the independent risk factors for MINS included ACCI (OR, 2.03; 95% CI, 1.40 to 2.96; P<0.001), smoking (OR, 3.12; 95% CI, 1.54 to 6.3; P=0.002), age (OR, 12.5; 95% CI, 6.1 to 25.8; P<0.001), BMI (OR, 3.12; 95% CI, 3.30 to 15.0; P<0.001), logitP=−3.0+0.71*ACCI+1.19*Smoking+1.95*BMI+2.53*Age (Table F2).
Receiver operating characteristic curve analysis was performed on the predicted values, the AUC = 0.862 (95% CI, 0.81 to 0.91; P<0.001) (Figure F2). The model was tested by Hosmer-Lemeshow (P=0.680), indicating that the regression model had good correction effect. The model can correctly distinguish 82.4% of research subjects, the sensitivity is 63.2%, the specificity is 91.5%, the positive predictive value is 77.9%, and the negative predictive value is 84.0%.
The 30-day follow-up rate of the control group was 146/150 (97%), while that of the experimental group was 145/148 (98%). The patients were reexamined 30 days after operation. There was no difference between hospitalization and 30-day follow-up. There was no death within 30 days after operation between the EG and CG, and there was no difference in the incidence of adverse events between the EG and CG (Table 4). Due to the small number of exploratory events, we did not carry out univariate or multiple regression models.
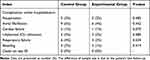 |
Table 4 Exploratory Outcomes |
The level of significance of subgroup analysis was chosen using the Bonferroni correction for multiple testing at 0.05/24 = 0.0021 due to the 24 subgroup analysis. No significant difference in the MINS could be detected between the two randomized groups, indicating that it may be due to chance. In subgroup analysis, we found that salbutamol/budesonide intervention can improve MINS in different types of surgery. The elaborate results of subgroup analysis and sensitivity analysis are presented in Table F3, Figure F1.
Discussion
Few studies have explored the intraoperative management and intervention of MINS, but intensive monitoring and early intervention for such patients are necessary. The evidence to guide clinicians in managing MINS is currently limited to observational studies. A meta-analysis of 287 studies showed that acetylsalicylic acid anticoagulation reduces cardiovascular events in high-risk patients.16 Statin also plays an important role in preventing primary cardiovascular events and improving mortality.17
Previous studies have shown that salbutamol/budesonide can significantly improve lung ventilation and has a protective effect on asthmatic and exercise-induced bronchoconstriction.18 The effect of combined use of the two to improve the clinical status and cardiopulmonary function of patients is significantly more than the effect of treatment alone.11,19 The results of our study showed that perioperative administration of salbutamol/budesonide reduced the incidence of MINS. HsTnT concentrations showed a difference between the two groups on the first postoperative day, probably because the beneficial effects of salbutamol/budesonide persisted on the first postoperative day. We control the intraoperative blood pressure to keep it at 20% of the basic value, in contrast to the lack of control of postoperative blood pressure management. The lack of control of postoperative blood pressure management may cause patients to experience long-term hypotension or hypertension in the ward.20 The occurrence of MINS in patients undergoing lobectomy during and after surgery may also be regulated by mechanisms other than myocardial ischemia (eg, inflammatory stress in the superficial layers of the myocardium or increased right ventricular afterload).9 Inflammatory stress may be another critical substrate for hsTnT formation and release, especially during surgery. We did not assess the correlation between postoperative blood pressure and inflammation and postoperative hsTnT release. Therefore, we cannot rule out that these influenced our results.2
We collected the arterial blood gas of patients at various time points during the operation, and the results showed that the patients in the experimental group had a higher partial pressure of arterial oxygen before leaving the operating room than those in the control group. We speculate that this is due to the improvement of lung ventilation by salbutamol and budesonide. High-inspired oxygen concentration is a simple way to improve arterial partial pressure of oxygen. However, studies have shown that high-inspired oxygen concentrations have a detrimental effect. A large retrospective analysis of 73,000 patients found high FiO2 was dose-dependent, accompanied by severe respiratory complications and 30-day mortality.21,22 A recent meta-analysis involving more than 16,000 patients showed that oxygen therapy for free increases mortality.23 Compared with our research, the most important differences between these studies are the study population, study method, and improved ventilatory time point. We administered salbutamol/budesonide to improve ventilation immediately after intubation, just before the oxygen mismatch occurred. This may be one of the reasons why drug intervention has different effects from increasing oxygen concentration. Therefore, we still believe that the administration of salbutamol/budesonide can improve pulmonary ventilation, thus affecting myocardial oxygen supply and continuously affecting postoperative troponin.
We also evaluated the effects of salbutamol/budesonide on pulmonary function and postoperative pulmonary complications, with the experimental group showing an improvement in pulmonary function in the first half hour after the start of surgery compared to pre-surgery, with little difference at the end of surgery compared to pre-surgery. Salbutamol takes effect 1 ~ 5 minutes after inhalation and reaches its peak at one hour. The peak value was reached 30 minutes after inhalation of 1 mg budesonide. Due to the changes in posture, tracheal traction during surgery, and catheter blockage by sputum, the effect of drugs on lung function cannot be accurately reflected during the operation. The postoperative pulmonary complication score of the experimental group was 2~3 points lower than that of the control group. The MANDALA study demonstrating that salbutamol/budesonide can help control bronchoconstriction and slow airway inflammation.24 A randomized controlled trial showed the use of ICS plus β2 receptor agonists to reduce persistent cough after lobectomy.12 The potential mechanism may be the comprehensive anti-inflammatory effect of corticosteroids. The use of salbutamol/budesonide is further evidence of its utility in improving pulmonary complications after thoracic surgery. A recent study has shown a significant correlation between acute post-operative pain and the incidence of MINS. In particular, a high pain score in the first three days post-operatively significantly increases the risk of myocardial ischemia.25 In our study, an intercostal nerve block and patient-controlled analgesia pump were used for the postoperative analgesia of our patient. We observed that patients in the experimental group had lower postoperative pain scores and analgesic dosage than those in the control group. However, follow-up treatment was decided by the surgeon after his return to the ward, and the surgeon was usually busy with the operation. The analgesics of the analgesic pump covered up symptoms of cardiac complications such as chest pain, and most patients were examined only at 3~4 weeks of follow-up.26 Therefore, we cannot rule out the possibility that postoperative pain management may influence our results.
40% of our patients were over the age of 70 years, and almost all of them had a history of pre-operative hypertension or coronary artery disease. This explains our high MINS rate. It is well known that the thoracic surgery population is aging. Ageing leads to pulmonary arteriosclerosis, which may decrease pulmonary vascular flow reserve. At the same time, age-related myocardial remodelling and downregulation of myocardial catecholamine receptors lead to decreased myocardial contractility.27,28 In a cohort study of elevated troponin levels after colorectal surgery, almost all of the patients who died were older than 70 years.29 A cohort study of 15,065 patients recommended an age greater than 75 years as an independent predictor of 30-day mortality in patients with MINS.30,31 Bae et al reported that the duration of surgery strongly predicts the development of postoperative MINS in patients undergoing non-cardiac surgery.32 The duration of surgery in the two groups was similar, but the control group had longer duration of anesthesia and more blood loss. Basically, the extension of the anesthesia time reflects the complexity of the operation, and the anesthesia time is longer in patients, the intraoperative bleeding incidence is higher. Bleeding is the leading risk factor of myocardial injury.17 The severity of anemia is related to the MINS, and the incidence of MINS increases with further decreases in oxygen-carrying capacity.33,34 In our multiple regression analysis, preoperative hemoglobin did not affect our results. However, it is vital to avoid preoperative anemia during perioperative anesthesia management in our patients, and the effect of correcting anemia before operation still needs to be investigated.
Our multiple regression analysis showed that overweight and even obese people had a higher incidence of postoperative MINS than those with normal body mass index. A recent study showed that underweight and obesity were positively related to mortality, which persisted during long-term follow-up,35 consistent with the results in our article. Interestingly, this difference in mortality only differed between the one-year groups, whereas the 30-day mortality results did not differ.31,36 We also found that smoking was an independent risk factor for MINS. In an observational study, smoking has been shown to be associated with MINS in patients undergoing thoracic surgery.9 This finding is important because smoking is the only modifiable pre-operative risk factor for the prevention of MINS. In an analysis of predictors of adverse events up to 30 days after non-cardiac surgery, the low-risk RCRI (one variable) underestimated the incidence of MINS and mortality rate, and the National Surgical Quality Improvement Program (NSQIP) proved to be less relevant to MINS.4,37 We collected the ACCI and RCRI scores of patients before the operation, and the results showed that the ACCI was positively correlated with the risk of MINS, and the higher the ACCI score, the greater the risk of MINS. However, our sample size was not large enough, and the ACCI needed to be combined with other predictive tools and biomarkers to predict MINS accurately.
Although a large number of articles have conducted in-depth research on MINS, the intraoperative management and intervention of MINS are still not completely clear. Our research provides a simple and repeatable method to help anesthesiologists manage MINS during operation. Our findings provide a valuable overview of the peri-operative effects of salbutamol/budesonide on non-cardiac surgery and may serve as a foundation for further research in the future. However, our study has several limitations. Firstly, it is a single-center study for high-risk cardiovascular patients and probably does not represent the general population of thoracotomy. Secondly, we measured troponin only 3 days before surgery. Although more than 90% of MINS occur within 3 days after surgery,34 we may still ignore possible myocardial injury 3 days after surgery. We have not measured inflammatory factors, so we cannot judge whether the anti-inflammatory mechanism has improved the incidence of myocardial injury. Although our study showed a high incidence of MINS, the 30-day mortality rate in patients with MINS was 0%, and we could not assess the significance between mortality and MINS. Therefore, a longer follow-up was required to determine whether the mortality rate was related to the use of salbutamol/budesonide.
Conclusion
In summary, intraoperative administration of salbutamol/budesonide reduced the incidence of myocardial injury after thoracic surgery, improved lung function to a certain extent, and reduced the incidence of postoperative pulmonary complications. Therefore, the administration of salbutamol/budesonide can improve postoperative myocardial injury in thoracic patients at risk for cardiovascular complications.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors state that they have no known competitive financial interests or personal relationships, which may affect the work reported in this article.
References
1. Zhang Z, Xu M, Wu D, Zhang X, Wu J. Postoperative myocardial injury in middle-aged and elderly patients following curative resection of esophageal cancer with aggressive or standard body temperature management: a randomized controlled trial. Anesth Analg. 2019;129(2):352–359. doi:10.1213/ANE.0000000000004022
2. Reiterer C, Kabon B, Taschner A, et al. Perioperative supplemental oxygen and NT-proBNP concentrations after major abdominal surgery – a prospective randomized clinical trial. J Clin Anesth. 2021;73:110379. doi:10.1016/j.jclinane.2021.110379
3. Devereaux PJ, Biccard BM, Sigamani A, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317(16):1642–1651. doi:10.1001/jama.2017.4360
4. Costa MCDBG, Furtado MV, Borges FK, et al. Perioperative troponin screening identifies patients at higher risk for major cardiovascular events in noncardiac surgery. Curr Probl Cardiol. 2021;46(3):100429. doi:10.1016/j.cpcardiol.2019.05.002
5. Shelley B, Glass A, Keast T, et al. Perioperative cardiovascular pathophysiology in patients undergoing lung resection surgery: a narrative review. Br J Anaesth. 2022. doi:10.1016/j.bja.2022.06.035
6. Kwon JH, Park J, Lee SH, et al. Pre-operative anaemia and myocardial injury after noncardiac surgery: a retrospective study. Eur J Anaesthesiol. 2021;38(6):582–590. doi:10.1097/EJA.0000000000001421
7. Reed GW, Horr S, Young L, et al. Associations between cardiac troponin, mechanism of myocardial injury, and long-term mortality after noncardiac vascular surgery. J Am Heart Assoc. 2017;6(6). doi:10.1161/JAHA.117.005672
8. Vasireddi SK, Pivato E, Soltero E, et al. Postoperative myocardial injury in patients classified as low risk preoperatively is associated with a particularly increased risk of long--term mortality after noncardiac surgery. J Am Heart Assoc. 2021;10(14):e019379. doi:10.1161/JAHA.120.019379
9. González-Tallada A, Borrell-Vega J, Coronado C, et al. Myocardial injury after noncardiac surgery: incidence, predictive factors, and outcome in high-risk patients undergoing thoracic surgery: an observational study. J Cardiothorac Vasc Anesth. 2020;34(2):426–432. doi:10.1053/j.jvca.2019.08.014
10. Haghi M, Hittinger M, Zeng Q, et al. Mono- and cocultures of bronchial and alveolar epithelial cells respond differently to proinflammatory stimuli and their modulation by salbutamol and budesonide. Mol Pharm. 2015;12(8):2625–2632. doi:10.1021/acs.molpharmaceut.5b00124
11. Sadowska AM, Manuel-y-Keenoy B, De Backer WA. Inhibition of in vitro neutrophil migration through a bilayer of endothelial and epithelial cells using beta2-agonists: concomitant effects on IL-8 and elastase secretion and impact of glucocorticosteroids. Pulm Pharmacol Ther. 2005;18(5):354–362. doi:10.1016/j.pupt.2005.01.006
12. Sawada S, Suehisa H, Yamashita M. Inhalation of corticosteroid and β-agonist for persistent cough following pulmonary resection. Gen Thorac Cardiovasc Surg. 2012;60(5):285–288. doi:10.1007/s11748-011-0910-1
13. Panettieri RA, Schaafsma D, Amrani Y, Koziol-White C, Ostrom R, Tliba O. Non-genomic effects of glucocorticoids: an updated view. Trends Pharmacol Sci. 2019;40(1):38–49. doi:10.1016/j.tips.2018.11.002
14. Berger MM, Oudemans-van S, Heleen M. Vitamin C supplementation in the critically ill patient. Curr Opin Clin Nutr Metab Care. 2015;18(2):193–201. doi:10.1097/MCO.0000000000000148
15. Hill A, Wendt S, Benstoem C, et al. Vitamin C to improve organ dysfunction in cardiac surgery patients—review and pragmatic approach. Nutrients. 2018;10(8):974. doi:10.3390/nu10080974
16. Collaboration AT. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86. doi:10.1136/bmj.324.7329.71
17. Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154(8):523–528. doi:10.7326/0003-4819-154-8-201104190-00003
18. LaForce C, Chipps BE, Albers FC, et al. Albuterol/budesonide for the treatment of exercise-induced bronchoconstriction in patients with asthma: the TYREE study. Ann Allerg Asthma Im. 2022;128(2):169–177. doi:10.1016/j.anai.2021.10.020
19. Cazzola M, Santus P, Di Marco F, et al. Bronchodilator effect of an inhaled combination therapy with salmeterol + fluticasone and formoterol + budesonide in patients with COPD. Respir Med. 2003;97(5):453–457. doi:10.1053/rmed.2002.1455
20. Zhao XJ, Zhu FX, Li S, Zhang HB, An YZ. Acute kidney injury is an independent risk factor for myocardial injury after noncardiac surgery in critical patients. J Crit Care. 2017;39:225–231. doi:10.1016/j.jcrc.2017.01.011
21. Myles PS, Leslie K, Chan MT, et al. The safety of addition of nitrous oxide to general anaesthesia in at-risk patients having major non-cardiac surgery (ENIGMA-II): a randomised, single-blind trial. Lancet. 2014;384(9952):1446–1454. doi:10.1016/S0140-6736(14)60893-X
22. Myles PS, Leslie K, Chan MT, et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. Anesthesiology. 2007;107(2):221–231. doi:10.1097/01.anes.0000270723.30772.da
23. Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–1705. doi:10.1016/S0140-6736(18)30479-3
24. Chipps BE, Albers FC, Reilly L, Johnsson E, Cappelletti C, Papi A. Efficacy and safety of as-needed albuterol/budesonide versus albuterol in adults and children aged ≥4 years with moderate-to-severe asthma: rationale and design of the randomised, double-blind, active-controlled MANDALA study. BMJ Open Respir Res. 2021;8(1). doi:10.1136/bmjresp-2021-001077
25. Turan A, Leung S, Bajracharya GR, et al. Acute postoperative pain is associated with myocardial injury after noncardiac surgery. Anesth Analg. 2020;131(3):822–829. doi:10.1213/ANE.0000000000005033
26. Spence J, LeManach Y, Chan MTV, et al. Association between complications and death within 30 days after noncardiac surgery. Can Med Assoc J. 2019;191(30):E830–E837. doi:10.1503/cmaj.190221
27. Riaz SP, Lüchtenborg M, Jack RH, et al. Variation in surgical resection for lung cancer in relation to survival: population-based study in England 2004–2006. Eur J Cancer. 2012;48(1):54–60. doi:10.1016/j.ejca.2011.07.012
28. Berra G, Noble S, Soccal PM, Beghetti M, Lador F. Pulmonary hypertension in the elderly: a different disease? Breathe. 2016;12(1):43–49. doi:10.1183/20734735.003416
29. Gorgun E, Lan BY, Aydinli HH, et al. Troponin elevation after colorectal surgery: significance and management. Ann Surg. 2016;264(4):605–611. doi:10.1097/SLA.0000000000001854
30. Botto F, Alonso CP, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120(3):564–578. doi:10.1097/ALN.0000000000000113
31. Khanna AK, Gan TJ. Myocardial injury after noncardiac surgery—slightly heavier may be better. Anesth Analg. 2021;132(4):957–959. doi:10.1213/ANE.0000000000005348
32. Bae MH, Lee JH, Yang DH, Park HS, Cho Y, Chae SC. Usefulness of surgical parameters as predictors of postoperative cardiac events in patients undergoing non-cardiac surgery. Circ J. 2014;78(3):718–723. doi:10.1253/circj.cj-13-1208
33. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Glob Heart. 2018;13(4):305–338. doi:10.1016/j.gheart.2018.08.004
34. Turan A, Cohen B, Rivas E, et al. Association between postoperative haemoglobin and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Brit J Anaesth. 2021;126(1):94–101. doi:10.1016/j.bja.2020.08.056
35. Tjeertes EK, Tjeertes E, Hoeks SE, et al. Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol. 2015;15:112. doi:10.1186/s12871-015-0096-7
36. Lee SH, Yang K, Park J, et al. Association between high body mass index and mortality following myocardial injury after noncardiac surgery. Anesth Analg. 2021;132(4):960–968. doi:10.1213/ANE.0000000000005303
37. Roshanov PS, Sessler DI, Chow CK, et al. Predicting myocardial injury and other cardiac complications after elective noncardiac surgery with the revised cardiac risk index: the VISION study. Can J Cardiol. 2021;37(8):1215–1224. doi:10.1016/j.cjca.2021.03.015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

