Back to Journals » Infection and Drug Resistance » Volume 15
Effects of Blood Culture Aerobic/Anaerobic Bottle Collection Patterns from Both Sides of the Body on Positive Blood Culture Rate and Time-to-Positivity
Authors Wen H, Wang W, Xie S, Sun Q, Liang Y, Wen B, Liu Y, Sun L, Zhang Z , Cao J, Liu X, Niu X, Ouyang Z, Dong N, Zhao J
Received 10 February 2022
Accepted for publication 27 May 2022
Published 10 June 2022 Volume 2022:15 Pages 2995—3004
DOI https://doi.org/10.2147/IDR.S358675
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Hainan Wen,1,* Weigang Wang,1,2,* Shoujun Xie,3 Qian Sun,1 Yueyi Liang,3 Baojiang Wen,1,2 Yanchao Liu,3 Lihong Sun,3 Zongwei Zhang,3 Jing Cao,1,2 Xiaoxuan Liu,1,2 Xiaoran Niu,1,2 Zirou Ouyang,1,2 Ning Dong,1,2 Jianhong Zhao1,2
1The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China; 2Hebei Provincial Center for Clinical Laboratories, Shijiazhuang, Hebei, People’s Republic of China; 3Department of Laboratory, the Affiliated Hospital of Chengde Medical university, Chengde, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianhong Zhao, Email [email protected]
Background: Although the principles for blood cultures (BCs) guidelines provide a recommendation for collection patterns, the complexity of clinical practice occasionally prompts clinicians to adopt non-standard collection patterns. Here, we investigate the influences of different BC collection patterns on detection of pathogens.
Methods: The BC collection patterns of 96 hospitals were surveyed online. And a retrospective study of BC data from a tertiary hospital was conducted.
Results: The results showed that 53.1% of hospitals adopted the recommended patterns. Among the 1439 episodes of true-positive BCs, 67.4% were found in both the left- and right-sided bottles; 58.2% were found in both aerobic and anaerobic bottles.
Conclusion: The present study suggested that the rate of standard collection patterns of blood culture was low and the non-standard collection patterns were associated with decreased detection of pathogens. Simultaneous collection of blood on the left and right sides was recommended as an effective pattern of BC collection.
Keywords: blood culture, collection pattern, online survey, time-to-positivity, pathogen detection
Introduction
Bloodstream infection (BSI) is the most common cause of morbidity and mortality worldwide.1 Blood culture (BC) can detect pathogens that cause BSI, which is essential to assess their antimicrobial susceptibility, providing significant guidance for the treatment of BSI.
Increasing the detection rate of pathogens in BSI has become a key challenge for clinicians. For adult patients, although blood volume is undoubtedly the most important variable in detecting bacteremia and fungemia,2–4 the patterns of BC, adequate blood volume, multiple sets of BCs, multiple puncture sites, and the combination of aerobic and anaerobic bottles can influence the rate of positive BCs.5–7
Although the current guidelines have presented recommendations for the collection of BC specimens,8 due to the large volume of blood drawn at a time, blood collection is markedly affected by the physician’s discretion and patients’ compliance. At present, a number of hospitals do not fully follow the procedures recommended by the guidelines,9 and blood is collected in accordance with advice presented by hospitals or physicians, including adopting a single puncture site, or using anaerobic bottles only when obligate anaerobic bacteria are highly suspected. There are currently no data on BC collection patterns in local hospitals. Thus, we conducted a questionnaire survey on the BC patterns of 96 hospitals (including secondary and tertiary hospitals) located in Hebei province, China. As a result, we found that there were a variety of inappropriate BC patterns in several hospitals in this region. Then, we retrospectively analyzed the rate and the time-to-positivity (TTP) of positive BCs in a large comprehensive tertiary hospital, in order to evaluate the influences of different BC patterns.
Materials and Methods
Study Design
A survey of BC collection was conducted in 96 hospitals, in addition to a single-center retrospective analysis of BC data in a tertiary hospital which belongs to these 96. The survey included 96 hospitals that participated in the Antimicrobial Resistance Surveillance System of Hebei Province (China). The retrospective analysis of BC collection patterns was conducted in a tertiary general hospital, with 2400 inpatient beds. We retrieved BC data of outpatients and inpatients from January 2018 to October 2020, including clinical diagnosis, time of drawing BCs, positive BC rate, TTP, and pathogenic bacteria detection results. The inclusion criteria were as follows: 1) adult patients aged ≥18 years, 2) the existence of two or more sets of BCs collected simultaneously. Therefore, the results of only one-set or one-bottle of BC collected simultaneously were excluded. Each positive-BC sample was assessed for contamination according to the following predefined criteria: when coagulase-negative Staphylococci (CoNS), Micrococcus species, Bacillus species, Corynebacterium species, and Propionibacterium acnes were present in a positive-BC sample, clinicians and microbiology laboratory staff work together to identify bacterial contamination. Informed consent was obtained from the study participants prior to the commencement of the study. All procedures will be performed in adherence to the Helsinki declaration. Ethical approval from the Institutional Review Board of the Affiliated Hospital of Chengde Medical University.
Survey Procedure
To our knowledge, there has been no survey on BC collection in Hebei province to date. To verify the performance of the questionnaire, pre-testing of 20% of the study population was performed to examine their performance on the questionnaire, and the required amendments were accordingly applied. The questionnaire survey was implemented on an online platform, developed by Tencent, Inc. (Shenzhen, China). We distributed electronic questionnaires among the microbiology laboratories staff in 96 hospitals. Participants filled in data truthfully after collecting BC data. There were eight items about BCs in the questionnaire, as follows: (i) how many sets of BCs did your laboratory receive per month?; (ii) what’s the method of BC collection in adult patients?; (iii) what’s the percentage of adult patients with two or more sets of BCs?; (iv) what’s the percentage of adult patients with two bottles (left and right aerobic bottles) of BCs from each side of the body?; (v) what’s the percentage of adult patients with two bottles (aerobic bottle + aerobic bottle) of BCs from one side?; (vi) what’s the percentage of adult patients with two different bottles (aerobic bottle + anaerobic bottle) of BCs on one site?; (vii) what’s the percentage of adult patients with only one bottle of BC?; and (viii) Did your microbiology laboratory conduct anaerobic cultures during normal time period? After the questionnaires were filled-out, our research team members collected and analyzed the data.
BC Method
The procedures used for blood collection and skin disinfection in patients were strictly carried out on the basis of the Principles and Procedures for Blood Cultures (CLSI-M47-A).8 One aerobic bottle (BACT/ALERT FA; bioMérieux, Paris, France) and one anaerobic bottle (BACT/ALERT FN; bioMérieux) from one puncture site were defined as a set of BCs. One or more sets of BCs collected simultaneously from the same patient were defined as one episode in this study. Blood was typically collected from the left and right limb veins, unless contraindicated or disapproved by the patient. The left and right sides mentioned in the current study represent one venipuncture site on the left and right limbs, respectively. A total of 8–10 mL of blood was injected into each bottle. A nurse, who was in charge of blood collection, marked the blood collection site on each culture bottle. All BC bottles were transported directly to the laboratory by medical staff within 2 h. BC bottles were incubated in an automatic BACT/ALERT 3D instrument (bioMérieux) for up to 7 days. The TTP of each BC was recorded, and liquid from each BC bottle was inoculated into a blood agar plate, a MacConkey agar plate, and a chocolate agar plate and incubated at 36°C for 18–24 h. An anaerobic Brucella culture medium was added to positive anaerobic bottles instead of positive aerobic bottles. Then anaerobic Brucella medium grew under anaerobic conditions at 36°C. The blood Gram stain results were immediately reported to clinicians.
Identification of Isolates
The pure colonies growing on solid media were identified using a VITEK®2 Compact Instrument (bioMérieux) or MALDI-TOF MS (bioMérieux) according to the manufacturer’s instructions.
Statistical Analysis
Descriptive statistics were used to describe the TTP of aerobic and anaerobic BCs, and data were presented as the median [interquartile range (IQR)]. The Pearson’s chi-square test, designated as the primary method of statistical analysis, was employed to analyze rates of positive BCs between the left and right sides, and rates of positive BCs between aerobic and anaerobic BCs. Then, Wilcoxon’s rank sum test, designated as the secondary method of statistical analysis, was utilized to analyze the outcome variables of the TTP between the aerobic and anaerobic BCs. P < 0.05 was considered statistically significant. SPSS 19.0 software (IBM, Armonk, NY, USA) was used to carry out statistical analysis.
Results
General Outcomes
Based on the survey results collected from 96 hospitals, we found that 53.1% (n = 51) of the hospitals adopted two or more BC sets on two sides (left and right sides), including hospitals that used two or more BC collection methods. Additionally, 10.4% (n = 10) of the hospitals collected one aerobic bottle on both the left and right sides, respectively; 5.2% (n = 5) of the hospitals collected two aerobic bottles on one side (meaning one site); 26.0% (n = 25) of the hospitals collected paired aerobic/anaerobic bottles on one side (meaning one site); and 5.2% (n = 5) of the hospitals only collected a single aerobic bottle (Figure 1).
Integration of Data
During the study period, a total of 17,678 episodes (29,366 sets) were collected in our microbiology laboratory and 1534 episodes (2622 sets) detected pathogens. Among them, 60 cases of BCs, where the pathogens were detected as contaminant, were excluded. This study excluded all patients for whom only a single set of BCs was collected. As a result, 1439 episodes (2527 sets) of true-positive BCs from adult patients were included in the present study (Figure 2). Among them, two sets of positive BCs accounted for the highest proportion (2278 sets (90.1%)), followed by three sets (n = 198, 7.8%), four sets (n = 39, 1.5%), and six sets (n = 12, 0.5%).
 |
Figure 2 Study flowchart. |
The Relationship Between Different BC Collection Patterns and the True-Positive Rates
Among 2562 sets of positive BCs, duplicate strains were excluded, and a total of 1439 episodes were detected. Gram-negative bacteria, Gram-positive bacteria, anaerobic bacteria, and fungi accounted for 58.4%, 41.6%, 4.4%, and 3.6%, respectively. We compared 1439 true-positive episodes between the left and right sides, and found that the true-positive rate of all episodes increased under different BC patterns on the left and right sides. The results showed that there was no significant difference in detection of BSI episodes between left and right collection side (P = 0.52) (Figure 3). We also found that the bilateral (left + right) combination significantly increased the detection rate of pathogens compared to unilateral collection and aerobic bottle collection. Additionally, the detection rate of collected aerobic and anaerobic bottles on the left or right side was 31.7% and 30.7%, respectively, higher than those of one aerobic bottle collected on each side. The increase in the number of bottles and collection sites remarkably improved the detection rate of pathogens compared with improper collection strategies (Figure 4).
No Significant Difference in the Rate or Distribution of True-Positive Episodes between the Left- and Right-Sided BCs
In the survey, 36.4% of hospitals used unilateral culture (including unilateral aerobic only and unilateral aerobic + anaerobic). Therefore, the distribution of true-positive episodes on the left and right sides was analyzed. The number of episodes detected on the left and right sides was 970 (67.4%), 245 (17.0%) of which were only detected on the left side, and 224 (15.6%) were only detected on the right side. There were significant differences among the three groups (P< 0.001), indicating that if only one-side collection was performed on the left or right side, 17.0% and 15.6% of episodes might be missed (Table 1). We then analyzed episodes that only occurred on one side. The most important pathogens that only grew on the left side included Escherichia coli, coagulase negative Staphylococcus, and Enterobacterales ord. nov., while pathogens that only grew on the right side were E. coli, Klebsiella pneumoniae, and Enterobacterales ord. nov. (Table 2). We found that there was no significant difference in the rate or distribution of true-positive episodes between the left- and right-sided BCs.
 |
Table 1 Distribution of True-Positive Episodes in the Left- and Right-Sided Blood Cultures |
 |
Table 2 Aerobic and Anaerobic Pathogens Grown Only in Single Side Bottles |
Distribution of True-Positive Episodes on the Aerobic and Anaerobic BCs
The survey results showed that at least 20.8% of hospitals did not collect anaerobic bottles. Therefore, we compared the number of true-positive episodes in aerobic and anaerobic bottles. As presented in Table 3, the total number of true-positive episodes in both aerobic and anaerobic bottles was 838 (58.2%), including 381 (26.5%) in only aerobic bottles, and 220 (15.3%) in only anaerobic bottles. There were significant differences among the three groups (P < 0.001). This revealed that when only aerobic bottles were collected, at least 15.3% of facultative and obligate anaerobes were missed. Table 4 provides a detailed analysis of pathogens that only grew in anaerobic bottles. There were 158 (11.5%, 158/1377) facultative anaerobes and fungus, and 62 (100%, 62/62) obligate anaerobic bacteria that grew only in anaerobic bottles, including S. aureus, K. pneumoniae and obligate anaerobes, which might cause serious consequences. If only aerobic BC bottles were collected, these pathogens might not be detected.
 |
Table 3 Distribution of True-Positive Episodes in Aerobic and Anaerobic Blood Cultures |
 |
Table 4 Pathogens Grown Only in Anaerobic Bottles |
Comparison of TTP Between the Aerobic and Anaerobic Bottles
Table 5 compares the median and interquartile range of the TTP between the aerobic and anaerobic bottles. Regardless of whether BCs were collected from the left or right side, the median TTP in the anaerobic bottles was shorter than that in the aerobic bottles by nearly 1 h, and the difference was statistically significant (P < 0.001). However, whether an aerobic bottle or anaerobic bottle was analyzed, there was no significant difference in TTP between the left and right sides. Table 6 summarizes the results of analysis of the TTP in aerobic and anaerobic bottles of the five most abundant true pathogens. Among them, E. coli, K. pneumoniae, and Enterococcus faecium were detected in anaerobic bottles sooner than in aerobic bottles (P < 0.001). In contrast, the median TTP of Staphylococcus aureus and S. epidermidis in the aerobic bottles was shorter than that in the anaerobic bottles (P < 0.05).
 |
Table 5 Comparison of Time-to-Positivity Between Aerobic and Anaerobic Blood Cultures |
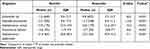 |
Table 6 Comparing Time-to-Positivity for Different Organisms in Aerobic and Anaerobic Blood Cultures (Hours) |
Discussion
Drawing blood from different peripheral venipuncture sites is a standard method recommended by the CLSI for clinically obtaining BCs.8 Puncture at different sites not only increases the detection rate of pathogens in the blood due to increased blood volume, but also provides a reliable basis for the determination of contaminating bacteria.10 However, the guideline does not recommend specific blood collection sites, and a limited number of studies have concentrated on the effects of different blood collection sites on the rate of positive BCs. The BCs included in the current study were all from the left and right limb veins, which provided a strong condition to investigate the influences of different blood collection sites on the rate of positive BCs. To our knowledge, there has been no research into the influences of the left and right sides of blood collection sites on the rate of positive BCs. In the present study, We found that among the 1439 true-positive episodes, the bilateral (left + right) combination significantly increased the detection rate of pathogens compared to unilateral collection. We speculate that there were two possible reasons for this. First, when blood was collected from only a single side, insufficient blood volume could lead to missed detection of pathogens. Weinstein et al11 reported that 91.5% of episodes were detected with the first set of BCs and 99.3% of episodes were detected with two sets of BCs. Tarai et al12 compared single BCs with paired BCs, and found that the rate of positive BCs from a single venipuncture site was significantly lower than that from two venipuncture sites (7.2% vs 11.8%). The second reason may be that the in vivo distribution of pathogens may differ during different phases of disease. BCs were collected simultaneously from the left and right side in our study; however, the pathogen was not detected in both the left and right BCs collected at the same time, with 17.0% and 15.6% of the episodes, respectively, detected only in the left- and right-sided BCs. This suggested that the pathogen was not evenly distributed in the blood of the left and right sides of the body, while further investigation needs to be carried out to indicate whether the distribution is related to the sites of primary infection. Because previous studies on sets of BCs were based on the number of venipuncture sites, and the specific sites of blood collection were not mentioned,11,13,14 direct comparisons were not possible here. It appears, from our current results, that the pattern of simultaneously collecting BCs on the left and right sides is feasible.
The majority of pathogens that cause BSI can grow in aerobic bottles, and injection of blood to anaerobic bottles may cause difficulties for patients. Therefore, the routine use of anaerobic bottles in BCs has caused controversy.15,16 In the present study, we found that 220 episodes would be missed if anaerobic bottles had not been drawn, accounting for 15.3% of the total number of episodes detected (1439). The missed bacteria included all of the anaerobic bacteria, as well as 158 facultative anaerobes, E. coli and K. pneumoniae, that grew in only anaerobic bottles. In a recent study of 19,739 BCs, 369 (15.8%) were positive only for anaerobic bottles (negative for aerobic bottles), which is consistent with the results of the present study.15 A Japanese study on BCs reported an increase of facultative anaerobes detected from anaerobic culture bottles, including 15% of Staphylococcus and 29% of E. coli.17 At present, the drug resistance rate of obligate anaerobes is increasing annually,18,19 and the use of some antibiotics may also cause facultative anaerobes to fail to grow in aerobic bottles, thus, it is quite unfavorable to the diagnosis and treatment of patients with BSI if anaerobic bottles are not adopted. Additionally, the CLSI guideline mentions that when less than the recommended volume of blood is drawn for culture, the blood should be inoculated into the aerobic vial first, while a better combination seems to be more reasonable. The results of the current research showed that the rates of positive BCs in the left/right aerobic plus anaerobic bottles were 31.7% and 30.7% higher, respectively, than those of two aerobic bottles collected on bilateral limbs. Therefore, it can be concluded that if a patient’s blood volume is only sufficient to meet the needs of two culture bottles, the combination of aerobic and anaerobic bottles at a single blood collection site is more efficacious than taking two aerobic bottles from two blood collection sites. This finding has rarely been reported in previous studies.
Regarding the question of pathogens that cause BSIs to grow faster in aerobic or anaerobic bottles, different studies have reached inconsistent conclusions. For instance, the findings of Passerini et al20 were inconsistent with ours, that is, the TTP of aerobic bottles was shorter than that of anaerobic bottles. This may be related to different types of culture systems used or differences in the composition of pathogenic bacteria in BSI. We found that in general, the TTP of the anaerobic bottles was nearly an hour shorter than that of the aerobic bottles. From the groups of organisms, the TTP of E. coli and K. pneumoniae in anaerobic bottles was shorter than that in aerobic bottles; in contrast, the TTP of S. aureus and S. epidermidis was shorter in the aerobic bottles. Grohs et al used the same blood culture apparatus as ours, and found that the TTP of Enterobacteriaceae in the anaerobic bottles was shorter than that in the aerobic bottles, while S. aureus had a shorter TTP in the aerobic bottles,21 which was consistent with our results. Defrance et al pointed out that a TTP ≤ 18 h was predictive of Enterobacteriaceae with a positive predictive value of 99.4%.22 Both of these are in favor of the early detection of pathogens that cause BSI. Initiation of an effective antimicrobial therapy as early as possible, following early detection of pathogens, can significantly improve disease outcomes,14,23 and the use of aerobic bottles alone is not conducive to early detection of pathogens and consequently may delay a patient’s treatment.
The present study contains several limitations. First, our questionnaire was a multi-center study, while the follow-up was performed in the form of a single-center study, thus, the number of hospitals should be increased and different instruments are required. Second, we did not determine whether different blood collection sites from the ipsilateral limb influenced the rate of positive BCs.
In summary, a combination of aerobic and anaerobic bottles from a single site was superior to two aerobic bottles from two different sites. Neglecting the use of anaerobic BC bottles may reduce the rate of positive BCs, and was not conducive to the early detection of pathogens. There was no significant difference in the rate of positive BCs between the two sides of the body. Simultaneous collection of blood on the left and right sides is recommended as an effective pattern of BC collection.
Data Sharing Statement
The data obtained from the study are available from the corresponding author upon request.
Acknowledgments
We thank the staff of the microbiology laboratories in all 96 hospitals who participated in the survey. We would like to express our sincere gratitude to Professor Yiwei Tang for his valuable comments, suggestions, and revisions of this manuscript.
Funding
This study was financially supported by the Special Foundation for National Science and Technology Basic Research Program of China (Grant Nos. 2019FY101200, and 2019FY101204), the Foundation of Hebei Provincial Department of Finance (Grant No. 361004), and the International Scientific and Technology Corporation Program of Hebei Provincial Department of Science and Technology of China (Grant No.183977118D).
Disclosure
The authors declare that there are no conflicts of interest.
References
1. McNamara JF, Righi E, Wright H, Hartel GF, Harris PNA, Paterson DL. Long-term morbidity and mortality following bloodstream infection: a systematic literature review. J Infect. 2018;77:1–8.2. doi:10.1016/j.jinf.2018.03.005
2. Khare R, Kothari T, Castagnaro J, Hemmings B, Tso M, Juretschko S. Active monitoring and feedback to improve blood culture fill volumes and positivity across a large integrated health system. Clin Infect Dis. 2020;70:262–268. doi:10.1093/cid/ciz198
3. Henning C, Aygül N, Dinnétz P, Wallgren K, Özenci V, Carroll KC. Detailed analysis of the characteristics of sample volume in blood culture bottles. J Clin Microbiol. 2019;57:e00268–e00319. doi:10.1128/JCM.00268-19
4. Hazen KC, Polage CR. Using data to optimize blood bottle fill volumes and pathogen detection: making blood cultures great again. Clin Infect Dis. 2020;70:269–270. doi:10.1093/cid/ciz203
5. Lamy B, Sundqvist M, Idelevich EA. Bloodstream infections - Standard and progress in pathogen diagnostics. Clin Microbiol Infect. 2020;26:142–150. doi:10.1016/j.cmi.2019.11.017
6. Dargère S, Cormier H, Verdon R. Contaminants in blood cultures: importance, implications, interpretation and prevention. Clin Microbiol Infect. 2018;24:964–969. doi:10.1016/j.cmi.2018.03.030
7. Doern GV, Carroll KC, Diekema DJ, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev. 2019;33:e00009–e00019. doi:10.1128/CMR.00009-19
8. Clinical and Laboratory Standards Institute (CLSI). Principles and procedures for blood cultures; approved guideline. CLSI Document M47-A. 2007;27:17.
9. Choi J, Ensafi S, Chartier LB, Van Praet O, Theodoro DL. A quality improvement initiative to decrease the rate of solitary blood cultures in the emergency department. Acad Emerg Med. 2017;24:1080–1087. doi:10.1111/acem.13161
10. McLeod Casey G. Reducing blood culture contamination in the emergency department. J Nurs Care Qual. 2020;35:245–251. doi:10.1097/NCQ.0000000000000441
11. Lee A, Mirrett S, Reller LB, Weinstein MP. Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol. 2007;45:3546–3548. doi:10.1128/JCM.01555-07
12. Tarai B, Jain D, Das P, Budhiraja S. Paired blood cultures increase the sensitivity for detecting pathogens in both inpatients and outpatients. Eur J Clin Microbiol Infect Dis. 2018;37:435–441. doi:10.1007/s10096-018-3188-8
13. Mirrett S, Weinstein MP, Reimer LG, Wilson ML, Reller LB. Relevance of the number of positive bottles in determining clinical significance of coagulase-negative staphylococci in blood cultures. J Clin Microbiol. 2001;39:3279–3281. doi:10.1128/JCM.39.9.3279-3281.2001
14. Garey KW, Rege M, Pai MP, et al. Time to initiation of fluconazole therapy impacts mortality in patients with candidemia: a multi-institutional study. Clin Infect Dis. 2006;43(1):25–31. doi:10.1086/504810
15. Lafaurie M, D’Anglejan E, Donay JL, Glotz D, Molina JM. Utility of anaerobic bottles for the diagnosis of bloodstream infections. BMC Infect Dis. 2020;20(1). doi:10.1186/s12879-020-4854-x
16. Ng LS, Kwang LL, Rao S, Tan TY. Anaerobic bacteremia revisited: species and susceptibilities. Ann Acad Med Singap. 2015;44:13–18.
17. Baron EJ, Miller JM, Weinstein MP, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2013 recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM)(a). Clin Infect Dis. 2013;57:e22–e121. doi:10.1093/cid/cit278
18. Nagy E, Urbán E, Nord CE; ESCMID Study Group on Antimicrobial Resistance in Anaerobic Bacteria. Antimicrobial susceptibility of Bacteroides fragilis group isolates in Europe: 20 years of experience. Clin Microbiol Infect. 2011;17:371–379. doi:10.1111/j.1469-0691.2010.03256.x
19. Gao Q, Wu S, Xu T, Zhao X, Huang H, Hu F. Emergence of carbapenem resistance in Bacteroides fragilis in China. Int J Antimicrob Agents. 2019;53:859–863. doi:10.1016/j.ijantimicag.2019.02.017
20. Passerini R, Cassatella Maria C, Salvatici M, et al. Recovery and time to growth of isolates in blood culture bottles: comparison of BD Bactec Plus Aerobic/F and BD Bactec Plus Anaerobic/F bottles. Scand J Infect Dis. 2014;46:288–293. doi:10.3109/00365548.2013.876510
21. Grohs P, Mainardi JL, Podglajen I, et al. Relevance of routine use of the anaerobic blood culture bottle. J Clin Microbiol. 2007;45:2711–2715. doi:10.1128/JCM.00059-07
22. Defrance G, Birgand G, Ruppé E, et al. Time-to-positivity-based discrimination between Enterobacteriaceae, Pseudomonas aeruginosa and strictly anaerobic Gram-negative bacilli in aerobic and anaerobic blood culture vials. J Microbiol Methods. 2013;93:77–79. doi:10.1016/j.mimet.2013.02.005
23. Khatib R, Saeed S, Sharma M, Riederer K, Fakih MG, Johnson LB. Impact of initial antibiotic choice and delayed appropriate treatment on the outcome of Staphylococcus aureus bacteremia. Eur J Clin Microbial Infect Dis. 2006;25:181–185. doi:10.1007/s10096-006-0096-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



