Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Effects of Acupuncture at Neiguan in Neural Activity of Related Brain Regions: A Resting-State fMRI Study in Anxiety
Authors Li C, Wang Y, Li B, Su S
Received 31 March 2022
Accepted for publication 29 June 2022
Published 6 July 2022 Volume 2022:18 Pages 1375—1384
DOI https://doi.org/10.2147/NDT.S368227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Yuping Ning
Chunlin Li,1 Yuangeng Wang,2 Baopeng Li,3 Shanshan Su4
1Department of Encephalopathy, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, People’s Republic of China; 2First College of Clinical Medicine, Shandong University of Traditional Chinese Medicine, Jinan, People’s Republic of China; 3Department of Radiology, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, People’s Republic of China; 4Department of Nephrology, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, People’s Republic of China
Correspondence: Chunlin Li, Department of Encephalopathy, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, No. 16369 Jingshi Road, Jinan, People’s Republic of China, Tel +86 137 91118881, Email [email protected]
Background: Acupuncture of PC6 points has the effects of calming, tranquilizing, regulating qi, and relieving pain and has been clinically found to alleviate anxiety disorders. To explore the mechanism of improvement at the Neiguan point acupuncture in anxiety patients, we used fMRI to observe the changes in brain function in patients with immediate anxiety before and after acupuncture at the Neiguan point.
Subjects and Methods: The experiment followed the principle of randomized, single-blind design. Twenty-four anxiety volunteers (14 males and 10 females, 20– 35 years old) were divided randomly into two groups: a group of acupuncture at Neiguan and a group of acupuncture at non-acupoint. Functional magnetic resonance imaging (fMRI) was applied to measure brain activity pre- and post-acupuncture. The amplitude of low-frequency fluctuations (ALFF) and seed-based functional connectivity (FC) was used to analyze the activity and network of brain regions. Statistical analysis was done using SPSS 21.0 and REST 1.8 software.
Results: ALFF results revealed that post-acupuncture at Neiguan increased the activity of the left parahippocampal gyrus, fusiform gyrus, and right superior temporal gyrus and decreased the activity of the right middle frontal gyrus, right precuneus, and cuneus. Post-acupuncture at non-acupoint led to a significant ALFF increase in the thalamus and middle frontal gyrus. The ALFF in the left middle frontal gyrus was decreased. Functional connectivity in several anterior default mode network (DMN) regions and vermis cerebelli at left parahippocampal/fusiform gyri was increased, and connectivity in bilateral superior temporal gyri was decreased. FC with posterior DMN regions decreased at the right middle frontal gyrus, right precuneus, and cuneus.
Conclusion: Our study elucidates that acupuncture at Neiguan modulates anxiety by activating or deactivating these brain anxiety-related regions and provides potential explanations for the application of PC6 acupuncture in mental diseases.
Keywords: PC6 acupuncture, mental disease, functional magnetic resonance imaging, functional connectivity
Introduction
Anxiety usually results from stress, which probably triggers gloomy thoughts and lasting fears that will produce more anxiety.1 As the third most common psychiatric illness, about 7.3% of the population suffered from anxiety disorders worldwide.2 Anxiety disorders often co-occur with multiple other mental diseases, such as depression and bipolar disorder, and such patients are liable to suicide.2 Anxiety disorders decrease 10.4% of the Disability Adjusted Life Years (DALYs) worldwide and bring about enormous economic and social pressure.3 Currently, treatments for anxiety disorders are mainly dependent on medication, and nonpharmacological treatments are often used as supplementary methods to enhance drug effects. Acupuncture is a traditional Chinese medicine (TCM) therapy that has been well recognized in western medicine in recent decades.4 Accumulating evidence has exhibited the effectiveness of acupuncture in various psychiatric diseases, such as depression, schizophrenia, and anxiety.5 A review systematically analyzed 32 English-language studies from 2000 to 2012 and reported that acupuncture significantly reduced the severity of anxiety.6 The most commonly used acupuncture point for anxiety relief in both human and animal experiments is PC6.
Neiguan (PC6 point) is a puncture point belonging to the pericardium channel, according to the TCM meridian and collateral theory. In TCM theory, acupuncture on the PC6 point was used to calm the mind, soothe the nerves, regulate qi, and relieve pain. In related research, acupuncture on PC6 exhibits a vital role in regulating feelings and controlling mood. Electroacupuncture on PC6 treatment decreases pain-induced anxiety-like behaviors by suppressing PKMzeta activity in the anterior cingulate cortex (ACC) in rats.7 Magnetic stimulation at the PC6 acupoint increased connections between cerebral cortex regions.8 Considering the stimulation of the posterior cingulate cortex, acupuncture at Neiguan may be a promising alternative treatment for Alzheimer’s disease and mild cognitive impairment.9 In addition, acupuncture at Neiguan could stimulate several important brain regions such as the amygdala and hippocampus, closely correlated with emotion and memory processing.10 Zhao et al reported that needling Neiguan attenuated ethanol withdrawal-induced anxiety in rats via inhibiting amygdaloid noradrenergic responses.11 However, the neural mechanism underlying the regulatory role of acupuncture in anxiety improvement is still ambiguous. When low-level laser therapy stimulates the PC6 acupuncture point, not only does the pulse rate decrease but oxygen saturation is also improved, reducing anxiety levels and effectively suppressing the vomiting reflex.12
Currently, functional magnetic resonance imaging (fMRI) has been applied to investigate the effect of acupuncture on the brain. A previous study revealed that acupuncture at Zusanli (ST36) increased the connectivity between subcortical regions and limbic/paralimbic (the amygdala, hippocampus, and anterior cingulate gyrus) to modulate emotions and cognitions.13 The amplitude of low-frequency fluctuations (ALFF), which quantitatively reflects the resting-state blood oxygen level-dependent (BOLD) signal, is a standard index to measure the activity of neurons in specific brain regions.14
For the mechanism of anxiety relief by acupuncture at the Neiguan acupuncture point may be related to the regulation of the center, this topic explores the functional changes in different brain regions affected by acupuncture at the Neiguan acupuncture point by comparing the fMRI results before and after acupuncture, to provide a basis for the mechanism of anxiety relief by acupuncture at the Neiguan acupuncture point. Therefore, in this study, we utilized fMRI to elucidate the neural mechanisms of how acupuncture at Neiguan improved anxiety symptoms. ALFF data were used to detect the activated brain regions and analyze the highly functional connected locations after acupuncture at Neiguan compared with after non-acupoint acupuncture.
Subjects and Methods
Subjects
A total of 24 (14 males and 10 females) healthy right-handed volunteers with anxiety disorders were selected and signed informed consent. All volunteers were 20 to 35 years old postgraduates of Shandong Traditional Chinese Medicine University in China. The average ages of the subjects were 25.6 ± 3.78 years for males and 26.1 ± 3.45 years for females (p < 0.05). The ethical review committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine approved the study (based on the Declaration of Helsinki (2021) Ethics Approval No. (014)–KY). The 24 volunteers were randomly divided into two groups according to a computer-generated random number table. One group (12 participants) had acupuncture at Neiguan. And the other group (12 participants) had acupuncture at non-acupoint. A single-blind method was adopted in which both groups did not know their grouping until the needling was performed.
Diagnostic Criteria
Anxiety scores of patients were evaluated by trained professionals using a self-rating anxiety scale (SAS). All volunteers were tested with the SAS score, and the scores for the SAS were between 50 to 60. The diagnosis of the anxiety disorder (ICD-10/F41) was made by an associate neurologist in charge of neurology. The diagnostic criteria refer to the diagnostic criteria of anxiety in the Chinese Classification and Diagnostic criteria for Mental Disorders (3rd Edition) [(CCMD-3)] issued in 2001. The inclusion and exclusion criteria of volunteers are shown in Figure 1.
 |
Figure 1 Volunteers inclusion and exclusion criteria. |
Interventions
Both the experimental group and the control group underwent MRI examination before the acupuncture operation. The experimental group was given the operation of acupuncture at Neiguan, and the needles were retained for 15 minutes after obtaining Qi, while the control group was given the non-acupuncture points and retained for 15 minutes. MRI examination was performed after the end of acupuncture. All the volunteers received training for fMRI analysis to banish fear and were given 15 minutes of instructions in a quiet environment. The contents include the following: the MRI examination is in a relatively closed environment, the air is relatively uncirculated, and accompanied by various noises, etc., may bring discomfort to the subject, the subject should be prepared psychologically in advance, and the subject should be provided with earplugs to ensure a comfortable ambient temperature. We used the manic earplugs (3M, USA) to block their ears to reduce noise disturbance and a head coil with a sponge to fix the heads of the participants to reduce head motion. When fMRI was performed, the participants were requested to close their eyes, stay in stillness and avert emotional activities. The acupuncturist then performed the acupuncture operation. After finishing the acupuncture, the volunteer rests for 15 minutes and then undergoes an MRI.
fMRI Analysis
All the fMRI analyses were performed on a 3.0T whole-body Achieva MRI scanner (Philips, UK) with an 8-channel radio frequency coil in the Affiliated Hospital of Shandong Traditional Chinese Medicine University. fMRI images were acquired using a gradient echo–echo planar imaging (GRE-EPI, TR/TE/FA 3000 mm/35 mm/90°, FOV 230 mm × 230 mm, slice thickness/gap 5.0 mm/0 mm, and matrix 128 × 128, interlayer scanning).
Acupuncture Manipulation
The acupuncture needles with a size of 40 mm × 0.40 mm (Old Silversmith Company, Hong Kong, China) were administered by an acupuncturist who has been practicing for at least 10 years. And the non-acupoint was located 2-cm to the left of Neiguan point (Figure 2). In the acupuncture group, the acupoints were selected according to the international standardized protocol, and the acupuncture points were selected from the left side of the limb, and the acupuncture points were directly stabbed 0.3 inches after routine alcohol disinfection. The needle is retained for 15 minutes after the status of De-Qi is obtained by the lifting and twisting technique. The amplitude of twisting is generally mastered at about 180°–360°. The amplitude of lifting and inserting is 3–5 minutes, and the frequency is 120–160 times/minute. During acupuncture, the De-Qi sensation should be elicited, which includes soreness, numbness, swelling, and pain. The volunteers then answered feeling questionnaires about the sensations including soreness, numbness, fullness, and aching experienced on the stimulated acupoints. A professional acupuncturist operated acupuncture. The fMRI was performed pre-and post-acupuncture, respectively, for every volunteer.
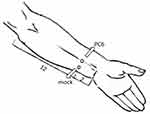 |
Figure 2 Diagram of acupoints. |
Data Pre-Processing and Calculating
Graph-theoretical Network Analysis Toolkit (GRETNA) and Resting-State fMRI Data Analysis Toolkit (REST) were applied to process the data. The first 10 volumes were abandoned for the adaptation of subjects to scanning and the signal equilibrium. Subsequently, slice timing, head motion correction, spatial normalization to the Montreal Neurological Institute (MNI) template (resampling voxel size = 3mm × 3mm × 3mm), linear trend removal, temporal bandpass filtering (0.01–0.08 Hz), and then spatially smoothed with a Gaussian filter of full width at half maximum of 4mm were conducted. For quality control, exclusion criteria include (1) the patients who were found to have the organic disease or anatomical structure asymmetry in the brain after fMRI; (2) patients who fail to complete the fMRI scan; (3) fMRI scanning with excessive data noise brutal to be calibrated. Moreover, none of the patients were excluded. Other parameters, including friston 24 head motion signals, and ventricular and white matter, were regressed out.
After linear regression by DPARSF 2.3 software, the amplitude of low-frequency fluctuations (ALFF, 0.01–0.1 Hz) values were calculated by convolving the extracted time curve with a Hamming bandpass filter for the whole-brain voxels. Then, ALFF map was obtained and standardized by dividing the map by average ALFF values. The standardized ALFF values of pre- and post-acupuncture at non-acupoint and Neiguan were calculated with a paired t-test to find significantly changed brain regions. For functional connectivity (FC) analysis, the significantly changed brain regions were set as seeds. The functional connectivity between the seeds and other brain regions was conducted. The results were uncorrected with P < 0.01.
Analysis
SPSS21.0 statistical software was used to analyze the data. Q test was used to compare the measurement data between groups, described as mean ± standard deviation (±s), and χ2 test was used to compare the count data. P was a two-sided test, and p < 0.05 was considered a significant difference; p < 0.01 was considered a very significant difference.
A two-sample t-test was performed using REST 1.8 software for each of the voxels at the corresponding location in the smoothed standardized ALFF maps of the 2 groups, and the difference was statistically significant at P < 0.05 (uncorrected) and voxel range ≥10 for each pair of voxels. The ALFF brain region (difference brain region) to which the peak point belonged was determined according to REST 1.8 software. The different brain regions of the 2 groups were set as seed points, and the functional connections between each seed point and other brain regions were analyzed separately.
Results
fMRI Analysis
All 24 participants were included for data analysis. And there was no significant difference in fMRI results between the two groups before acupuncture. The results of fMRI from the patients punctured in the Neiguan group showed a positive activation in the left parahippocampal, occipitotemporal lobe, and right superior temporal gyrus; and a negative activation in the right middle frontal gyrus, right precuneus, and cuneus (Figure 3A and B). The peak voxels within those significantly different clusters are shown in Table 1.
 |
Table 1 Peak Voxels Within Significantly Different Clusters After Acupuncture at Neiguan |
When volunteers were acupunctured at non-acupoint, we detected a significant ALFF increase in the thalamus and middle frontal gyrus. Additionally, a decreased ALFF in the left middle frontal gyrus was detected (Figure 4A and B, Table 2).
 |
Table 2 Peak Voxels Within Significantly Different Clusters After Acupuncture at Non-Acupoint |
Functional Connectivity (FC) Analysis
To detect the functional connectivity of brain regions with the positively and negatively activated regions for acupuncture at Neiguan, seed-based functional connectivity was performed in a sphere with a radius of 4 mm (Table 3). We set the activated regions as seeds, and then a paired t-test analysis was performed. Seed-based FC analysis seeding at left parahippocampal and occipitotemporal convolution for positively activated regions showed increased FC in the vermis cerebelli and left occipitotemporal left gyrus frontalis inferior, and angular convolution. Right superior temporal gyrus seed revealed increased functional connectivity with right cerebellar hemispheres, right middle temporal gyrus, right gyrus frontalis inferior, right orbitofrontal back, right occipitotemporal convolution, gyrus lingualis, and right anterior central gyrus. Besides, there was a decreased connectivity between the right superior temporal gyrus seed and the left superior temporal gyrus.
 |
Table 3 Seed-Based Functional Connectivity (FC) Analysis After Acupuncture at Neiguan |
For negatively activated regions, we observed decreased FC between the right middle frontal gyrus and heterolateral middle frontal gyrus, cuneus and gyrus angularis, right precuneus/cuneus, and homolateral orbitofrontal back and precuneus (Table 3).
Discussion
Previous studies on the function of brain regions in which acupuncture improves anxiety are mostly animal experiments.14 Fewer studies have been conducted from a clinical trial perspective.
In the present study, we investigated the role of acupuncture at Neiguan acupoint in relieving anxiety using fMRI. After acupuncture, the feeling questionnaire exhibited that acupuncture at Neiguan obviously resulted in sensations compared to non-acupoint acupuncture, suggesting the effectiveness of acupuncture. ALFF results revealed that post-acupuncture at Neiguan increased the activity of the left parahippocampal gyrus, fusiform gyrus, and right superior temporal gyrus, and the activity of the right middle frontal gyrus, right precuneus, and cuneus was decreased compared to pre-acupuncture. As one of the main lobes in the cortex, the temporal lobe plays an essential role in cognition, such as the procession of emotion, memory, and language. About 19% of patients with temporal lobe epilepsy had an anxiety disorder, suggesting the linkage of temporal lobe dysfunction with anxiety.15 The parahippocampal gyrus, located between the hippocampus and temporal lobe, functions in spatial memory and navigation. Lines of evidence have reported that the activity of the parahippocampal gyrus is involved in the regulation of sensory memory.16–18 Davies et al reported that anxiety is associated with the abnormal activation of the parahippocampal gyrus.19 Cannabidiol, which had anxiolytic effects, augmented the activation of the parahippocampal gyrus in patients with anxiety compared to placebo.20 Besides, the fusiform gyrus, lying below the parahippocampal gyrus, is involved in several recognition-related neural pathways. The dysregulation of the fusiform gyrus takes the primary responsibility for cognitive disorders and several mental diseases.21,22 Park et al demonstrated that shift workers who had anxiety and depression disorders had decreased cerebral blood flow in the parahippocampal/fusiform gyrus compared to day workers.23 Patients with major depressive disorder showed decreased fusiform gyrus activity during emotional face procession.24 Our study observed increased ALFF in the left parahippocampal/fusiform gyrus and right superior temporal gyrus. Combining our results with these previous studies, we reasonably infer that it is partially through activating the parahippocampal/fusiform gyrus and right superior temporal gyrus that acupuncture at Neiguan improved anxiety symptoms.
In addition, in our study, acupuncture at Neiguan decreased the activity of the right middle frontal gyrus, right precuneus, and cuneus compared to pre-acupuncture. The middle frontal gyrus, a significant component of the frontal lobe, showed an enhanced response to angry faces in anxiety patients.25 The precuneus is a part of the cuneus in front of the occipital lobe. Yuan et al reported that anxiety and depression were positively correlated with hyper-function of precuneus.26 Additionally, accumulating studies have reported that the middle frontal gyrus and precuneus are hyperactivated in patients with anxiety.26–28 Therefore, acupuncture at Neiguan, which deactivated these brain regions, could help ease patients’ anxiety.
Moreover, after non-acupoint acupuncture, the ALFF value in the right thalamus was augmented. Thalamus has intimate connections with the amygdala, which is a crucial region regulating neural pathways of anxiety disorders.29 Besides, contrary to acupoint acupuncture, non-acupoint acupuncture elevated the right middle frontal gyrus, which plays a positive role in anxiety degree.25 Thus, we inferred that non-acupoint acupuncture activating the thalamus and right middle frontal gyrus might have no effects on or even aggravate the anxiety.
Furthermore, FC was performed to analyze the interested region-related brain networks changed by acupoint acupuncture. The results revealed increased functional connectivity of left parahippocampal/fusiform gyri with homolateral vermis cerebelli, gyrus frontalis inferior, and gyrus angular. And the FC of the right superior temporal gyrus with homolateral cerebellar hemisphere, gyrus temporalis medius, gyrus frontalis inferior, gyrus frontalis inferior, and fusiform gyrus increased also. Hippocampal, superior temporal gyrus, gyrus frontalis inferior, gyrus temporalis medius, Orbitofrontal back, and gyrus angularis are significant components of anterior default mode network (DMN), the abnormal activity of which was responsible for the anxiety syndrome.30 Several investigations have reported the separation of DMN in major depression patients.31,32 Consistently, our results revealed that acupuncture at Neiguan enhanced the connectivity of these anterior DMN regions and relieving anxiety. Contrarily, the FC of right middle frontal gyrus with heterolateral middle frontal gyrus, cuneus and gyrus angularis, right precuneus/cuneus with right orbitofrontal back, and right precuneus was declined after acupuncture at Neiguan. The middle frontal gyrus, precuneus, and cuneus were posterior DMN regions, which are responsible for perpetual processing and autobiographical memory. Zhao X-H et al reported that the connectivity of posterior DMN was positively correlated with anxiety.33 Therefore, in our study, acupoint acupuncture could decrease FC of posterior DMN regions to reduce anxiety symptoms.
Baptiste et al highlighted the critical role of gyrus lingualis in anxiety and depression.34 They found that the volume of right gyrus lingualis was reduced in these patients.34 Additionally, the cerebellum and prefrontal gyrus are two crucial brain regions associated with emotional experience.35 Verhoeven et al reported that neuroimaging of Phelan-McDermid patients suggested severe major depression in them and structural imperfection in vermis cerebelli.36 The connectivity between the motor cortex and right hippocampus was reported to be stronger in patients who stutter when they were in a high level of anxiety.37 However, no study investigated the connectivity of DMN between the two regions. In our study, for the first time, we found that acupoint acupuncture augmented the connectivity of the right superior temporal gyrus with prefrontal gyrus and right cerebellar hemispheres, left parahippocampal/fusiform gyri, and vermis cerebelli. In addition, hypoconnectivity was observed in the bilateral superior temporal gyri. Consistently, Zhao et al detected that the defective connectivity between bilateral superior temporal gyri caused abnormal activity in anxiety patients.38 Moreover, after non-acupoint acupuncture, the ALFF value in the right thalamus was augmented. Thalamus has intimate connections with the amygdala, which is a crucial region regulating neural pathways of anxiety disorders. Besides, contrary to acupoint acupuncture, non-acupoint acupuncture elevated the right middle frontal gyrus, which plays a positive role in anxiety degree. Thus, we inferred that non-acupoint acupuncture might aggravate the anxiety by activating the thalamus and right middle frontal gyrus.
In this study, the differential brain areas with changes in whole-brain functional connectivity after acupuncture at the Neiguan acupuncture point reflected the main effect sites of acupuncture points for the treatment of grafted women, reflecting the basic pattern of acupuncture point-brain functional area connection and effect and, to some extent, illustrating the modulatory effect of acupuncture at the Neiguan acupuncture point on the brain functional areas responsible for emotion regulation, which has research implications for revealing the mechanism of action of acupuncture for anxiety. It provides a theoretical basis for the subsequent study of acupuncture point combination and acupuncture point regularity for irritable and anxious states in TCM.
Limitations
In addition to the small sample size due to funding issues, image perturbation and blurring are also important factors affecting the study, and subjects were instructed to keep their head position as stable as possible. No distinction was made between the sexes of the subjects. Females had a higher proportion of gray matter tissue and greater intracerebral connectivity compared to males who had a high proportion of white matter in the limbic region of the brain, whereas males had high interhemispheric connectivity; therefore, follow-up studies should further refine the gender grouping.
Conclusion
In the present study, acupuncture at the Neiguan acupoint altered the activity of several brain regions, which exerted essential roles in the modulation of anxiety. In summary, acupuncture of the Neiguan point produced a modulatory effect on brain regions responsible for emotions, providing some basis for the study of brain mechanisms of acupuncture of the Taichong point for the treatment of irritability and anxiety.
Acknowledgments
This work was funded by the Traditional Chinese Medicine Science and Technology Development Program of Shandong Province (2019-0110) and Jinan 2020 Science and Technology Innovation Development Plan (Clinical Medicine Science and Technology Innovation Plan) (202019152).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vismara M, Girone N, Cirnigliaro G. Peripheral biomarkers in DSM-5 anxiety disorders: an updated overview. Brain Sciences. 2020;10. doi:10.3390/brainsci10080564
2. Alonso J, Liu Z, Evans-Lacko S, et al. Treatment gap for anxiety disorders is global: results of the World Mental Health Surveys in 21 countries. Depress Anxiety. 2018;35:195–208. doi:10.1002/da.22711
3. Murrough JW, Yaqubi S, Sayed S, Charney DS. Emerging drugs for the treatment of anxiety. Expert Opin Emerg Drugs. 2015;20:393–406. doi:10.1517/14728214.2015.1049996
4. Gu T, Lin L, Jiang Y, et al. Acupuncture therapy in treating migraine: results of a magnetic resonance spectroscopy imaging study. J Pain Res. 2018;11:889–900. doi:10.2147/JPR.S162696
5. Tu CH, MacDonald I, Chen YH. The effects of acupuncture on glutamatergic neurotransmission in depression, anxiety, schizophrenia, and Alzheimer’s disease: a review of the literature. Front Psychiatry. 2019;10:14. doi:10.3389/fpsyt.2019.00014
6. Errington-Evans N. Acupuncture for anxiety. CNS Neurosci Ther. 2012;18:277–284. doi:10.1111/j.1755-5949.2011.00254.x
7. Du J, Fang J, Wen C, et al. The effect of electroacupuncture on PKMzeta in the ACC in regulating anxiety-like behaviors in rats experiencing chronic inflammatory pain. Neural Plast. 2017;2017:3728752. doi:10.1155/2017/3728752
8. Yu HL, Xu GZ, Guo L, et al. Magnetic stimulation at Neiguan (PC6) acupoint increases connections between cerebral cortex regions. Neural Regen Res. 2016;11:1141–1146. doi:10.4103/1673-5374.187053
9. Zhang G, Yin H, Zhou YL, et al. Capturing amplitude changes of low-frequency fluctuations in functional magnetic resonance imaging signal: a pilot acupuncture study on NeiGuan (PC6). J Altern Complement Med. 2012;18:387–393. doi:10.1089/acm.2010.0205
10. Dhond RP, Yeh C, Park K, Kettner N, Napadow V. Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain. 2008;136:407–418. doi:10.1016/j.pain.2008.01.011
11. Zhao Z, Kim SC, Liu H. Manual acupuncture at PC6 ameliorates acute restraint stress-induced anxiety in rats by normalizing amygdaloid noradrenergic response. Evid-Based Complementary Altern. 2017;2017:1–8. doi:10.1155/2017/4351723
12. Goel H, Mathur S, Sandhu M, et al. Effect of low-level laser therapy on P6 acupoint to control gag reflex in children: a clinical trial. J Acupunct Meridian Stud. 2017;10(5):317–323. doi:10.1016/j.jams.2017.07.002
13. Feng Y, Bai L, Ren Y, et al. Investigation of the large-scale functional brain networks modulated by acupuncture. Magn Reson Imaging. 2011;29:958–965. doi:10.1016/j.mri.2011.04.009
14. Zang YF, He Y, Zhu CZ, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev. 2007;29:83–91. doi:10.1016/j.braindev.2006.07.002
15. Bassetto RM, Wscieklica T, Pouza KCP, et al. Effects of electroacupuncture on stress and anxiety-related responses in rats. An Acad Bras Cienc. 2017;89:1003–1012. doi:10.1590/0001-3765201720160531
16. Pope RA, Thompson PJ, Rantell K, Stretton J, Wright MA, Foong J. Frontal lobe dysfunction as a predictor of depression and anxiety following temporal lobe epilepsy surgery. Epilepsy Res. 2019;152:59–66. doi:10.1016/j.eplepsyres.2019.03.003
17. Cabeza R, Rao SM, Wagner AD, Mayer AR, Schacter DL. Can medial temporal lobe regions distinguish true from false? An event-related functional MRI study of veridical and illusory recognition memory. Proc Natl Acad Sci USA. 2001;98:4805–4810. doi:10.1073/pnas.081082698
18. Mather M, Henkel LA, Johnson MK. Evaluating characteristics of false memories: remember/know judgments and memory characteristics questionnaire compared. Mem Cognit. 1997;25:826–837. doi:10.3758/BF03211327
19. Norman KA, Schacter DL. False recognition in younger and older adults: exploring the characteristics of illusory memories. Mem Cognit. 1997;25:838–848. doi:10.3758/BF03211328
20. Davies C, Wilson R, Appiah-Kusi E, et al. A single dose of cannabidiol modulates medial temporal and striatal function during fear processing in people at clinical high risk for psychosis. Transl Psychiatry. 2020;10:311.
21. Harvey PO, Pruessner J, Czechowska Y, Lepage M. Individual differences in trait anhedonia: a structural and functional magnetic resonance imaging study in non-clinical subjects. Mol Psychiatry. 2007;12(703):767–775. doi:10.1038/sj.mp.4002021
22. Kroes MC, Rugg MD, Whalley MG, Brewin CR. Structural brain abnormalities common to posttraumatic stress disorder and depression. J Psychiatry Neurosci. 2011;36:256–265. doi:10.1503/jpn.100077
23. Park YK, Kim JH. Altered regional cerebral blood flow associated with mood and sleep in shift workers: cerebral perfusion magnetic resonance imaging study. J Clin Neurosci. 2019;15:438–447. doi:10.3988/jcn.2019.15.4.438
24. Pujol J, Harrison BJ, Ortiz H, et al. Influence of the fusiform gyrus on amygdala response to emotional faces in the non-clinical range of social anxiety. Psychol Med. 2009;39:1177–1187. doi:10.1017/S003329170800500X
25. Karina Blair PD, Jonathan Shaywitz MD, Bruce W, et al. Response to emotional expressions in generalized social phobia and generalized anxiety disorder: evidence for separate disorders. Am J Psychiatry. 2008;165:1193–1202. doi:10.1176/appi.ajp.2008.07071060
26. Yuan C, Zhu H, Ren Z, et al. Precuneus-related regional and network functional deficits in social anxiety disorder: a resting-state functional MRI study. Compr Psychiatry. 2018;82:22–29. doi:10.1016/j.comppsych.2017.12.002
27. Blair K, Shaywitz J, Smith BW, et al. Response to emotional expressions in generalized social phobia and generalized anxiety disorder: evidence for separate disorders. Am J Psychiatry. 2008;165:1193–1202.
28. Schlund MW, Verduzco G, Cataldo MF, Hoehn-Saric R. Generalized anxiety modulates frontal and limbic activation in major depression. Behav Brain Funct. 2012;8:8. doi:10.1186/1744-9081-8-8
29. Asami T, Yoshida H, Takaishi M, et al. Thalamic shape and volume abnormalities in female patients with panic disorder. PLoS One. 2018;13:e0208152. doi:10.1371/journal.pone.0208152
30. Yan R, Tao S, Liu H, et al. Abnormal alterations of regional spontaneous neuronal activity in inferior frontal orbital gyrus and corresponding brain circuit alterations: a resting-state fMRI study in somatic depression. Front Psychiatry. 2019;10:267. doi:10.3389/fpsyt.2019.00267
31. Bluhm R, Williamson P, Lanius R, et al. Resting state default-mode network connectivity in early depression using a seed region-of-interest analysis: decreased connectivity with caudate nucleus. Psychiatry Clin Neurosci. 2009;63:754–761. doi:10.1111/j.1440-1819.2009.02030.x
32. Zhu X, Wang X, Xiao J, et al. Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biol Psychiatry. 2012;71:611–617. doi:10.1016/j.biopsych.2011.10.035
33. Zhao X-H, Wang P-J, Li C-B, et al. Altered default mode network activity in patient with anxiety disorders: an fMRI study. Eur J Radiol. 2007;63:373–378. doi:10.1016/j.ejrad.2007.02.006
34. Couvy-Duchesne B, Strike LT, de Zubicaray GI, et al. Lingual gyrus surface area is associated with anxiety-depression severity in young adults: a genetic clustering approach. eneuro. 2018;5:
35. Picó-Pérez M, Radua J, Steward T, Menchón JM, Soriano-Mas C. Emotion regulation in mood and anxiety disorders: a meta-analysis of fMRI cognitive reappraisal studies. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79:96–104. doi:10.1016/j.pnpbp.2017.06.001
36. Verhoeven WM, Egger JI, Willemsen MH, de Leijer GJ, Kleefstra T. Phelan-McDermid syndrome in two adult brothers: atypical bipolar disorder as its psychopathological phenotype? Neuropsychiatr Dis Treat. 2012;8:175–179. doi:10.2147/NDT.S30506
37. Yang Y, Jia F, Siok WT, Tan LH. The role of anxiety in stuttering: evidence from functional connectivity. Neuroscience. 2017;346:216–225. doi:10.1016/j.neuroscience.2016.11.033
38. Zhao X, Xi Q, Wang P, Li C, He H. Altered activity and functional connectivity of superior temporal gyri in anxiety disorders: a functional magnetic resonance imaging study. Korean J Radiol. 2014;15:523–529. doi:10.3348/kjr.2014.15.4.523
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


