Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Effectiveness of a Multifaceted Educational Intervention to Enhance Therapeutic Regimen Adherence and Quality of Life Amongst Iranian Hemodialysis Patients: A Randomized Controlled Trial (MEITRA Study)
Authors Zhianfar L, Nadrian H , Asghari Jafarabadi M , Espahbodi F , Shaghaghi A
Received 24 January 2020
Accepted for publication 31 March 2020
Published 14 April 2020 Volume 2020:13 Pages 361—372
DOI https://doi.org/10.2147/JMDH.S247128
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Leila Zhianfar,1 Haidar Nadrian,2 Mohammad Asghari Jafarabadi,3 Fatemeh Espahbodi,4 Abdolreza Shaghaghi1
1Health Education & Promotion Department, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran; 2Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran; 3Epidemiology and Biostatistics Department, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran; 4Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
Correspondence: Abdolreza Shaghaghi
Health Education & Promotion Department, Faculty of Health, Tabriz University of Medical Sciences, Golgasht Ave, Tabriz, P.C 516667411, Iran
Tel +98 41 33376227
Email [email protected]
Purpose: A multimodal intervention designed and executed to improve therapeutic regimen adherence and quality of life in a sample of Iranian hemodialysis patients. Its feasibility and impact was assessed post intervention.
Patients and Methods: This randomized controlled trial (RCT) study was conducted at two hemodialysis wards of the Shahrvand hospital located in Sari, the capital city of the Mazandaran province, north of Iran. The study sample included patients with end-stage renal disease (ESRD) receiving outpatient hemodialysis treatment. Considering 10% attrition, 70 registered patients were randomly categorized into intervention and control groups. The proposed intervention included playing of relevant educational video tracks, conducting eight cognitive behavioral therapy (CBT) group sessions, and telephone-based peer support. Data were collected applying a set of questionnaires including sociodemographic, Beck Depression Inventory (BDI-SF), Multidimensional Scale of Perceived Social Support (MSPSS), Patient Satisfaction with Nursing Care Quality Questionnaire (PSNCQQ), End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ) and the World Health Organization Quality of Life (WHOQOL-SF) scale. Sociodemographic and clinical data were collected at baseline in both groups and the postintervention assessment was performed in the intervention and nonintervention groups after one month and three months.
Results: A significant change in the self-reported depression symptoms (P=0.001), mean social support score (P=0.001), nursing care satisfaction score (P=0.001), quality of life score (P=0.001) and interdialytic weight gain (IDWG) (P=0.001) was observed among the participants in the intervention group compared to the baseline measures. The highest rise in the ESRD-AQ scores within the intervention group was observed after one month of intervention (mean difference=131.88) compared to the baseline values. Same pattern of statistically significant changes in mean scores of the intervention group’s attendants in all subscales of the ESRD-AQ were also ascertained.
Conclusion: This interventional study revealed that inaugurating of a feasible low-cost intervention without need to add major logistic or financial inputs into existing health-care systems, especially in resource limited contexts, is achievable. Findings of this study could provide insights into scientific basis of evidence-informed interventions applicable in the realm of health-care delivery.
Keywords: hemodialysis patients, intervention, adherence
Introduction
Patients with chronic kidney disease (CKD) generally need complex and costly hospital-based care with prolonged multidrug treatment throughout their lives which is difficult to follow due to the overwhelming burden of the illness and long time input needed to fulfil the therapy objective.1 The standard care protocol for CKD patients may include hemodialysis, drug therapy and dietary recommendations to restrict fluid and sodium intake.2
The outward increasing trend of CKD incidence worldwide and reaching the eighteenth rank in the 2010 list of global death causes (with an annual rate of 16.3 per 100,000) warrants attention and action to promote the therapy outcome and patients’ quality of life.3
Nonadherence to the therapeutic regimen by hemodialysis patients (HDPs) is a common incident worldwide that could pose serious medical, social, and economic consequences for patients, their families and wider communities.4
Available research evidence pointed out to current dilemma in fluid restriction among 9.7–72% of the HDPs,5,6 poor adherence to medication in the range of 3–80% and not following recommended dietary restrictions in 2–81% of the CKD sufferers.7,8
A meagre amount of studies that exist to examine the effectiveness of several interventions on boosting therapeutic adherence by HDPs often relied on small sample sizes and nonrandom designs.9,10
Knowledge enhancement was also reported to be the main executed intervention to improve behavioral profile among HDPs but it is likewise suggested that knowledge improvement interventions are insufficient for maintenance of the modified behaviors in the long-term per se.11 Instead, application of a multifaceted intervention approach that excogitate and contrive mental status and social support along with application of alternating information delivery methods were recommended to boost effectiveness of interventions.12,13
Depression, for instance, as a common comorbidity in end stage renal disease (ESRD) patients with overall estimated prevalence rates of 20–44%14 was reported to interfere with the therapeutic regimen adherence15,16 and impair interdialytic weight control among the patients.16 Cognitive behavioral therapy (CBT), in consequence, was recommended to be included in the intervention packages to ameliorate ESRD patients’ therapeutic adherence.17 Provision of social support18,19 and peer support20,21 are other suggested propositions to add to the value of interventions that address therapeutic regimen adherence among CKD patients.
Follow-up and facilitating complete adherence to the crucial therapeutic and lifestyle recommendations in HDPs may be burdensome especially in resource limited countries where a baseline shortage of logistic infrastructure including manpower and financial resources may pose serious health risks for the patients and financial restraints to the health systems and wider communities.
The main aim of this study was to assess feasibility and impact of a multimodal intervention designed to improve therapeutic and lifestyle adherence recommendations in a sample of Iranian HDPs and to inform future mitigation projects that seek to strengthen and enhance therapeutic and lifestyle adherence recommendations in the Iranian HDPs hence, to improve their quality of life.
Patients and Methods
Study Design
This randomized controlled trial study (registration number: IRCT20171213037859N1) was conducted in two hemodialysis wards at the Shahrvand hospital located in Sari, the capital city of the Mazandaran province, north of Iran. The study sample included patients with ESRD receiving outpatient hemodialysis treatment (average of four hours per session, three times a week).
Sample Size
The sample size was decided based on the reported rate of fluid restriction adherence in the study of Zolfaghari et al22 and considering 10% attrition, 35 registered patients were randomly selected in each of the two proposed hospitals which had been randomly tagged as distinctive intervention and control groups.
Participant Recruitment
To recruit the study sample 110 hemodialysis patients were approached from 10 September to 22 October 2018, of them, 70 (63.63%) agreed to give their informed consent for participation in the study. To comply with the research ethics guideline on inclusion of human subjects in research, confidentiality of the study data, patients’ voluntary participation in the study, and their right to withdraw in any stage and without obligation to give any reason were explained at the start of the study. The study respondents were only included after reading the study information sheet (or by their guardians) and giving their written informed consent. The study inclusion criteria were being diagnosed with the ESRD and receiving hemodialysis for at least three months, being 18 years of age or older and being independent for doing daily activities (walking, eating etc) with at least reading and writing literacy level. The exclusion criteria were having a diagnosis of mental or cognitive problems, use of antidepressants and having a depression score of less than four (according to the Beck Depression Inventory scoring mechanism).
Ethical Consideration
The study protocol was approved by the institutional level Medical Research Ethics Board of Trustees (MREBoT) at the Tabriz University of Medical Sciences (approval number: IR.TBZMED.REC.1397.425). All the study participants were requested to give their written informed consent after receiving adequate information about the study aim and procedures. The trial stages were also implemented in accordance with principles of the Helsinki Declaration. Access to the study data will be granted by the corresponding author on reasonable request.
Data Collection Measures
The Beck Depression Inventory (BDI-SF) is a 13-item questionnaire23 that assesses depressive symptomatology and consists of cognitive and somatic subscales. The scale’s items have four options of Likert-type response categories ranging from 0–3. Thus, every individual respondent could obtain an overall scale score in the range of 0–39 with higher scores indicating a greater level of depressive symptoms (ie a score of 0–3 represents normal psychological status or no depression, 4–7 presence of a mild depression, 8−11 mild to moderate depressive illness, 12−15 moderate depressive state, and 16–39 existence of severe depression among the respondents). Validity of the BDI-SF was formerly tested for use among Persian-speaking patients with chronic disorder.24
The Multidimensional Scale of Perceived Social Support (MSPSS) is a 12-item questionnaire25 that measures the respondents’ perceived social support coming from three sources, ie family members, friends and the most important people in the patient's life. The 12 items of the applied version of MSPSS26 in this study have five-point Likert-type response options ranging from 1 (strongly disagree) to 5 (strongly agree). The minimum total score of a respondent could be in the range of 12–60. A score of 12–24 indicates low perceived social support, 24–36 an average level of social support, and a score above 36 a high level of perceived social support. This scale’s validity and reliability for use among the Persian-speaking population were verified in previous studies.27
The Patient Satisfaction with Nursing Care Quality Questionnaire (PSNCQQ) has 19 items, plus two additional questions in four sub-categories, ie knowledge and professional skill (seven items), communication (four items), nursing ethics (five items) and patient education (five items).28 The PSNCQQ was developed to measure satisfaction with the overall quality of care during the hospital stay, overall quality of nursing care, and intention to recommend the hospital to family and friends. The PSNCQQ’s items have five-point Likert-type response options ranging from poor (1) to excellent (5) therefore; an individual interviewee could attain a total score in the range of 21–105 with score of 21–49 representing low satisfaction, 50–77 relatively desirable satisfaction, and 78–105 a high level of satisfaction. The translated Persian version of the PSNCQQ was psychometrically approved for use among Persian-speaking populations earlier by Negarandeh et al.29
The End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ) measures adherence of ESRD patients to the recommended self-care behaviors including limitation of fluid intake, change in dietary pattern, regular medication use and keeping up with scheduled dialysis sessions. The ESRD-AQ consists of 46 questions/items in five sections.30 The first section pursues general information about patients’ ESRD history (five items), the second section contains questions about HD treatment and attendance (14 items), the third section has questions about medications’ use (nine items), the fourth section contains questions about adherence to fluid restrictions (10 items) and fifth section has questions about adherence to diet recommendations (eight items). The response ranges to the ESRD-AQ’s items include a combination of Likert-type scales, multiple choices and “yes/no” answer options and higher overall scores indicate better adherence. The instrument was formerly validated for use among Persian-speaking patients31 and indicated acceptable psychometric properties.
The World Health Organization Quality of Life (WHOQOL-SF) questionnaire32 contains 26 items with five-point Likert-type response options. The instrument assesses interviewees’ quality of life in four broad areas, ie physical health, psychological health, social relationships, and the environment. The overall score value for an individual respondent could range from 26–130, with higher scores indicating a better quality of life.
Study Procedures
Random allocation was applied to assign the study participants into intervention and control groups. Sociodemographic and clinical data were collected at baseline in both groups and the proposed intervention was tailored to the individual participants’ literacy level at two layers, ie patients’ and their families and nursing staff over eight weeks’ time. The postintervention assessment of the changes was performed in the intervention and nonintervention groups after one month and three months to examine stability of changes over time.
Intervention
The proposed intervention in this study in adherence with the general recommendations33–35 for better compliance of patients with chronic medical conditions to educational interventions, included playing of relevant video tracks to sensitize the patients and their family members to the importance of full adherence to the therapeutic regimen, conduction of eight CBT group sessions as deemed necessary and congruous to the patients’ preferences along with telephone-based peer support conciliation to assist them in better adaptation with their illness and hemodialysis therapy. The educational video tracks had been displayed in three consecutive sessions about an hour after the start of dialysis therapy when the patients were in a stable and convenient situation. In the third session an experienced nephrologist was also invited to answer the patients or their family members’ questions about the HDPs’ medical conditions or prescribed therapeutic regimen. Practicing nurses in the study venue also received the educational video tracks in their social media repositories to familiarize them with the content ready for answering the patients probable questions.
Two informative pamphlets were also distributed among the patients and their next of kin to explain the main medications commonly prescribed for HDPs and the reasons and importance of diet and fluid restrictions in CKD patients who undertake hemodialysis.
The CBT group sessions were scheduled based on the reported advantages regarding its effectiveness and efficiency in reducing depression and anxiety symptoms of the chronic disease sufferers36,37 and due to logistic limitations in planning and administration of individually tailored CBT interventions. Thus, a series of eight group CBT sessions were organized and an invited psychiatrist provided his consultation about the strategies to accommodate the health conditions resulting from the CKD. The sessions were assigned after the end of hemodialysis therapy and each session lasted about 90 minutes.
The peer support intervention to improve the study participants’ therapeutic adherence was programmed to be implemented by volunteer peers with almost identical characteristics to the patients. All the appointees were briefed for basic communication skills and the area that must be focused on amid support tasks’ fulfillment. These volunteers were invited to be in contact with a maximum of seven patients with at least four follow-up telephone calls and care support a week. Flexibility of the duration of the phone callsand making their contents compatible with the patients’ needs and preferences were also addressed during the peer briefing sessions as recommended in other studies.38
Further to the abovementioned interventions the importance of emotional and instrumental support of the patients was emphasized for the guardian family members and two videos about effective communication skills were shared with the hemodialysis wards’ practicing nurses in their preferred social media. A summary of the interventions linked to the employed strategies and the determined target groups is shown in Table 1.
 |
Table 1 The Employed Intervention Strategies and Types of Activities to Enhance Therapeutic Regimen Adherence and Quality of Life in the MEITRA Study |
Data Analysis
The study’s qualitative and quantitative variables comparisons were performed using chi-squared and independent t-tests. Paired t-test was used to compare quantitative variables within groups. Covariance analysis was utilized to assess the impact of the intervention on the outcome variables after adjusting for baseline values as well as potential confounders. Data analysis was executed by SPSS 24 software (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY, USA: IBM Corp (released 2016) at the significant level of 0.05.
Results
Among the approached 70 patients in the two study groups only 33 participants in each group (94.28%) completed the study without major violation of the intended protocol. The dropout patients included three patients who personally requested to be transferred to other hemodialysis centers and one patient who died after start of the study. The study attendees were homogeneous regarding sociodemographic characteristics, the disease-related therapeutic adherence behaviors and some other baseline health conditions as connoted in Tables 2 and 3.
 |
Table 2 Sociodemographic Attributes of the Participants in the MEITRA Study |
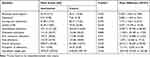 |
Table 3 Baseline Comparisons of the Study Participants in the Intervention and Control Groups in the MEITRA Study |
A sizable number of the study participants (33/66) were middle-aged (40–60 years old) CKD sufferers, about 54 (77.15%) were illiterate or had low educational attainment and 51 (77.27%) were under hemodialysis therapy protocol for at least one year (Table 2).
Primary Outcomes
A significant change in the self-reported depression symptoms and, therefore, overall mean depression score compared to the baseline measures was observed in the intervention group (P=0.001) (mean difference=2.1). Such a change, however, was not detected in the control group (P=0.768). The improvement were also noticeable in mean social support score (P=0.001), nursing care satisfaction score (P=0.001), quality of life score (P=0.001) and interdialytic weight gain (IDWG) (P=0.001) among the participants in the intervention group but no statistically significant change was observed in the mean scores of these output variables in the control group (Table 4).
 |
Table 4 Comparison of the Primary Output Variables Between the Intervention and Control Groups in the MEITRA Study |
The IDWG which was calculated as the weekly average of the difference between predialysis weight and the weight at the end of the previous dialysis session is generally considered as a measure of behavioral compliance due to its clinical relevance, feasibility, accuracy and known predictive validity to envisage the medical outcomes.37
Secondary Outcomes
The mean total scores of the participants in the intervention group in application of the ESRD-AQ indicated a significant (P=0.001) improvement both in one month and three months measurements after the intervention while the change in the control group was not statistically different from the baseline measurements (P=0.193). The highest rise in the ESRD-AQ scores within the intervention group was observed after one month of intervention (mean difference=131.88) compared to the baseline values, however, a meager decline was evident in the mean scores of the ESRD-AQ three months after the intervention among the participants (mean difference=27.27) in the intervention group compared to their first month assessment postintervention. The same pattern of statistically significant changes in mean scores of the intervention group’s attendants in all subscales of the ESRD-AQ were also ascertained as enumerated in Table 5. The observed changes in the total mean scores of ESRD-AQ and its subscales were not statistically meaningful (P>0.19) among the control group’s attendees.
 |
Table 5 Comparison of the End-Stage Renal Disease Adherence (ESRD-A) and its Subscales’ Scores Between the Intervention and Control Groups in the MEITRA Study |
Discussion
Ultimate therapeutic adherence by HDPs could have substantial implications for improving clinical outcomes hence, for their health, quality of life and longevity. The main aim of this study was to assess feasibility and impact of adherence to a multimodal intervention designed to improve therapeutic and lifestyle recommendations in a sample of Iranian HDPs and to inform future mitigation projects that seek to strengthen and enhance therapeutic regimen adherence in HDPs.
The findings of this study revealed that arrangement and implementation of a multifaceted intervention to boost the Iranian HDPs is feasible and conducive. HDPs in developing and underdeveloped countries are generally facing added burden to their illness due to inherent healthcare insufficiencies, financial costs, and inadequacies in social support and services.39 Therefore, any step to fulfill the HDPs’ disease-related needs and expectations in the context of deficient facilities, unfulfilled mental health requirements and poor social support systems might have imperative consequences on the patients’ physical, mental and social wellbeing.
The effectiveness of CBT in reduction of depression symptoms in HDPs was reported in previous studies,36,40-43 which is synchronous with findings of this study. Alleviation of social isolation and improvement of self-esteem, self-care and quality of life through providing social, mental and physical peer support to HDPs by those who have a common health condition was also suggested in earlier studies.38,44 Prearranged telephone-based peer support as a low cost and convenient way of support provision45,46 was appropriately utilized in this research. The family members’ engagement and enrichment of their perception, awareness and self-efficiency in providing the expected support to their family member HDP was another auspicious experience in this research and had been addressed based on the findings of earlier research for embracing health-related advantages.47–49 The health-care providers (HCPs) in the study venue (nursing staff and physicians) were also sensitized and advised to be mindful about the HDPs’ need for emotional support and encouragement in having a better therapeutic adherence profile, congruent with the pinpointed recommendations in the scientific literature to accomplish therapeutic goals and clinical targets.50,51 This is while lack of abovementioned physical, psychological and social support, for instance, family members’ support,52 in the planned health care for the HDPs were suggested to be associated with difficulty with fluid restrictions and coming to dialysis therefore, failing to achieve proposed clinical outcomes.53
As a priori facets of current knowledge which addresses efficacy of multifaceted health-care interventions and the synergy that they could create through combining advantages of the separate individual interventions,54,55 successful implementation of a multimodal patient support mechanism in this study warrants further prospective exploration.
Use of social media to communicate with HCPs and updating them with various elements of nursing and caring skills akin to their professional duties and responsibilities were recommended based on the empirical research evidence,56,57 which was one of the creative components of the multifaceted intervention. This study indicated that use of all these separate useful interventions in one package to have a better therapeutic adherence by HDPs is feasible and efficient. The main advantage of this study was its conduct in a naturalistic setting and the multichannel integration of intervention modalities (compared to the implemented single or limited approach interventions)36,38,41-44 to increase chance of success in change of HDPs therapeutic behaviors and also to provide a baseline evidence for comparison purposes. Extra human resources were not required for successful implementation of the intervention and it can be delivered at scale with minimal human resources and without increasing the costs for health systems. The intervention utilized an existing technology platform and expertise therefore, it can be regarded as a relatively low cost and feasible initiative that can be easily expanded throughout the Iranian National Health System (INHS) and possibly other countries’ health systems.
Limitations
The main advantages of this study were the low cost and multifaceted nature of the proposed interventions and application of scientifically sound clinical indicators to assess the intervention impacts.
Congruent with other interventional research, however, numerous potentially confounding factors existed that might have affected the internal and external validity of this study.
Recruitment of a convenient sample of HDPs in this study is a probable source of confounding bias that could limit external validity of the findings. It is also possible that those patients with high internal motive to change their therapeutic behaviors have consented to participate in the study therefore; the study results are prone to selection bias in a positive direction.
The study inclusion criteria allowed participation of a broad range of HDPs in the study and not necessarily those with a poor therapeutic adherence profile. The probability of the ceiling effect in consequence, must not be completely ruled out in the interpretation of the study findings.
The patients that were randomly allocated into intervention and control groups were admitted in two separate HD wards of the same hospital, therefore contamination bias could have occurred during the study implementation.
The number of applied data collection instruments was also a potential source of bias (response bias) due to its probable effect on reliability of responses as a result of the respondents’ decreased attention or tiredness.
The involved HCPs were aware of the study protocol and its aims ahead of the study initiation. In such circumstances, the awareness might have had an impact on their performance during the study implementation. Their workload must also be considered as another source of bias (intervention bias) with a highly probable effect on their performance during the study conduction.
The intervention’s impacts on clinical outcomes and therapeutic adherence of the patients were studied in the short-term (one month and three months after intervention) therefore, long-term trajectories of the intervention are not recognizable.
Despite all these limitations, it is encouraging that a brief and low-cost multifaceted intervention showed improvement in clinical outputs and therapeutic adherence of the HDPs in a context that is causing extra burden to the ESRD patients due to factors such as economic predicaments, deficient social support, and inadequate health-care facilities.
Conclusions
This interventional study revealed that inaugurating of a feasible low-cost multifaceted intervention without the need to add major logistic or financial inputs into existing health-care systems especially in resource limited contexts is achievable. The implemented multifaceted interventions in this study included planning CBT session for HDPs, involvement of peers with a common health condition and also family members’ engagement to enrich their perception and self-efficiency in providing the expected support, the HCPs sensitizing to be mindful about the HDPs’ need for emotional support and use of social media to communicate with the HCPs to update them with various elements of the required and elemental nursing and caring skills. Such interventions could be more efficacious and enduring than high cost, inflexible and risk-like supercilious programs or single-dimension interventions. Current pressure of surpassing health-care costs of HDPs and their unmet needs warrant application of more pragmatic care provision approaches. Findings of this study could provide insights into scientific basis of evidence-informed interventions applicable in the realm of health-care delivery.
Acknowledgments
This manuscript was prepared based on the findings of a research project that had been conducted for partial fulfilment of the requirements to obtain a PhD degree by the first author. The research was funded partly by the Tabriz University of Medical Sciences and approved by the institutional level Medical Research Ethics Board of Trustees (MREBoT) (approval number: IR.TBZMED.REC.1397.425) and also by the Iranian Registry of Clinical Trials (approval number: IRCT20171213037859N1). The authors would like to thank valuable assistance of the nursing staff and managerial team of the Shahrvand hospital and most importantly the participating patients and their family members without which this research would not have been possible.
Funding
This research was supported partially by Tabriz University of Medical Sciences (grant number: 5-D-193090- 1397-06-10).
Disclosure
The authors claim no conflicts of interest in conducting this review and reporting its findings.
References
1. Kaveh K, Kimmel PL. Compliance in hemodialysis patients: multidimensional measures in search of a gold standard. Am J Kidney Dis. 2001;37(2):244–266. doi:10.4161/org.7.1.13997
2. Fleming GM. Renal replacement therapy review: past, present and future. Organogenesis. 2011;7(1):2–12. doi:10.4161/org.7.1.13997
3. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
4. Cvengros JA, Christensen AJ, Lawton WJ. The role of perceived control and preference for control in adherence to a chronic medical regimen. Ann Behav Med. 2004;27(3):155–161. doi:10.1207/s15324796abm2703_3
5. Chan YM, Zalilah MS, Hii SZ. Determinants of compliance behaviours among patients undergoing hemodialysis in Malaysia. PLoS One. 2012;7(8):e41362. doi:10.1371/journal.pone.0041362
6. Denhaerynck K, Manhaeve D, Dobbels F, et al. Prevalence and consequences of nonadherence to hemodialysis regimens. Am J Crit Care. 2007;16(3):222–235.
7. Rambod M, Peyravi H, Shokrpour N, Sarebanhassanabadi M. Dietary and fluid adherence in Iranian hemodialysis patients. Health Care Manag (Frederick). 2010;29(4):359–364. doi:10.1097/HCM.0b013e3181fa0691
8. Theofilou P. The effect of sociodemographic features and beliefs about medicines on adherence to chronic kidney disease treatment. J Clin Res Bioeth. 2012;3:2. doi:10.4172/2155-9627.1000134
9. Matteson ML, Russell C. Interventions to improve hemodialysis adherence: a systematic review of randomized-controlled trials. Hemodial Int. 2010;14(4):370–382. doi:10.1111/j.1542-4758.2010.00462.x
10. Welch JL, Thomas-Hawkins C. Psycho-educational strategies to promote fluid adherence in adult hemodialysis patients: a review of intervention studies. Int J Nurs Stud. 2005;42(5):597–608. doi:10.1016/j.ijnurstu.2004.09.015
11. White CA. Cognitive behavioral principles in managing chronic disease. West J Med. 2001;175(5):338–342. doi:10.1136/ewjm.175.5.338
12. Howren MB, Kellerman QD, Hillis SL, Cvengros JA. Effect of a behavioral self-regulation intervention on patient adherence to fluid-intake restrictions in hemodialysis: a randomized controlled trial. Ann Behav Med. 2016;50(2):167–176. doi:10.1007/s12160-015-9741-0
13. Idier L, Untas A, Koleck M, Chauveau P, Rasclea N. Assessment and effects of therapeutic patient education for patients in hemodialysis: a systematic review. Int J Nurs Stud. 2011;48(12):1570–1586. doi:10.1016/j.ijnurstu.2011.08.006
14. Cukor D, Cohen SD, Peterson RA, Kimmel PL. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18(12):3042–3055. doi:10.1681/ASN.2007030345
15. McDade-Montez EA, Christensen AJ, Cvengros JA, Lawton WJ. The role of depression symptoms in dialysis withdrawal. Health Psychol. 2006;25(2):198–204. doi:10.1037/0278-6133.25.2.198
16. Taskapan H, Ates F, Kaya B, Emul M. Psychiatric disorders and large interdialytic weight gain in patients on chronic haemodialysis. Nephrology (Carlton). 2005;10(1):15–20. doi:10.1111/j.1440-1797.2005.00321.x
17. Kimmel PL, Cukor D, Cohen SD, Peterson RA. Depression in end-stage renal disease patients: a critical review. Adv Chronic Kidney Dis. 2007;14(4):328–334. doi:10.1053/j.ackd.2007.07.007
18. Karamanidou C, Clatworthy J, Weinman J, Horne R. A systematic review of the prevalence and determinants of nonadherence to phosphate binding medication in patients with end-stage renal disease. BMC Nephrol. 2008;9:2. doi:10.1186/1471-2369-9-2
19. Clarke AL, Young HM, Hull KL, et al. Motivations and barriers to exercise in chronic kidney disease: a qualitative study. Nephrol Dial Transplant. 2015;30(11):1885–1892. doi:10.1093/ndt/gfv208
20. Hughes J, Wood E, Smith G. Exploring kidney patients’ experiences of receiving individual peer support. Health Expect. 2009;12(4):396–406. doi:10.1111/j.1369-7625.2009.00568.x
21. Perry E, Swartz J, Brown S, et al. Peer mentoring: a culturally sensitive approach to end-of-life planning for long-term dialysis patients. Am J Kidney Dis. 2005;46(1):111–119. doi:10.1053/j.ajkd.2005.03.018
22. Zolfaghari M, Sookhak F, Asadi Noughabi A, Haghani H. Effect of cognitive-behavioral intervention on adherence to dietary and fluid-intake restrictions in hemodialysis patients. J Nurs Educ. 2013;2(3):9–17.
23. Dabson KS, Mohammad Khani P. Psychometric characteristics of beck depression inventory–II in patients with major depressive disorder. J Rehabil. 2007;8(SUPPLEMENT(29)):82–88.
24. Dadfar M, Kalibatseva Z. Psychometric properties of the persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica (Cairo). 2016;2016:8196463. doi:10.1155/2016/8196463
25. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Pers Assess. 1988;52(1):30–41. doi:doi.10.1207/s15327752jpa5201_2
26. Bruwer B, Emsley R, Kidd M, Lochner C, Seedat S. Psychometric properties of the multidimensional scale of perceived social support in youth. Compr Psychiatry. 2008;49(2):195–201. doi:10.1016/j.comppsych.2007.09.002
27. Salimi AR, Joukar B, Nikpour R. Internet and communication: perceived social support and loneliness as antecedent variables. Psychol Stud (Mysore). 2009;5(3):81–102.
28. Laschinger HS, Hall LM, Pedersen C, Almost J. A psychometric analysis of the patient satisfaction with nursing care quality questionnaire: an actionable approach to measuring patient satisfaction. J Nurs Care Qual. 2005;20(3):220–230. doi:10.1097/00001786-200507000-00006
29. Negarandeh R, Mohammadi S, Zabolypour S, Arazi Ghojegh T. Relationship between quality of senior nursing students’ caring behaviors and patients’ satisfaction. Hayat. 2012;18(3):10–21.
30. Kim Y, Evangelista LS, Phillips LR, Pavlish C, Kopple JD. The end-stage renal disease adherence questionnaire (ESRD-AQ): testing the psychometric properties in patients receiving in-center hemodialysis. Nephrol Nurs J. 2010;37(4):377–393.
31. Khalili F, Eslami AA, Farajzadegan Z, Hassanzadeh A. The association between social-psychological factors and treatment adherence behaviors among maintenance hemodialysis patients in Isfahan,Iran: a conceptual framework based on social cognitive theory. Health Syst Res. 2011;7(3):278–290.
32. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi:10.1017/S0033291798006667.
33. Karimi Moonaghi H, Hasanzadeh F, Shamsoddini S, Emamimoghadam Z, Ebrahimzadeh S. A comparison of face to face and video-based education on attitude related to diet and fluids: adherence in hemodialysis patients. Iran J Nurs Midwifery Res. 2012;17(5):360–364.
34. Hemmati Maslakpak M, Shams S. A comparison of face to face and video-based self care education on quality of life of hemodialysis patients. Int J Community Based Nurs Midwifery. 2015;3(3):234–243.
35. Baraz S, Mohammadi I, Boroumand B. A comparative study on the effect of two methods of self-care education (direct and indirect) on quality of life and physical problems of hemodialysis patients. AMUJ. 2006;9(1):7–22.
36. Duarte PS, Miyazaki MC, Blay SL, Sesso R. Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int. 2009;76(4):414–421. doi:10.1038/ki.2009.156
37. Cukor D, Ver Halen N, Asher DR, et al. Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol. 2014;25(1):196–206. doi:10.1681/ASN.2012111134
38. Dennis CL. The process of developing and implementing a telephone-based peer support program for postpartum depression: evidence from two randomized controlled trials. Trials. 2014;15:131. doi:10.1186/1745-6215-15-131
39. Wetmore JB, Collins AJ. Meeting the world’s need for maintenance dialysis. J Am Soc Nephrol. 2015;26(11):2601–2603. doi:10.1681/ASN.2015060660
40. Powles WE, Beck AT. Depression: causes and treatment. Am J Clin Hypn. 1974;16(4):281–282. doi:10.1080/00029157.1974.10403697
41. Marvi A, Bayazi MH, Rahmani M, Deloei AK. Studying the effect of cognitive behavioral group training on depression in hemodialysis patients. Procedia Soc Behav Sci. 2011;30:1831–1836. doi:10.1016/j.sbspro.2011.10.353
42. Valsaraj BP, Bhat SM, Latha KS. Cognitive behaviour therapy for anxiety and depression among people undergoing haemodialysis: a randomized control trial. J Clin Diagn Res. 2016;10(8):VC06–VC10. doi:10.7860/JCDR/2016/18959.8383
43. Allart-van Dam E, Hosman CM, Hoogduin CA, Schaap CP. Prevention of depression in subclinically depressed adults: follow-up effects on the ‘coping with depression’ course. J Affect Disord. 2007;97(1–3):219–228. doi:10.1016/j.jad.2006.06.020
44. Thong MS, Kaptein AA, Krediet RT, Boeschoten EW, Dekker FW. Social support predicts survival in dialysis patients. Nephrol Dial Transplant. 2007;22(3):845–850. doi:10.1093/ndt/gfl700
45. Lewis E, Huang HC, Hassmen P, Welvaert M, Pumpa KL. Adding telephone and text support to an obesity management program improves behavioral adherence and clinical outcomes: a randomized controlled crossover trial. Int J Behav Med. 2019;26(6):580–590. doi:10.1007/s12529-019-09815-1
46. Elswick A, Fallin-Bennett A. Voices of hope: a feasibility study of telephone recovery support. Addict Behav. 2020;102:106182. doi:10.1016/j.addbeh.2019.106182
47. Mi T, Li X, Zhou G, Qiao S, Shen Z, Zhou Y. HIV disclosure to family members and medication adherence: role of social support and self-efficacy. AIDS Behav. 2020;24(1):45–54. doi:10.1007/s10461-019-02456-1
48. Damodaran S, Huttlin EA, Lauer E, Rubin E. Mental health trainee facilitation of sibling support groups: understanding its influence on views and skills of family-centered care. Acad Psychiatry. 2019. doi:10.1007/s40596-019-01150-7
49. Lee HW, Park Y, Jang EJ, Lee YJ. Intensive care unit length of stay is reduced by protocolized family support intervention: a systematic review and meta-analysis. Intensive Care Med. 2019;45(8):1072–1081. doi:10.1007/s00134-019-05681-3
50. Jutterstrom L, Hornsten A, Sandstrom H, Stenlund H, Isaksson U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes - a randomized study. Patient Educ Couns. 2016;99(11):1821–1829. doi:10.1016/j.pec.2016.06.016
51. Dunn S, Rossiter L, Ferne J, Barnes E, Wu W. Improved adherence to colposcopy through nurse-led telephone counselling and multifaceted patient support. J Obstet Gynaecol Can. 2013;35(8):723–729. doi:10.1016/S1701-2163(15)30863-X
52. Al Husna CH, Yetti K, Sukmarini L. Determinant of fluid adherence among hemodialysis patients in Malang, Indonesia. Enferm Clin. 2019;29 Suppl 2:117–122. doi:10.1016/j.enfcli.2019.04.018
53. Snyder RL, Jaar BG, Lea JP, Plantinga LC. Association of patient-reported difficulty with adherence with achievement of clinical targets among hemodialysis patients. Patient Prefer Adherence. 2020;14:249–259. doi:10.2147/PPA.S227191
54. Giles M, Graham L, Ball J, King J. Implementation of a multifaceted nurse-led intervention to reduce indwelling urinary catheter use in four Australian hospitals: a pre- and postintervention study. J Clin Nurs. 2019. doi:10.1111/jocn.15142
55. Sorensen L, Idemoto L, Streifel J, et al. A multifaceted intervention to improve the quality of care for patients undergoing total joint arthroplasty. BMJ Open Qual. 2019;8(3):e000664. doi:10.1136/bmjoq-2019-000664
56. Todorovic J, Terzic-Supic Z, Djikanovic B, Nesic DM. Can social media intervention improve physical activity of medical students? Public Health. 2019;
57. Mariano MCO, Maniego JCM, Manila H, et al. Social media use profile, social skills, and nurse-patient interaction among registered nurses in tertiary hospitals: a structural equation model analysis. Int J Nurs Stud. 2018;80:76–82. doi:10.1016/j.ijnurstu.2017.12.014
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
