Back to Journals » Journal of Multidisciplinary Healthcare » Volume 10
Effectiveness of a diabetes mellitus pictorial diary handbook program for middle-aged and elderly type 2 diabetes mellitus patients: a quasi-experimental study at Taladnoi Primary Care Unit, Saraburi, Thailand
Authors Eknithiset R , Samrongthong R
Received 4 April 2017
Accepted for publication 5 July 2017
Published 21 August 2017 Volume 2017:10 Pages 327—334
DOI https://doi.org/10.2147/JMDH.S138815
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Rapat Eknithiset, Ratana Somrongthong
College of Public Health Sciences, Chulalongkorn University, Pathumwan, Bangkok, Thailand
Aim: The research question is “How does a diabetes mellitus (DM) pictorial diary handbook (PDHB) affect the knowledge, practice, and HbA1c among patients with DM type 2?” The aim of this study was to evaluate the effect of a PDHB program among middle-aged and elderly patients with DM type 2 in primary care units in Thailand.
Patients and methods: A quasi-experimental study design was applied. DM type 2 patients were recruited in the PDHB program by a simple random sampling method. The 3-month program consisted of a weekly health education structured for ~20 minutes, a 15-minute group activity training, a 10-minute individual record of participants’ knowledge and practice regarding diet control, exercise, oral hypoglycemic drug taking, diet, self-care, alcohol consumption, smoking, weight management, and HbA1c, and a 15- to 30-minute home visit as well as the PDHB for recording self-care behavior daily. The control group received only the usual diabetes care. The primary expected outcomes were changes in HbA1c from the baseline data to 3 months after the program compared between the intervention and control groups. The secondary expected outcomes were compared within the intervention group. The third expected outcomes were changes in the mean score of knowledge and practice from baseline to 3 months after the program within and between the intervention and control groups.
Results: Compared with the baseline data, there was no significant difference in HbA1c, knowledge, and practice mean score between the intervention and control groups. However, there was a significant difference in HbA1c, knowledge, and practice mean score in the intervention group after they received a 3-month PDHB program and within the intervention group (p-value =0.00).
Conclusion: The PDHB program was effective in lowering HbA1c while also improving the mean score of knowledge and practice among elderly patients with DM type 2. However, larger and longer trial studies will be needed to evaluate the sustainability of this program.
Keywords: diabetes mellitus type 2 patients, diary handbook, glycated hemoglobin, HbA1c, Saraburi, Thailand
Introduction
Diabetes is one of the most common chronic diseases requiring medical care in the Saraburi province of Thailand, ranking seventh in terms of national prevalence, according to statistics provided by the Saraburi Provincial Health Office (2012).1 Several studies on the prevalence of diabetes in Thailand have noted that the prevalence increases with age and reaches a peak at some point after age 55.2–7 The prevalence of diabetes among the residents in Saraburi was 0.4% in 2001 but has increased to 1.1% in 2012.8 Although diabetes was not among the top five most prevalent conditions, the number of patients who suffered from complications of diabetes was quite high in Saraburi province. According to the two medical directors from Taladnoy, Khokyai subdistrict, and Horathep subdistrict health-promoting hospitals, many elderly adults living in the areas are suffering from diabetes. Given rising diabetes rates and the significant burden that diabetes places on individuals and health care systems, the development of effective interventions to reduce the devastating impacts of this disease is critical. Prior research has shown that many aspects of type 2 diabetes can be mitigated using effective interventions.9–11 The findings from prior studies also indicated that the most effective interventions tended to be of longer duration, incorporated multiple written materials and more contact hours,12 and encouraged patient self-regulation.13,14 However, a review of the literature indicates that the majority of diabetes interventions conducted thus far have been quite brief in nature, including, in some cases, only one information session, and most have not provided any opportunities for patient participation or incorporated follow-up activities despite the proven efficacy of booster sessions.12
According to the research on knowledge, attitudes, and practices of diabetes mellitus (DM) type 2 patients in a multidisciplinary program at a DM clinic at Phanom Phrai Hospital in the Phanom Phrai district, Roi Et province, Thailand, a multidisciplinary program including home visits, a diet diary, and follow-up on self-care behaviors could help DM type 2 patients control their HbA1c.15 Culturally appropriate diabetes education interventions are more effective than “usual care” in improving diabetes knowledge and healthy lifestyles in ethnic minority populations.16 The existing program at the primary health care unit does not include any interventions or special programs for DM type 2 with culturally appropriate problem solving for diabetes patients; they treat patients with routine care. Therefore, there is a need to develop diabetes interventions of greater intensity and duration that involve patients more actively in the process in order to improve outcomes.
Diabetes interventions should be grounded in valid theoretical frameworks. Protection motivation theory (PMT), a widely respected and commonly used model, has proven effective for predicting a broad spectrum of health-related behaviors across a wide range of demographic segments.17 According to the PMT, a care taker’s motivation to protect patients from cancer recurrence by taking their medications can be forecast by two main factors within the theory: threat appraisal and coping appraisal. Threat appraisal can be defined as the survivors’ perceptions of the health threat, constitutes the combination of the survivors’ perceived vulnerability and perceived severity.18 Both strategies from PMT were applied to the pictorial diary handbook (PDHB) program. Mobile phone text messaging has been shown to reduce glycated hemoglobin,19 and participants are willing to pay for such programs, including the mobile phone use and the cost of short message service (SMS), for diabetes interventions in Bangladesh.20
The primary research question is “How does a DM PDHB affect the knowledge, practice, and HbA1c among patients with DM type 2?” The DM PDHB has been developed in conjunction with a multidisciplinary team to be locally and culturally appropriate for capturing details of self-care behaviors with which DM type 2 patients struggle most prominently. In addition, the diary is colorful and sized to be accessible for elderly patients. The entire DM PDHB program is described in Table 1. The general objective of this research study was to develop an appropriate21 DM PDHB program for middle-aged and elderly patients with DM type 2 patients at Taladnoi Primary Care Unit, Khokyai Primary Care Unit, and Horathep Primary Care Unit in Saraburi, Thailand. The specific objectives were 1) to compare the mean scores of knowledge, practice, and HbA1c between DM type 2 patients in the intervention group and those in the control group at baseline and month 3 and 2) to compare the mean scores of knowledge, practice, and HbA1c regarding self-care among DM type 2 patients within intervention and control groups at baseline and month 3. The following hypotheses were proposed:
  | Table 1 Schedule of diabetes PDHB program Abbreviation: PDHB, pictorial diary handbook. |
- The mean scores of knowledge, practice, and HbA1c between DM type 2 patients in the intervention group and those in the control group at baseline and month 3 are different.
- The mean scores of knowledge, practice, and HbA1c regarding self-care for DM type 2 patients within the intervention and control groups at baseline and month 3 are different.
In order to achieve the research objectives stated earlier, a model is proposed as depicted in research.21 Subsequently, the results of hypotheses are presented. The paper concludes with a discussion of the results and implications of the research as well as limitations and directions for future research.
Patients and methods
A quasi-experimental study was conducted using an intervention group at Taladnoi Primary Care Unit and a control group at Khokyai Primary Care Unit and Horathep Primary Care Unit, which are located in Banmoh district, Saraburi province, Thailand. This province is a rural area located ~107 km from Bangkok, Thailand’s capital. The sample size of the study was 140 subjects, split equally into the intervention and control groups of 70 subjects each without any attrition. The sample included both male and female patients, aged 50–70 years. All subjects had been diagnosed with DM type 2 patients for >6 months and were undergoing treatment at Taladnoi or Khokyai Primary Care Unit. The research was conducted between October 2016 and January 2017.
Table 1 describes the schedule of the diabetes PDHB program activities from month 1 through month 3 for the intervention group.
Instruments
A five-part questionnaire was utilized to collect sociodemographic data, medical histories, knowledge scores, practice scores, and HbA1c measurements. Data collection was carried out in three stages. The preparation began with the validation of the questionnaire by three medical doctors; a coefficient of ~0.5 was valid at 0.81 by the Items–Objective Congruence Index. Additionally, a preliminary study was also conducted to test the reliability of the questionnaire in order to increase the accuracy and consistency of data acquired in the study. The seven questions regarding knowledge of DM type 2 patients’ self-care behaviors generated decent reliability, with a Kuder–Richardson 20 coefficient of 0.81. Similarly, the Cronbach’s alpha coefficient for the part of the questionnaire measuring practices related to DM type 2 patients’ behavior was 0.95, an adequate level. The biomarker (HbA1c) was defined in the following step. This study included patients aged 50–70 years, both male and female, who had received a diagnosis of DM type 2 at least 6 months prior that required a medical doctor’s treatment. The researcher explained the objective of the research and obtained written consent from the subjects who were recruited under the inclusion criteria and willing to join the research. The subjects completed the questionnaires regarding self-care knowledge and practice at baseline and immediately following the intervention, including providing a baseline and post-intervention HbA1c measurement. Patients’ HbA1c was measured by a private laboratory institute at baseline and after the intervention at the primary health care unit for both the intervention and the control groups. According to the World Health Organization (WHO) guideline, the HbA1c target is set at 7.0; the participants needed to control their blood sugar at a level ≤7.0.
The intervention consisted of a health education session attended by the intervention group every week for 3 months at 45 minutes per session. Additionally, home visits of 15–30 minutes per session were conducted by the researcher once a month for 3 months, which included the researcher reviewing the daily records of the DM type 2 PDHB and analyzing whether the participants should alter their self-care behavior.
The maximum potential score for knowledge of self-care among the patients was 7 points, and the maximum potential score for self-care practice was 18 points. The mean and SD of knowledge of DM type 2 were used to classify the scores as “high”, “moderate”, or “low”. A high level of DM type 2 patient’s knowledge was defined as a score greater than or equal to mean+SD, a moderate level of knowledge was defined as a score between mean±SD, and a low level of knowledge was defined as a score less than or equal to mean–SD. A high level of practice was defined as a score greater than or equal to mean+SD, a moderate level of practice was defined as a score between mean±SD, and a low level was defined as a score less than or equal to mean–SD.
Data analysis
Data analyses were conducted using SPSS statistical package version 16 (SPSS Inc., Chicago, IL, USA). Descriptive statistics, including frequency distribution, percentage, mean, SD, independent t-test, paired t-test, and chi-square test, were used to describe the following demographic characteristics of the subjects: sociodemographic characteristics and knowledge and practice related to diet control, exercise, oral hypoglycemic drug taking, self-care, alcohol consumption, smoking, weight management, and blood sugar control. Using data measuring knowledge, practice, and HbA1c, the paired t-test was used to analyze the differences between baseline and month 3 and an independent t-test was used to analyze the difference between the control and intervention groups. All analyses used a 95% CI, and the level of significance for all the statistical tests was set at p-value <0.05.
Ethical consideration
This study was approved by the Ethics Review Committee for Research Involving Human Research Subjects at Suan Sunandha Rajabhat University (COA No. 1-014/2016). Prior to taking part in the study, the study objectives and data collection processes were fully explained to the subjects, who then signed a written consent form to indicate their willingness to join the study.
Results
Table 2 describes the sociodemographic characteristics of the subjects at the baseline survey in both the intervention and control groups. A total of 74.28% of participants were female, and their mean age was 62.26±6.7 years in the intervention group and 61.97±7.3 years in the control group. In the intervention group, 81.42% were married, compared to 88.57% in the control group. Of the two groups, 78.57% of participants had completed their education at a level lower than grade 6 in the intervention group, while 85.71% of participants in the control group had a sixth grade education. Agriculture was the major occupation in both intervention and control groups, at 37.14% and 38.57%, respectively. All participants of both groups were Buddhist, and 81.42% of participants in the intervention group and 72.85% of participants in the control group were homemakers. Furthermore, the mean household income was 6,277.14±5,191.83 Thai baht and 6,755.71±4,912.47 Thai baht in the intervention and control groups, respectively. The mean household expenses were equal to 5,008.57±4,097.2 Thai baht in the intervention group and 5,315.71±3,955.02 Thai baht in the control group. The mean duration of DM type 2 was 13.77±6.15 years in the intervention group and 13.54±6.03 years in the control group, and the average HbA1c was 7.21±1.23% in the intervention group and 7.24±1.34% in the control group. The mean HbA1c in the control group and intervention group was not statistically significantly different. Likewise, the 70 subjects in the control group and 70 subjects in the intervention group had similar characteristics at baseline. It could be concluded that the subjects in the intervention and control groups had similar characteristics at baseline.
  | Table 2 Sociodemographic characteristics of subjects Notes: Significant at p-value <0.05. aChi-square test. bIndependent t-test. Abbreviations: PDHB, pictorial diary handbook; DM, diabetes mellitus. |
Table 3 describes the clinical outcome variables at the baseline survey among 140 DM type 2 patients. The average HbA1c was 7.21±1.23% in the intervention group and 7.24±1.34% in the control group. The average HbA1c in the control group and intervention group was not statistically significantly different at baseline.
  | Table 3 Baseline clinical outcome variables (N=140) Note: Significant at p-value <0.05, using independent t-test. Abbreviation: PDHB, pictorial diary handbook. |
Table 4 describes knowledge and practice scores regarding diet control, exercise, oral hypoglycemic/drug taking, self-care, alcohol consumption, smoking, weight management, and blood sugar control at baseline. There were no statistically significant differences among the overall scores of knowledge and practice between the intervention and the control groups (p-value =0.96 and p-value =0.93).
  | Table 4 Baseline of knowledge and practice outcome variables (N=140) Note: Significant at p-value <0.05, using independent t-test. Abbreviation: PDHB, pictorial diary handbook. |
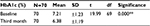
Table 5 describes the change in HbA1c from baseline to month 3 in the intervention and control groups. There was no statistically significant difference between baseline and month 3 among control group (p-value =0.942). However, there was statistically significant difference in HbA1c in the intervention group from baseline to month 3 (p-value <0.001).
Table 6 describes the change in HbA1c% mean from baseline to month 3 within the intervention group. The HbA1c% mean score showed statistically significant differences from baseline to month 3 within the intervention group at p-value =0.00.
Table 7 describes the change in HbA1c from baseline to month 3 within the control group. The HbA1c% had no statistically significant differences from baseline to month 3 within the control group at p-value =0.178.
  | Table 7 Modifications in HbA1c from baseline to month 3 of PDHB within the control group (N=70) Note: Significant at p-value <0.05, using paired t-test. Abbreviation: PDHB, pictorial diary handbook. |
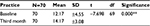
Table 8 describes the change in knowledge from baseline to month 3 within the intervention group. The knowledge mean score showed statistically significant differences from baseline to month 3 in the intervention group at p-value =0.00.
Table 9 describes the change in knowledge from baseline to month 3 within the control group. The knowledge mean score had no statistically significant differences from baseline to month 3 in the intervention group at p-value =1.00.
  | Table 9 Modification in knowledge from baseline to month 3 within the PDHB control group (N=70) Note: Significant at p-value <0.05, using paired t-test. Abbreviation: PDHB, pictorial diary handbook. |
Table 10 describes the change in practice mean score from baseline to month 3 within the intervention group. Practice mean scores exhibited statistically significant differences from baseline to month 3 within the intervention group at p-value =0.00.
Table 11 describes the change in practice mean scores from baseline to month 3 within the control group. Practice mean scores demonstrated no statistically significant differences from baseline to month 3 within the control group at p-value =0.611
  | Table 11 Modification in practice from baseline to month 3 within the PDHB control group (N=70) Note: Significant at p-value <0.05, using paired t-test. Abbreviation: PDHB, pictorial diary handbook. |
The hypothesis that mean scores of knowledge, practice, and HbA1c between DM type 2 patients in the intervention group and the control group at baseline and month 3 are different is accepted. The hypothesis that the mean scores of knowledge, practice, and HbA1c regarding self-care for DM type 2 patients within the intervention and control groups at baseline and month 3 are different is also accepted. Furthermore, during the study, there were not any changes in dosage size and/or type of oral hypoglycemic medications. Patients had appointments with the health care professionals at the primary health care unit every month; or every month to take the medicine home for 1–2 months at a time. Moreover, there were no any hypo- or hyperglycemic events or symptoms among the patients during the study, because the DM type 2 education session was provided every month to influence their self-care behavior.
Discussion
This study focused on the effectiveness of a DM PDHB program on knowledge, practice, and HbA1c mean score in older patients with DM type 2 via a quasi-experimental study at the Taladnoi primary care unit in Saraburi, Thailand. At enrolment, the patients’ demographic details, past and present medical and medication history, family history, diet, and smoking status were obtained in a suitably designed patient profile form. Additionally, HbA1C was recorded at baseline and month 3. The patients in the intervention group participated in a DM PDHB program over a period of 3 months, and the changes in knowledge and practice of diabetic patients regarding self-care behaviors and HbA1c were documented. During the education session, the pharmacist explained issues relevant to diabetes, such as pathophysiology and the cause of diabetes, short- and long-term complications of diabetes, the relevance of the biomarker HbA1c, and recommendations for appropriate lifestyle changes, eg, exercise, smoking cessation, weight management, hypoglycemic drug taking, self-care, alcohol consumption, and nutrition. The majority of the participants were female, had DM type 2, had received a diagnosis of DM type 2 more than 13 years (mean) prior, and had HbA1c mean levels equal to 7.21±1.23% in the intervention group and 7.24±1.34% in the control group. The knowledge and practice mean scores were regarding to diet control, exercise, oral hypoglycemic/other drug taking, self-care, alcohol consumption, smoking, weight management, and HbA1c. There were no statistically significant differences among the overall scores of knowledge and practice between the intervention and the control groups at baseline (p-values=0.96 and 0.93, respectively). There were no statistically significant differences in HbA1c between the intervention and the control groups at baseline (p-value =0.94). After the subjects had participated in this program for 3 months, they achieved many of the desirable dietary and lifestyle changes. DM PDHB program has improved knowledge mean score and practice mean score after three month intervention completed, both of knowledge mean score and practice mean score were significant different at p-value=0.00 accordingly. The study found that the DM PDHB program produced a statistically significant change in HbA1c at a p-value of 0.00 after the 3-month intervention.
These findings are consistent with studies that use a multifactorial intervention on cardiovascular disease to influence the knowledge, practice and HbA1c level in patients with type 2 diabetes. Additionally, “Diabetes Camp” can be used as continuing education for diabetes self-management in middle-aged and elderly people with type 2 DM, and another study has documented the effect of a diabetes counseling program on knowledge, attitudes, and practice among diabetic patients in the Erode District of South India.22–24 This intervention could be applied in other countries in order to improve self-care behaviors among patients with chronic diseases. The increase in the knowledge score in the intervention group after the 3-month intervention is consistent with the study on effects of the First Line Diabetes Care (FiLDCare) self-management education and support project on knowledge, attitudes, perceptions, self-management practices, and glycemic control. This quasi-experimental study conducted in the Northern Philippines explored the effectiveness of individual and group interventions for people with type 2 diabetes, including providing education on self-care behavior that could control their HbA1c.14,25,26 This study showed statistical significance in lowering participants’ HbA1c results accordingly.
Conclusion
The DM PDHB program is effective in increasing knowledge and improving practice mean scores regarding diet control, exercise, oral hypoglycemic/other drug taking, self-care, alcohol consumption, smoking, and weight management as well as lowering mean HbA1c levels. This intervention could be applied for any other chronic diseases in different contexts and in other countries.
Limitations and recommendations
There are several limitations to this study. First, the proposed conceptual model in this study was empirically tested using data collected from people living in the center of Thailand. These results might vary for patients in other regions, as well as in other countries, since each region has their own eating habits and food culture, but the conceptual model could be adapted to any other rural or urban area, in either developed or developing countries. In the interest of generalization, future research should be conducted to test this model in other diabetes type contexts in others countries in the world. Second, this study fell short in examining all the relationships between the affective evaluation constructs, eg, between patients in other age ranges or food cultures and patients eating at home versus dining out. Future research should investigate these relationships in order to better understand the effects of food preferences in a more challenging environment. Finally, a longitudinal study of diabetes patients in Thailand should be conducted to elicit the changing patterns of patients’ medical needs and desires.
Acknowledgments
The authors would like to express their gratitude for the support and help of Associate Professor Dr. Ratana Samrongtong and the health care teams from Taladnoi, Horathep, and Khokyai primary care units in Saraburi, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Saraburi Provincial Office General Information. Secondary General Information 2013. Available from: http://odpc4.ddc.moph.go.th/documents/425661802.46122.docx. | ||
Chaicharn D, Alessandra F. Diabetes management in Thailand: a literature review of the burden, costs, and outcome. Globalization Health. 2013;9(11):1–18. | ||
Aekplakorn W, Chariyalertsak S, Kessomboon P, et al. Prevalence and management of diabetes and metabolic risk factors in Thai adults: the Thai National Health Examination Survey IV, 2009. Diabetes Care. 2011;34(9):1980–1985. | ||
Aekplakorn W, Abbott-Klafter J, Premgamone A, et al. Prevalence and management of diabetes and associated risk factors by regions of Thailand: Third National Health Examination Survey 2004. Diabetes Care. 2007;30(8):2007–2012. | ||
Aekplakorn W, Stolk RP, Neal B, et al. The prevalence and management of diabetes in Thai adults: the international collaborative study of cardiovascular disease in Asia. Diabetes Care. 2003;26(10):2758–2763. | ||
Bhuripanyo K, Ruangratanaamporn O, Mahanonda N, et al. Impaired fasting glucose, diabetes mellitus and coronary risk factors. J Med Assoc Thai. 2000;83(suppl 2):S146–S152. | ||
Alexander CM, Landsman PB, Teutsch SM. Diabetes mellitus, impaired fasting glucose, atherosclerotic risk factors, and prevalence of coronary heart disease. Am J Cardiol. 2000;86(9):897–902. | ||
Bureau of Non Communicable Disease. Diabetes Morbidity rate 2001-2012. Secondary Diabetes Morbidity Rate 2001-2012; 2012. Available from: http://thaincd.com/s/dl-8328/document/file/info/non-communicable-disease/%E0%B8%AA%E0%B8%A3%E0%B8%B8%E0%B8%9B%E0%B8%9C%E0%B8%B9%E0%B9%89%E0%B8%9B%E0%B9%88%E0%B8%A7%E0%B8%A2%E0%B9%80%E0%B8%9A%E0%B8%B2%E0%B8%AB%E0%B8%A7%E0%B8%B2%E0%B8%99%E0%B9%81%E0%B8%A5%E0%B8%B0%E0%B8%84%E0%B8%A7%E0%B8%B2%E0%B8%A1%E0%B8%94%E0%B8%B1%E0%B8%99%E0%B8%97%E0%B8%B5%E0%B9%88%E0%B8%84%E0%B8%A7%E0%B8%9A%E0%B8%84%E0%B8%B8%E0%B8%A1%E0%B9%84%E0%B8%94%E0%B9%89.xlsx | ||
Keeratiyutawong P, Hanucharurnkul S, Melkus GDE, Panpakdee O, Vorapongsathorn T. Effectiveness of a self-management program for Thais with type 2 diabetes. Thai J Nurs Res. 2006;10(2):85–97. | ||
Malathy R, Narmadha MP, Ramesh S, Alvin JM, Dinesh BN. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm. 2011;3(1):65–72. | ||
Megeid FYA, El-Sayed MMA. Health education intervention improves knowledge, attitude and practices of mothers of insulin dependent diabetes mellitus. World Appl Sci J. 2012;17(11):1398–1404. | ||
Fan L, Sidani S. Effectiveness of diabetes self-management education intervention elements: a meta-analysis. Can J Diabetes. 2009;33(1):18–26. | ||
Stadler G, Oettingen G, Gollwitzer PM. Intervention effects of information and self-regulation on eating fruits and vegetables over two years. Health Psychol. 2010;29(3):274–283. | ||
Ebrahimi H, Sadeghi M, Amanpour F, Vahedi H. Evaluation of empowerment model on indicators of metabolic control in patients with type 2 diabetes, a randomized clinical trial study. Prim Care Diabetes. 2016;10(2):129–135. | ||
Eknithiset R, Hongsranagon P, Havanond P. Knowledge, attitude, and practice (KAP) of diabetes mellitus type II patients in multidisciplinary program at diabetes mellitus clinic, Phanomphrai Hospital, Phanomphrai district, Roi-Et province. Thailand J Health Res. 2010;24:87–92. | ||
Pottie K, Hadi A, Chen J, Welch V, Hawthorne K. Realist review to understand the efficacy of culturally appropriate diabetes education programmes. Diabet Med. 2013;30(9):1017–1025. | ||
Gaston A, Prapavessis H. Using a combined protection motivation theory and health action process approach intervention to promote exercise during pregnancy. J Behav Med. 2014;37(2):173–184. [New York: Springer Science+Business Media 2012:1-12]. | ||
Karmakar M, Pinto SL, Jordan TR, Mohamed I, Holiday-Goodman M. Predicting adherence to aromatase inhibitor therapy among breast cancer survivors: an application of the protection motivation theory. Breast Cancer (Auckl). 2017;11:1178223417694520. | ||
Shariful Islam SM, Niessen LW, Ferrari U, Ali L, Seissler J, Lechner A. Effects of mobile phone SMS to improve glycemic control among patients with type 2 diabetes in Bangladesh: a prospective, parallel-group, randomized controlled trial. Diabetes Care. 2015;38(8):e112–e113. | ||
Shariful Islam SM, Lechner A, Ferrari U, Seissler J, Holle R, Niessen LW. Mobile phone use and willingness to pay for SMS for diabetes in Bangladesh. J Public Health. 2015;38(1):163–169. | ||
Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol. 1987;52(3):596. | ||
Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383–393. | ||
So YP, Sun YK, Hye ML, et al. Diabetes camp as continuing education for diabetes self-management in middle-aged and elderly people with type 2 diabetes mellitus. Diabetes Metab J. 2017;1(1):1–14. | ||
Al-Harith K, Mohamed AH, Al-Asru S, Syed Azhar SS, Shameni S. Perception and knowledge of patients with type 2 diabetes in Malaysia about their disease and medication: a qualitative study. Res Soc Adm Pharm. 2011;7(2):180–191. | ||
Ku GM, Kegels G. Effects of the First Line Diabetes Care (FiLDCare) self-management education and support project on knowledge, attitudes, perceptions, self-management practices and glycaemic control: a quasi-experimental study conducted in the Northern Philippines. BMJ Open. 2014;4(8):e005317. | ||
Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educ. 2015;41(4):417–430. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.