Back to Journals » Journal of Pain Research » Volume 16
Effectiveness and Safety of Acupotomy on Lumbar Spinal Stenosis: A Pragmatic, Pilot, Randomized Controlled Trial
Authors Lee JH , Lee HJ, Woo SH, Park YK, Han JH, Choi GY, Heo ES, Kim JS , Park CA, Lee WD, Yang CS , Kim AR , Han CH
Received 3 December 2022
Accepted for publication 14 February 2023
Published 6 March 2023 Volume 2023:16 Pages 659—668
DOI https://doi.org/10.2147/JPR.S399132
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Houman Danesh
Jung Hee Lee,1,* Hyun-Jong Lee,1,* Sang Ha Woo,1 Yu-Kyeong Park,1 Ji Hoon Han,1 Ga-Young Choi,1 Eun Sil Heo,1 Jae Soo Kim,1 Chung A Park,2 Woo Dong Lee,3 Chang Sop Yang,4 Ae-Ran Kim,5 Chang-Hyun Han4,6
1Department of Acupuncture & Moxibustion, College of Korean Medicine, Daegu Haany University, Daegu, Republic of Korea; 2Department of Diagnostics, College of Korean Medicine, Daegu Haany University, Daegu, Republic of Korea; 3Pre-Major of Cosmetics and Pharmaceutics, College of Herbal Bio-Industry, Daegu Haany University, Daegu, Republic of Korea; 4KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea; 5Clinical Research Coordinating Team, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea; 6Korean Convergence Medicine, University of Science & Technology (UST), Campus of Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
*These authors contributed equally to this work
Correspondence: Chang-Hyun Han, KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, 34054, Republic of Korea, Tel +82 42 868 9498, Fax +82 42 869 2775, Email [email protected]
Purpose: In Korea, complex treatments such as acupotomy, acupuncture, and physical therapy are performed for lumbar spinal stenosis (LSS). Although there are reports of acupotomy as monotherapy or acupuncture treatment for LSS, pragmatic studies are lacking. Therefore, this study aimed to determine the effectiveness and safety of acupotomy for LSS to provide baseline evidence for a large-scale study.
Materials and Methods: This pragmatic randomized controlled pilot study enrolled 34 participants and randomly assigned them to two groups (n=17/group). The intervention was conducted for 8 weeks. Acupotomy plus and usual care groups received acupuncture (17 acupoints) and interferential current therapy (ICT) twice weekly; however, the acupotomy plus group received an additional acupotomy (7 acupoints) for treatment of the usual care group. The primary outcome was measured using visual analog scales (VAS), and secondary outcomes were assessed using the self-rated walking distance, short-form McGill Pain Questionnaire (SF-MPQ), and the Oswestry Disability Index (ODI). Outcome measurements were conducted at baseline and 4, 8, and 12 weeks after the commencement of the intervention. Adverse events were assessed at each visit. Hematological and biochemical examinations were performed at screening and week 8.
Results: Overall, 33 of the 34 participants completed the study, and one participant in the usual care group dropped out. In both groups, VAS scores at weeks 4, 8, and 12 significantly improved compared to baseline. Also, self-rated walking distance, SF-MPQ, and ODI scores were significantly improved at weeks 4, 8, and 12 than at baseline. However, there were no significant differences in the time-dependent and group-to-time interactions between the two groups. In addition, no severe adverse reactions were reported, and there were no significant differences in hematological and biochemical results.
Conclusion: This study provides baseline data for large-scale studies on the effectiveness and safety of acupotomy in LSS.
Clinical Trial Number: KCT0006234.
Keywords: complementary therapy, pragmatic clinical trial, low back pain, acupuncture therapy
A Letter to the Editor has been published for this article.
Introduction
Lumbar spinal stenosis (LSS), a degenerative disease that causes neurological symptoms in the lower extremities, is associated with the anatomical reduction of the intervertebral foramen and spinal canal.1,2 The main symptoms of LSS usually include pain other than intermittent neurogenic claudication, loss of sensation, discomfort, and weakness in the legs within the spinal level.3 Accordingly, LSS affects walking and daily activities and reduces the quality of life.2,4 LSS treatment involves both conservative and surgical treatments. Surgical treatment includes decompressive laminectomy and minimally invasive lumbar decompression.5,6 The indications for surgery vary widely, but in adult patients aged >65 years, spinal stenosis is the most common indication for low back surgery.7 However, radiographic findings and clinical symptoms of spinal stenosis may not necessarily correlate, and thus, surgical procedures should be cautiously decided.8 On the other hand, conservative treatments encompass pharmacological management with nonsteroidal anti-inflammatory medications, epidural steroid injections, physical therapy, and regular exercise.5 No conclusive evidence has been reported as regards the superior treatment modality (surgical vs conservative) for LSS.9 With respect to side effects, 10–24% of cases occur under surgical treatment; therefore, patients with LSS are more interested in conservative treatments.
Acupotomy, a traditional form of acupuncture, is a unique Korean medical treatment modality that involves a sharp blade attached to the tip of the needle. The treatment effect is a combination of acupuncture and microsurgery.10 A systematic review11 showed that acupotomy has a significant benefit in LSS treatment. However, in Korean clinical practice, disease treatment mainly involves multiple modalities rather than a single modality. Thus, LSS is treated with a combination of acupotomy, acupuncture, and physical therapy rather than acupotomy or acupuncture alone. Pragmatic studies regarding the effect of combination treatment (acupotomy, acupuncture, physical therapy) for LSS are lacking. Therefore, this pragmatic pilot randomized controlled trials aimed to evaluate the effectiveness and safety of acupotomy in patients with LSS to provide baseline evidence for further large-scale clinical studies.
Materials and Methods
Study Design
This assessor-blinded, pragmatic, pilot, randomized controlled trial was approved by the Institutional Review Board of Daegu Oriental Hospital, Daegu Haany University (DHUMC-D-21001-ANS-01) and registered at CRIS (KCT0006234). The protocol of this study has been previously registered and published.12 The study complied with the Korean Good Clinical Practice guidelines and the Declaration of Helsinki. Participants signed an informed consent form after explaining the intervention process during the trial period. As for the number of participants, 20 people were recruited for each group without determining the sample size. The study was conducted at Daegu Oriental Hospital of Daegu Hanny University from March to October 2022. The procedures were conducted 16 times over 8 week, and participants were followed up for 4 weeks.
Participants
Participants diagnosed with LSS were included, with eligibility for participation determined based on the results of a physical examination, questionnaire, and radiological examination. The inclusion criteria were as follows: (1) age 50–80 years; (2) pain or discomfort in the low back or lower extremity for at least 3 months; (3) diagnosis of LSS on computed tomography or magnetic resonance imaging; (4) Visual Analog Scale (VAS) score of 4–7; (5) no difficulty in language, concentration, and expression; (6) availability for follow-up evaluations during the trial period; and (7) voluntary participation. The exclusion criteria were as follows: (1) history of hypersensitivity reactions or side effects to acupuncture treatment; (2) need for severe surgical treatment for cauda equina syndrome or neurological symptoms of sensory or motor paralysis; (3) spinal surgery before the trial; (4) a lumbar epidural nerve block within 3 months of the trial; (5) neurodegenerative diseases or neuromuscular scoliosis; (6) abnormal liver function, defined as alanine aminotransferase and aspartate aminotransferase levels three times higher than the reference range; (7) abnormal renal function test results (blood urea nitrogen level 7–23 mg/dL, creatinine level 0.6–1.3 mg/dL); (8) or current neurological or psychologically significant disease; (9) pregnant or lactating women and those who have planned pregnancy or refuse appropriate contraceptive options; (10) anticoagulant medication; (11) artificial pacemaker; and (12) deemed inappropriate to participate in the clinical trial by the clinical trial director.
Randomization and Blinding
Randomization involved using a random number that was blocked, randomized, and generated by independent statisticians who were not included in this study and was sealed in an opaque allocation envelope. The allocation sequence of the binary random numbers was generated by the “rbinom” function in the R program with sample size 1 and the probability of success 0.5, until the experimental and control groups were equal in size. These successive trials were stochastically independent. The participants were equally and randomly assigned into the acupotomy plus and usual care groups at the same probability. The outcome assessor did not intervene in the randomization and intervention procedures.
Interventions
The intervention was conducted twice a week for a total of 8 weeks. Both groups (acupotomy plus and usual care) received acupuncture (17 acupoints) and interferential current therapy (ICT) twice weekly, but the acupotomy plus group received an additional acupotomy (7 acupoints) treatment than the usual care group (Table 1).
 |
Table 1 Study Schedule |
Acupotomy
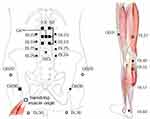
Acupotomy was performed by a Korean medical doctor using a 0.50×50 mm sterile, disposable, and stainless steel acupotomy (DongBang Acupuncture Inc., Gyeonggi-do, Republic of Korea). Acupoints were based on the governor’s vessel at the level corresponding to stenosis on imaging diagnosis, bilateral Hyeopcheok acupoints, and Hyeopcheok acupoints at the adjacent upper and lower levels (7 acupoints). The hip tenderness point around GB30 and the tenderness point of the hamstring muscle origin were additionally treated at the participant’s request (Figure 1). The needle was inserted at a depth of 25–50 mm and was removed immediately after insertion.
Acupuncture
Acupuncture was performed by a Korean medical doctor using 0.30×40 mm, 0.35×60 mm sterile, disposable, stainless steel acupuncture needles (Dong Bang Acupuncture Inc., Boryeong, Republic of Korea). Acupoints were conducted based on GV3 and bilateral BL23, BL24, BL25, BL26, GB30, GB31, BL40, and BL60 (17 acupoints) and further procedures were performed according to the participant’s needs (GB29, BL36, BL37, BL55, BL57) (Figure 1). For GB29 and GB30, 0.35×60 acupuncture was used, and 0.30×40 acupuncture was used for other acupoints.
The acupuncture needle was inserted to a depth of 25–50 mm and maintained for 20±5 min. During the insertion time, an electroacupuncture (ES-160; ItoCo. Ltd., Saitama, Japan) was performed using BL24 and BL26 at a frequency of 3 Hz.
ICT
ICT (GOODPL Inc., Gangwon-do, Republic of Korea) was performed within a range of 4000–4100 Hz by attaching four pads to both sides of the stenosis level. The intensity was maintained at 15±5 min for the participant not to feel pain.
Outcome Measurement
Outcome measures were evaluated at baseline, weeks 4 and 8 (the end of the intervention), and week 12 (4 weeks after the end of the intervention). The primary outcome measure was VAS; meanwhile, the secondary outcome measures were the self-rated walking distance, short-form McGill Pain Questionnaire (SF-MPQ), and Oswestry Disability Index (ODI). The VAS score was measured as follows: the participants indicated a point that represented the intensity of the pain in the past week on a horizontal line (0–10 cm; 0 means no pain, 10 means the worst severe pain), in which the score was determined by measuring the distance from the lowest anchor point to the participant’s mark across the line.13 In this study, the average score of low back pain and lower extremity radiating pain experienced during the last week was assessed as a standard.
Furthermore, the self-rated walking distance was the fourth question in the ODI, and assessors checked the distance the participants could walk without a break. The score ranged from 0 to 5, with higher scores indicating lower walking ability.14 The SF-MPQ consisted of 15 items, including sensory and affective items and the present pain index (PPI). Each item was rated from none (0) to severe (3); the final score was calculated by summing the scores for each item. PPI was used to evaluate current pain intensity from no pain (0) to excruciating (5).15,16 The ODI consisted of ten items: pain intensity, personal care, lifting things, walking, sitting, standing, sleeping, sex life, social life, and travelling.17 Each item was rated from 0 to 5, and the total score was calculated by dividing the sum of each question score by the number of answered questions × 5 and converting it into a percentage. A higher score indicated more functional disorders experienced in daily life due to back pain.
Adverse Events and Safety
Side effects were evaluated during each follow-up visit. Both adverse events related and unrelated to the intervention were recorded. The safety of the intervention was evaluated at baseline and week 8 through hematological and biochemical examinations. These examinations included white blood cell count, red blood cell count, differential count, hematocrit, hemoglobin level, erythrocyte sedimentation rate, platelet count, alanine aminotransferase level, aspartate aminotransferase level, blood urea nitrogen level, creatinine level, C-reactive protein level, prothrombin time, partial thromboplastin time, serum sodium level, serum potassium level, and serum chloride level.
Statistical Analysis
For participants who dropped out, last observation carried forward impute method were used in the analysis. The data were analyzed using intention-to-treat (ITT) analysis. Between-group comparisons of baseline characteristics were performed using Student’s t-test or Mann–Whitney U-test according to the normality of data distribution. The chi-square (χ2) test was utilized to analyze the qualitative data. The VAS, self-rated walking distance, SF-MPQ, and ODI scores were compared between baseline and weeks 4, 8, and 12 in each group using the paired t-test or Wilcoxon signed-rank test based on the normality of data distribution. Repeated-measures analysis of variance was used to identify the difference between groups and the group × time interaction in the VAS, self-rated walking distance, SF-MPQ, and ODI scores. The hematological and biochemical examinations were compared between baseline and weeks 8 using the paired t-test. All statistical analyses were conducted using SPSS (version 19.0, for Windows, IBM, Armonk, NY, USA) and in compliance with the Statistical Guidelines for Clinical Testing (KFDA, 2000). P<0.05 was considered statistically significant.
Results
Participant Enrollment
The screening was conducted on 42 participants. Of these, 34 were registered in the trial, excluding eight who failed to screen (acceptance rate of 80.95%). Among the 34 participants, 33 completed the trial, and one dropped out (dropout rate: 3.03%). The participant belonged to the usual care group; consent to participate was withdrawn because of a traffic accident, and the participant prioritized treatment (Figure 2).
 |
Figure 2 Study flow chart. |
Baseline Characteristics
The baseline participant characteristics are shown in Table 2, and there were no significant between-group differences in sex, age, and outcome measures.
 |
Table 2 Between-Group Comparison of Baseline Participant Characteristics |
Outcome Measurement
In both groups, VAS scores significantly improved at weeks 4, 8, and 12 than those at baseline. Similarly, self-rated walking distance, SF-MPQ, and ODI scores significantly improved at weeks 4, 8, and 12 than that baseline. However, there were no significant differences in VAS, self-rated walking distance, SF-MPQ, and ODI in a time-dependent manner and group-to-time interactions between the two groups (Table 3).
 |
Table 3 Changes in Outcome Measures from Baseline to Week 12 |
Adverse Events and Safety
No intervention-related severe side effects were reported in both groups. All side effects, including shoulder pain, sprained foot pain, sputum, tailbone pain, neck pain, sprained back pain, abdominal pain, systemic pain, sore throat discomfort, and fatigue after COVID-19 Pfizer vaccine, were unrelated to the intervention. Also, there was no significant difference in hematological and biochemical parameters between baseline and week 8 (Table 4).
 |
Table 4 Changes in the Results of Hematological and Biochemical Parameters from Baseline to Week 8 |
Discussion
Acupotomy is widely used in treating musculoskeletal diseases, including spinal diseases, especially in China and Korea; It relieves adhesion of deep tissue, reduces inflammation, and increases the pain threshold, thus reducing pain.18 In addition, owing to the sharp knife at the end of the acupuncture needle, acupotomy combines the effects of acupuncture and microsurgery to improve local blood circulation.19 Acupotomy has been reported to be more effective than other traditional medicine interventions, including acupuncture and manipulation, in LSS.20
Acupuncture is a widely used treatment modality for low back pain or chronic pain, and patients with spinal diseases are inclined to undergo acupuncture as a conservative treatment.21 In spinal stenosis, acupuncture was found to be effective in LSS treatment through biochemical mechanisms to induce analgesia and stimulate peripheral receptors of neurons.22 ICT is a popular treatment that alleviates pain in patients with chronic back pain. According to the gate control theory, stimulation via ICT relieves chronic back pain by interfering with the transmission of nociceptive receptor information from the spinal dorsal horn.23 Oriental medicine clinics attempt to increase the effectiveness of therapeutic modalities by combining treatments such as acupotomy, acupuncture, and ICT; however, pragmatic studies are still lacking. Therefore, this study evaluated the therapeutic effectiveness of acupotomy, which has been a recent research hotspot, compared to that of general treatment using acupuncture and ICT for treating LSS.
The results showed that VAS, self-rated walking distance, SF-MPQ, and ODI scores were significantly improved over time in both acupotomy plus and usual care groups. However, there was no significant difference in effectiveness and safety between the usual care group that received acupuncture and ICT and the acupotomy plus group that received acupotomy in addition to acupuncture and ICT. Middle- and old-age patients with LSS may have thickened ligamentum flavum of the lumbar spine. A study on the effective acupotomy depth for LSS24 showed that the sufficient depth to treat the ligamentum flavum should be approached to an average depth of ≥5 cm. The length of the acupotomy used in this study was 5 cm, indicating that the depth of stimulation around the spine was shallow. Therefore, acupotomy is also considered to be effective by physical stimulation like acupuncture, but it appeared that there was no significant effect of dissecting the thickened tissue. So the effect of acupotomy seemed to be similar to that of acupuncture and there was no synergistic effect with the addition of acupotomy. Recently, studies on ultrasound guide procedures have been reported to increase the accurate depth of the needle and the accuracy of the treatment area.25,26 It is thought that further research is needed on this method. Adverse effects in relation to either acupotomy alone or combination treatment did not occur, and there were no significant differences in hematological and biochemical results. Although no acupotomy-related adverse effects occurred, the possibility of nerve damage or bleeding should always be considered, given the sharp tip of the acupotomy.
This study had some limitations. First, the sample size was small, with the trial involving only 34 participants, and thus, there were limitations in the effectiveness evaluation. Second, as mentioned above, the stimulation depth during acupotomy was shallow, which could explain the insignificant difference in effectiveness between combination treatment with acupuncture and ICT and with the addition of acupotomy. Third, since the results of research on chronic pain can change depending on the patient’s expectations, it is thought that the effect of the expected effect on treatment should be considered in future studies.27 It seems necessary to study the depth of acupuncture in future studies, as previous studies on acupotomy for LSS did not include a detailed description of the procedure. Therefore, it is necessary to establish the strength and depth of effective acupotomy treatment for LSS.
Conclusion
This pilot study can provide baseline evidence for large-scale clinical trials on the effectiveness and safety of including acupotomy in combination treatment comprising acupuncture and ICT for LSS in clinical practice.
Abbreviations
ICT, interferential current therapy; ITT, intention-to-treat; LSS, Lumbar spinal stenosis; ODI, Oswestry Disability Index; PPI, present pain index; SF-MPQ, short-form McGill Pain Questionnaire; VAS, visual analog scales.
Data Sharing Statement
All available data from this trial are presented in the article. We would welcome any third-party scrutiny, and interested parties should contact the corresponding author.
Ethics Approval and Informed Consent
This trial was approved by the Institutional Review Board of Daegu Oriental Hospital, Daegu Haany University (DHUMC-D-21001-ANS-01), and registered at CRIS (KCT0006234). Participants signed an informed consent form after explaining the intervention process during the trial period.
Consent for Publication
All study participants provided consent for publication in this journal.
Acknowledgments
This study was financially supported by grants from the project KSN1823211 of the Korea Institute of Oriental Medicine (KIOM), Republic of Korea.
Author Contributions
All authors made a significant contribution to this work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;2:253–265. doi:10.1016/j.berh.2009.11.001
2. Oka H, Matsudaira K, Takano Y, et al. A comparative study of three conservative treatments in patients with lumbar spinal stenosis: lumbar spinal stenosis with acupuncture and physical therapy study (LAP study). BMC Complement Altern Med. 2018;18:1865–1869. doi:10.1016/0006-2952(75)90405-0
3. Hadianfard MJ, Aminlari A, Daneshian A, et al. Effect of acupuncture on pain and quality of life in patients with lumbar spinal stenosis: a case series study. J Acupunct Meridian Stud. 2016;4:178–182. doi:10.1016/j.jams.2015.11.032
4. Kim KH, Kim YR, Baik SK, et al. Acupuncture for patients with lumbar spinal stenosis: a randomised pilot trial. Acupunc Med. 2016;4:267–274. doi:10.1136/acupmed-2015-010962
5. Lafian AM, Torralba KD. Lumbar spinal stenosis in older adults. Rheum Dis Clin North Am. 2018;3:501–512. doi:10.1016/j.rdc.2018.03.008
6. Deer T, Sayed D, Michels J, et al. A review of lumbar spinal stenosis with intermittent neurogenic claudication: disease and diagnosis. Pain Med. 2019;20(Suppl 2):S32–S44. doi:10.1093/pm/pnz161
7. Kim D, Shin J, Moon Y, et al. Long-term follow-up of spinal stenosis inpatients treated with integrative Korean medicine treatment. J Clin Med. 2020;10:74. doi:10.3390/jcm10010074
8. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;8:794–810. doi:10.1056/NEJMoa0707136
9. Zaina F, Tomkins-Lane C, Carragee E, et al. Surgical versus non‐surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;1:CD010264.
10. Kwon CY, Yoon SH, Chung SY, et al. Clinical efficacy and safety of miniscalpel-needle treatment for tension-type headache: a systematic review and meta-analysis. Chin J Integr Med. 2020;26:713–720. doi:10.1007/s11655-020-3179-3
11. Kwon CY, Yoon SH, Lee BR, et al. Acupotomy for the treatment of lumbar spinal stenosis: a systematic review and meta-analysis. Medicine. 2019;32:e16662.
12. Han JH, Lee HJ, Woo SH, et al. Effectiveness and safety of acupotomy on lumbar spinal stenosis A pragmatic randomized, controlled, pilot clinical trial: a study protocol. Medicine. 2021;100(51):e28175. doi:10.1097/MD.0000000000028175
13. Cline ME, Herman J, Shaw ER, et al. Standardization of the visual analogue scale. Nurs Res. 1992;41:378–380. doi:10.1097/00006199-199211000-00013
14. Tomkins-Lane CC, Battié MC, Macedo LG. Longitudinal construct validity and responsiveness of measures of walking capacity in individuals with lumbar spinal stenosis. Spine J. 2014;9:1936–1943. doi:10.1016/j.spinee.2013.11.030
15. Wright KD, Asmundson GJG, McCreary DR. Factorial validity of the short-form McGill pain questionnaire (SF-MPQ). Eur J Pain. 2001;3:279–284. doi:10.1053/eujp.2001.0243
16. Ferreira SL, Ciampi De Andrade D, Jacobsen Teixeira M. Development and validation of a Brazilian version of the Short-Form McGill Pain Questionnaire (SF-MPQ). Pain Manag Nurs. 2013;14:210–219. doi:10.1016/j.pmn.2011.04.006
17. Fairbank JCT. Why are there different versions of the Oswestry disability index. J Neurosurg Spine. 2014;20:83–86. doi:10.3171/2013.9.SPINE13344
18. Lee ES, Jeong JY, Seo DG, et al. Clinical research of cervical acupotomy effects with acupuncture on facial & trigemial nerve branch on peripheral facial paralysis and postauricular pain. Acupuncture. 2014;31:143–154. doi:10.13045/acupunct.2014061
19. Yoon SH, Kim YS, Kwon MG, et al. Randomized controlled trials of miniscalpel acupuncture for lumbar spinal stenosis cited in the China National Knowledge Infrastructure Database. Acupuncture. 2017;3:59–69. doi:10.13045/acupunct.2017093
20. Kwon C, Yoon S, Lee B. Clinical effectiveness and safety of acupotomy: an overview of systematic reviews. Complement Ther Clin Pract. 2019;36:142–152. doi:10.1016/j.ctcp.2019.07.002
21. Kim KH, Kim TH, Lee BR, et al. Acupuncture for lumbar spinal stenosis: a systematic review and meta-analysis. Complement Ther Med. 2013;21:535–556. doi:10.1016/j.ctim.2013.08.007
22. Clark A, Lucke-Wold BP. Acupuncture and spinal stenosis: considerations for treatment. Future Integr Med. 2022;1:1–8.
23. Lai WY, Cui H, Hu Y. Correlation between change in pain, disability, and surface electromyography topographic parameters after interferential current treatment in patients with chronic low back pain. J Phys Ther Sci. 2021;33:772–778. doi:10.1589/jpts.33.772
24. Zhu X, Qiu Z, Liu Z, et al. CT-guided percutaneous lumbar ligamentum flavum release by needle knife for treatment of lumbar spinal stenosis: a case report and literature review. J Pain Res. 2020;13:2073–2081. doi:10.2147/JPR.S255249
25. Xu H, Zhang Y, Wang C. Ultrasound-guided hydrodilatation of glenohumeral joint combined with acupotomy for treatment of frozen shoulder. J Back Musculoskelet Rehabil. 2022;35(5):1153–1160. doi:10.3233/BMR-210272
26. Lin S, Lai C, Wang J, et al. Efficacy of ultrasound-guided acupotomy for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2023;102(2):e32663. doi:10.1097/MD.0000000000032663
27. Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128(3):264–271. doi:10.1016/j.pain.2006.12.006
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.