Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Effect of the Ramathibodi Rapid Response System Triggered by the Ramathibodi Early Warning Score and Clinical Warning Signs on in-Hospital Mortality and the Incidence of Cardiopulmonary Resuscitation in Adult Hospitalized Patients
Authors Kwantong C, Sutherasan Y , Junhasavasdikul D , Petnak T, Theerawit P
Received 5 July 2023
Accepted for publication 21 November 2023
Published 5 December 2023 Volume 2023:19 Pages 1025—1038
DOI https://doi.org/10.2147/TCRM.S426061
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Chutipong Kwantong,1 Yuda Sutherasan,2 Detajin Junhasavasdikul,2 Tananchai Petnak,2 Pongdhep Theerawit3
1Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Division of Pulmonary and Pulmonary Critical Care Medicine, Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 3Division of Critical Care Medicine, Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Yuda Sutherasan, Division of Pulmonary and Pulmonary Critical Care Medicine, Department of Medicine, Faculty of Medicine Ramathibodi Hospital, 270 Rama VI Road, Ratchathewi, Bangkok, 10400, Thailand, Tel +6622011619, Fax +6622011629 Ext 2, Email [email protected]
Purpose: The Ramathibodi Rapid Response System (RRRS), implemented in March 2017, aims to identify and respond to patients with deteriorating conditions outside the ICU. It employs the Ramathibodi early warning score and clinical signs to monitor all admitted patients, providing expert physician monitoring and early treatment for stabilization and appropriate care triage. This study assesses the RRRS’s effectiveness in reducing in-hospital mortality and CPR events outside the ICU.
Patients and Methods: We conducted a retrospective observational study from March 2014 to February 2020 in a tertiary care hospital’s general wards. We included adult patients experiencing unplanned ICU admission, sudden cardiac arrest, or unexpected death. The study compared in-hospital mortality and CPR incidence outside the ICU between pre- and post-RRRS implementation groups. The associations between RRRS implementation and in-hospital mortality and the incidence of CPR outside the ICU were assessed using multiple logistic regression analyses.
Results: We evaluated 17,741 admissions, with 9168 before RRRS implementation (1 March 2014 to 28 February 2017) and 8573 after RRRS implementation (1 March 2017 to 29 February 2020). The implementation of RRRS was associated with a significant reduction in in-hospital mortality, which decreased from 30.0% to 20.8% (odds ratio, 0.62; 95% confidence interval [CI], 0.57 to 0.66; P< 0.0001). Even after adjusting for age, sex, and comorbidities, the reduction in in-hospital mortality remained significant (adjusted odds ratio, 0.58; 95% CI, 0.54 to 0.63; P< 0.0001). The incidence of CPR outside the ICU also decreased from 1.8% to 1.1% (adjusted odds ratio, 0.6; 95% CI, 0.46 to 0.77; P< 0.0001). Additionally, the rate of ICU transfer increased from 85.4% to 92.1% (risk difference, 6.7; 95% CI, 7.6 to 5.8; P< 0.0001) after implementing the RRRS.
Conclusion: Implementing the RRRS is associated with a reduction in in-hospital mortality and the incidence of CPR outside the ICU.
Keywords: rapid response system, rapid response team, deteriorating patient, in-hospital mortality, cardiopulmonary resuscitation, intensive care unit, implementation protocol
Introduction
The rapid response system (RRS) was first described in the 1990s as a strategy to detect and respond to deteriorating patients outside the intensive care unit (ICU).1 In the general ward, patients may deteriorate to the point of unplanned ICU admission, sudden cardiac arrest, or unexpected death. Half of the serious adverse events are thought to be preventable.2 Conceptually, the RRS is a safety system involving early warning signs for monitoring deterioration. The rapid response team (RRT) prescribes interventions to relieve the trajectory of deterioration and decides to transfer the patients to ICU as early as possible. Early warning signs and characteristics of the RRT may vary in each healthcare center. Many studies of RRSs have shown benefits in decreased hospital cardiac arrest and mortality rates.3–7
Ramathibodi is a hospital capable of super tertiary care and a medical school campus, and it has at least 5000 outpatient visits each day and 1300 beds for tertiary medical care. Several months before protocol implementation, various assessment scores, such as the national early warning score, Modified Early Warning Score, and systemic inflammatory response syndrome criteria, were applied as early warning signs in the general ward of different departments in Ramathibodi Hospital. The lack of uniform evaluation tools and response systems led to different responses of healthcare workers to the patient’s deterioration that could alter the patient’s outcome. Moreover, patients’ morbidities also depend on each physician’s clinical judgment, which may vary depending on clinical skills. Therefore, the Ramathibodi rapid response systems (RRRS) was created and applied in March 2017 as the standard protocol. This system comprises the Ramathibodi Early Warning Score (REWS) and Ramathibodi Clinical Warning Signs (RCWS) as tools to monitor all admitted patients.
We performed a retrospective, observational study to assess the efficacy of the RRRS regarding in-hospital mortality, sudden cardiac arrest outside the ICU, and the rate of ICU transfers in the general ward of Ramathibodi Hospital. The rapid response team and protocol used standard management for all deteriorating patients.
Materials and Methods
Study Population
The research ethics board committee of Ramathibodi Hospital reviewed and approved this study (COA. MURA2020/1358). Due to the retrospective and qualitative nature of the study, the ethics committee has waived the requirement of the informed-consent process. The research involves no more than minimal risk to the subjects. In addition, we confirmed that the data was anonymized and maintained with confidentiality and compliance with the Declaration of Helsinki.
A retrospective observational study was conducted on adult patients aged older than 15 years. The patients who developed acute deterioration, namely sudden cardiac arrest outside the ICU (except in the Emergency Department), unplanned ICU admission, or unexpected death while admitted to the general ward from March 2014 to February 2020 at Ramathibodi Hospital, Bangkok, Thailand, were included in this study. Patients who required palliative care or changed to a treatment plan to palliative care when admitted were excluded from this study.
Outcomes
The primary outcome measured the effectiveness of the implementation of RRRS on in-hospital mortality. The secondary objectives included assessing the impact of the RRRS on the incidence of cardiopulmonary resuscitation (CPR) outside the Intensive Care Unit (ICU) and the rate of patient transfers to the ICU. The study involved a comparative analysis of in-hospital mortality, CPR incidents occurring outside the ICU, and the ICU transfer rate between groups before and after the implementation of the RRRS.
Definitions
In-hospital mortality was defined as the rate of all adult patients who died while they were in the hospital, except for those who were recognized as having palliative care.
The incidence of CPR outside the ICU was defined as the rate of all adult patients who had sudden cardiac arrest resulting in the activation of CPR outside the ICU or the semi-ICU. The CPR rate within the ICU was not included because ICU teams handled cardiopulmonary arrests without activating the code system. Out-of-hospital or CPR within the Emergency Department was excluded.
The ICU transfer rate was defined as the rate of all adult patients who were transferred from the general ward to the ICU or semi-ICU ward because of any deteriorating conditions. Patients who were transferred for an interventional procedure or postoperative monitoring were excluded.
RRRS
On admission, vital signs, oxygen saturation, and the level of consciousness were used to calculate the REWS (Table 1). Regarding the REWs, we reached a consensus among the members of the committee from different departments of the hospital that we modified the early warning score from the previous publication, the standardized early warning(SEW) score, and used the different cut points from previous publication to define the scores of some parameters, ie, RR and HR (Table 1).8 Peterson et al8 reported a significant linear relationship between in-hospital mortality and the admission SEW score. Mortality increased by more than eight times for a score of ≥4 compared to 0–3. Then, we used the cut-off value of 4 to define moderate-risk patients (Table 2). In high-risk patients, we used the cut-off value of 6 or any parameter score equal to 3 to increase the sensitivity of detection of patient deterioration.The patients were classified according to the REWS as being at no risk (score: 0), low risk (score: 1–3), moderate risk (score: 4–5), or high risk (score: ≥6 or a score of 3 for at least one parameter). If the patients are classified as low risk, moderate risk and high risk, the nurses increased the frequency of REWS monitoring as shown in Table 2.
 |
Table 1 The Ramathibodi Early Warning Score(REWS) |
 |
Table 2 The Classification of Patients According to the REWS and Clinical Response |
When the patient’s condition became critical and life-threatening, the REWS or common and specific RCWS were used to detect an event and trigger a systematic response. The Common Ramathibodi Clinical Warning Signs (RCWS) were shown in Table 3 which were modified form The ABCDE (Primary Survey) approach where the acronym “ABCDEF” represents airway, breathing, circulation, disability, exposure and family-centered. The response provided closed monitoring and early treatment by expert physicians to rapidly stabilize and triage the patient to a location where services met the patient’s needs (Table 2 and Table 3). The specific RCWS are clinical syndromes proposed in particular wards. The head nurse in specific wards provided a regular training course for healthcare workers for early detection of these syndromes. The nurses also provided specific assessments and management for these syndromes, such as triggering the sepsis protocol in suspected sepsis patients, evaluating probabilities for deep vein thrombosis, vital signs, and hemoglobin checking in suspected upper gastrointestinal bleeding, early notifying the physician when the patients met criteria of pregnancy-induced hypertension and checking fetal surveillance. Furthermore, fast track systems of specific diseases were activated by this system depending on the particular clinical warning signs (ie, stroke fast track, myocardial infarction fast track, and sepsis fast track).
 |
Table 3 Common Ramathibodi Clinical Warning Signs (RCWS) |
Data Collection and Outcome Measurements
The patients’ data were collected from the hospital database by searching the International Classification of Disease (ICD)-9 and ICD 10. The patients’ data, such as cardiopulmonary resuscitation, mortality, and transfer rate to the ICU, were extracted using a business intelligence tool (Supplementary File 1). The patients’ characteristics, such as age, sex, ward admission, comorbidities, principal diagnosis, principal procedure, and length of hospital stay, were collected.
Electronic medical records and CPR record forms were reviewed for all patients with a CPR code to classify the sites of CPR, namely CPR in the Emergency Department, ICU, or general ward.
Statistical Analyses
Continuous variable data are presented as the mean and standard deviation (SD) for data with a normal distribution or the median with interquartile range for data without a normal distribution. These data were compared between RRRS groups using Student’s t-test and the Mann–Whitney U-test. Categorical variable data are shown as frequencies and percentages and were compared between groups by the chi-square test or Fisher’s exact test as appropriate. We examined the sensitivity and specificity of REWS for predicting the rate of ICU transfer from the cohort of pre-protocol period. Logistic regression analysis was employed to demonstrate the probability of unplanned ICU admission and in-hospital mortality associated with the total REWS at admission. Univariate and multivariable logistic regression analyses were used to evaluate the correlation between implementing the RRRS and the in-hospital mortality and CPR rates. In the univariate analysis, age, sex, and factors with P<0.10 were included in the multivariable analysis. P values <0.05 were considered significant. Statistical analyses were performed with Stata statistical software, version 15 (Stata Corp, LLC, College Station, TX, USA).
Results
During the study period, 18,415 events (ie, acute deterioration, sudden cardiac arrest outside the ICU [except in the Emergency Department], unplanned ICU admission, or unexpected death while admitted to the general ward), were assessed for eligibility. We excluded 402 patients from the analysis because they received palliative care. Finally, 17,741 events were evaluated, with 9168 events in the pre-RRRS implementation period and 8573 events in the post-RRRS implementation period (Figure 1). The numbers of primary and secondary outcomes are shown in a Venn diagram in Figure 2.
 |
Figure 1 Study population. |
 |
Figure 2 Venn diagram of study outcomes shows the classification of the study population as the proportion of primary and secondary outcomes. |
Baseline Patients’ Characteristics
Table 4 shows the clinical and demographic characteristics of the patients included in the study. The mean age of the patients in both groups was 63±17 years. Significant differences in comorbidities, such as cardiac disease, acute respiratory failure, infection, chronic kidney disease, solid malignancy, diabetes, and hypertension, were observed between the two groups. However, the percentage of these comorbidities slightly varied in each group.
The data of the total REWS at admission available in 1144 medical patients who hospitalized during the pre-protocol period. We analyzed the performance of the total REWS at admission among those patients. Of 1144 cases, 55 patients (4.8%) were transferred to ICU, and only three underwent CPR outside the ICU during admission. Forty patients (3.49%) had a total REWS between 4–5, while nine patients (0.79%) had a total REWS score of ≥6 at admission. Our findings indicate that a total REWS ≥3 and/or any parameter score equal to 3 yielded a sensitivity and specificity of 40.0% and 91.8%, respectively, for predicting unplanned ICU admission. In the logistic regression analysis, the total REWS at admission is correlated with an increased rate of ICU transfer and in-hospital mortality (odds ratio 1.83; 95% confidence interval [CI] 1.56–2.14 and odds ratio 1.67; 95% CI 1.36–2.04, respectively). The likelihood of ICU transfer and in-hospital death escalated with the increasing total REWS at admission (Supplementary Figures 1 and 2).
The Impact of the RRRS on in-Hospital Mortality, the Incidence of CPR Outside the ICU and, the Rate of ICU Transfer
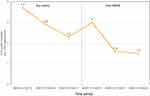
During the study period, in-hospital mortality in deteriorating patients significantly decreased from 30.0% (n=2748) before implementing the RRRS to 20.8% (n=1787) after implementing the RRRS (odds ratio, 0.62; 95% CI, 0.57 to 0.66; P<0.0001) (Table 5). In the multivariate analysis, the reduction in in-hospital mortality remained significant after adjusting for age, sex, and comorbidities (adjusted odds ratio, 0.58; 95% CI, 0.54 to 0.63; P<0.0001) (Table 6). In-hospital deaths per 1000 admissions tended to be decreased after RRRS implementation compared with those before RRRS implementation (Figure 3).
 |
Table 5 Patient’s Outcomes in Pre-RRRS Implementation and Post-RRRS Implementation Group |
 |
Table 6 The Impact of RRRS Implementation on in-Hospital Mortality (Logistic Regression Analysis) |
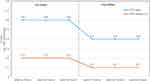
Table 7 shows the effect of RRRS implementation on the incidence of CPR outside the ICU by logistic regression analysis. The incidence of CPR outside the ICU significantly decreased from 1.8% (167 events) before RRRS implementation to 1.1% (96 events) after RRRS implementation (odds ratio, 0.61; 95% CI, 0.47 to 0.79; P<0.0001). This incidence remained significant after adjusting for age, sex, and comorbidities (adjusted odds ratio, 0.6; 95% CI, 0.46 to 0.77; P<0.0001). The events of CPR outside the ICU per 1000 admissions decreased from 0.2 before RRRS implementation to 0.1 after RRRS implementation (Figure 4).
 |
Table 7 The Impact of RRRS Implementation on the Incidence of CPR Outside ICU (Logistic Regression Analysis) |
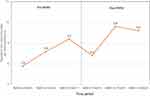
The rate of in-hospital mortality and the incidence of CPR outside the ICU were decreased after RRRS implementation compared with before RRRS implementation. Additionally, the rate of transfer from the ward to the ICU or semi-ICU increased from 85.4% (7832 events) before RRRS implementation to 92.1% (7897 events) after RRRS implementation (Table 5). The trend of ICU/semi-ICU transfer is shown in Figure 5.
Discussion
In this study, the RRRS triggered by the REWS and RCWS resulted in a lower death rate and incidence of cardiac arrest outside the ICU. The reduction in in-hospital mortality and incidence of cardiac arrest outside the ICU remained significant after adjusting for age, sex, and comorbidities between the pre- and post-implementation RRRS in the multivariable analysis. Our results are consistent with a previous, randomized, well-designed study on the effects of the RRS on the outcome of in-hospital patients.9 The authors of this previous study conducted a stepped wedge design that included 7450 patients. The RRS and critical care outreach service implementation resulted in lower in-hospital mortality, with an odds ratio of 0.52 (95% CI, 0.32 to 0.85).
Many studies of rapid response systems have shown benefits of decreased hospital cardiac arrest and mortality rates.3–7 However, the MERIT trial, which randomized 23 Australian hospitals to implement RRS or use usual care did not show an improvement in the composite endpoint consisting of an unexpected death, unplanned ICU admission, or cardiac arrest after RRS implementation.10 In contrast to our study, the MERIT trial conducted a 6-month study period for implementing RRS that may have been too short for optimal functioning of the protocol.
In 2015, we performed a pilot study regarding implementing the rapid response system in the internal medicine ward. We reported that in patients at moderate risk, in-hospital mortality and ICU transfer percentage were lower in the protocol group than in the pre-protocol group.11 Then we started to organize setting the protocol and plan to implement the protocol in the whole hospital.
Before RRRS implementation, the Ramathibodi rapid response committee expected that REWS and RCWS monitoring tools would detect deteriorating patients at an early stage. Nevertheless, the low sensitivity of the early warning score had been criticized previously,12,13 as observed in our study that a total REWS ≥3 and/or any parameter score equal to 3 yielded a sensitivity and specificity of 40.0% and 91.8%, respectively, for predicting unplanned ICU admission. However, in our study, we were concerned about the low sensitivity of early warning score; therefore, we added the clinical warning signs in our quality improvement program to increase the sensitivity for recognition and management in specific urgent conditions.
Concerning the likelihood of ICU transfer and in-hospital mortality derived from the logistic regression equation, there is a sharp increase in the likelihood of both ICU transfer and in-hospital death when the total REWS increases from 2 to 3 (Supplementary Figures 1 and 2). This observation suggests that the dynamic changes in the total REWS might be beneficial, warranting further investigation into this issue.
The rapid response teams would then be activated and the patients would be managed early, including intervention and ICU/semi-ICU transfer following the ABCDEF model in the RCWS. An effective RRRS may increase the rate of ICU transfer by earlier detection and providing early treatment, as well as by ICU transfer of deteriorating patients. The outcome of ICU/semi-ICU admission rates increased after RRRS implementation in our study. This result also supports our findings of lower in-hospital mortality and cardiac arrest rates outside the ICU with improved clinical outcomes. Furthermore, these findings suggest that healthcare workers had good compliance with the RRRS protocol. However, this positive outcome may interfere with confounders, such as new treatment guidelines, medication, intervention, or another medical technology that may be applied in clinical practice over time.
Our findings suggest that implementation of the RRRS with the REWS and RCWS for early identification and RRT for rapid management was practical and effective for patients at risk for deterioration in the general ward.
Limitations
There are some limitations to our study. First, this was a retrospective, observational study that compared pre- and post-RRRS implementation groups. Therefore, the baseline characteristics and the severity of patients’ comorbidities may not be comparable. An incomplete or uncorrected ICD-10 could have affected the study outcomes. The multicenter randomized controlled trial regarding the implementation of RRRS warrants validation of our results. Second, we only included patients who developed acute deterioration, namely sudden cardiac arrest outside the ICU, unplanned ICU admission, or unexpected death while admitted to the general ward. Consequently, not all admitted patients were included in the univariate and multivariate analyses owing to the difficulty of acquiring large datasets.
Third, adherence to the protocol and patient severity parameters at entry were not assessed. Finally, our center has a shortage of ICU beds. Therefore, the ICU transfer rate may have been underestimated.
Conclusions
The implementation of the RRRS is associated with a significant reduction in in-hospital mortality and the incidence of CPR outside the ICU in deteriorating adult patients. This study highlights the importance of using early warning systems to monitor and respond to deteriorating patients outside the ICU. Our findings underscore the need for validation through a multicenter randomized controlled trial on RRRS implementation.
Abbreviations
RRS, rapid response system; RRRS, Ramathibodi rapid response system; ICU, intensive care unit; CPR, cardiopulmonary resuscitation; CI, confidence interval; RRT, rapid response team; REWS, Ramathibodi Early Warning Score; RCWS, Ramathibodi Clinical Warning Signs; ICD, International Classification of Disease; SD, standard deviation.
Data Sharing Statement
The dataset used and analyzed during the current study is available from the corresponding author upon reasonable request.
Ethics Approval
The research ethics board committee of Ramathibodi Hospital reviewed and approved this study (COA. MURA2020/1358). Due to the retrospective and qualitative nature of the study, the ethics committee has waived the requirement of the informed-consent process. The research involves no more than minimal risk to the subjects. In addition, we confirmed that the data was anonymized and maintained with confidentiality and compliance with the Declaration of Helsinki.
Acknowledgments
We would like to acknowledge the invaluable help and contributions of the Ramathibodi rapid response system committee (Supplementary File 2). We thank Ellen Knapp, PhD, from Edanz for editing a draft of this manuscript.
This article’s abstract with interim findings was presented at the 35th ESICM Annual Congress, October 22–26, 2022, as a poster presentation.
Author Contributions
All authors contributed significantly to the work reported, including the conception, study design, execution, acquisition of data, analysis, and interpretation. All authors have drafted, written, substantially revised, or critically reviewed the article. All authors have agreed on the journal to which the article will be submitted. All authors reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors agree to take responsibility and be accountable for the contents of the article.
Funding
The authors did not receive any funding for this work.
Disclosure
All authors declare that they have no financial or personal relationships that could inappropriately influence or bias the content of this article.
References
1. Daffurn K, Lee A, Hillman KM, Bishop GF, Bauman A. Do nurses know when to summon emergency assistance? Intensive Crit Care Nurs. 1994;10(2):115–120.
2. Neale G, Woloshynowych M, Vincent C. Exploring the causes of adverse events in NHS hospital practice. J R Soc Med. 2001;94(7):322–330. doi:10.1177/014107680109400702
3. Ludikhuize J, Brunsveld-Reinders AH, Dijkgraaf MG, et al. Outcomes associated with the nationwide introduction of rapid response systems in the Netherlands. Crit Care Med. 2015;43(12):2544–2551. doi:10.1097/CCM.0000000000001272
4. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19(1):254. doi:10.1186/s13054-015-0973-y
5. Beitler JR, Link N, Bails DB, Hurdle K, Chong DH. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Crit Care. 2011;15(6):R269. doi:10.1186/cc10547
6. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18–26. doi:10.1001/archinternmed.2009.424
7. Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: a systematic review and meta-analysis. J Hosp Med. 2016;11(6):438–445. doi:10.1002/jhm.2554
8. Paterson R, MacLeod DC, Thetford D, et al. Prediction of in-hospital mortality and length of stay using an early warning scoring system: clinical audit. Clin Med. 2006;6(3):281–284. doi:10.7861/clinmedicine.6-3-281
9. Priestley G, Watson W, Rashidian A, et al. Introducing Critical Care Outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med. 2004;30(7):1398–1404. doi:10.1007/s00134-004-2268-7
10. Hillman K, Chen J, Cretikos M, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091–2097.
11. Sutherasan Y, Theerawit P, Suporn A, Nongnuch A, Phanachet P, Kositchaiwat C. The impact of introducing the early warning scoring system and protocol on clinical outcomes in tertiary referral university hospital. Ther Clin Risk Manag. 2018;14:2089–2095. doi:10.2147/TCRM.S175092
12. Downey C, Tahir W, Randell R, Brown J, D J. Strengths and limitations of early warning scores: a systematic review and narrative synthesis. Int J Nurs Stud. 2017;76:106–119. doi:10.1016/j.ijnurstu.2017.09.003
13. Cuthbertson BH, Smith G. A Warning on Early-Warning Scores! Oxford University Press; 2007:704–706.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.