Back to Journals » Risk Management and Healthcare Policy » Volume 17
Effect of Regular Aerobic Exercise on Cognitive Function, Depression Level and Regulative Role of Neurotrophic Factor: A Prospective Cohort Study in the Young and the Middle-Aged Sample
Authors Kong L, Miu L, Yao W, Shi Z
Received 26 December 2023
Accepted for publication 22 March 2024
Published 12 April 2024 Volume 2024:17 Pages 935—943
DOI https://doi.org/10.2147/RMHP.S456765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Lingming Kong,1,* Liqin Miu,2,* Wenwei Yao,2 Zhiyuan Shi3
1Mental Health Research Center, No. 904th Hospital, Changzhou, Jiangsu, 213003, People’s Republic of China; 2Psychiatry Department, the 2nd People’s Hospital of Jintan District, Changzhou, Jiangsu, 213200, People’s Republic of China; 3College of Clinical Medicine, Yangzhou University, Yangzhou, Jiangsu, 225009, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lingming Kong, Mental Health Research Center, North Peace Road 55, No. 904th Hospital, Changzhou, Jiangsu, 213003, People’s Republic of China, Email [email protected]
Purpose: Mild cognitive impairment (MCI) and depressive disorder (DD), which are associated with unhealthy lifestyles, are prevalent worldwide. This study aimed to investigate the effects of regular aerobic exercise on cognitive function, depression, and the regulatory role of neurotrophic growth factors for providing scientific basis in preventing MCI and DD in healthy individuals.
Patients and Methods: Eighty members of the fitness center and 80 community residents were recruited, who were administered by the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) and the Patient Health Questionnaire (PHQ-9). Brain-derived neurotrophic factor (BDNF) and glial cell-line-derived neurotrophic factor (GDNF) in the peripheral blood were detected by enzyme-linked immunosorbent assay (ELISA).
Results: The RBANS and other factor scores, except for visuospatial abilities, were higher and PHQ-9 scores were lower in the study group than in the control group. The concentrations of BDNF and GDNF in the study group were higher than those in the control group. RBANS and its factor scores positively and PHQ-9 negatively correlated with BDNF and GDNF levels. Finally, multiple regression analysis showed that BDNF, as a predictor of RBANS, could explain 59.90% of its variance and that GDNF was a predictor of PHQ-9 could explain 12.30% of the variance.
Conclusion: Regular aerobic exercise can improve cognitive function and depressive symptoms by increasing the BDNF and GDNF levels.
Keywords: cognitive impairment, depression level, brain derived neurotrophic factor, glial cell line-derived neurotrophic factor, aerobic exercise
Introduction
As the proposal of the “bio-psycho-social” medical model and its application in clinical practice, public concern about the role of lifestyle and behavioral habits in disease prevention, treatment, rehabilitation, and health maintenance has greatly increased. As deputy of Chinese Society Behavioral Medicine, Yang put forward the theory of ”behavior determines health”, which was promoted in the Chinese community, countryside, and school for many years.1 Zeng found that smoking is a high-risk factor for mild cognitive impairment (MCI) in the 65–69 year age group. Another study reported that the prevalence of MCI among the elderly in Nanchang was 16.95% and older age, marital status of unmarried, divorced or widowed, low educational level, and low income were risk factors for MCI.2,3 In recent years, the incidence of MCI, which is often considered as a risk factor for Alzheimer’s disease, shows an increasing trend in the younger age group, it has proved that MCI is strongly associated with high blood pressure, oxidized cholesterol and lipid levels.4–6 Dietary structure may be a predictor of cognitive impairment, an epidemiological study found that the incidence of cognitive impairment in people aged 40 and above in the Zhejiang Province of China was 14.2% and the moderate and severe overconsumption of cereals (particularly rice and its products) and eggs and lower intake of soybean and its products were risk factors for cognitive impairment.7 Unhealthy lifestyles, especially high-intake of ‘junk food’ characterized by a high percentage of saturated fats as well as a high proportion of simple ‘refined’ carbohydrates and sugars, is increasingly prevalent globally and are documented as a leading global risk to mental health, a large number of evidences show that junk food usually links with neurodegenerative conditions, such as Alzheimer’s disease and other forms of cognitive decline, it is argued that junk food-induced cognitive decline may be related to impaired central insulin modulation in the hippocampus, which is critical for memory processing. More specifically, high intake of junk food also associates intergenerationally with ill health, maternal and paternal diet which impacts brain development and neural behaviors of their offspring may potentially predispose children to attention deficit hyperactivity disorder and academic failure.8–11 Poor sleep quality and sleep deprivation may also correlate with cognitive impairment. It was found that intestinal flora disorder and systemic inflammatory response accompanied by significant cognitive dysfunction in domains of attention and memory could be observed in healthy adults after 40 h of sleep deprivation. Transplantation of the ”sleep-deprivation microbiota” into germ-free (GF) mice could activate the Toll-like receptor 4/nuclear factor-κB signaling pathway and impaired cognitive function in the GF mice. Mice that harbored ”sleep-deprivation microbiota” also exhibited ascending neuroinflammation and microglial activity of the hippocampus and medial prefrontal cortex that greatly associated with cognitive function. There is a high risk of internet addiction in persons who stay up late using the internet, spend too much time online, and share personal information soon after meeting others on social media sites, and it is argued that internet addiction may result in cognitive dysfunction furtherly12,13 These results suggest that passive (such as insomnia) or active (staying up late, working overtime, too much nightlife, etc) sleep deprivation can damage brain function and induce cognitive impairment.
In addition, it is widely accepted that the incidence of depressive disorder is high in developed countries and increases annually in developing countries.14,15 It has become a main research topic to explore the etiology of depressive disorder in the context of behavioral addiction and the obesity epidemic. It has been reported that problematic mobile phone use, including loss of control, withdrawal, caving, and virtual socialization dependence, is strongly associated with depressive disorder and related symptoms of anxiety, stress sensitivity, sleep disturbance, and somatic symptoms. At the same time, lack of sleep, irregular eating, living alone, urban life, and exposure to particulate matter less than 2.5 µm in diameter (PM2.5) are also proved as risk factors of depressive disorder.16–18 Body mass index (BMI), a standard that commonly used to measure the degree of obesity and health level of the human body, is related to endocrine imbalance, sleep quality, dietary structure, physical exercise habits, one recent study showed that lower BMI, especially in those with BMI below 22.1 kg/m2, is associated with a higher risk of recent suicide attempts (SA) in Chinese patients with first-episode drug-naïve (FEDN) of major depressive disorder (MDD).19 Some other studies suggested that Individuals with MDD exhibited reduced total 24-h heart rate variability (HRV) and daytime HRV, as well as ascended levels of inflammatory markers of C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-α), and multivariate analyses revealed robust inverse associations of total 24-h HRV and daytime HRV with IL-6, that is, an attenuated daytime HRV may correlate with higher circulating levels of IL-6 in MDD patients. Furthermore, one study confirmed that erythrocyte linoleic acid (LA) was positively associated with higher appendicular lean mass (ALM/BMI), higher pre-meal heart rate variability, and better reported overall sleep quality.20,21 In summary, it was confirmed that an individual’s lifestyle, behavioral habits, diet structure, and environmental pollution are strongly related to depressive disorder.
Previous studies have found that processing speed, attention/vigilance, working memory, verbal learning and memory, visual learning and memory, and social cognition in patients with MDD had significantly impaired performance compared with their controls, while depressive symptoms are usually considered as risk factors for cognitive decline.22,23 Based on clinical observations, we know that the interaction process of cognitive decline and depressive symptoms could determine the symptom severity, treatment response, and prognosis of MCI, MDD, and Alzheimer’s disease.
Regular aerobic exercise plays a positive role in controlling blood pressure, lowering blood lipids, improving sleep quality, and reducing problematic use of mobile phones, which can further alleviate individuals’ depressive symptoms and promote the improvement of cognitive function.24,25 There is a lack of in-depth exploration of the neural mediators of how regular aerobic exercise improves depressive symptoms and cognitive impairment. Neurotrophic factor is a type of protein that exerts great influence on the development, survival, and apoptosis of neurons and the regulation and implementation of brain function, one previous study suggested that aerobic exercise may evidently affect the level of neurotrophic factors in circulating blood,26 therefore, this study hypothesized that regular aerobic exercise could improve cognitive impairment and depressive symptoms by regulating neurotrophic factors.
The aim of this study was to investigate the effects of regular aerobic exercise on cognitive function, depression levels, and the regulatory effects of brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF).
Material and Methods
Participants
Eighty fitness club members, including 58 females and 22 males, aged 27–44 years, were recruited as part of the study group in a fitness center by random sampling from January 2021 to December 2022. The inclusion criteria were as follows: good health without severe physical diseases, mental disorders, or disease history; all members participating in fitness clubs for the first time; aerobic exercise consisting of swimming, riding a spinning bike, running on a treadmill, aerobic gymnastics, pilates, and yoga; and aerobic exercise at least four times a week and 2 h once (National Fitness Guide, General Administration of Sport in China).
Eighty community residents were enrolled as the control group by convenience sampling, including 47 females and 33 males with an age distribution ranging from 31 to 47 years. The inclusion criteria were as follows: good health without dysfunction or disability in working, interpersonal communication, and family life; no experience of life events within six months; and absence of regular exercise habits.
Participants with serious diseases (eg, diabetes, cardiovascular, and cerebrovascular diseases, brain trauma, major depressive disorder, schizophrenia, etc), disease history, psychosocial function disability, experience of severe mental trauma event in the past six months (eg, death of spouse, divorce, serious accidents, etc), a history of psychoactive substance abuse, and treatment history of antidepressants, physical therapy, and psychotherapy in the past were excluded.
All participants were administered the mental assessment scale and enzyme-linked immunosorbent assay(ELISA) test after six months of regular aerobic exercise.
Evaluation Scales
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)
RBANS was used to evaluate cognitive performance in patients with MDD and in a healthy population. RBANS has good reliability and validity and consists of 12 subtests (list learning, story memory, figure copy, line orientation, picture naming, semantic fluency, digit span, coding, list recall, list recognition, story recall, and figure recall), which are assigned to five factors: immediate memory (IM), visuospatial abilities (VB), language (L), attention (A), and delayed memory (DM) for a total scale score. The higher the score, the better the cognitive function.27
Patient Health Questionnaire (PHQ-9)
The PHQ-9 contains nine items, which are scored on a scale of 0 to 3 to assess the depression level in the past two weeks. The PHQ-9 is applicable to depression assessment in patients with MDD and healthy individuals, with higher scores indicating more severe depression.28
Detection of Neurotrophic Factor in Peripheral Blood
Peripheral blood (5 mL), collected from the median cubital vein into EDTA-containing anticoagulant tubes from 8:00 to 9:00 a.m. on an empty stomach, was centrifuged at 3600 rpm at 5°C for 15 min, and the isolated serum was extracted and stored in a medical ultra-low temperature refrigerator at –80°C for later use. An ELISA was used to detect the concentrations of BDNF and GDNF in peripheral blood with the lowest detection concentration of the ELISA kit (0.05 ng/mL), and the detection procedure was carried out according to the manufacturer’s instructions.
Statistical Processing
SPSS (version 21.0; IBM Corp., Chicago, IL, USA) was used for statistical analysis. An independent sample t-test was used for between-group comparisons and Pearson’s correlation, and multiple regression analysis was used to determine the relationship between variables. Measurement data was presented as by “mean ± standard deviation ( )” and two-sided p-values <0.05 were considered statistically significant.
)” and two-sided p-values <0.05 were considered statistically significant.
Results
Comparison of Cognitive Function and Depression Level Between Study Group and Control Group
Independent sample t-tests were conducted for between-group comparison of cognitive function and depression level, as shown in Table 1. The total score and factor scores, except for visuospatial abilities, were higher and the total score of the PHQ-9 was lower in the study group than in the control group (p<0.05 or 0.01).
 |
Table 1 Between-Group Comparison of Cognitive Function and Depression Level ( |
Comparison of Neurotrophic Growth Factor Between Study Group and Control Group
An independent sample t-test for the comparison of BDNF and GDNF in the serum of peripheral blood suggested that the concentrations of BDNF and GDNF in the serum of the study group were higher than those in the control group (p<0.05) (Table 2).
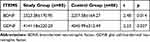 |
Table 2 Comparison of Neurotrophic Growth Factor Between Study Group and Control Group ( |
Correlation Analysis of Cognitive Function, Depression Level, and Neurotrophic Growth Factor in Study Group
Pearson’s correlation between cognitive function, depression level, and neurotrophic growth factors in study group showed that total score and factor scores of RBANS positively, total score of PHQ-9 negatively correlated with the concentrations of BDNF and GDNF (p<0.05 or 0.01) (Table 3).
 |
Table 3 Pearson’s Correlation of Cognitive Function, Depressive Level and Neurotrophic Growth Factor in Study Group(r) |
Multiple regression analysis of cognitive function, depression level, and neurotrophic growth factor in study group
Using the total scores of RBANS and PHQ-9 as dependent variables and the concentrations of BDNF and GDNF as independent variables, multiple regression analysis verified that BDNF had a predictive effect on the total scores of RBANS and explained 59.90% of RBANS variation (p< 0.01) and GDNF significantly predicted the total PHQ-9 score and could explain 12.30% of its variation (p<0.05) (Table 4).
 |
Table 4 Multiple Regression Analysis of Cognitive Function, Depression Level and Nerve Growth Factor in Study Group |
Discussion
Based on economic development and scientific and technological progress in the first 20 years of the twenty-first century, people’s lives have become increasingly intelligent and informed, which is recognized as a sign of social progress that has greatly changed the styles of reading, social communication, entertainment, and thinking. At the same time, stress in life has become more and more severe, one previous study seemingly indicated that stress was strongly associated with smartphone addiction, and consequently, online games, mobile phone misuse, and virtual communication, which constitute the main part of daily life in the young and the middle-aged people, have caused many health problems, including MCI, depressive disorder, behavioral addiction, obesity, and are known as a public health concerns.29–31 It is argued that regular aerobic exercise is a key part of the disease prevention and rehabilitation system associated with a healthy lifestyle. Therefore, there is an urgent need to further explore the neural mechanism about how regular aerobic exercise could improve cognitive function and ameliorate depressive symptoms.
This study investigated the effects of regular aerobic exercise on cognitive function, depressive levels, and the regulatory mechanisms of neurotrophic factors. The results showed that the total score of RBANS and factor scores, except visuospatial abilities, were higher, the total score on PHQ-9 was lower in the study group than in the control group, and the concentrations of BDNF and GDNF in the serum of the study group were higher than those of the controls. The concentrations of BDNF and GDNF were associated with the total score of the RBANS and factor scores and the total score of the PHQ-9. These results indicate that regular aerobic exercise can improve cognitive impairment and depressive symptoms by increasing the concentrations of BDNF and GDNF.
Previous studies have confirmed that BDNF and GDNF are essential for survival, differentiation, growth, neuronal maturation, axon targeting, synaptic development, and synaptic plasticity.32,33 Previous studies have reported that BDNF and GDNF are significantly associated with cognitive function and depressive disorders, one study found that BDNF in the serum was a predictor of cognitive impairment in patients with small cerebral vessel disease. In addition, the reduction of BDNF is considered to be an important pathological mechanism of depressive disorder, and it has been shown that BDNF in the serum is reduced in patients with depressive disorder, and a variety of antidepressants, including escitalopram, ketamine, and radix stellariae, can improve depression by increasing BDNF levels.34,35 GDNF is also associated with cognitive impairment in patients with schizophrenia, obsessive-compulsive disorder, and hypertension, and can regulate synaptic plasticity by binding to the GDNF family receptor α. GDNF, which controls the survival, development, and maintenance of dopaminergic and serotonergic neurons, also has neuroprotective properties by inhibiting oxidative stress and neuroinflammatory damage,36,37 so it is conducive to the maintenance and promotion of cognitive function. Other studies have proposed that GDNF, as a member of the transforming growth factor β superfamily, is important for the survival of dopaminergic neurons, and a decrease in GDNF aggravates the apoptosis of dopaminergic neurons and may eventually induce depressive disorder.38,39 It could be concluded that the decrease in BDNF and GDNF is one of the pathological bases of cognitive impairment and depression episodes.
Regular aerobic exercise can promote the dynamic balance and maintain a high level of BDNF and GDNF in the human body. It is argued that aerobic exercise may affect BDNF level through multiple pathways, eg, lactic acid metabolites released by mouse muscles during aerobic exercise can penetrate blood–brain barrier and induce BDNF expression in hippocampus. Furthermore, aerobic exercise can induce the upregulation of PGC-1α gene expression in neurons, which promotes the secretion of fibronectin type III domain-containing protein 5 (FNDC5) and irisin synthesis, leading to an increase in BDNF levels. BDNF also increases by activating the peroxisome proliferator-activated receptor γ coactivator-1α (PGC1α) or FNDC5 pathway and improving the penetration of cathepsin B into the blood–brain barrier during aerobic exercise.40,41 One study reported that aerobic exercise combined with SSRIs can significantly increase GDNF levels and improve the therapeutic effect in adolescents with depressive disorders by inhibiting oxidative stress, regulating glial cell function, and inhibiting apoptosis, etc.42,43 Based on the condition of higher levels of BDNF and GDNF, cognitive function could be improved and depression levels could be ameliorated.
At present, the urbanization process in China has greatly changed people’s lifestyles, and almost every social group may face various pressures and uncertainties in the future. Smartphones, as the main sources of information acquisition, electronic payments, amusement, pressure relief, and social contact, are becoming very popular and bring great benefit to people’s daily lives. At the same time, mobile phone misuse was believed to associate with a series of mental health problems, such as game addiction, online shopping addiction, job burnout, and depressive disorder. Moreover, it was verified that lack of exercise identity, exercise behavior were risk factors of mobile phone addiction.44,45 The results of this study clearly showed that a health-promoting lifestyle, especially regular aerobic exercise, has a beneficial impact on the prevention and rehabilitation of cognitive impairment and depressive disorders. To the best of our knowledge, this is the first study to explore the effect of regular aerobic exercise on cognitive function and depression and its preliminary neural mechanism in healthy people, which, to some degree, bridges the gap in the field of health promotion between patients in clinical settings and healthy individuals. This may have great implications for the general population in terms of health maintenance, conservation of medical expenditure, and improvement of quality of life.
The present study may have some limitations; however, it is offset by a variety of strengths that require consideration. First, the data were cross-sectional, which did not allow us to conclude causal relationships. Second, the small sample size may have made the results susceptible to type II errors; therefore, caution should be exercised when applying these data to other settings.
The following are some directions for future research: There is an urgent need to conduct prospective studies to observe health outcomes and quality of life in the healthy group of regular aerobic exercise in future research. Previous studies have explored the pathophysiology of BDNF in improving cognitive impairment and depressive symptoms and clinical intervention programs for BDNF upregulation in previous studies46,47 However, the role of GDNF and its pathological mechanism in mental disorders is a new research area, suggesting a new hypothesis that GDNF may also alter cognitive function and induce depressive symptoms by promoting the survival of dopaminergic neurons and high-affinity uptake of dopamine and preventing the degeneration of dopaminergic neurons.48 More empirical research is necessary to provide new evidence for this hypothesis. Moreover, based on the results of the present study, it could conclude that GDNF, as a potential therapeutic target, may be valuable for treatment of MDD and MCI in clinical practice, discovery of new drug and its pharmacological mechanism that targeted at GDNF upregulation is another research direction.
Conclusion
In this study, it was observed that regular aerobic exercise can improve cognitive function and ameliorate depressive symptoms by increasing the concentrations of BDNF and GDNF in healthy people. These findings provide preliminary evidence that aerobic exercise is a valid strategy for maintaining cognitive function and preventing depressive disorders in the general population.
Ethics Statement
This study was reviewed and approved by the Ethical Review Committee for Medical Research at No.904th Hospital, China. All participants provided written informed consent to participate in this study. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Acknowledgments
The authors thank all participants in this study for their cooperation and Prof. Kong DR for critically reading the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yang ZY. Behavior determines health. Clin Focus. 2011;26:1081.
2. Zeng SJ, Zhang CG, Cui ZW, et al. Study on association between smoking and risk of mild cognitive impairment in elderly in xuhui. Health Health Edu Health Prom. 2022;17:249–290.
3. Tao XQ, Liao X, Li MQ, et al. Epidemiological study on mild cognitive impairment among the elderly in Nanchang community. Chin J Gerontol. 2016;36:3283–3286.
4. Liu LJ, Hayden KM, May NS, et al. Association between blood pressure levels and cognitive impairment in older women: a prospective analysis of the women’s health initiative memory study. Lancet Healthy Longev. 2022;3(1):e42–e53. doi:10.1016/S2666-7568(21)00283-X
5. Liu W, Zhou C, Wang YS, et al. Vitamin D deficiency is associated with disrupted cholesterol homeostasis in patients with mild cognitive impairment. J Nutr. 2021;151(12):3865–3873. doi:10.1093/jn/nxab296
6. Tumati S, Boyd E, Ismail Z, et al. Neuropsychiatric symptoms and their relationship with white matter hyperintensities in mild vascular cognitive impairment, mild cognitive impairment, alzheimer’s disease and mixed dementia – a COMPASS-ND study. Am J Geriat Psychiat. 2023;31(3):S45–S46. doi:10.1016/j.jagp.2022.12.203
7. Zhu SW, He MJ, Su DT, et al. Association between the diet balance index-based dietary quality and cognitive function among Zhejiang population aged 40 years and older. J Hygiene Res. 2022;51:374–380.
8. Bodden C, Hannan AJ, Reichelt AC. Of ‘junk food’ and ‘brain food’: how parental diet influences offspring neurobi-ology and behaviour. Trends Endocrinol Metab. 2021;32(8):566–578. doi:10.1016/j.tem.2021.04.001
9. Francis H, Stevenson R. The longer-term impacts of Western diet on human cognition and the brain. Appetite. 2013;63:119–128. doi:10.1016/j.appet.2012.12.018
10. Strachan MWJ, Reynolds RM, Marioni RE, et al. Cognitive function, dementia and type 2 diabetes mellitus in the elderly. Nat Rev Endocrinol. 2011;7(2):108–114. doi:10.1038/nrendo.2010.228
11. McNay EC, Recknagel AK. Brain insulin signaling: a key component of cognitive processes and a potential basis for cognitive impairment in type 2 diabetes. Neurobiol Learn Mem. 2011;96(3):432–442. doi:10.1016/j.nlm.2011.08.005
12. Wang Z, Chen WH, Li SX, et al. Gut microbiota modulates the inflammatory response and cognitive impairment induced by sleep deprivation. Mol Psychiatry. 2021;26(11):6277–6292. doi:10.1038/s41380-021-01113-1
13. Kumar T, Rajendran V, Dutta G, et al. Prevalence of internet addiction and impact of internet socialization on professional, academic, social lives and sleep pattern among students and professionals from various fields across India. Adv Med Educ Pract. 2023;14:1369–1378. doi:10.2147/AMEP.S438215
14. Hunt GE, Malhi GS, Lai HMX, et al. Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: systematic review and meta-analysis. J Affect Disord. 2020;266:288–304. doi:10.1016/j.jad.2020.01.141
15. Liao DD, Dong M, Ding KR, et al. Prevalence and patterns of major depressive disorder and subthreshold depressive symptoms in South China. J Affect Disord. 2023;329:131–140. doi:10.1016/j.jad.2023.02.069
16. Winkler A, Jeromin F, Doering BK, et al. Problematic smartphone use has detrimental effects on mental health and somatic symptoms in a heterogeneous sample of German adults. Comput Hum Behav. 2020:113. doi:10.1016/j.chb.2020.106500
17. Liu JH, Liu CX, Wu T, et al. Prolonged mobile phone use is associated with depressive symptoms in Chinese adolescents. J Affect Disord. 2019;259:128–134. doi:10.1016/j.jad.2019.08.017
18. Roberts S, Arseneault L, Barratt B, et al. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019;272:8–17. doi:10.1016/j.psychres.2018.12.050
19. Liu JJ, Jia FN, Li CW, et al. Association between body mass index and suicide attempts in Chinese patients of a hospital in Shanxi district with first-episode drug-naïve major depressive disorder. J Affect Disord. 2023;339:377–383. doi:10.1016/j.jad.2023.06.064
20. Euteneuer F, Neubert M, Salzmann S, et al. Associations between indices of 24-hour heart rate variability and inflammation in individuals with major depressive disorder. Int J Psychophysiol. 2023;188:72–78. doi:10.1016/j.ijpsycho.2023.03.009
21. Belury M, Cole R, Andridge R, et al. Erythrocyte linoleic acid is associated with higher heart rate variability and better sleep quality: a possible link to reducing risk for cardiometabolic diseases. Curr Dev Nutr. 2022;6:412. doi:10.1093/cdn/nzac055.001
22. Huang X, Lai S, Lu X, et al. Cognitive dysfunction and neurometabolic alternations in major depressive disorder with gastrointestinal symptoms. J Affect Disord. 2023;322:180–186. doi:10.1016/j.jad.2022.10.036
23. Spira AP, Rebok GW, Stone KL, et al. Depressive symptoms in oldest-old women: risk of mild cognitive impairment and dementia. Am J Geriatr Psychiatry. 2012;20(12):1006–1015. doi:10.1097/JGP.0b013e318235b611
24. Arsh A, Afaq S, Carswell C, et al. Effectiveness of physical activity in managing co-morbid depression in adults with type 2 diabetes mellitus: a systematic review and meta-analysis. J Affect Disord. 2023;329:448–459. doi:10.1016/j.jad.2023.02.122
25. Ahn J, Kim M. Effects of aerobic exercise on global cognitive function and sleep in older adults with mild cognitive impairment: a systematic review and meta-analysis. Geriatr Nurs. 2023;51:9–16. doi:10.1016/j.gerinurse.2023.02.008
26. Rodriguez-Ayllon M, Plaza-Florido A, Mendez-Gutierrez A, et al. The effects of a 20-week exercise program on blood-circulating biomarkers related to brain health in overweight or obese children: the active brains project. J Sport Health Sci. 2023;12(2):175–185. doi:10.1016/j.jshs.2022.12.007
27. Zhang BH, Tan YL, Zhang WF, et al. Repeatable battery for the assessment of neuropsychological status as a screening test in Chinese: reliability and validity. Chin Mental Health J. 2003;22:865–869.
28. Li S, Yu RJ, Guo Y, et al. Reliability and validity comparison and correlation analysis of PHQ-9 in community postpartum depression evaluation. J Clin Psychosom Dis. 2020;26:99–137.
29. Ma D, Li B, Liu X, et al. The moderating effect of self-efficacy on pregnancy stress and smartphone addiction of pregnant women in late pregnancy: a longitudinal study. Risk Manag Healthc Policy. 2024;17:41–48. doi:10.2147/RMHP.S445581
30. Robayo-Pinzon S, Foxall GR, Montoya-Restrepo LA, et al. Does excessive use of smartphones and apps make us more impulsive? An approach from behavioural economics. Heliyon. 2021;7(2):e06104. doi:10.1016/j.heliyon.2021.e06104
31. Bediou B, Wac K. The role of cognition in mediating the relationship between media use and health in a media saturated world. Encyclop Child Adolesc Health. 2023;3:299–313.
32. Prowse N, Hayley S. Microglia and BDNF at the crossroads of stressor related disorders: towards a unique trophic phenotype. Neurosci Biobehav Rev. 2021;131:135–163. doi:10.1016/j.neubiorev.2021.09.018
33. Grondin R, Littrell OM, Zhang ZM, et al. GDNF revisited: a novel mammalian cell-derived variant form of GDNF increases dopamine turnover and improves brain biodistribution. Neuropharmacology. 2019;147:28–36. doi:10.1016/j.neuropharm.2018.05.014
34. Chen RS, Sun YS, Wang DH, et al. Relationship between serum BDNF,NPY,SVD score and cognitive function in patients with cerebral small vascular disease. J Brain Nerv Dis. 2022;30:638–642.
35. Wang XL, Liu XR, Li ZP. Research progress of depressive disorder and brain derived neurotrophic factor. J Henan Med College Staff Work. 2021;33:625–628.
36. Xiao WH, Ye F, Liu CL, et al. Cognitive impairment in first-episode drug-naïve patients with schizophrenia: relationships with serum concentrations of brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:163–168. doi:10.1016/j.pnpbp.2017.03.013
37. Qin SY, Gao Y. Effect of different-intensity exercise on control of blood pressure, cognitive function, glial cell line derived neurotrophic factor of serum in male patients with primary hypertension. Chin J Hypertension. 2020;28:785–788.
38. Liu XY, Ma XJ, Zhang J, et al. Association between plasma levels of BDNF and GDNF and the diagnosis, treatment response in first-episode MDD. J Affect Disord. 2022;315:190–197. doi:10.1016/j.jad.2022.07.041
39. Jeuring H. The effectiveness of dopamine stimulating agents in depressive disorder. Am J Geriat Psychiat. 2023;31(3):S46–S47. doi:10.1016/j.jagp.2022.12.204
40. Ke JH, Wang B. Effects of aerobic exercise on memory and its neurobiological mechanism. Adv Psychol Sci. 2022;30(1):115–128. doi:10.3724/SP.J.1042.2022.00115
41. Zhong QL, Zhong SM, Lai SK, et al. Research progress on the mechanisms of exercise improving cognitive dysfunction in major depressive disorder. Chin J Nerv Mental Dis. 2022;48:701–704.
42. Fu ZJ, Xu MY, Wang TD, et al. Effects of aerobic exercise therapy combined with selective 5-hydroxytryptamine reuptake inhibitor on the remission of psychiatric symptoms and social function in adolescent patients with depression. J Clin Patholl Res. 2022;42:3047–3054.
43. Dai JR, Guo SS, Luo L. Effects of exercise rehabilitation on ischemic stroke. J Qufu Normal University. 2017;43:119–123.
44. Liu J, Wang W, Hu Q, et al. The relationship between phubbing and the depression of primary and secondary school teachers: a moderated mediation model of rumination and job burnout. J Affect Disord. 2021;295:498–504. doi:10.1016/j.jad.2021.08.070
45. Wan XY, Ren YJ. Exercise identity, exercise behavior and mobile phone addiction: a cross-sectional mediation study with a sample of rural left-behind children in China. Heliyon. 2023;9(4):e14953. doi:10.1016/j.heliyon.2023.e14953
46. Vyas CM, Mischoulon D, Chang G, et al. Relation of serum BDNF to major depression and exploration of mechanistic roles of serum BDNF in a study of vitamin D3 and omega-3 supplements for late-life depression prevention. J Psychiatr Res. 2023;163:357–364. doi:10.1016/j.jpsychires.2023.05.069
47. Wang Y, Bai LP, Liu W, et al. Altered BDNF levels are associated with cognitive impairment in parkinson’s disease patients with depression. Parkinso Relat Disord. 2022;103:122–128. doi:10.1016/j.parkreldis.2022.08.020
48. Moriarty N, Gantner CW, Hunt CPJ, et al. A combined cell and gene therapy approach for homotopic reconstruction of midbrain dopamine pathways using human pluripotent stem cells. Cell Stem Cell. 2022;29:434–448. doi:10.1016/j.stem.2022.01.013
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


