Back to Journals » Infection and Drug Resistance » Volume 16
Effect of Platelet Parameters on Linezolid-Related Thrombocytopenia in Hospitalized Patients
Authors Zhang L, Yan Y, Liao R, Dong H
Received 10 February 2023
Accepted for publication 31 August 2023
Published 12 September 2023 Volume 2023:16 Pages 6145—6154
DOI https://doi.org/10.2147/IDR.S408102
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Lu Zhang, Yan Yan, Ru Liao, Haiyan Dong
Department of Pharmacy, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, 710061, People’s Republic of China
Correspondence: Haiyan Dong, Department of Pharmacy, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, 710061, People’s Republic of China, Tel/Fax +86-29-85323508, Email [email protected]
Background: Linezolid-induced thrombocytopenia incidence varies considerably. Linezolid-related thrombocytopenia in patients has received few studies which have investigated risk factors including platelet parameters except for platelet counts. The study aims to analyze the effect of platelet parameters, including mean platelet volume and platelet large cell ratio, on linezolid-related thrombocytopenia in patients.
Methods: The effect of platelet parameters on linezolid-related thrombocytopenia was identified by univariate and multivariate logistic regressions. A Kaplan–Meier survival analysis was carried out to compare the survival of patients who developed linezolid-related thrombocytopenia with patients who did not.
Results: Thrombocytopenia occurred at a rate of 41.5% (66/159) after linezolid therapy in hospitalized patients. Platelet parameters, including the difference in mean platelet volume (MPV/fL=0.08 (− 1.2– 0.9)vs-0.5 (− 1.5– 0.3), (OR, 0.459; P = 0.001), the difference in platelet large cell ratio (PLCR/fL=0.9 (− 5.1– 6.2)vs-3.8 (− 8.6– 2.4), (OR, 1.156; P = 0.001), baseline platelet counts (OR, 0.995; P = 0.006) and duration of linezolid therapy≥ 10d (OR, 1.346; P = 0.007), were significantly associated with linezolid-related thrombocytopenia in hospitalized patients. In addition, other risk factors which also are associated with linezolid-related thrombocytopenia include baseline red blood cells, co-medication with parecoxib and co-medication with caspofungin. Accumulated in-hospital mortality of patients with thrombocytopenia was significantly higher than that of patients without thrombocytopenia during linezolid treatment (19.7% vs 8.6%, P = 0.003).
Conclusion: The difference in mean platelet volume, the difference in large platelet ratio, baseline platelet counts and duration of linezolid therapy≥ 10d significantly affected the development of linezolid-related thrombocytopenia in hospitalized patients.
Keywords: linezolid, platelet parameters, thrombocytopenia, risk factors
Introduction
Linezolid is the first approved fully synthetic oxazolidinone antibacterial drug, in (vancomycin-resistant enterococci-resistant Enterococcus, VRE), methicillin-resistant Staphylococcus aureus (multi-drug-resistant Staphylococcus aureus, MRSA), Mycobacterium tuberculosis (Mycobacterium tuberculosis) infection and other diseases treatment playing a pivotal role in.1,2 With the clinical application of linezolid, a wide range of thrombocytopenia caused by same (adverse drug reaction, ADR) has become increasingly prominent, and the risk of treatment failure in patients has increased.3
Thrombocytopenia, defined as a platelet count < 75% of baseline count and ˂ 100×109/L after medication,3 or defined as a ≥10×104 cells/mm³ decrease from the baseline or a ≥ 30% reduction,4 is among the most common adverse events during linezolid treatment.5,6 Due to the difference in inclusion criteria and/or exclusion criteria among prior studies, the incidence of thrombocytopenia varies considerably (2.4–78.6%).7–9
The utility of platelet parameters have been found to play an important role in discerning thrombocytopenia.10 For example, platelet size, measured as MPV and PLCR, has been proved to have prognostic and diagnostic values in discriminating thrombocytopenia.11 It also has been found to be a factor for discriminating hypoproductive and hyperdestructive thrombocytopenia.12 A strong positive correlation is found between MPV and quantities of granular megakaryocytes (P = 0.03), whereas a negative relationship existed between MPV and platelet-form megakaryocytes (P = 0.028).13 MPV and PLCR were significantly higher in patients with immune thrombocytopenia than in patients with hypoproductive thrombocytopenia (P < 0.0001).14 Although studies have reported that lower baseline platelet values,3 lower body weight15 and longer medication time16 et al in patients are independent risk factors for linezolid-related thrombocytopenia, few studies have investigated platelet parameters as risk factors for linezolid-related thrombocytopenia.
Previous studies have reported thrombocytopenia induced by linezolid at various levels, improvement of treatment measures, clinical efficacy of linezolid, and predictors of linezolid-induced thrombocytopenia. However, studies are insufficient and often limited due to variability in study design and patient populations. Most studies included patients with a hematological neoplastic disease. Such a disease may considerably hamper the assessment of thrombocytopenia. In addition, some published studies on risk factors for linezolid-induced thrombocytopenia from Asian countries and several Western countries showed considerable inter-study variability in their findings.
Therefore, the purpose of this study is to identified the effect of platelet parameters on linezolid-related thrombocytopenia in hospitalized Chinese patients (patients with hematological malignancies are excluded) by analyzing risk factors of thrombocytopenia in hospitalized patients treated with linezolid.
Materials and Methods
Patients and Study Design
The study population included hospitalized patients treated with linezolid in a tertiary teaching hospital in China during the period from January 2020 to December 2021. Inclusion criteria: (1) patients received linezolid therapy during hospitalization; (2) patients with at least two of the following symptoms: i) body temperature > 38°C or < 36°C; ii) respiration rate (> 20 times/min) or PaCO2 < 32mmHg; iii) heart rate > 90 times/min; iv) peripheral white blood cell (WBC) count > 10×109/L, peripheral WBC count < 4×109/L, or normal peripheral WBC count but immature cells > 10%. Exclusion criteria: (1) patients with incomplete data; or (2) pregnant patients.
For each included patient, a standardized electronic case report system was used by investigators to collect data including social demographic characteristics, clinical diagnosis, comorbidities, laboratory values, length of ICU and hospital stay. The study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University, and the informed consent was waived since the study was retrospective and the data were collected anonymously.
Definition
In the present study, thrombocytopenia was defined as a decrease in platelet count of ≥ 25% and a final count of < 100×109/L.3
After 7 days of medication. In the present study, thrombocytopenia was defined as a decrease in platform count of ≥ 25% and a final count of <100 × 109/L. 159 inpatients of 66 (41.5%) had thrombocytopenia after Linezolid treatment. Count the cases where the decrease in platelet count after medication is greater than or equal to 25% compared to the baseline examination value before medication, as shown in the Table 1.
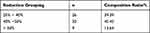 |
Table 1 Status of Thrombocytopenia in Positive Cases |
Statistical Analysis
Quantitative variables were summarized with mean ± standard deviation (SD) or median with interquartile range (IQR) depending on normality of the distribution. Number (percentage) was used for qualitative variables. The Shapiro–Wilk test was carried out to test normality. Independent t test or Mann–Whitney U-test was implemented for data comparison while appropriate and categorical variables are analyzed with Chi-square test or Fisher exact test. Variables with P < 0.1 in the univariate analysis were included in the multivariate analysis. Before multivariate analysis, collinearity test was conducted to determine the collinearity among those factors. If tolerance (T) > 0.1 or variance inflation factor (VIF) < 10, no collinearity existed among those factors. Then risk factors were confirmed according to the multivariate analysis. The odds ratios (OR) and corresponding 95% confidence intervals (95% CI) were reported.
The cumulative incidence of in-hospital mortality, was compared through a Log rank test and presented with Kaplan–Meier curves.
All statistical analysis was performed on the Statistical Package for the Social Sciences version 19.0 (SPSS, Chicago, IL, USA). All tests were two-side, and P < 0.05 was considered statistically significant.
Results
Demographics and Clinical Characteristics of Study Population
A total of 159 hospitalized patients received linezolid therapy from January 2020 to December 2021 were finally included in the study, of which male patients accounting for 67.3% (107/159). The patients’ median age was 62 years, and 69 of 159 patients (43.3%) aged ≥ 65 years. The leading infection type was pulmonary infection (86.2%), followed by intra-abdominal infection (27.0%). Specific patient characteristics are shown in Table 2. Platelet count in patients with thrombocytopenia: Before medication: (159.1±57.3)×109/L and After medication: (105.6 ± 51.3)×109/L in Figure 1.
 |
Table 2 Characteristics of Patients Enrolled in the Study |
 |
Figure 1 Trend in platelet counts before and following linezolid. |
Risk Factors Associated with Thrombocytopenia
Among the patients included, 66 (41.5%) patients developed thrombocytopenia. Table 3 shows the demographic data, comorbidities, laboratory tests and concomitant medications of hospitalized patients with linezolid-related thrombocytopenia and patients without thrombocytopenia.
 |
Table 3 Univariate Logistic Regression Results for Risk Factors Developing Thrombocytopenia |
In the univariate analysis, renal insufficiency, CRRT, the difference in MPV, the difference in PLCR, baseline PLT counts, baseline RBC, baseline CREA, baseline ALT, lactic acid<2.5mmol/L, combined use of parecoxib or/and caspofungin were associated with a higher risk of linezolid related thrombocytopenia in hospitalized patients (P< 0.1). No significant difference was observed in the thrombocytopenia incidence in relation to other baseline levels and other concurrent medications, including baseline CREA, baseline ALT and CRRT et al Table 3 details the information of the patients.
According to the univariate analysis, the collinearity of these potential prognostic variables was estimated. No multi-collinearity was found with VIF < 10. Therefore, the aforementioned factors were included in the multivariate analysis. Finally, the multivariate analysis shows that the difference in MPV (OR, 0.459 [95% CI, 0.372–0.857]; P = 0.001), the difference in PLCR (OR, 1.156 [95% CI, 1.078–1.359]; P = 0.001), baseline platelet counts (OR, 0.995 [95% CI, 0.991–0.998]; P = 0.006), baseline RBC (OR, 0.578 [95% CI, 0.459–0.916]; P = 0.005), co-medication with parecoxib (OR, 1.346 [95% CI, 0.951–1.528]; P = 0.007), duration of linezolid therapy ≥10 d,(OR, 1.169 [95% CI, 0.857–1.421]; P = 0.001), co-medication with caspofungin (OR, 2.521 [95% CI, 1.056–6.238]; P = 0.001) were found to be independently associated with linezolid-related thrombocytopenia in hospitalized patients (Table 4).
 |
Table 4 Factors Independently Associated with Thrombocytopenia in Hospitalized Patients with Linezolid Therapy |
Kaplan–Meier curves demonstrated a higher accumulated incidence of in-hospital mortality in patients suffered from linezolid-related thrombocytopenia than those who did not. P value is 0.003 from the Log rank test, as shown in Figure 2.
 |
Figure 2 Kaplan–Meier estimates of the cumulative incidence of in-hospital mortality. |
Discussion
66 hospitalized patients developed thrombocytopenia after linezolid therapy.
A previous study by Shen et al, found that LI-TP was closely associated with the duration of linezolid treatment, with their ROC curve indicating that a treatment duration ≥12 days was more likely to cause thrombocytopenia. Nukui et al, reported that half of the patients in their study developed thrombocytopenia within days of linezolid treatment, which is consistent with our results that 49.3% of elderly patients developed LI-TP within 10 days of initiating linezolid treatment. Duration of linezolid therapy ≥10 days was considered a significant risk factor for LI-TP in elderly patients in this study. Several studies speculated that LI-TP is caused by inhibiting the proliferation of progenitor cells and the onset of the decrease in platelet count is delayed and reaches a nadir at around 2 weeks.
In the present study, we found that the difference in MPV and the difference in PLCR were independently risk factors influencing thrombocytopenia in patients. To our knowledge, this relationship has not been reported previously. It has been demonstrated that some morphological platelet indices, such as MPV, are valuable for distinguishing thrombocytopenia. MPV is process in bone marrow.17 Enlarged MPV can be used as a measurement of young platelets, indicating that the origin of thrombocytopenia was peripheral destruction.18 Previous studies have shown that the mechanism for thrombocytopenia in patients was the increased platelet destruction caused by platelet desialylation.19 Thus, we tentatively speculated that the mechanism of thrombocytopenia in patients treated with linezolid might be decreased platelet count generation.
In addition, an increase in PLCR may indicate the presence of platelet aggregates, micro-erythrocytes, and giant platelet.20 Therefore, the increase in PLCR may be caused by the aggregation of platelets when they exert antimicrobial effect. Additionally, platelets generated from megakaryocytes in the bone marrow and released in the bloodstream through pseudopodial projections named proplatelets.21,22 The increase in the ratio of large platelets indicates that the mechanism of small platelets formation was impaired and the maturity was lowered. Therefore, we speculated that linezolid related thrombocytopenia may be caused by the decreased platelet production and increased platelet aggregation reflected by the increase in PLCR. Future work should explore the potential pathophysiologic link between platelet parameters and platelet dysfunction.
A previous study pointed out that for the blood in patients with risk factors such as advanced age and low platelet baseline value, the risk of thrombocytopenia is higher.5,6 The relation between plate reduction and the combination of the above risk factors and thrombocytopenia has not been reported so far. It is worth mentioning that previous studies have shown that compared with patients with lower platelet counts, the rate of thrombocytopenia in patients with higher baseline platelet counts is about 5 times higher.12 Meanwhile, the data in this treatise point out that patients with high baseline platelet counts are more likely to have a large and rapid platelet drop within 7 days of medication. In addition, patients with less concomitant anti-infective drugs often have low level of infection, relatively high baseline platelet value, and are more likely to develop platelet drop in a short time.
The mechanism of thrombocytopenia caused by linezolid is still unclear. Given the recent advances in our understanding and the studies on the role of platelet indices in thrombocytopenia, we imply that the inhibition of the formation of platelets may be a mechanism of linezolid-related thrombocytopenia.
Previous studies have shown that lower baseline platelet count may be closely related to linezolid-associated thrombocytopenia.23,24 Zhang et al reported that the ratio of platelet count (day 7/day 0) < 1 (OR = 10.021; P = 0.012) and the baseline platelet count (OR = 0.985; P = 0.036) were independent risk factors of thrombocytopenia at day 14 of linezolid therapy in patients with acute-on-chronic liver failure.25 Choi et al reported that only baseline platelet count < 150×103/mm3 was an independent predictor of early-onset (≤ 6 days) thrombocytopenia.26 It seems to indicate that the occurrence of linezolid-related thrombocytopenia is dependent on baseline platelet counts.
Baseline red blood cells were found to be associated with thrombocytopenia in this study. The increased risk of thrombocytopenia could be related to linezolid-induced myelosuppression, leading to red cell aplasia27 or abnormal erythroblast morphology.28 Whereas Bernstein et al failed to find any association,29 their conclusion may remain some uncertainties. Since some of their studies were based on case reports, the conclusions varied according to the difference in pathophysiological conditions. On the contrary, the present research identified the mechanism from the platelet indicators with a relatively large sample size. However, the assessment of the mechanism of linezolid-induced thrombocytopenia would be useful on the molecular level.
In the present study, the co-medication with parecoxib or/and caspofungin was a risk factor for thrombocytopenia which may be accounted for the variability in linezolid concentration caused by parecoxib, and may significantly alter plasma linezolid exposure.30 Studies have shown that linezolid caused thrombocytopenia related to higher drug exposure.31 In addition, caspofungin induced peripheral destruction of platelets acts as a likely contributor to linezolid induced thrombocytopenia.32
The patients included in this study were not monitored for blood drug concentration, but the dose of Linezolid and the change of blood drug concentration were related to the incidence of thrombocytopenia. According to relevant literature studies, thrombocytopenia is related to the valley concentration of Linezolid. The target concentration of Linezolid (2–8 mg/L), the higher the valley concentration, the higher the incidence of adverse reactions. Zuo M et al33–35 found that creatinine clearance, hemodialysis, duration of Linezolid use, and valley concentration of Linezolid were independent risk factors for thrombocytopenia. The steady-state trough concentration of Linezolid was significantly correlated with thrombocytopenia. These studies all show that the thrombocytopenia caused by Linezolid is related to the dosage and trough concentration of the drug.
In-hospital mortality estimated by Kaplan–Meier method was higher in hospitalized patients with thrombocytopenia after linezolid treatment (19.7% vs 8.6%, P = 0.003). The increased mortality in septic thrombocytopenic patients could be explained by increased serious thrombotic complications and platelet consumption reflected by thrombocytopenia or increased bleeding frequency/severity.36 Therefore, linezolid-related thrombocytopenia is associated with higher mortality during sepsis.
Thrombocytopenia is one of the common indicators of poor prognosis in critically ill patients, and is associated with longer ICU hospital stays and higher mortality rates.37 GURU K et.al38 et al showed that patients with thrombocytopenia at admission were treated with Linezolid, the mortality rate was three times that of patients without thrombocytopenia, and every 50% increase in platelet, accompanied by a 40% decrease in mortality rate. According to Du et al,39 the main causes of death of critically ill patients who were treated with Linezolid included Respiratory failure, septic shock and organ failure. Previous studies have confirmed that thrombocytopenia is associated with multiple system and organ dysfunction such as ALI, ARDS, capillary leakage syndrome, acute renal failure, and septic shock.40,41 Therefore, thrombocytopenia may lead to adverse outcomes such as patient death through multiple complex pathophysiological pathways. We look forward to more basic research to elucidate the mechanisms behind this.
In clinical work regarding linezolid-related thrombocytopenia, the harm of rare diseases and complex risk factors should be responded with the following proper prevention and treatment measures. ① Linezolid should only be used in the treatment or prophylaxis of confirmed or highly suspected infections caused by susceptible bacteria, In order to reduce the generation of drug-resistant bacteria and ensure the linezolid efficacy of amines. The use of linezolid in elderly and young patients with severe infections should be of particular concern. ② Reduce the combined use of antibacterial drugs as much as possible. ③ Blood routine tests are required before and during the medication. Monitoring is necessary to reduce the occurrence of serious adverse events. ④ In the event of linezolid-related thrombocytopenia, the use of drug should be discontinued immediately. Platelet counts generally return to normal/basal levels within 7 to 14 days. When platelet counts are significantly reduced, platelet transfusion, subcutaneous injection of human thrombopoietin and other treatments should be carried out.
There remain some limitations in the study. Firstly, the results lack molecular regulation of the mechanism of linezolid-related thrombocytopenia. Secondly, some factors may be missed since most of the factors considered in our study were based on literatures. Finally, the mechanism of linezolid-induced thrombocytopenia has not yet been elucidated, and there is still controversy over the topic. Therefore, further studies are required for the verification on cellular and molecular level. Despite of these limitations, the results may attribute to the study on the mechanism of linezolid-induced thrombocytopenia.
Conclusion
Platelet parameters, including the difference in MPV, the difference in PLCR and baseline platelet counts were significantly associated with the occurrence of linezolid-related thrombocytopenia in patients. Platelet parameters have an important implication in linezolid-induced thrombocytopenia. Platelet parameters monitoring should be encouraged for optimizing the utilization of linezolid in hospitalized patients.
Data Sharing Statement
The clinical data of patients used to support the findings of this study are included within the article.
Ethical Approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University (Xi’an, China) [XJTU1AF2019LSK-163] and complied with the Declaration of Helsinki.
Funding
This study was funded by the National Natural Science Foundation of China (No. 82173898), and the Programs for The First Affiliated Hospital of Xi’an Jiaotong University (No. 2019ZYTS-01).
Disclosure
The authors declare that there is no conflict of interest in this work.
References
1. Lazaris A, Coleman DC, Kearns AM, et al. Novel multiresistance cfr plasmids in linezolid-resistant methicillin-resistant Staphylococcus epidermidis and vancomycin-resistant Enterococcus faecium (VRE) from a hospital outbreak: co-location of cfr and optrA in VRE. J Antimicrob Chemother. 2017;72(12):3252–3257. doi:10.1093/jac/dkx292
2. Leach KL, Brickner SJ, Noe MC, et al. Linezolid, the first oxazolidinone antibacterial agent. Ann N Y Acad Sci. 2011;1222(1):49–54. doi:10.1111/j.1749-6632.2011.05962.x
3. Dong HY, Xie J, Chen LH, et al. Therapeutic drug monitoring and receiver operating characteristic curve prediction may reduce the development of linezolid-associated thrombocytopenia in critically ill patients. Eur J Clin Microbiol Infect Dis. 2014;33(6):1029–1035. doi:10.1007/s10096-013-2041-3
4. Takahashi Y, Takesue Y, Nakajima K, et al. Risk factors associated with the development of thrombocytopenia in patients who received linezolid therapy. J Infect Chemother. 2011;17(3):382–387. doi:10.1007/s10156-010-0182-1
5. Lee EY, Caffrey AR. Thrombocytopenia with Tedizolid and Linezolid. Antimicrob Agents Chemother. 2018;62. doi:10.1128/AAC.01453-17
6. Tsuji Y, Holford NHG, Kasai H, et al. Population pharmacokinetics and pharmacodynamics of linezolid-induced thrombocytopenia in hospitalized patients. Br J Clin Pharmacol. 2017;83:1758–1772. doi:10.1111/bcp.13262
7. Nukui Y, Hatakeyama S, Okamoto K, et al. High plasma linezolid concentration and impaired renal function affect development of linezolid-induced thrombocytopenia. J Antimicrob Chemother. 2013;68(9):2128–2133. doi:10.1093/jac/dkt133
8. Gerson SL, Kaplan SL, Bruss JB, et al. Hematologic effects of linezolid: summary of clinical experience. Antimicrob Agents Chemother. 2002;46(8):2723–2726. doi:10.1128/aac.46.8.2723-2726.2002
9. Wu VC, Wang YT, Wang CY, et al. High frequency of linezolid-associated thrombocytopenia and anemia among patients with end-stage renal disease. Clin Infect Dis. 2006;42(1):66–72. doi:10.1086/498509
10. George MR, Creer MH. Advanced platelet parameters: underutilized tools in the diagnosis and management of thrombopoietic states? Transfusion. 2017;57(4):874–875. doi:10.1111/trf.14044
11. Kaito K, Otsubo H, Usui N, et al. Platelet size deviation width, platelet large cell ratio, and mean platelet volume have sufficient sensitivity and specificity in the diagnosis of immune thrombocytopenia. Br J Haematol. 2005;128(5):698–702. doi:10.1111/j.1365-2141.2004.05357.x
12. Numbenjapon T, Mahapo N, Pornvipavee R, et al. A prospective evaluation of normal mean platelet volume in discriminating hyperdestructive thrombocytopenia from hypoproductive thrombocytopenia. Int J Lab Hematol. 2008;30(5):408–414. doi:10.1111/j.1751-553X.2007.00969.x
13. Tang YT, He P, Li YZ, et al. Diagnostic value of platelet indices and bone marrow megakaryocytic parameters in immune thrombocytopenic purpura. Blood Coagul Fibrinolysis. 2017;28(1):83–90. doi:10.1097/mbc.0000000000000612
14. Negash M, Tsegaye A. Diagnostic predictive value of platelet indices for discriminating hypo productive versus immune thrombocytopenia purpura in patients attending a tertiary care teaching hospital in Addis Ababa, Ethiopia. BMC Hematol. 2016;16(1):18. doi:10.1186/s12878-016-0057-5
15. Chen C, Guo DH, Cao X, et al. Risk factors for thrombocytopenia in adult Chinese patients receiving linezolid therapy. Curr Ther Res Clin Exp. 2012;73(6):195–206. doi:10.1016/j.curtheres.2012.07.002
16. Hirano R, Sakamoto Y, Tachibana N, et al. Retrospective analysis of the risk factors for linezolid-induced thrombocytopenia in adult Japanese patients. Int J Clin Pharm. 2014;36(4):795–799. doi:10.1007/s11096-014-9961-6
17. Yang J, Zhou X, Fan X, et al. mTORC1 promotes aging-related venous thrombosis in mice via elevation of platelet volume and activation. Blood. 2016;128(5):615–624. doi:10.1182/blood-2015-10-672964
18. Zhang XH, Wang QM, Zhang JM, et al. Desialylation is associated with apoptosis and phagocytosis of platelets in patients with prolonged isolated thrombocytopenia after allo-HSCT. J Hematol Oncol. 2015;8:116. doi:10.1186/s13045-015-0216-3
19. Li MF, Li XL, Fan KL, et al. Platelet desialylation is a novel mechanism and a therapeutic target in thrombocytopenia during sepsis: an open-label, multicenter, randomized controlled trial. J Hematol Oncol. 2017;10:104. doi:10.1186/s13045-017-0476-1
20. Yilmaz T, Yilmaz A. Relationship between Altered Platelet Morphological Parameters and Retinopathy in Patients with Type 2 Diabetes Mellitus. J Ophthalmol. 2016;2016:9213623. doi:10.1155/2016/9213623
21. Mancuso ME, Santagostino E. Platelets: much more than bricks in a breached wall. Br J Haematol. 2017;178(2):209–219. doi:10.1111/bjh.14653
22. Machlus KR, Italiano JE. The incredible journey: from megakaryocyte development to platelet formation. J Cell Biol. 2013;201(6):785–796. doi:10.1083/jcb.201304054
23. Boak LM, Rayner CR, Grayson ML, et al. Clinical population pharmacokinetics and toxicodynamics of linezolid. Antimicrob Agents Chemother. 2014;58(4):2334–2343. doi:10.1128/AAC.01885-13
24. Natsumoto B, Yokota K, Omata F, et al. Risk factors for linezolid-associated thrombocytopenia in adult patients. Infection. 2014;42(6):1007–1012. doi:10.1007/s15010-014-0674-5
25. Zhang YM, Yu W, Zhou N, et al. High frequency of thrombocytopenia in patients with acute-on-chronic liver failure treated with linezolid. Hepatobiliary Pancreat Dis Int. 2015;14(3):287–292. doi:10.1016/S1499-3872(15)60379-4
26. Choi GW, Lee JY, Chang MJ, et al. Risk factors for linezolid-induced thrombocytopenia in patients without haemato-oncologic diseases. Basic Clin Pharmacol Toxicol. 2019;124(2):228–234. doi:10.1111/bcpt.13123
27. Waki F, Ohnishi H, Shintani T, et al. Linezolid-induced pure red cell aplasia in a patient with Staphylococcus epidermidis infection after allogeneic stem cell transplantation. Transpl Infect Dis. 2012;14(4):E1–6. doi:10.1111/j.1399-3062.2012.00728.x
28. Ebeling F, Helminen P, Anttila VJ. Appearance of ring sideroblasts in bone marrow during linezolid therapy. Scand J Infect Dis. 2009;41(6–7):480–482. doi:10.1080/00365540902971203
29. Bernstein WB, Trotta RF, Rector JT, et al. Mechanisms for linezolid-induced anemia and thrombocytopenia. Ann Pharmacother. 2003;37(4):517–520. doi:10.1345/aph.1C361
30. Cojutti P, Maximova N, Crichiutti G, et al. Pharmacokinetic/pharmacodynamic evaluation of linezolid in hospitalized paediatric patients: a step toward dose optimization by means of therapeutic drug monitoring and Monte Carlo simulation. J Antimicrob Chemother. 2015;70(1):198–206. doi:10.1093/jac/dku337
31. Matsumoto K, Shigemi A, Takeshita A, et al. Analysis of thrombocytopenic effects and population pharmacokinetics of linezolid: a dosage strategy according to the trough concentration target and renal function in adult patients. Int J Antimicrob Agents. 2014;44(3):242–247. doi:10.1016/j.ijantimicag.2014.05.010
32. Lynch J, Wong-Beringer A. Caspofungin: a potential cause of reversible severe thrombocytopenia. Pharmacotherapy. 2004;24(10):1408–1411. doi:10.1592/phco.24.14.1408.43148
33. Hanai Y, Matsuo K, Ogawa M, et al. A retrospective study of the risk factors for linezolid-induced thrombocytopenia and anemia. J Infect Chemother. 2016;22(8):536–542. doi:10.1016/j.jiac.2016.05.003
34. Taubert M, Zoller M, Maier B, et al. Predictors of inadequate linezolid concentrations after standard dosing in critically ill patients. Antimicrob Agents Chemother. 2016;60(9):5254–5261. doi:10.1128/AAC.00356-16
35. Zuo M, Sun Y, Zhao X, et al. Evaluating linezolid dose regimens against methicillin-resistant Staphylococcus aureus based on renal function in populations with different body weight. J Clin Pharm Ther. 2022;30.
36. Thiery-Antier N, Binquet C, Vinault S, et al. Is Thrombocytopenia an Early Prognostic Marker in Septic Shock? Crit Care Med. 2016;44(4):764–772. doi:10.1097/ccm.0000000000001520
37. Mauro P, Andrea A, Passamontiserena M, et al. Hemostasis changes during veno-venous extracorporeal membrane oxygenation for respiratory support in adults. Minerva Anestesiol. 2016;82(2):170–179.
38. Guru Pramod K, Singh Tarun D, Akhoundi A, et al. Association of thrombocytopenia and mortality in critically ill patients on continuous renal replacement therapy. Nephron. 2016;133(3):175–182. doi:10.1159/000447543
39. Rong-Hui D, Li-Rong L, Cheng-Qing Y, et al. Predictors of mortality for patients with severe coronavirus disease infections: a prospective cohort study. Eur Respir J. 2020;55(5). doi:10.1183/13993003.00524-2020
40. Samad G, Nashmil P, Leili P, et al. Prognostic value of platelet indices in patients with acute pulmonary thromboembolism. J Cardiovasc Thorac Res. 2020;12(1):56–62. doi:10.34172/jcvtr.2020.09
41. Ostovan MA, Ghaffari S, Pourafkari L, et al. Modification of simplified pulmonary embolism severity index and its prognostic value in patients with acute pulmonary embolism. Heart Lung Circ. 2016;25(2):184–190. doi:10.1016/j.hlc.2015.08.008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
