Back to Journals » Patient Preference and Adherence » Volume 17
Effect of Multimodal Health Education Combined with the Feedback Method in Perioperative Patients with Lung Cancer: A Randomised Controlled Study
Authors Yuan Z, Gao L, Zheng M, Ye X, Sun S
Received 25 October 2022
Accepted for publication 10 January 2023
Published 16 February 2023 Volume 2023:17 Pages 413—420
DOI https://doi.org/10.2147/PPA.S394826
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Zheng Yuan,1 Lixia Gao,2 Meijie Zheng,3 Xiaobo Ye,4 Sujuan Sun1
1Department of Nursing, Hebei General Hospital, Shijiazhuang, 050000, People’s Republic of China; 2Department of Cardiovascular Medicine for the Elderly, Hebei General Hospital, Shijiazhuang, People’s Republic of China; 3Department of Gastroenterology, Hebei General Hospital, Shijiazhuang, People’s Republic of China; 4Second Department of Thoracic Surgery, Hebei General Hospital, Shijiazhuang, People’s Republic of China
Correspondence: Sujuan Sun, Department of Nursing, Hebei General Hospital, No. 348, Heping West Road, Shijiazhuang, Hebei, People’s Republic of China, Tel +86-311-85988114, Email [email protected]
Objective: To explore the effect of multimodal health education combined with a feedback method in perioperative patients with lung cancer.
Methods: A total of 200 lung cancer patients were divided into the observation group and the control group. The observation group adopted the multimodal health education combined with the feedback method, and the control group adopted the conventional health education model. The postoperative extubation time, length of hospital stay, time to first leaving the bed, postoperative exercise compliance, emotional-distress index and patient satisfaction were compared between the two groups.
Results: The postoperative extubation time (2.80 ± 1.03 days), the emotional-distress index (8.26 ± 3.01) and the time to first leaving the bed (23.74 ± 11.87 h) were all lower in the observation group than in the control group, with a statistically significant difference (P < 0.05). The postoperative exercise compliance (49.69 ± 3.60) and patient satisfaction (98.32 ± 1.66) values were higher in the observation group than in the control group, with statistically significant differences (P < 0.05).
Conclusion: Multimodal health education combined with the feedback method can improve the postoperative exercise compliance of lung cancer patients, reduce their postoperative rehabilitation time and improve their postoperative psychological state and satisfaction, which is in line with the concept of promoting the enhanced recovery of lung cancer patients.
Keywords: lung cancer, enhanced recovery after surgery, feedback method, multimodal health education
Introduction
The number of new cases of lung cancer in 2020 was estimated to be 2.207 million worldwide, ranking second among all malignant tumours, with the mortality rate of lung cancer ranking first in the world.1,2 At present, the treatment of lung cancer involves a multidisciplinary treatment mode based on surgery, with the survival rate for stage I lung cancer with surgical resection approximately 90% or above.3 However, attendant problems are inevitable, including surgical trauma and low postoperative nursing efficiency in the treatment process, which will affect the quality of life of the patients.4 While clinically eligible for discharge, more than half of a sampled population had severe symptoms at discharge following lung cancer surgery.5
In recent years, the concept of enhanced recovery after surgery (ERAS) has been gradually accepted in the field of thoracic surgery.6 The concept of ERAS in nursing mainly includes preoperative health education, preoperative smoking cessation, respiratory function exercise, postoperative analgesia, early ambulation, nutrition management, early removal of the drainage tube and other measures.7–9 Perioperative health education is one of the most important measures of the ERAS concept. However, the effect of routine health education is not good,10 and the feedback method can ensure that patients understand the relevant content, improve their compliance, shorten the average length of hospital stay, reduce the readmission and case fatality rates and improve the rehabilitation effect.11–13 In foreign countries, the feedback method is widely used in the field of health education and has achieved good results.14 Meanwhile, in China, various studies have explored the multimodal and multidisciplinary team health education model, but have not adjusted it in time according to the feedback of the patients.15 In the present study, patients in the control group and those in the observation group are compared to explore the effect of the multimodal health education method combined with the feedback method on the post-surgery rehabilitation of patients with lung cancer. It was hypothesised that compared with the control group, the observation group would exhibit better postoperative rehabilitation.
Data and Methods
Participants
A total of 200 patients admitted for lung cancer surgery in the thoracic surgery department of Hebei Provincial People’s Hospital from July to December 2021 were selected as the study participants. The patients were randomly divided into the control group and the observation group using the random number table method. The inclusion criteria were as follows: ① aged 18–80 years; ② plans for thoracoscopic surgery for lung cancer; ③ patients pathologically confirmed to have lung cancer; ④ patients with complete medical records; ⑤ patients with normal communication and expression ability; ⑥ the patients or their family members gave their informed consent to participate in this study; and ⑦ patients able to use a smartphone. The exclusion criteria included the following: ① perioperative pulmonary infection, respiratory failure and other complications; ② patients with a heart, brain, kidney, liver and/or other organ lesions or functional insufficiency; ③ the pathological results were found in patients with non-malignant tumours; and ④ extubation under an abnormal condition. The study was approved by the Ethics Committee of Hebei Provincial People’s Hospital (batch number:), and all participating patients signed the informed consent form.
Methods
Intervention Method
The control group adopted routine health education methods. Routine health education includes the nurses advising the patients to quit smoking and take respiratory exercises prior to surgery and explaining the attendant precautions during the perioperative period. Following the operation, the patients are routinely given oxygen inhalation, undergo vital sign monitoring and offered guidance and assistance in leaving the bed or turning over, knocking on the back and expectoration. The observation group used the multimodal health education combined with the feedback method, as described below.
The Professional Team
A health education team for the thoracic surgery department was established, including two attending physicians, three nurses, and one rehabilitation physician. The doctors are mainly responsible for explaining the surgical treatment plan and perioperative risks and hidden dangers to patients, while the nurse is largely responsible for the perioperative education work during the patient’s hospitalisation period. The rehabilitation doctors are responsible for the respiratory function exercise during hospitalisation, mainly for patients with relatively poor preoperative lung function and patients with relatively complicated surgery. Prior to the intervention, the members of the health education team should be trained according to the implementation process, paying attention to the feedback method, such that they can master the relevant lung cancer knowledge and skilfully use the feedback method to educate the patients.16 During the whole process, regular seminars are held to record the problems found in the process of health education and to propose effective solutions to ensure the unity and scientific nature of health education.
Health Education Materials and Process
Based on the Clinical Practice Guidelines for ERAS in China (2021 edition)17 and the high-frequency problems of clinical lung cancer patients, the Manual of Rapid Rehabilitation of Thoracic Surgery was compiled. Medical, nursing, anaesthesia, rehabilitation and other experts were then invited to discuss and revise the manual. The manual uses plain language, illustrations, red marks and other methods to emphasise key points to help lung cancer patients understand and memorise the relevant knowledge. The main contents include the following: ① admission education, including department environment introduction, introduction to the doctor in charge and the responsible nurse, precautions for laboratory examination, safety education and individualised guidance; ② preoperative education, including patient preparation, substance preparation, preoperative evaluation content, respiratory function exercise, the use of incentive spirometry, limb function exercise, postoperative bed arrangement, postoperative coordination points and postoperative symptom management; ③ postoperative education, including body posture, pain management, early getting out of bed, airway management, nutrition and diet management, pipeline management and pulmonary embolism prevention; and ④ discharge guidance, including lung function exercises, reasonable diets, incision management, drug guidance and follow-up guidance. Here, following admission, each patient was issued a copy of the manual to facilitate the learning of the relevant content.
A perioperative health education video for thoracic surgery was also created. The contents included the following: publicity and education of admission rules and regulations, preoperative preparation, postoperative precautions education, respiratory function exercise, upper limb function exercise, lower limb function exercise, the method of tapping the back and sputum discharge, carrying out chest-tube precautions and discharge guidance. The video was converted into QR code before being placed in the ward, where patients can easily use a mobile phone for WeChat scanning, with the QR code sent to the department’s patient WeChat group and the responsible nurse providing guidance for the viewing method following the patient’s admission.
Implementation Process for Multimodal Health Education Combined with the Feedback Method
The nurses adopt a combination of group education and one-to-one individualised education during the patient’s hospitalisation. Based on the health education process of thoracic surgery, group education is first conducted in the form of PowerPoint and video presentations before individual one-to-one education is provided. Here, the nurse used concise and understandable Mandarin during the instruction process. Following the guidance, the patient’s acceptance was assessed before they were encouraged to conduct language repetition and action demonstrations, with the nurse evaluating the patient’s performance immediately. During the evaluation, the nurse should question the patient using a soft tone, with the patient encouraged when giving the correct answer. When answering incorrectly, the nurse should attempt to identify the reason for the error, explain the issue clearly and give further guidance until the patient can correctly repeat the language and demonstrate accurate actions. In addition, the nurse should record the time, the patient’s name and hospital number, the education theme, specific content, the retelling results and any notes during each education session.
Evaluation Method
Information Collection
The information pertaining to medical history, living habits, age and gender was collected. In the case of no statistical difference between the two groups, the groups were deemed as comparable.
The postoperative recovery was also recorded for both groups, including in terms of extubation time, the time to first leaving the bed and the total length of the hospital stay.
Postoperative Exercise Compliance Scale for Lung Cancer Patients
This scale includes 15 entries, each of which involves a 5-level scoring method, from “completely possible” to “completely impossible”. Each component can receive a score of 0–4, with a total possible score of 0–60 points. A higher score indicates better adherence to functional exercise.18
Huaxi Emotional-Distress Index
This scale includes 11 items and four dimensions: depression, anxiety, acute symptoms and suicide factors, with a 5-level score of 0–4 (from “none” to “full time”) and a possible total score of 36 points. All patients must be evaluated in terms of each of the first nine items. If the total score for the first nine items is >8 points, items 10 and 11 will then be evaluated, otherwise, the evaluation will be concluded. A score of <9 indicates no recent bad mood, 9–12 indicates a mildly bad mood, 13–16 indicates a moderately bad mood and >16 indicates a severe bad mood.19
Nursing Satisfaction Score
The satisfaction with the nursing work was compared between the two groups, with a patient satisfaction questionnaire completed on the day before discharge. The questionnaire included 10 items, with 10 points given for highly satisfied, 8 points for satisfied, 5 points for moderately satisfied and 0 points for dissatisfied; the total possible score is 100 points.
Sample Size Calculation
In this study, the estimated length of stay in the control group was 9.84 ± 3.28 days, and that of the observation group was expected to decrease by 1.6 days. The sample size was calculated according to the following formula:
where N represents the sample size of each group, α is 0.05 and the Z value is bilateral. Here, Zα = 1.96, β was unilateral and the study’s grasp level (test efficiency) was 0.9, Zβ = 1.28. Meanwhile, σ represents the standard deviation, which in this study was 3.28, δ represents the difference between the average value of the observation group and the control group. In this study, δ =1.6.
The final calculation indicated that the sample size of each group was 88. Considering the expected 20% loss rate, it was ultimately determined that 110 participants should be included in each group.
Statistical Methods
The statistical analysis was performed using SPSS26.0 statistical software. The measurement data meeting the normal distribution were expressed in terms of mean ± standard deviation ( ), with inter-group comparisons performed using a t-test. The continuous data following non-normal distribution were counted using the Kruskal–Wallis test, with the count data represented by cases (%) and the inter-group comparisons performed using the chi-square test. The test level was α =0.05, and the difference was significant when P ≤ 0.05.
), with inter-group comparisons performed using a t-test. The continuous data following non-normal distribution were counted using the Kruskal–Wallis test, with the count data represented by cases (%) and the inter-group comparisons performed using the chi-square test. The test level was α =0.05, and the difference was significant when P ≤ 0.05.
Results
Clinical Data of the Lung Cancer Patients
To ensure that the two groups were comparable, the information pertaining to medical history, living habits, age and gender was collected. There were no differences in terms of any of the above variables between the two groups. A total of 100 lung cancer patients admitted to the hospital from July to September 2021 were selected as the controls, with 32 males and 68 females and a mean age of 58.18 ± 10.58 years. Thirty-five of these patients had a history of smoking, four had preoperative coronary heart disease, 21 had hypertension, and 10 had diabetes. A total of 100 lung cancer patients admitted to the hospital from October to December 2021 were selected as the observation group, with 39 males and 61 females and a mean age of 56.71 ± 10.34 years. Among them, 40 patients had a smoking history, four had preoperative coronary heart disease, 37 had hypertension and 15 had diabetes. There was no significant difference in the general clinical data between the two groups (P > 0.05) (Table 1).
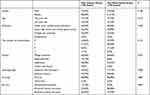 |
Table 1 General Clinical Data of Lung Cancer Patients |
Comparison of Postoperative Recovery Between the Two Groups
In this study, to evaluate the recovery of the lung cancer patients in the two groups, the postoperative extubation time, time to first leaving the bed, length of hospital stay, postoperative exercise compliance, emotional-distress index and level of satisfaction were compared between the two groups. The postoperative extubation time was significantly lower in the observation group (2.80 ± 1.03 days) than in the control group (3.41 ± 2.09 days), with a statistically significant difference (P < 0.05). The time to first leaving the bed was 31.22 ± 16.22 h in the control group and 23.74 ± 11.87 h in the observation group, with the time significantly less in the latter at a statistically significant difference (P < 0.05). The length of hospital stay was 10.44 ± 5.29 days in the control group and 9.35 ± 3.74 days in the observation group, indicating no significant difference between the two groups (P > 0.05). The postoperative exercise compliance was significantly higher in the observation group (49.69 ± 3.60) than in the control group (43.26 ± 5.02), with the difference statistically significant (P < 0.05). The emotional-distress index was 9.49 ± 3.69 in the control group but was significantly lower in the observation group (8.26 ± 3.01), with the difference statistically significant (P < 0.05). The patient satisfaction was significantly higher in the observation group (98.32 ± 1.66) than in the control group (94.48 ± 2.6), with the difference statistically significant (P < 0.05). Overall, the recovery was clearly better in the observation group (Table 2). No adverse events occurred in this study.
 |
Table 2 Comparison of Postoperative Recovery Between the Two Lung Cancer Groups |
Discussion
In this study, the postoperative extubation time, the emotional-distress index values and the time to first leaving the bed were all lower in the observation group than in the control group, with a statistically significant difference. The postoperative exercise compliance and patient satisfaction were higher in the observation group than in the control group, with statistically significant differences.
The feedback method involves the patient receiving health education from the medical staff, after which the patient uses their own language to repeat or demonstrate the understood health-related knowledge.20 This creates opportunities for healthcare workers to further understand the extent of the patient’s understanding of the relevant education information. If the patient has an inaccurate understanding of the education information, the medical staff can explain and re-evaluate it repeatedly to ensure that the patient masters a variety of perioperative health knowledge such that it can be effectively transmitted. The feedback method is an easily understood, valuable and feasible method of health education. Various researchers, including Zhang Huazhi,21 have demonstrated that surgical treatment can result in massive trauma for lung cancer patients, while postoperative pain and complications lead to poor compliance and slow recovery. Elsewhere, Yang et al22 demonstrated that lung cancer patients not only suffer from pain in the perioperative period but often experience a series of psychological problems, such as fear and anxiety, which will seriously affect their physical and mental health, as well as their perioperative recovery.
The present study thus focused not only on the postoperative physical condition of lung cancer patients, but also on the patient’s psychological recovery following surgery. Therefore, a health education team for thoracic surgery was formed, which included two attending physicians, three nurses and one rehabilitation physician. Health education was then provided in the form of video presentations, presenting an exploration of the multidisciplinary health education for patients undergoing surgery for lung cancer.
In this study, the observation group adopted the multimodal health education combined with the feedback method. The results indicated that the postoperative exercise compliance of the lung cancer patients was higher in the observation group than in the control group, while the extubation time and the time to first leaving the bed were shorter in the observation group than in the control group, indicating that the multimodal health education method could improve the postoperative exercise compliance of lung cancer patients and shorten their postoperative recovery time. These findings were similar to those obtained by Huang et al.23
Medical staff conduct multimodal health education for patients and use the feedback method to professionally evaluate the patient’s level of mastery of the relevant perioperative health education knowledge before conducting repeated education to ensure that the patient is familiar with the perioperative precautions, increasing their confidence and compliance and ensuring that they cooperate with the doctors as effectively as possible during the treatment. With the guidance and companionship of the nursing staff, the patient may immediately take the initiative in undertaking ankle pump exercises, effectively coughing after waking or leaving the bed as soon as possible following the doctor’s advice. This will promote the elimination of the patient’s sputum and will discharge the drainage fluid after removing the drainage tube as soon as possible, promoting timely pulmonary re-expansion.
In this study, during the whole perioperative period, the medical staff would encourage and comfort the patients, ensuring that they feel cared for, thus reducing the occurrence of psychological problems, such as perioperative depression and anxiety, and improving the satisfaction with the medical treatment. These findings are consistent with those obtained by Chen.24
However, the length of hospital stay was not significantly different across the two groups, which is not consistent with the results obtained in most studies.15 This may be related to the degree of surgical trauma, the patient’s tolerance to anaesthesia and/or pain and other factors. Therefore, it is crucial that multiple teams closely cooperate to minimise the surgical trauma and optimise the anaesthesia, postoperative pain and airway management in view of accelerating the rehabilitation of lung cancer patients.
To sum up, the implementation of multimodal health education combined with the feedback method for perioperative patients with lung cancer can significantly improve the postoperative exercise compliance, reduce the postoperative rehabilitation time, improve the postoperative psychological state of the patients, enhance the patient’s satisfaction, ensure the patients’ rapid recovery and provide a theoretical and scientific basis for the application of the ERAS concept during the clinical perioperative period.
This study involves a number of limitations. First, the scalability of this study may be limited due to the small sample size. Furthermore, due to the small number of observation indicators and the lack of certain indicators, such as lung function, further high-quality studies and a large sample are needed to validate the observed benefits.
Conclusion
Multimodal health education combined with the feedback method may improve the postoperative exercise compliance, reduce the postoperative rehabilitation time, improve the postoperative psychological state and enhance lung cancer patients’ satisfaction with the treatment/care, of all which are in line with the concept of promoting the enhanced recovery of such patients.
Data Sharing Statement
All data generated or analyzed during this study are included in this article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hebei General Hospital. Written informed consent was obtained from all participants.
Funding
There is no funding to report.
Disclosure
All authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Siegel RL, Miler KD, Jemal A. Cancer statistics 2015. CA Cancer J Clin. 2015;65(1):5–29. doi:10.3322/caac.21254
2. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;713:209–249. doi:10.3322/caac.21660
3. Wu MC, Wu ZD, Wu ZH. Surgery.
4. Cai QX, Zhang LJ, Zhu WW. Multidisciplinary enhanced recovery after surgery in video-assisted thoracoscopic surgery for lung cancer. J Nurs Sci. 2018;33(19):31–34.
5. Liao J, Wang Y, Dai W, et al. Profiling symptom burden and its influencing factors at discharge for patients undergoing lung cancer surgery: a cross-sectional analysis. J Cardiothorac Surg. 2022;17(1):229. doi:10.1186/s13019-022-01974-9
6. Nelson DB, Mehran RJ, Mena GE, et al. Enhanced recovery after surgery improves postdischarge recovery after pulmonary lobectomy. J Thorac Cardiovasc Surg. 2022. doi:10.1016/j.jtcvs.2022.09.064
7. Coughlin SM, Emmerton-Coughlin HMA, Malthaner R. Management of chest tubes after pulmonary resection: a system- atic review and meta analysis. Can J Surg. 2012;55(4):264–270. doi:10.1503/cjs.001411
8. Alessandro G, Domenico V, Luca V, et al. Enhanced recovery after surgery and video-assisted thoracic surgery lobecto- my: the Italian VATS Group surgical protocol. J Thorac Dis. 2018;10(Suppl 4):S564–S570. doi:10.21037/jtd.2018.01.157
9. Marzia U, Stefano F, Matteo S, et al. Anesthesia and fast-track in video- assisted thoracic surgery (VATS): from evidence to practice. J Thorac Dis. 2018;10(Suppl 4):S542–S554. doi:10.21037/jtd.2017.12.83
10. Pan CL, Zhang S, Zhang ZR. Application of teach-back method in nursing health education. J Nurs Sci. 2016;31(14):110–112.
11. Kemp EC, Floyd MR, Mccord-Duncan E, Lang F. Patients prefer the method of “tell back-collaborative inquiry” to assess understanding of medical information. J Am Board Fam Med. 2008;21(1):24–30. doi:10.3122/jabfm.2008.01.070093
12. National Quality Forum (NQF). Safe practices for better healthcare-2010 update: a consensus report[EB/OL]. (2010-04)[2016-02-03]. Available from: https://www.qualityfo-rum.org/Publications/2010/04/SafePractices_10_A-bridged.Aspx.
13. Peter D, Robinson P, Jordan M, Lawrence S, Casey K, Salas-Lopez D. Reducing readmissions using teach-back: enhancing patient and family education. J Nurs Adm. 2015;45(1):35–42. doi:10.1097/NNA.0000000000000155
14. Parsons LC, Revell MA. Orthopedic injuries: protocols to prevent and manage patient falls. Nurs Clin North Am. 2015;50(4):645–666. doi:10.1016/j.cnur.2015.07.007
15. Cui LM, Cui YM, Su QZ, et al. Application of multidisciplinary team cooperation nursing mode in lung cancer patients undergoing surgery. Qilu J Nurs. 2019;25(24):19–22.
16. Wilson FL, Baker LM, Nordstrom CK, Legwand C. Using the teach-back and Orem’s self-care deficit nursing theory to increase childhood immunization communication among low-income mothers. Issues Compr Pediatr Nurs. 2008;31(1):7–22. doi:10.1080/01460860701877142
17. Cao H, Chen YJ, Gu XP. Clinical practice guidelines for enhanced recovery after surgery in China (Version 2021). Chin J Pract Surg. 2021;41(9):961–992.
18. Qiu PP, Kang MQ, Li W. The correlation study of rehabilitation exercise compliance and fatigue and pain after lung cancer surgery. J Nurs Sci. 2014;29(02):21–23. doi:10.3870/hlxzz.2014.02.021
19. Liu SS, Zheng RJ, Li JY, Yu CH. Application of HEI in psychological status measurement of nurses in oncology department. Sichuan Med J. 2017;38(11):1330–1335. doi:10.16252/j.cnki.issn1004-0501-2017.11.029
20. Agency for Healthcare Research and Quality. AHRQ Health literacy Universal Precautions Toolkit.
21. Zhang HZ, Guo XY, Li XS, et al. Etiological characteristics of postoperative pulmonary infections in lung cancer patients and influencing factors. Chin J Nosocomiol. 2018;28(1):77–80.
22. Yang J, Chu X, Jin SQ. Effect of Newman comprehensive model of psychological nursing on quality of life and self efficacy in patients with NSCLS negative mood. China J Health Psychol. 2019;27(8):1156–1158.
23. Huang L, Wang XX, Zhang J. Effects of teach back method on the compliance of respiratory function exercise in esophageal cancer patients underwent thoracic surgery. Chin J Nurs. 2016;51(1):26–28. doi:10.3761/j.issn.0254-1769.2016.01.005
24. Chen C. Application of multidisciplinary team cooperation nursing model in lung cancer surgery patients. Chin Med Guide. 2022;20(13):123–126. doi:10.15912/j.cnki.gocm.2022.13.015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.