Back to Journals » Journal of Pain Research » Volume 12
Effect of ketorolac in intra-articular injection analgesia for postoperative pain in patients undergoing shoulder arthroscopy: a pilot-controlled clinical study
Authors Xu J, Qu Y, Li H, Jiang T, Zheng C, Wang B, Shen P
Received 28 June 2018
Accepted for publication 23 August 2018
Published 17 January 2019 Volume 2019:12 Pages 417—422
DOI https://doi.org/10.2147/JPR.S178413
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael A Ueberall
Jianda Xu,1,* Yuxing Qu,1 Huan Li,2 Tao Jiang,1,* Chong Zheng,1 Bin Wang,1 Pengfei Shen1
1Department of Orthopaedics, Changzhou Traditional Chinese Medical Hospital, Changzhou, Jiangsu 213003, China; 2Department of Arthroplasty, The First People’s Hospital of Changzhou, Changzhou, Jiangsu 213003, China
*These authors contributed equally to this work
Background: To date, a regional approach using local anesthetics has become a popular analgesic method for arthroscopy. The optimal postoperative analgesia method for shoulder arthroscopy is still debated.
Objective: This study was designed to evaluate the effect and safety of using ketorolac in combination with a multimodal drug regime (ropivacaine, morphine, and triamcinolone acetonide) after shoulder arthroscopy.
Methods: A total of 60 patients were included in a pilot study and patients were randomized into an experimental group (n=30) and a control group (n=30). The following parameters were used to evaluate pain relief levels postoperatively: the Visual Analog Scale (VAS) at 1, 3, 6, 12, 24, and 48 hours postoperatively, morphine consumption, and initial analgesic desired time. Complications were also recorded.
Results: Except for 1 hour postoperatively, patients in the experimental group experienced lower VAS scores during the first 48 hours postoperatively (P<0.05). The VAS score in both groups increased after 3 hours postoperatively and peaked at 12 hours postoperatively (2.54±0.86 vs 3.25±1.18). The VAS scores on movement in the experimental group were lower than those in the control group at 24 or 48 hours postoperatively (P=0.004, 0.001). A total of 18 (60.0%) patients in the experimental group required no additional analgesia, compared with 10 (33.3 %) in the control group (P=0.035). The mean rescue analgesia was 11.40±5.56 mg in the experiment group, while 16.57±8.48 mg in the control group (P=0.016). The initial analgesic desired time was delayed significantly in the experimental group (16.50±14.57 hours vs 8.9±6.32 hours, P=0.000).
Conclusion: Adding ketorolac to intra-articular injection analgesia is a safe and effective method to improve pain relief after shoulder arthroscopy, and further prospective controlled trials are necessary to allow definite treatment recommendations.
Keywords: ketorolac, intra-articular injection analgesia, postoperative pain, shoulder arthroscopy
Introduction
Shoulder arthroscopy is a common practice in managing shoulder diseases (such as rotator cuff tear, subacromial bursitis, and glenoid labial tear). About 45% of patients have severe pain postoperatively, which results in undue discomfort and delayed discharge.1
There are many different analgesia methods (including intramuscular injections, intravenous injections, nerve blocks, and intra-articular analgesia) used in controlling pain. The optimal postoperative analgesia method for shoulder arthroscopy is still debated. In the last decade, a regional approach (intraoperative infiltration and intra-articular injection) using local anesthetics has become a popular analgesic method for shoulder arthroscopy. Stein et al reported the effectiveness and safety of intra-articular morphine after arthroscopic knee surgery, which is explained by the presence of opiate receptors in the nerve endings anchored to the inflamed synovial tissue.2 Levine and Taiwo confirmed the same result and reported that morphine had a mild but definite analgesic effect via a binding site with the characteristics of the mu-opioid receptor.3 Compared with hyaluronic acid and saline, triamcinolone acetonide produced a faster reduction in pain after injection.4 Panigrahi et al studied the analgesic effect of dexamethasone with ropivacaine, and confirmed that the combined intra-articular group had significantly low pain scores.5 Therefore, a multimodal drug regime (ropivacaine, morphine, and triamcinolone acetonide) is regularly used after shoulder arthroscopy in our clinics.
To the best of our knowledge, there has been little research concerning the use of nonsteroidal antiinflammatory drugs (NSAIDs) in the intra-articular injection mixture. We hypothesized that adding an intra-articular ketorolac injection would produce more profound pain relief, which could alter the sensitivity of the peripheral nociceptors activated by the trauma of surgery. The primary aim of this study was to evaluate the effect of using ketorolac in combination with a multimodal drug regime (ropivacaine, morphine, and triamcinolone acetonide) after shoulder arthroscopy. Morphine consumption and initial analgesic desired time were measured as secondary end points. Finally, we investigated the safety of an intra-articular ketorolac injection.
Methods
The pilot controlled clinical trial (double-blind study) was designed and approved by the Ethics Review Committee of Changzhou Traditional Chinese Medical Hospital, affiliated to Nanjing University of Traditional Chinese Medicine. Written informed consent was obtained.
From April 2015 to July 2017, 60 patients, American Society of Anesthesiologists (ASA) I–III, aged 39–63 (average 52.5±7.9) years were enrolled in this pilot study. All the patients (37 females and 23 males) were recommended to undergo shoulder arthroscopy and received patient-controlled intravenous analgesia postoperatively. They were randomized to an experimental group and a control group (n=30 each) using a random number table. Patients were excluded if they had inflammatory shoulder arthritis, if they demonstrated alcohol or drug abuse, if they were undergoing chronic treatment with NSAIDs or steroid medication, or if they had severe neurologic or psychiatric diseases that made them difficult to participate in the study.
The baseline demographics were similar in both groups (Table 1) with respect to age, gender, body mass index (BMI), ASA, height, duration of surgery, side of surgery, and preoperative Visual Analog Scale (VAS). None of the patients required analgesia therapy in the post-anesthesia care unit.
  | Table 1 The baseline characteristics of all enrolled 60 patients Abbreviations: ASA, American Society of Anesthesiologist; BMI, body mass index; VAS, Visual Analog Scale. |
All patients received general anesthesia. The surgeries were performed by one senior experienced orthopedic surgeon who specializes in arthroscopy. Mobilization started from the second postoperative day and was undertaken by one physiotherapist using the same rehabilitation scheme. On the following days, patients underwent rehabilitation twice a day and performed exercises.
Multimodal analgesic regime
All patients were administered a preemptive oral analgesic regimen of imrecoxib (100 mg, Jiang Su Hengrui Medicine Co. Ltd, Lianyungang, China; 200 mg, peros) within 1 hour preoperatively. When the surgery was finished and after the cleaning solution was removed, intra-articular injection (20 mL) was administered through the incision.
The control group received a 20 mL intra-articular injection of the multimodal drug regime (450 mg of ropivacaine with 5 mg of morphine and 25 mg of triamcinolone acetonide).
The experimental group received a 20 mL intra-articular injection of the multimodal drug treatment containing ketorolac (450 mg of ropivacaine with 5 mg of morphine, 25 mg of triamcinolone acetonide, and 10 mg of ketorolac).
Imrecoxib (100 mg PO twice daily) was administered as a primary analgesic treatment, which was started 12 hours postoperatively until discharge. Morphine was used when analgesia was desired, and narcotic consumption was recorded. Ondansetron was used to treat post-operative nausea and vomiting (PONV).
Study clinical parameters
The follow-up duration was defined as the time between the injection of the drug into the joint and the recording time. The initial analgesic desired time was defined as the time between the injection of the drug into the joint and the first analgesic administration time. Postoperative side-effects and complications (such as nausea and vomiting) were also recorded.
Baseline demographics
The following baseline demographics were evaluated: age, sex, BMI (kg/m2), ASA, side of surgery, preoperative VAS score, and duration of surgery (minutes).
Pain
The postoperative pain relief level was evaluated using morphine consumption, initial analgesic desired time, and the VAS. VAS scores were recorded postoperatively at 1, 3, 6, 12, 24 and 48 hours. The VAS scores at movement were recorded at 24 and 48 hours postoperatively. The enrolled patients were trained to mark their pain level on a 10-cm VAS.6
Statistical analysis
The SPSS statistical package (Version 17.0, SPSS Inc., Chicago, IL, USA) was employed for statistical analyses. The normality of distribution for continuous numeric variables was assessed using the Kolmogorov–Smirnov test. Normally distributed variables are presented as mean with SD, and otherwise, as medians with inter-quartile ranges (95% CI). Student’s t-test was used for normally distributed continuous variables, while other variables were assessed using Pearson’s chi-squared test or Wilcoxon’s rank sum test. P<0.05 was considered to indicate statistical significance.
Results
Pain and rescue analgesic requirement
Except for the first postoperative hour, patients in the experimental group experienced lower VAS scores during the first 48 hours (P<0.05, Table 2). The VAS score in both groups increased after 3 hours postoperatively and peaked at 12 hours postoperatively (2.54±0.86 vs 3.25±1.18, Table 2).
  | Table 2 The VAS scores during 48 hours postoperatively Abbreviation: VAS, Visual Analog Scale. |
The VAS scores at movement in the experimental group were lower compared with the control group at 24 or 48 hours postoperatively (P=0.004, 0.001, Table 2), which meant that combining ketorolac with the multimodal drug regime resulted in more comfort during walking.
A total of 18 (60.0%) patients in the experimental group required no additional analgesia during the first 48 hours post surgery, compared with 10 (33.3 %) in the control group (P=0.035). The mean rescue analgesia was 11.40±5.56 mg in the experimental group and 16.57±8.48 mg in the control group (P=0.016, Table 3). The initial analgesic desired time was delayed significantly in the experimental group (16.50±14.57 hours vs 8.91±6.32 hours, P=0.000, Table 3).
  | Table 3 The rescue analgesia and initial analgesic desired time 48 hours postoperatively |
Postoperative complications
The incidence of PONV was low overall (Table 4). No other obvious side effects or complications related to the addition of ketorolac were found.
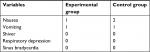  | Table 4 Complications found during 48 hours postoperatively |
Discussion
Our findings confirmed that combining ketorolac with a multimodal drug regime produced more pain relief during the first 48 hours after surgery. Adding ketorolac resulted in a significant reduction in morphine consumption in the first 48 hours postoperatively. The initial analgesic desired time in the experimental group was also prolonged.
Postoperative pain
Effective postoperative pain relief permits earlier mobility and rehabilitation. Multimodal pain therapy is recommended as a sufficient analgesia, which increases the analgesic effect and duration. The rationale for this therapy is to maximize the additive or synergistic effects of different analgesics, but reduce concomitant side effects.7
Preemptive oral analgesia usually results in a lower intensity and duration of afferent noxious stimuli, which minimizes the pain impulses from the surgical wound to the dorsal horn. In addition, it reduces secondary hyperalgesia by producing a lower threshold of dorsal root neurons and decreased receptive fields. We have previously assessed the effects of preemptive analgesia in total knee arthroplasty and confirmed that preemptive analgesia could improve analgesia, reduce inflammatory reactions, and accelerate functional recovery.8
A systematic review concluded that morphine could reduce postoperative pain scores and analgesic consumption. Jaureguito et al reported that the efficacy and duration of action of intra-articular morphine depends on the dose.9 Denti et al reported that the combination of bupivacaine and morphine resulted in better pain relief in patients with anterior cruciate ligament reconstruction, and preemptive analgesia was better than postoperative anesthetic administration.10 Intra-articular injection of corticosteroids is a major conservative treatment. The peak analgesic effect starts at 12 hours postoperatively. Stein et al suggested that the inflammatory response usually disrupts the number and activation of opioid receptors present on sensory nerve terminals and reduces the analgesic effect. However, these changes are reversed within several hours.11 The reactive hyperemia of ischemia was found in inflamed synovial tissue, which could be reduced by triamcinolone acetonide. The pharmacokinetics of the analgesic drugs may explain the time of the maximum synergistic effect in the present results.
The main analgesic mechanism of NSAIDs is a peripheral rather than central mechanism, and increasing local NSAID concentrations may be beneficial. An intra-articular injection of ketorolac has shown promising pain reduction after arthroscopy.
Arthroscopic therapy usually activates the cyclooxygenase enzyme system and prostaglandin synthesis in inflamed synovial tissue. The inflamed tissues usually hinder opioid-mediated analgesia and reduce patient comfort.12 As an NSAID, ketorolac can effectively inhibit the synthesis process, and alter the local concentration and sensitivity of peripheral nociceptors, and control pain scores.13 Gupta et al reported on the synergistic analgesic effect of ketorolac and morphine in local intra-articular analgesia.14 Lashbrook et al established an experimental rat model of neuropathic pain and demonstrated the synergistic antiallodynic effects of opiates combined with ketorolac.15 They also found that prostanoids were produced via both the COX1 and COX2 pathways.15 Intra-articular ketorolac reduced the inflammation in synovial tissue after surgical trauma and produced an additive analgesic effect in combination with morphine. Intra-articular ketorolac injection produced better patient comfort, especially when combined with bupivacaine, ropivacaine, and morphine. The current study demonstrated lower VAS scores in the experimental group. Including ketorolac resulted in reduced morphine consumption and a prolonged initial analgesic desired time.
Dosage and volume of intra-articular injections
Different regimes have been used for intra-articular injection at the end of arthroscopic procedures. To date, no conclusive results concerning dosage and volume have been established.
Raja et al reported that 3 mg of morphine in a 20 mL volume produced no obvious analgesic effect in patients following arthroscopic knee surgery.16 However, Joshi et al found that the administration of 5 mg of morphine in a 45mL volume produced excellent local analgesia.17 De Andrés et al concluded that the combination of morphine and bupivacaine in a volume of 20 mL was preferable to bupivacaine or morphine alone, although it produced a similar analgesic effect.18
Considering the volume of the shoulder and our own experience, we chose a multimodal drug regime in a 20 mL volume.
Side effects and safety
There have been some concerns about the use of intra-articular ketorolac injections. In the present study, no serious complications were observed, although the limited patient numbers provided an insufficient study power to conclusively confirm the safety of the treatment.
To the best of our knowledge, no studies of intra-articular ketorolac injections found an increased incidence of complications. Gupta et al suggested that intra-articular ketorolac injection was a safe choice and provided a better local analgesia rather than systemic effects.14 Andersen et al confirmed that adding ketorolac to a local infiltration analgesic did not increase the incidence of infection or delayed wound healing, and pain intensity and morphine consumption were reduced significantly.19
Some animal studies have also confirmed the safety of intra-articular ketorolac. Reggin et al assessed the safety of intra-articular NSAID injection through histological and mechanical analyses in rat models and concluded that no detrimental mechanical, histological, or functional changes were found.20 Dogan et al used 30 rabbit hind knee joints to assess the effects of ketorolac and morphine on articular cartilage and synovial membrane. They concluded that more histopathological changes were found in the ketorolac and morphine groups after 48 hours and 10 days, but morphine and ketorolac could be safely used intra-articularly.21 NSAIDs help diminish catabolism in human osteoarthritic cartilage, which results in fewer histopathological changes and less cartilage damage.22
Limitations of the study
The sample size in the current study was relatively small, although the study did successfully illustrate the benefits of including ketorolac in a multimodal therapy. Long-term functional outcomes were not assessed, including the long-term side effects of intra-articular therapy. Therefore, further studies are needed.
Conclusion
The current study shows that the combination of ketorolac and a multimodal drug regime (ropivacaine, morphine, and triamcinolone acetonide) leads to improved post-surgical pain scores, but further prospective controlled trials are necessary to allow for definite treatment recommendations.
Disclosure
The authors report no conflicts of interest in this work.
References
de Mulder K, Petré D, Declercq G. Arthroscopy of the shoulder. Current concepts review. Acta Orthop Belg. 1999;65(4):447–457. | ||
Stein C, Comisel K, Haimerl E, et al. Analgesic effect of intraarticular morphine after arthroscopic knee surgery. N Engl J Med. 1991;325(16):1123–1126. | ||
Levine JD, Taiwo YO. Involvement of the mu-opiate receptor in peripheral analgesia. Neuroscience. 1989;32(3):571–575. | ||
Penning LI, de Bie RA, Walenkamp GH. Subacromial triamcinolone acetonide, hyaluronic acid and saline injections for shoulder pain an RCT investigating the effectiveness in the first days. BMC Musculoskelet Disord. 2014;15:352. | ||
Panigrahi R, Mahapatra AK, Priyadarshi A, Palo N, Das DS, Biswal MR. Intraarticular analgesics following shoulder arthroscopy: comparison of ropivacaine/dexamethasone with ropivacaine. J Evol Med Dent Sci. 2015;04(06):946–952. | ||
Stubbs DF. Visual analogue scales. Br J Clin Pharmacol. 1979;7(1):124. | ||
Kehlet H, Dahl JB. The value of “Multimodal” or “Balanced Analgesia” in postoperative pain treatment. Anesth Analg. 1993;77(5):1048–1056. | ||
Jianda X, Yuxing Q, Yi G, Hong Z, Libo P, Jianning Z. Impact of preemptive analgesia on inflammatory responses and rehabilitation after primary total knee arthroplasty: a controlled clinical study. Sci Rep. 2016;6(1):30354. | ||
Jaureguito JW, Wilcox JF, Cohn SJ, Thisted RA, Reider B. A comparison of intraarticular morphine and bupivacaine for pain control after outpatient knee arthroscopy. A prospective, randomized, double-blinded study. Am J Sports Med. 1995;23:350–353. | ||
Denti M, Randelli P, Bigoni M, Vitale G, Marino MR, Fraschini N. Pre- and postoperative intra-articular analgesia for arthroscopic surgery of the knee and arthroscopy-assisted anterior cruciate ligament reconstruction. A double-blind randomized, prospective study. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):206–212. | ||
Stein C, Hassan AH, Przewlocki R, Gramsch C, Peter K, Herz A. Opioids from immunocytes interact with receptors on sensory nerves to inhibit nociception in inflammation. Proc Natl Acad Sci USA. 1990;87(15):5935–5939. | ||
Stein C, Pflüger M, Yassouridis A, et al. No tolerance to peripheral morphine analgesia in presence of opioid expression in inflamed synovia. J Clin Investig. 1996;98(3):793–799. | ||
Reuben SS, Connelly NR. Postoperative analgesia for outpatient arthroscopic knee surgery with intraarticular bupivacaine and ketorolac. Anesth Analg. 1995;80(6):1154–1157. | ||
Gupta A, Axelsson K, Allvin R, et al. Postoperative pain following knee arthroscopy: the effects of intra-articular ketorolac and/or morphine. Reg Anesth Pain Med. 1999;24(3):225–230. | ||
Lashbrook JM, Ossipov MH, Hunter JC, Raffa RB, Tallarida RJ, Porreca F. Synergistic antiallodynic effects of spinal morphine with ketorolac and selective COX1- and COX2-inhibitors in nerve-injured rats. Pain. 1999;82(1):65–72. | ||
Raja SN, Dickstein RE, Johnson CA. Comparison of postoperative analgesic effects of intraarticular bupivacaine and morphine following arthroscopic knee surgery. Anesthesiology. 1992;77(6):1143–1147. | ||
Joshi GP, McCarroll SM, Brady OH, Hurson BJ, Walsh G. Intra-articular morphine for pain relief after anterior cruciate ligament repair. Br J Anaesth. 1993;70(1):87–88. | ||
de Andrés J, Valía JC, Barrera L, Colomina R. Intra-articular analgesia after arthroscopic knee surgery: comparison of three different regimens. Eur J Anaesthesiol. 1998;15(1):10–15. | ||
Andersen KV, Nikolajsen L, Haraldsted V, Odgaard A, Søballe K. Local infiltration analgesia for total knee arthroplasty: should ketorolac be added? Br J Anaesth. 2013;111(2):242–248. | ||
Riggin CN, Tucker JJ, Soslowsky LJ, Kuntz AF. Intra-articular tibiofemoral injection of a nonsteroidal anti-inflammatory drug has no detrimental effects on joint mechanics in a rat model. J Orthop Res. 2014;32(11):1512–1519. | ||
Dogan N, Erdem AF, Gundogdu C, Kursad H, Kizilkaya M. The effects of ketorolac and morphine on articular cartilage and synovium in the rabbit knee joint. Can J Physiol Pharmacol. 2004;82(7):502–505. | ||
Vignon E, Mathieu P, Louisot P, Richard M. In vitro effect of nonsteroidal antiinflammatory drugs on proteoglycanase and collagenase activity in human osteoarthritic cartilage. Arthritis Rheum. 1991;34(10):1332–1335. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
