Back to Journals » International Journal of General Medicine » Volume 15
Effect of Insulin Injection Techniques on Glycemic Control Among Patients with Diabetes
Authors Abujbara M , Khreisat EA, Khader Y , Ajlouni KM
Received 15 October 2022
Accepted for publication 7 December 2022
Published 15 December 2022 Volume 2022:15 Pages 8593—8602
DOI https://doi.org/10.2147/IJGM.S393597
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mousa Abujbara,1 Eiman A Khreisat,2 Yousef Khader,3 Kamel M Ajlouni4
1Department of Diabetes and Endocrinology, the National Centre (Institute) for Diabetes, Endocrinology and Genetics/The University of Jordan, Amman, Jordan; 2Department of Nursing, the National Centre (Institute) for Diabetes, Endocrinology and Genetics/The University of Jordan, Amman, Jordan; 3Department of Community Medicine, Jordan University of Science and Technology (JUST), Irbid, Jordan; 4Department of Endocrinology and Diabetes, the National Centre (Institute) for Diabetes, Endocrinology and Genetics/The University of Jordan, Amman, Jordan
Correspondence: Kamel M Ajlouni, Department of Endocrinology and Diabetes, the National Centre (Institute) for Diabetes, Endocrinology and Genetics/The University of Jordan, Amman, Jordan, Email [email protected]
Objective: Previous studies have shown that healthcare professionals rarely instruct patients about proper insulin injection techniques. This study aimed to assess the practices of insulin injection techniques among patients with diabetes treated and assess the effect of these practices on glycemic control.
Patients and Methods: This cross-sectional study was conducted between November 2020 and February 2021. A random systematic sampling technique was used to recruit study subjects at specialist outpatient clinics. Subjects with type 1 or 2 diabetes mellitus who had been using insulin injections for at least a year were included in this study.
Results: A total of 298 subjects with type 1 diabetes and 553 with type 2 diabetes participated in this study. The mean age of patients with type 1 diabetes was 20.1 ± 10.4 years. The mean age of patients with type 2 diabetes was 58.6 ± 9.5 years. The median type 1 diabetes duration was 6.0 years, and median type 2 diabetes duration was 15.0 years. About 66.8% of patients with type 1 diabetes and 69.4% of patients with type 2 diabetes were rotating insulin injection sites. Almost 36.6% of patients with type 1 diabetes and 50.5% of patients with type 2 diabetes reported using the same insulin needle more than three times. The prevalence of lipohypertrophy was 57.0% among patients with type 1 diabetes and 55.5% among patients with type 2 diabetes. The absence of lipohypertrophy, rotation of insulin injection site, and total daily insulin dose ≤ 50 units were all independently significantly associated with better glycemic control.
Conclusion: Insulin injection techniques were suboptimal among significant proportion of patients with diabetes in Jordan. Improper insulin injection technique, especially the rotation of injection sites and lipohypertrophy formation, was associated with uncontrolled blood glucose levels. Educational interventions that focus on insulin injection techniques among Jordanian patients with diabetes are strongly recommended.
Keywords: type 2 diabetes mellitus, type 1 diabetes mellitus, insulin therapy, lipohypertrophy
Introduction
Insulin is the primary treatment for patients with Type 1 diabetes mellitus (T1DM). It is often used as a supplement to oral hypoglycemic agents for patients with type 2 diabetes mellitus (T2DM) who have failed to achieve the glycemic target.1 Insulin has been the most effective treatment in controlling hyperglycemia among patients with diabetes for over the past 90 years. It is given subcutaneously, either through an insulin pump or via multiple daily insulin injection devices.2 All proper insulin administration techniques should be applied to achieve the desired outcomes from insulin therapy. Several studies showed that the greatest benefit from insulin treatment is achieved by correcting insulin injection techniques.3,4
Previous studies have shown that healthcare professionals rarely instruct patients about proper insulin injection techniques.3,5 The injection techniques, including the appropriate needle length, rotating insulin injection sites, changing needles between injections, and checking injection sites for the presence of lipohypertrophy (LH) are all crucial factors in the glycemic control.3 Lipohypertrophy is defined as the development of lumps, raised areas, firmness, or hardness in the fatty tissue under the skin caused by the repeated injection or infusion of insulin.6 There is a strong inverse association between lipohypertrophy and rotation of insulin injection sites. Patients frequently rotating their injection sites had lower lipohypertrophy prevalence.7–9
Studies about the effect of insulin injection technique on glycemic control are scarce, especially in the Middle East Region.10 The current literature available in Jordan includes only one published study that assesses the association between lipohypertrophy and some factors of insulin injection technique in type 2 diabetic patients. This may indicate the need for more research on this subject.11
This study aimed to assess the practices of insulin injection techniques among patients with diabetes treated at the National Center for Diabetes, Endocrinology and Genetics (NCDEG) in Amman, Jordan, and assess the effect of these practices on glycemic control.
Methods
This cross-sectional study was conducted between November 2020 and February 2021 at the outpatient clinics of the National Center for Diabetes, Endocrinology, and Genetics (NCDEG) in Amman, Jordan. The study methods and procedures are similar to those that had been used in an earlier study in 2015.11 A systematic sampling technique was used to recruit study subjects by choosing every fifth patient who attended the diabetes specialist outpatient clinics for regular follow-up during the study period. At NCDEG, patients are routinely referred to the educational clinic for comprehensive training on insulin administration techniques at the beginning of insulin implementation and regularly during their follow-ups every three to six months.
Patients with type 1 diabetes mellitus or type 2 diabetes mellitus who had been using insulin injections for at least a year were eligible for inclusion in the study. Women with gestational diabetes and infants were excluded from this study. The total sample was 851 subjects which translate to a margin of error of about 3.2%, given a prevalence of 37% and a 95% confidence level.
At enrolment, trained researchers administered a comprehensive structured questionnaire prepared explicitly for the purpose of the research based on similar previous studies.3,11,12 The main data obtained included sociodemographic variables, diabetes history, co-morbidities, current medications, practices of insulin injection techniques, and other variables. Insulin injection techniques were assessed by asking the subjects or their caregivers to demonstrate how they take insulin, checking the correct dose, angle degree of insulin injection, injection site, rotation of injection site, and time of needle lift after injection.
The researchers examined the site of insulin injection for the presence of LH (grade 1, grade 2, or grade 3). Also, the researchers checked the needle length with the support of a catalog that contains pictures of insulin type and type of needle length picture to help the subjects to identify the type of insulin and needle they were using. Glycosylated hemoglobin (HbA1c) level and anthropometric measurements were extracted from the medical records.
Grade 1 lipohypertrophy was defined as visible hypertrophy of fat tissue but palpably normal, while grade 2 as a massive thickening of fat tissue with firm consistency and grade 3 as lipoatrophy. Glycemic control was classified, according to the American Diabetes Association (ADA) criteria, as controlled if HbA1c is <7% and uncontrolled if HbA1c ≥7%.
The study was approved by the Ethical Committee at the National Center for Diabetes, Endocrinology, and Genetics in Amman, Jordan. All procedures performed in this study were in accordance with the 1964 Helsinki Declaration and its later amendments. A written informed consent was obtained from each adult subject (18+ years old). Caregiver written informed consent was taken for younger subjects (<18 years). Also, the ascent was taken from children aged seven to 17 years. Data were treated with rigorous confidentiality and used strictly and exclusively for scientific study purposes. Interviews with the subjects were conducted with proper social distancing measures to avoid Coronavirus Disease 2019 (COVID-19) hazards.
Statistical analysis was conducted using the Statistical Package for Social (SPSS, version 20). Continuous variables were described using mean ±Standard Deviation (SD), and categorical data were described using percentages. Percentages were compared using Chi-square test. Multivariate logistic regression analysis was performed to examine the effect of certain variables on glycemic control after adjustment of potential confounders. P values <0.05 was considered statistically significant.
Results
This study included 298 patients with T1DM and 553 insulin-treated patients with T2DM (Table 1). The age of patients with T1DM ranged between 2 and 68 years with a mean ±SD age of 20.1 ± 10.4 years. The mean ±SD age of patients with T2DM was 58.6 ± 9.5 years. Around half of patients with T1DM and T2DM were females. The median T1DM duration was 6.0 years, and median T2DM duration was 15.0 years. The mean ±SD insulin treatment duration in T2DM subjects was 6.7 ± 5.7 years, and the median was five years (Table 2).
 |
Table 1 Socio-Demographic Characteristics of Study Subjects |
 |
Table 2 Clinical and Laboratory and Anthropometric Characteristics of Study Subjects |
Overall, 85.6% of patients with T1DM and 96.0% of patients with T2DM used to inject insulin in the abdomen. Almost 42.3% of patients with T1DM reported that they inject insulin three times or less per day, and 48.8% of patients with T2DM reported injecting insulin two times or less per day.
In total, 13.8% of patients with T1DM and 4.9% of patients with T2DM were using injection needles of 4 mm length, 16.8% of patients with T1DM and 7.6% of patients with T2DM were using injection needles of 5 mm length, 29.5% of patients with T1DM and 12.5% of patients with T2DM were using injection needles of 6 mm length, and 39.9% of patients with T1DM and 75.0% of patients with T2DM were using injection needles of 8 mm length.
In addition, 66.8% and 69.4% of T1DM and T2DM subjects were rotating insulin injection sites regularly. The angle of insulin injection was 90° among 95.3% of T1DM subjects and 91.3% of T2DM subjects. Moreover, 36.6% of T1DM subjects and 50.5% of T2DM subjects were using the same insulin needle more than three times (Table 3). The prevalence of lipohypertrophy was 57.0% among patients with T1DM subjects and 55.5% among patients with T2DM (Table 4).
 |
Table 3 Insulin Injection Technique Characteristics for Study Subjects |
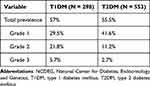 |
Table 4 Prevalence of Lipohypertrophy Among Diabetic Subjects in NCDEG |
The laboratory results showed that 46 T1DM subjects (15.4%) and 80 T2DM subjects (14.5%) had controlled glucose levels as defined by HbA1c <7%. Insulin injection techniques were associated with glycemic control assessed by HbA1c level among T2DM and T1DM subjects. In particular, there was a significant association between glycemic control and lipohypertrophy among T1DM (p-value <0.001) and T2DM subjects (p-value <0.001). Also, there was a significant association between glycemic control and rotation of insulin injection site among T1DM (p-value <0.001) and T2DM subjects (p-value <0.001). Lifting the needle inside for 10 seconds after the injection was significantly associated with better glycemic control among patients with T1DM (p-value 0.029) and patients with T2DM (p-value 0.010) (Table 5).
 |
Table 5 Glycemic Control According to Relevant Insulin Injection Technique Characteristics of Subjects at NCDEG |
In the multivariate analysis, the absence of lipohypertrophy (Odds ratio (OR) 2.2, 95% confidence interval (CI) 1.0–4.9, p-value 0.041), and rotation of insulin injection site (OR 4.7, 95% CI 1.3–17.6, p-value 0.022) were independently significantly associated with increased odds of controlled glycemic level among T1DM subjects. Among T2DM subjects, lipohypertrophy (OR 0.5, 95% CI 0.3–0.8, p-value 0.003) and total daily insulin dose ≤50 units (OR 0.5, 95% CI 0.3–0.9, p-value 0.012) were independently significantly associated with decreasing odds of controlled glycemic level. Also, among T2DM subjects, not having cardiovascular disease was independently significantly associated with increased odds of controlled glycemic level (OR 2.7, 95% CI 1.6–4.7, p-value <0.001) (Table 6).
 |
Table 6 Logistic Regression Analysis for the Socio-Demographic, Laboratory, and Clinical Factors and Insulin Injection Technique Affecting Glycemic Control |
Discussion
The prevalence of lipohypertrophy varies widely across countries. The current study shows that almost half of Jordanian diabetes mellitus (DM) subjects had lipohypertrophy. A systematic review and meta‐analysis of 26 studies reported an overall estimated prevalence of lipohypertrophy of 49% among T2DM subjects and 34% among T1DM subjects.13 Insufficient health education about injection techniques in Jordan might explain the high prevalence of lipohypertrophy among current study subjects.
At our center, patients are routinely referred to education clinics, where specialized diabetes nurses provide them with extensive theoretical and practical training on insulin injection techniques according to ADA recommendations. These education sessions are provided at the initiation of insulin therapy and are regularly repeated every three to six months. However, the current study and previous studies in Jordan have revealed some serious gaps in DM patients’ education.14 This emphasizes the need for additional creative DM educational resources and methods. Also, there is a need to involve additional health workers in the educational process, such as pharmacists, laboratory technicians, and community health workers.15,16
In our study, the prevalence of uncontrolled glycemic levels was significantly higher among subjects with lipohypertrophy. This finding is similar to a previous study in Egypt among T1DM subjects.17 However, a recent Saudi study did not find an association between lipohypertrophy and glycemic control among T2DM subjects.18 The differences in identifying this association between studies might be explained by differences among research subjects, sampling techniques, and settings.
It is worth mentioning here that the current study results indicated a low percentage of patients with controlled blood glucose levels as defined by HbA1c <7%. Similarly, previous studies in Jordan revealed a consistently low percentage of patients with controlled blood glucose levels ranging between 7% and 45%.19,20
In the current study, the rate of glycemic control was found to increase significantly by rotating the insulin injection site in both T1DM and T2DM subjects. de Villiers reported a similar association between the rotating injection site and glycemic control.22 However, Bochanen et al in 2022 did not find an association between the rotating injection site and HbA1c levels. Still, the frequency of hypoglycemia episodes decreased after rotating the injection site.23
The majority of current study subjects reported using the same needle multiple times. However, the current guidelines do not recommend the reuse of insulin needles to avoid the risk of skin complications such as pain, infection, and forming of lipohypertrophy.24 Arguably, there is currently no strong evidence supporting or against this common practice among DM subjects.25
It is recommended to keep the insulin needle under the skin for at least 10 seconds after the injection. This technique prevents insulin leakage and guarantees patients taking a full dose.1 Almost three-quarters (84.9% of T1DM and 73.1% of T2DM) of Jordanian DM subjects reported keeping their needles under the skin for this recommended duration. In previous studies, the rate of keeping the needle under the skin at least 10 seconds after the injection varied from 26% in Brazil to 90.3% in Poland.21,26
The multivariate analysis showed that T1DM subjects with a university educational level were more likely to have controlled glucose levels. The better maturity level might explain this better control among the educated subjects, which could lead to better adherence to insulin injection techniques compared to other children and adolescent T1DM subjects.
The main strength of the study was that the insulin injection practices were assessed using structured interviews and observing patients’ practices. The current study results can help guide healthcare providers in exploring best practices to improve insulin injection techniques and educational approaches to reach ideal glycemic control among DM subjects in Jordan. However, there are some limitations to this study. The study was conducted in a single diabetes center. This might limit the generalization of study outcomes to other settings. Another limitation is the cross-sectional nature of this study, where it is impossible to reach a causal conclusion between glycemic control and insulin injection techniques.
Conclusion
The practices of insulin injection techniques were suboptimal among significant proportion of patients with diabetes in Jordan. A high percentage of Jordanian patients do not rotate the injection site, reuse the needle multiple times, and do not leave the needle inside for 10 seconds after the injection. Improper insulin injection technique, especially the rotation of injection sites and lipohypertrophy formation, was associated with uncontrolled blood glucose levels. Educational interventions that target insulin injection techniques might improve glycemic control among Jordanian DM subjects and should be implemented. Evidence-based insulin injection technique recommendations and guidelines, including technological and innovative solutions, need to be adopted in Jordan. The current study was conducted in a single-center study; therefore, the generalization of study outcomes is limited. Additional multi-center and longitudinal research studies are required to build evidence-based practices and explore barriers to adherence to proper insulin injection techniques. Also, more efforts are needed in healthcare institutions to raise awareness among healthcare providers, especially nurses and pharmacists, about proper insulin injection techniques and how to advocate for their patients.
Abbreviations
DM, diabetes mellitus; HbA1c, glycosylated hemoglobin; LH, lipohypertrophy; NCDEG, National Center for Diabetes, Endocrinology and Genetics; SD and standard deviation; T1DM and type 1 diabetes mellitus; T2DM and type 2 diabetes mellitus.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Frid AH, Kreugel G, Grassi G., et al. New insulin delivery recommendations. Mayo Clin Proc. 2016;91(9):1231–1255. doi:10.1016/j.mayocp.2016.06.010
2. Chaudhury A, Duvoor C, Reddy Dendi VS, et al. Clinical review of antidiabetic drugs: implications for type 2 diabetes mellitus management. Front Endocrinol (Lausanne). 2017;8:6. doi:10.3389/fendo.2017.00006
3. Dagdelen S, Deyneli O, Olgun N, et al. Turkish insulin injection technique study: population characteristics of Turkish patients with diabetes who inject insulin and details of their injection practices as assessed by survey questionnaire. Diabetes Ther. 2018;9(4):1629–1645. doi:10.1007/s13300-018-0464-7
4. Nakatani Y, Matsumura M, Monden T, Aso Y, Nakamoto T. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013;30(10):897–906. doi:10.1007/s12325-013-0066-8
5. Huang MC, Hung CH, Yu CY, Berry DC, Shin SJ, Hsu YY. The effectiveness of multimedia education for patients with type 2 diabetes mellitus. J Adv Nurs. 2017;73(4):943–954. doi:10.1111/jan.13194
6. Tandon N, Kalra S, Balhara YPS, et al. Forum for Injection Technique (FIT), India: the Indian recommendations 2.0, for best practice in Insulin Injection Technique, 2015. Indian J Endocrinol Metab. 2015;19(3):317–331. doi:10.4103/2230-8210.152762
7. Chen L, Xing Q, Li J, et al. Injection technique education in patients with diabetes injecting insulin into areas of lipohypertrophy: a randomized controlled trial. Diabetes Ther. 2021;12(3):813–826. doi:10.1007/s13300-021-01013-1
8. Kamrul-Hasan A, Paul AK, Amin MN, et al. Insulin injection practice and injection complications - results from the Bangladesh insulin injection technique survey. Eur Endocrinol. 2020;16(1):41–48. doi:10.17925/EE.2020.16.1.41
9. Pozzuoli GM, Laudato M, Barone M, Crisci F, Pozzuoli B. Errors in insulin treatment management and risk of lipohypertrophy. Acta Diabetol. 2018;55(1):67–73. doi:10.1007/s00592-017-1066-y
10. Yuan L, Li F, Jing T, et al. Insulin injection technique is associated with glycemic variability in patients with type 2 diabetes. Diabetes Ther. 2018;9(6):2347–2356. doi:10.1007/s13300-018-0522-1
11. Al Ajlouni M, Abujbara M, Batieha A, Ajlouni K. Prevalence of lipohypertrophy and associated risk factors in insulin-treated patients with type 2 diabetes mellitus. Int J Endocrinol Metab. 2015;13(2):548. doi:10.5812/ijem.20776
12. Alhazmi GA, Balubaid RN, Sajiny S, Alsabbah R. Assessment of insulin injection technique among diabetic patients in Makkah region in Saudi Arabia. Cureus. 2020;12(9):e10679. doi:10.7759/cureus.10679
13. Deng N, Zhang X, Zhao F, Wang Y, He H. Prevalence of lipohypertrophy in insulin-treated diabetes patients: a systematic review and meta-analysis. J Diabetes Investig. 2017;9(3):536–543. doi:10.1111/jdi.12742
14. Al-Sahouri A, Merrell J, Snelgrove S. Barriers to good glycemic control levels and adherence to diabetes management plan in adults with Type-2 diabetes in Jordan: a literature review. Patient Prefer Adherence. 2019;13:675–693. doi:10.2147/PPA.S198828
15. Lyles BE, Chua S, Barham Y, et al. Improving diabetes control for Syrian refugees in Jordan: a longitudinal cohort study comparing the effects of cash transfers and health education interventions. Confl Health. 2021;15(1):41. doi:10.1186/s13031-021-00380-7
16. Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–526. doi:10.18553/jmcp.2012.18.7.516
17. Omar MA, El-Kafoury AA, El-Araby RI. Lipohypertrophy in children and adolescents with type 1 diabetes and the associated factors. BMC Res Notes. 2011;4:290. doi:10.1186/1756-0500-4-290
18. AlJaber AN, Sales I, Almigbal TH, Wajid S, Batais MA. The prevalence of lipohypertrophy and its associated factors among Saudi patients with type 2 diabetes mellitus. J Taibah Univ Med Sci. 2020;15(3):224–231. doi:10.1016/j.jtumed.2020.03.006
19. Al-Qerem W, Jarab AS, Badinjki M, Hammad A, Ling J, Alasmari F. Factors associated with glycemic control among patients with type 2 diabetes: a cross-sectional study. Eur Rev Med Pharmacol Sci. 2022;26(7):2415–2421. doi:10.26355/eurrev_202204_28475
20. Almomani MH, Al-Tawalbeh S. Glycemic control and its relationship with diabetes self-care behaviors among patients with type 2 diabetes in northern Jordan: a Cross-Sectional Study. Patient Prefer Adherence. 2022;16:449–465. doi:10.2147/PPA.S343214
21. Gorska-Ciebiada M, Masierek M, Ciebiada M. Improved insulin injection technique, treatment satisfaction and glycemic control: results from a large cohort education study. J Clin Transl Endocrinol. 2020;19:100217. doi:10.1016/j.jcte.2020.100217
22. de Villiers FPR. Lipohypertrophy—a complication of insulin injections. J Endocrinol Metab Diabetes South Af. 2006;11(2):64–66. doi:10.1080/22201009.2006.10872145
23. Bochanen N, Decochez K, Heleu E, et al. Lipohypertrophy Monitoring Study (LIMO): effect of single use of 4 mm pen needles combined with education on injection site rotation on glycaemic control: confirmation of an unpleasant truth. Diabet Med. 2022;39(1):e14672. doi:10.1111/dme.14672
24. Bahendeka S, Kaushik R, Swai AB, et al. EADSG guidelines: insulin storage and optimisation of injection technique in diabetes management. Diabetes Ther. 2019;10(2):341–366. doi:10.1007/s13300-019-0574-x
25. Zabaleta-Del-Olmo E, Vlacho B, Jodar-Fernández L, et al. Safety of the reuse of needles for subcutaneous insulin injection: a systematic review and meta-analysis. Int J Nurs Stud. 2016;60:121–132. doi:10.1016/j.ijnurstu.2016.04.010
26. Calliari LE, Cudizio L, Tschiedel B, et al. Insulin Injection Technique Questionnaire: results of an international study comparing Brazil, Latin America and World data. Diabetol Metab Syndr. 2018;10:85. doi:10.1186/s13098-018-0389-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
