Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Effect of Helicobacter Pylori Infection on Glucose Metabolism, Lipid Metabolism and Inflammatory Cytokines in Nonalcoholic Fatty Liver Disease Patients
Authors Xiao QY, Wang RL, Wu HJ, Kuang WB, Meng WW, Cheng Z
Received 5 December 2023
Accepted for publication 27 February 2024
Published 14 March 2024 Volume 2024:17 Pages 1127—1135
DOI https://doi.org/10.2147/JMDH.S453429
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Qing-Yu Xiao,1 Ren-Ling Wang,2 Hai-Jun Wu,1 Wen-Bin Kuang,3 Wei-Wei Meng,4 Zhen Cheng5
1Department of Blood Transfusion, Shenzhen Baoan Shiyan People’s Hospital, Shenzhen, 518108, China; 2Department of Oncology, Kaiping Central Hospital, Jiangmen City, Guangdong Province, 529399, People’s Republic of China; 3Department of Laboratory, Longhua District Central Hospital, Shenzhen, 518110, People’s Republic of China; 4Department of Laboratory, Shenzhen Baoan Shiyan People’s Hospital, Shenzhen, 518108, China; 5Guantian Community Healthcare Center, Shenzhen Baoan Shiyan People’s Hospital, Shenzhen, Guangdong province, 518100, People’s Republic of China
Correspondence: Zhen Cheng, Guantian Community Healthcare Center, Shenzhen Baoan Shiyan People’s Hospital, About 50 Meters South of hkc Huike Industrial Park, Dezheng Road, Baoan District, Shenzhen, Guangdong province, 518100, People’s Republic of China, Tel +86 13632854050, Email [email protected]
Objective: To probe into the influence of Helicobacter pylori (Hp) infection on glucose metabolism, lipid metabolism, and inflammatory cytokines in patients with nonalcoholic fatty liver disease (MASLD).
Methods: A total of 140 MASLD patients admitted to our Hospital between June 2020 and May 2021 were selected as the research objects. Based on the presence or absence of Hp infection, they were divided into the study group (73 cases with infection) and control group (67 cases without infection). Glucose metabolism indicators [fasting blood glucose (FBG), 2-hour postprandial glucose (2hPG), fasting insulin (FINS), glycated hemoglobin (HbAlc)], lipid metabolism indicators [total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C)], and inflammatory indicators [interleukin-37 (IL-37), interleukin-18 (IL-18)] were measured and compared between the two groups.
Results: In terms of glucose metabolism indicators, the study group exhibited higher levels of FBG (5.84± 0.49 vs 5.40± 0.51, t=2.535, P=0.012), 2hPG (7.26± 1.30 vs 6.50± 1.53, t=3.321, P< 0.001), and FINS (11.13± 4.13 vs 9.12± 3.72, t=3.224, P< 0.001), and Insulin resistance index (HOMA-IR) (2.97± 0.35 VS 2.13± 0.54, t=3.761, P< 0.001) and a lower level of HbAlc (5.25± 0.56 vs 6.12± 0.57, t=5.473, P< 0.001) compared to the control group. Regarding lipid metabolism indicators, the study group exhibited higher levels of TC (5.64± 1.49 vs 5.01± 1.32, t=3.332, P< 0.001), TG (1.89± 0.34 vs 1.32± 0.43, t=3.411, P< 0.001), and LDL-C (3.31± 0.43 vs 2.12± 0.29, t=4.142, P< 0.001), and a lower level of HDL-C (1.45± 0.21 vs 1.78± 0.42, t=4.347, P< 0.001) compared to the control group. As for the inflammatory indicators, the study group exhibited higher levels of IL-37 (45.56± 6.02 vs 34.02± 3.28, t=9.332, P< 0.001) and IL-18 (73.57± 5.82 vs 60.34± 4.84, t=10.141, P< 0.001) compared to the control group.
Conclusion: It is crucial to place appropriate emphasis on the impact of Hp infection on the glucose metabolism, lipid metabolism, and inflammatory response in MASLD patients, warranting careful consideration during the treatment of these patients.
Keywords: Helicobacter pylori, infection, nonalcoholic fatty liver disease, glucose metabolism, lipid metabolism, inflammatory indicators
A Letter to the Editor has been published for this article.
Introduction
Nonalcoholic fatty liver disease (MASLD) refers to hepatic disorders with a lipid content alteration of over 5%, is now recognized as a global public health problem. MASLD affects 20% to 45% of the general population, and prevalence is increasing globally.1 This condition is mainly caused by obesity, diabetes, hyperlipidemia and other metabolic syndrome or malnutrition, total parenteral nutrition, sharp weight loss after weight loss surgery, drugs / environment and so on.2 Failure to implement timely preventive and therapeutic measures can result in the progression of MASLD to more severe conditions, including advanced liver fibrosis, cirrhosis, and even the development of malignancies. Nonalcoholic steatohepatitis (NASH) has emerged as the primary cause of chronic liver inflammation.3–5 MASLD can give rise to a spectrum of clinical pathological syndromes.6–8 The etiology of MASLD involves insulin resistance (IR) and genetic defects, which profoundly impact the normal physiological functioning of the body and may have negative effects on the patients’ quality of life.
In recent years, extensive research has identified the etiology of MASLD, which includes obesity, visceral adiposity, dyslipidemia, type 2 diabetes, and hypertension. Consequently, MASLD is regarded as an integral component of metabolic syndrome within the liver.9 Currently, MASLD has proven a significant hepatic disorder with global health implications. Additionally, MASLD has the third highest incidence in the United States, behind only hepatitis C and alcoholic liver disease (ALD). Therefore, prioritizing effective strategies for the prevention and treatment of MASLD is paramount. Based on pertinent studies, it is anticipated that NASH will soon surpass other causes and become the primary determinant of mortality in liver transplantation.10,11 However, the underlying mechanisms involved in the pathogenesis of MASLD remain enigmatic. Current evidence suggests that its onset may stem from multifaceted factors, including dysfunctional adipose tissue, insulin resistance, and genetic mutations.12,13 Nonetheless, the implementation of effective measures for MASLD prevention and control remains of utmost urgency.
Helicobacter pylori (Hp), a helical-shaped microaerobic Gram-negative bacterium, is capable of transmission via the fecal-oral or oral-oral route.14,15 It invades the gastric mucosa, thereby causing a range of gastrointestinal disorders,16 including gastritis, duodenal ulcers, gastric cancer, and lymphoid tissue lymphoma.17,18 Recent research suggests that Hp infection not only contributes to gastrointestinal diseases but also gives rise to extraintestinal manifestations. Moreover, persistent Hp infection can elicit immune and inflammatory responses in the host organism.19–21 One study found that 39.4% of 505 MASLD patients were infected with HP.22 Conversely, Hp infection has also been implicated in the development of MASLD. If preventive and therapeutic measures are not implemented in time, MASLD may progress to more serious conditions, including advanced liver fibrosis, cirrhosis, and even malignant tumors. A previous study established a close link between MASLD and bladder cancer, which is one of the most serious malignant tumors in the elderly, as evidenced by the association between MASLD and insulin resistance and non-metastatic bladder cancer patients: a cross-sectional retrospective study.23 Individuals with this condition commonly exhibit disturbances in both glucose and lipid metabolism.24 The relationship between Hp infection and MASLD has attracted extensive attention from scholars at home and abroad. A meta-analysis involving 15 studies showed that Hp infection was positively correlated with MASLD.25 The study results of Tang et al26 showed that Hp infection was an independent risk factor for MASLD progression. Polyzos et al27 also reached a similar conclusion. However, no significant difference was found in Hp infection rate between patients with nonalcoholic simple fatty liver and MASLD during intra-group analysis, suggesting that Hp infection was not a factor promoting the progression of nonalcoholic simple fatty liver to nonalcoholic steatohepatitis. Therefore, exploring the mechanism of Hp infection in MAFLD is of great significance to guide the prevention or treatment of MAFLD. The purpose of this study is to investigate the influence of Hp infection on glucose metabolism, lipid metabolism, and inflammatory cytokines in patients with MASLD.
Objects and Methods
Research Objects
Convenient sampling was employed to select 140 patients with MASLD who were admitted to our Hospital between June 2020 and May 2021. Based on the presence or absence of Hp infection, they were divided into the study group (73 cases with infection) and control group (67 cases without infection). Inclusion criteria: (1) clinical diagnosis meeting the diagnostic criteria of the “Prevention and Treatment Guidelines for Nonalcoholic Fatty Liver Disease”28 (2) MASLD activity score (NAS) >4 scores; (3) no history of excessive alcohol consumption, with a weekly ethanol intake of <140 g for males and <70 g for females; (4) No severe anemia or acute infection / inflammation. Exclusion criteria: (1) severe cardiovascular, liver, or lung diseases; (2) patients with other severe malignant tumors, drug-induced hepatitis, cirrhosis, acute or chronic viral hepatitis, or endocrine disorders; (3) recent use of antibiotics; (4) those unwilling to adhere to medical advice or cooperate closely. This study was approved by the Ethics Committee of our Hospital. All study participants were fully informed and provided written consent.
Data Collection
Demographic characteristic and serological data were collected from the patients. The demographic characteristics included age, gender, disease duration, smoking history, height, BMI, hypertension, and diabetes. The collection and detection of all indicators were carried out before the hospital treatment.
Serological indicators included: (1) glucose metabolism indicators [fasting blood glucose (FBG), 2-hour postprandial glucose (2hPG), fasting insulin (FINS), glycated hemoglobin (HbAlc), Insulin resistance index (HOMA-IR)]; (2) lipid metabolism indicators [total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C)]; (3) inflammatory indicators [interleukin-37 (IL-37), interleukin-18 (IL-18)].
Hp detection was conducted using the 14C-urea breath test. The test kit was provided by Shenzhen Zhonghe Headway Bio-Sci & Tech Co., Ltd., with the Chinese Medical Approval Number H20068129. The detection process was as follows: (1) All patients took one 14C-urea pill (Chinese Medical Approval Number H20000020, Shenzhen Zhonghe Headway Bio-Sci & Tech Co., Ltd., drug specification: 278 KBq (0.75 μCi)) on an empty stomach in the morning and remained seated for 30 minutes; (2) A disposable breath tube was inserted into the bottom of a carbon dioxide (CO2) reagent tube, and the patient breathed normally until the CO2 reagent discoloration stopped; (3) Take the liquid in 5mL scintillation bottle and use LKB1217 type liquid scintillation counter to measure the decay number per minute to detect the value ≥ 100dpm is positive.
MASLD testing and diagnosis: Diagnosis of MASLD is made when liver imaging findings are consistent with diffuse fatty liver and no other explanations are present; or when patients with components of metabolic syndrome have unexplained persistent elevation of serum ALT or AST, GGT for more than six months. Confirmation of MASLD diagnosis can be made when abnormal liver enzymes and imaging findings improve or return to normal after weight loss and improvement of IR.28
Process of serological indicator testing: All patients had 3 mL of venous blood drawn in the morning. The blood samples were centrifuged at 1000 r/min to separate the upper clear liquid, which was then stored at −60°C for further testing. (1) Glucose metabolism indicators: FINS levels were measured using radioimmunoassay, with the test kit provided by Beijing Furui Runze Biotechnology Co., Ltd. FBG and 2hBG levels were measured using the glucose oxidase method, with the test kit provided by Shanghai Enzyme Linked Biotechnology Co., Ltd. HOMA-IR is calculated by the following formula: HOMA-IR=FPG×FINS/22.5. HbAlc levels were measured using high-performance liquid chromatography, with the test kit provided by Hepeng (Shanghai) Biotechnology Co., Ltd. (2) Lipid metabolism indicators: Detection was performed using the BK-400 fully automated biochemical analyzer (Biobase Biodustry (Shandong) Co., Ltd.), with the test kit provided by Shanghai Enzyme Linked Biotechnology Co., Ltd. (3) Inflammatory indicators: Detection was performed using the BK-2008R ELISA Reader (Shanghai Huanxi Medical Co., Ltd.), with the test kit provided by Shanghai Jingkang Bioengineering Co., Ltd.
Statistical Analysis
Statistical software IBM SPSS Statistics version 21.0 IBM SPSS Inc., Chicago, USA) was employed for data analysis. Quantitative data were tested for normality using the K-S method. If the quantitative data conformed to a normal distribution, it was represented as mean ± standard deviation (x±s), with inter-group comparisons being performed using t-tests. If the quantitative data did not conform the normal distribution, it was expressed by the median (quartile range). Count data were presented as frequency (n) or percentage (%), and inter-group comparisons were conducted using χ2 tests. A difference was considered statistically significant at P< 0.05.
Results
Demographic Characteristics
The study group included 73 cases (14C-urea detection value ≥100dpm, mean detection value of 424.05±51.38), while the control group included 67 cases (14C-urea detection value <100dpm, mean detection value of 74.36±19.63). In the study group, there were 37 males and 36 females, with an age range of 27 to 62 years and a mean age of 51.21 ± 9.76 years. The disease duration ranged from 2.5 to 13.5 years, with a mean duration of (9.51 ± 2.53) years. In the control group, there were 32 males and 35 females, with an age range of 28 to 62 years and a mean age of 53.0 ± 12.0 years. The disease duration ranged from 2 to 14 years, with a mean duration of (9.75 ± 2.56) years. There were no statistically significant differences between the two groups in terms of age, gender, disease duration, smoking history, height, body mass index (BMI), percentage of hypertension, percentage of diabetes, ALT and AST (P> 0.05), as shown in Table 1.
 |
Table 1 Comparison of Baseline Data Between Two Groups |
Comparison of Glucose Metabolism Indicators Between Two Groups
The results showed statistically significant differences (P<0.05) in FBG, 2hPG, FINS, and HbAlc levels between the two groups. The study group exhibited higher levels of FBG (5.84±0.49 VS 5.40±0.51, t=2.535, P=0.012), 2hPG (7.26±1.30 VS 6.50±1.53, t=3.321, P<0.001), and FINS (11.13±4.13 VS 9.12±3.72, t=3.224, P<0.001), HOMA-IR (2.97±0.35 VS 2.13±0.54, t=3.761, P<0.001) and a lower level of HbAlc (5.25±0.56 VS 6.12±0.57, t=5.473, P<0.001) compared to the control group, as suggested in Table 2.
 |
Table 2 Comparison of Glucose Metabolism Indicators Between Two Groups (x±s) |
Comparison of Lipid Metabolism Indicators Between Two Groups
The results demonstrated statistically significant differences (P<0.05) in TC, TG, LDL-C, and HDL-C levels between the two groups. The study group exhibited higher levels of TC (5.64±1.49 VS 5.01±1.32, t=3.332, P<0.001), TG (1.89±0.34 VS 1.32±0.43, t=3.411, P<0.001), and LDL-C (3.31±0.43 VS 2.12±0.29, t=4.142, P<0.001), and a lower level of HDL-C (1.45±0.21 VS 1.78±0.42, t=4.347, P<0.001) compared to the control group, as indicated in Table 3.
 |
Table 3 Comparison of Lipid Metabolism Indicators Between Two Groups (x±s) |
Comparison of Inflammatory Indicators Between Two Groups
The results revealed that the study group exhibited higher levels of IL-37 (45.56±6.02 VS 34.02±3.28, t=9.332, P<0.001) and IL-18 (73.57±5.82 VS 60.34±4.84, t=10.141, P<0.001) compared to the control group, as presented in Table 4.
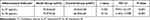 |
Table 4 Comparison of Inflammatory Indicators Between Two Groups (x±s) |
Discussion
The results of this study revealed statistically significant differences (P<0.05) in the glucose metabolism indicators and lipid metabolism indicators namely FBG, 2hPG, FINS, HOMA-IR, HbAlc, TC, TG, LDL-C, and HDL-C between the two groups of patients. The study group exhibited higher levels of FBG, 2hPG, FINS, HOMA-IR, TC, TG and LDL-C and a lower level of HbAlc and HDL-C compared to the control group.
In recent years, scientific research has revealed a significant association between Hp and MASLD. The presence of Hp has been found to impact the occurrence and progression of MASLD. A prospective cohort multicenter pilot study with 2 years of follow-up in 369 adults without MASLD at baseline indicated that HP infection was positively associated with MASLD development. This was shown by increased markers of insulin resistance, inflammatory mediators such as interleukin-6 and C-reactive protein, and lipid metabolism such as the leptin/adiponectin ratio, and decreased lipid metabolism marker, HDL. Furthermore, these MASLD risk factors can be recovered after eradication of HP infection.29 Besides, the lipid metabolism markers of TC, triglyceride, HDL-C and LDL-C showed no significant difference between HP-positive and HP-negative MASLD patients in a study. Notably, a significant difference occurred after removal of the confounding factor of MASLD status.30 Obesity is an important cause of MASLD, and central obesity is significantly associated with infection of Hp, so infection with Hp may indirectly lead to the disease of MASLD,31 searchers postulate that IR may serve as a bridge between Hp and MASLD.32 In the pathogenesis of MASLD, IR plays a pivotal role.33 Over the years, clinical trials have confirmed the substantive contribution of chronic inflammation to IR. Hp is capable of enhancing the expression of tumor necrosis factor, C-reactive protein, interleukin, and other insulin resistance indicators, consequently increasing IR.34,35 Fetuin-A, as an integral pro-inflammatory mediator, exerts a significant influence on inflammation and other immunological disorders.32 Recent research has revealed a substantial elevation in levels of fetuin-A in populations affected by Hp infection, suggesting its potential to facilitate IR,36,37 which possesses considerable implications in the treatment of diabetes. Additionally, the reciprocal interaction between IR and the immune system fosters metabolic inflammation, while Hp infection influences immune cells such as mast cells, dendritic cells, and eosinophils, thereby contributing to IR.38 Hp can also invade the liver via the hepatobiliary duct in a retrograde manner, triggering chronic liver inflammation and causing severe damage and apoptosis of liver cells.39,40 IR can result in disturbances in glucose and lipid metabolism within the organism, which can impede the activity of microsomal lipid peroxidase and subsequently lead to lipid accumulation in patients.41 Furthermore, Hp infection has been observed to induce significant alterations in blood lipid levels, thus establishing abnormal blood lipid profiles as prevalent phenomena among MASLD patients.42
The presence of Hp may induce the generation of inflammatory cytokines in gastric epithelial cells, thereby initiating a chronic inflammatory response. Additionally, these inflammatory cytokines may also inhibit the activity of lipoprotein lipase, affecting lipid levels in the bloodstream. Moreover, certain inflammation cytokines can potentially influence the activity of hepatic lipase, resulting in alterations of TC, TG, LDL-C, and HDL-C levels. Furthermore, these inflammation cytokines affect the expression of glucose transporters on cell membranes, significantly impacting insulin sensitivity in patients, leading to abnormal glucose metabolism and consequent hyperglycemia.43,44
As an important member of the IL-1 family, IL-37 can be expressed in various cell types, including monocytes, macrophages, lymphocytes, and neutrophils, exerting anti-inflammatory effects. According to recent research,45 the levels of IL-37 in the bloodstream of MASLD patients are significantly elevated. This alteration provides valuable insight into the extent of liver cell damage and aids in the assessment of severity of the disease. IL-18 plays a crucial role in the therapeutic process of MASLD. It is not solely sourced from monocytes and macrophages but also possesses diverse additional functions. According to the latest research,46 there is a remarkable increase in the levels of IL-18 within the bodies of MASLD patients, which might be a key factor in the pathogenesis of MASLD. The activation of IL-18 triggers the production of numerous inflammatory mediators, thereby exacerbating the inflammatory response in hepatocytes.47 Our study results demonstrate that the levels of IL-37 (45.56±6.02 VS 34.02±3.28, t=9.332, P<0.001) and IL-18 (73.57±5.82 VS 60.34±4.84, t=10.141, P<0.001) in the study group were significantly higher compared to the control group, aligning with the aforementioned research findings. Previous studies have shown that there is an increase in interleukin-37 in patients with peptic ulcer infected with Helicobacter pylori, which is significant in the circulating concentration of interleukin-37 in patients with peptic ulcer infected with Helicobacter pylori.48 It can be hypothesized that the presence of Hp may induce an inflammatory response by stimulating the large release of IL-6, IL-8, IL-37, IL-18, and NF-κB, which are potent vascular active substances, thereby contributing to the development of inflammation.49 In addition, Helicobacter pylori activates NLRP3 inflammatory bodies through ROS signaling pathway and induces human monocytes to produce IL-1 β and IL-18.50 To sum up, alleviating Hp infection will contribute to the treatment of MASLD to some extent, such as some natural products, which will play an important role in alleviating Hp infection and MASLD.51,52
It was shown that fasting insulin, HOMA-IR, CRP and C-LDL levels decreased in HP positive patients 6 weeks after successful eradication with a sequential regimen, suggesting a beneficial effect on atherogenic metabolic abnormalities and CLGI.53 An argument favouring the role of low-grade inflammation in the lipid profile alterations is that successful eradication of HP infection induced an increase of HDL-C, apo A, while TC and LDL remained unchanged.54,55 These results were not reproduced in large Spanish and Chinese trials and the minor changes of blood lipids were attributed rather to lifestyle modifications.56–58 Based on these data, some experts suggested to perform large interventional trials aimed at evaluating the benefit of HP eradication on the prevention of metabolic syndrome and type 2-diabetes mellitus.59 In the most recent study of 308 Lebanese subjects, no association of HP with insulin resistance and metabolic syndrome was found and the authors concluded, that eradication of the infection to prevent these conditions is not warranted. Metabolic syndrome, however, is a multifactorial condition in which HP infection seems to play only a minor, if any role. The prevalence of the infection is decreasing spontaneously in the developed countries, while that of metabolic syndrome is constantly increasing: parallel epidemiologic studies of these 2 conditions have not been performed and it would be intriguing to see whether spontaneous and/or eradication-induced decrease of HP burden of the general population will result any change in the development and natural course of metabolic syndrome. It must be proven by future controlled long-term trials, whether eradicating the infection will result prevention of these conditions.
To sum up, the novelty of this study is to explore the relationship between Helicobacter pylori infection and non-alcoholic fatty liver, and to study its effects on glucose metabolism, lipid metabolism and the level of inflammatory cytokines. It provides a new perspective for understanding the pathogenesis of nonalcoholic fatty liver. Despite achieving some notable results, this study exhibits several limitations. Firstly, the small sample size may introduce selection bias and hinder the generalizability of the findings, thereby imposing certain restrictions on the accuracy of the conclusions. Secondly, the limited sample size and potential interactions between IL-37, IL-18, and Hp infection among MASLD patients may complicate the elucidation of certain mechanisms, necessitating the exclusion of these interactive effects for subsequent analysis. In addition, the diagnostic methods of Helicobacter pylori infection used in the study may have some limitations. Different detection methods may lead to missed diagnosis or misdiagnosis of Helicobacter pylori infection, thus affecting the accuracy of the results. In addition to Helicobacter pylori infection, there are many other factors that may affect the development and metabolic disorders of non-alcoholic fatty liver, such as genetic factors, lifestyle, eating habits and so on. The existence of these factors may interfere with the association between Helicobacter pylori infection and non-alcoholic fatty liver disease. Future research endeavors should employ large-scale and multicenter randomized controlled trials to objectively and effectively assess the influence of Hp infection on the glucose metabolism, lipid metabolism, and inflammatory cytokines, in MASLD patients.
In sum, it is crucial to place appropriate emphasis on the impact of Hp infection on the glucose metabolism, lipid metabolism, and inflammatory response in MASLD patients, warranting careful consideration during the treatment of these patients.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of Shiyan People’s Hospital (No. EC-20230118-1004), and informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Funding
Shenzhen Baoan District science and Technology Innovation Bureau (2021JD141).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract. 2022;28(5):528–562. doi:10.1016/j.eprac.2022.03.010
2. Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol. 2019;70(3):531–544. doi:10.1016/j.jhep.2018.10.033
3. Estes C, Anstee QM, Arias-Loste MT, et al. Modeling MASLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69(4):896–904. doi:10.1016/j.jhep.2018.05.036
4. Younossi ZM, Tampi R, Priyadarshini M, Nader F. Burden of illness and economic model for patients with Non-Alcoholic Steatohepatitis (NASH) in the United States. Hepatology. 2018;69(2). doi:10.1002/hep.30254
5. Fan XF, Deng YQ, Wu GL. [Study on the distribution and characteristics of Chinese medicine syndrome in patients with nonalcoholic fatty liver disease]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2011;31(10):1332–1336. Chinese.
6. Fierbinteanu Braticevici C, Sporea I, Panaitescu E, Tribus L. Value of acoustic radiation force impulse imaging elastography for non-invasive evaluation of patients with nonalcoholic fatty liver disease. Ultrasound Med Biol. 2013;39(11):1942–1950. doi:10.1016/j.ultrasmedbio.2013.04.019
7. Betancourt AM, King AL, Fetterman JL, et al. Mitochondrial-nuclear genome interactions in non-alcoholic fatty liver disease in mice. Biochem J. 2014;461(2):223–232. doi:10.1042/BJ20131433
8. Zheng JS, Xu A, Huang T, Yu X, Li D. Low docosahexaenoic acid content in plasma phospholipids is associated with increased non-alcoholic fatty liver disease in China. Lipids. 2012;47(6):549–556. doi:10.1007/s11745-012-3671-4
9. Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference [published correction appears in Hepatology. 2003 Aug;38(2):536]. Hepatology. 2003;37(5):1202–1219. doi:10.1053/jhep.2003.50193
10. Elliott C, Frith J, Day CP, Jones DE, Newton JL. Functional impairment in alcoholic liver disease and non-alcoholic fatty liver disease is significant and persists over 3 years of follow-up. Dig Dis Sci. 2013;58(8):2383–2391. doi:10.1007/s10620-013-2657-2
11. Masuda K, Ono M, Fukumoto M, et al. Usefulness of Technetium-99 m-2-methoxy-isobutyl-isonitrile liver scintigraphy for evaluating disease activity of non-alcoholic fatty liver disease. Hepatol Res. 2012;42(3):273–279. doi:10.1111/j.1872-034X.2011.00923.x
12. Polyzos SA, Kountouras J, Zavos C. Nonalcoholic fatty liver disease: the pathogenetic roles of insulin resistance and adipocytokines. Curr Mol Med. 2009;9(3):299–314. doi:10.2174/156652409787847191
13. Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (MASLD). Metabolism. 2016;65(8):1038–1048. doi:10.1016/j.metabol.2015.12.012
14. Ahmed KS, Khan AA, Ahmed I, et al. Prevalence study to elucidate the transmission pathways of Helicobacter pylori at oral and gastroduodenal sites of a South Indian population. Singapore Med J. 2006;47(4):291–296.
15. Mladenova I, Durazzo M. Transmission of Helicobacter pylori. Minerva Gastroenterol Dietol. 2018;64(3):251–254. doi:10.23736/S1121-421X.18.02480-7
16. Tsay FW. Hsu PHPinfection and extra-gastroduode-nal diseases. J Biomed Sci. 2018;25(1):65. doi:10.1186/s12929-018-0469-6
17. Liu WZ, Xie Y, Lu H, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi:10.1111/hel.12475
18. Wessler S, Krisch LM, Elmer DP, Aberger F. From inflammation to gastric cancer - the importance of Hedgehog/GLI signaling in Helicobacter pylori-induced chronic inflammatory and neoplastic diseases. Cell Commun Signal. 2017;15(1):15. doi:10.1186/s12964-017-0171-4
19. Lv NH, Xie C. Review and prospect of Helicobacter pylori infection research in China. Chin J Digest. 2021;41(4):217–220.
20. Hanafiah A, Lopes BS. Genetic diversity and virulence characteristics of Helicobacter pylori isolates in different human ethnic groups. Infect Genet Evol. 2020;78:104135. doi:10.1016/j.meegid.2019.104135
21. Li LN, Liu Y, Zhang HC, Wu T, Dai Y, Wang WH. Effect of Helicobacter pylori infection on inflammatory colorectal cancer induced by AOM/DSS in mice and its immune mechanism. Nat Med J China. 2020;100(34):2689–2695. doi:10.3760/cma.j.cn112137-20200112-00076
22. Wang J, Dong F, Su H, et al. H. pylori is related to NAFLD but only in female: a cross-sectional study. Int J Med Sci. 2021;18(11):2303–2311. doi:10.7150/ijms.50748
23. Tarantino G, Crocetto F, Di Vito C, et al. Association of MASLD and insulin resistance with non metastatic bladder cancer patients: a cross-sectional retrospective study. J Clin Med. 2021;10(2):346. doi:10.3390/jcm10020346
24. Zhu BB, Zhou HK, Bai XF, Liu Y, Li WP. Research progress on the relationship between Hp infection and non-alcoholic fatty liver disease. Hainan Med J. 2017;28(11):1833–1835.
25. Zhou BG, Yang HJ, Xu W, Wang K, Guo P, Ai YW. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: a systematic review and meta-analysis of observational studies. Helicobacter. 2019;24(3):e12576. doi:10.1111/hel.12576
26. Tang DM, Kumar S. The Association Between Helicobacter pylori infection and nonalcoholic fatty liver disease. Curr Gastroenterol Rep. 2017;19(2):5. doi:10.1007/s11894-017-0545-1
27. Polyzos SA, Kountouras J, Papatheodorou A, et al. Helicobacter pylori infection in patients with nonalcoholic fatty liver disease. Metabolism. 2013;62(1):121–126. doi:10.1016/j.metabol.2012.06.007
28. Fan JG, Wei L, Zhuang H. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: a 2018 update. J Pract Hepatol. 2018;21(2):177–186.
29. Abdel-Razik A, Mousa N, Shabana W, et al. Helicobacter pylori and non-alcoholic fatty liver disease: a new enigma? Helicobacter. 2018;23(6):e12537. doi:10.1111/hel.12537
30. Chen C, Zhang C, Wang X, et al. Helicobacter pylori infection may increase the severity of nonalcoholic fatty liver disease via promoting liver function damage, glycometabolism, lipid metabolism, inflammatory reaction and metabolic syndrome. Eur J Gastroenterol Hepatol. 2020;32(7):857–866. doi:10.1097/MEG.0000000000001601
31. Wu QQ, Qin K, wang YJ. Central obesity is associated with helicobacter pylori infection: a large-scale cross-sectional retrospective study in West China. Int J Diabetes Dev Countries. 2019;40(2). doi:10.1007/s13410-019-00765-8
32. Kebapcilar L, Bilgir O, Cetinkaya E, Akyol M, Bilgir F, Bozkaya G. The effect of Helicobacter pylori eradication on macrophage migration inhibitory factor, C-reactive protein and fetuin-a levels. Clinics. 2010;65(8):799–802. doi:10.1590/s1807-59322010000800010
33. Cheng DD, He C, Ai HH, Huang Y, Lu NH. The possible role of helicobacter pylori infection in non-alcoholic fatty liver disease. Front Microbiol. 2017;8:743. doi:10.3389/fmicb.2017.00743
34. Chen CX, Mao YS, Foster P, Zhu ZW, Du J, Guo CY. Possible association between Helicobacter pylori infection and nonalcoholic fatty liver disease. Appl Physiol Nutr Metab. 2017;42(3):295–301. doi:10.1139/apnm-2016-0499
35. Nagura H, Ohtani H, Sasano H, Matsumoto T. The immuno-inflammatory mechanism for tissue injury in inflammatory bowel disease and Helicobacter pylori-infected chronic active gastritis. Roles of the mucosal immune system. Digestion. 2001;63(Suppl 1):12–21. doi:10.1159/000051905
36. Peverill W, Powell LW, Skoien R. Evolving concepts in the pathogenesis of NASH: beyond steatosis and inflammation. Int J Mol Sci. 2014;15(5):8591–8638. doi:10.3390/ijms15058591
37. Ou HY, Yang YC, Wu HT, Wu JS, Lu FH, Chang CJ. Increased fetuin-A concentrations in impaired glucose tolerance with or without nonalcoholic fatty liver disease, but not impaired fasting glucose. J Clin Endocrinol Metab. 2012;97(12):4717–4723. doi:10.1210/jc.2012-2414
38. Li M, Shen Z, Li YM. Potential role of Helicobacter pylori infection in nonalcoholic fatty liver disease. World J Gastroenterol. 2013;19(41):7024–7031. doi:10.3748/wjg.v19.i41.7024
39. Boursier J, Mueller O, Barret M, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63(3):764–775. doi:10.1002/hep.28356
40. Včev A, Nakić D, Mrđen A, et al. Helicobacter pylori infection and coronary artery disease. Coll Antropol. 2007;31(3):757–760.
41. Chai Y, Guo N, Yao HX, et al. Effect of Helicobacter pylori eradication therapy on lipid metabolism and insulin resistance in non-alcoholic fatty liver disease. Chin J Nosocomiol. 2021;31(9):1319–1323.
42. Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–1031. doi:10.1038/nature05414
43. Yang SX, Cai SL, Yang N, et al. Effect of Helicobacter pylori infection on glucose and lipid metabolism in patients with metabolic syndrome. Chin J Nosocomiol. 2021;31(20):3135–3138.
44. Tang WZ, Wang ZL, Wang XJ, et al. Study on the impact of Helicobacter pylori infection on glucose metabolism in patients with chronic hepatitis B cirrhosis. Chin J Nosocomiol. 2019;29(24):3715–3718.
45. Cox MJ, Turek EM, Hennessy C, et al. Longitudinal assessment of sputum microbiome by sequencing of the 16S rRNA gene in non-cystic fibrosis bronchiectasis patients. PLoS One. 2017;12(2):e0170622. doi:10.1371/journal.pone.0170622
46. Zhao JM, Yan XX, Li GX, et al. Characteristics of clinical feature in the patients with chronic obstructive pulmonary disease with bronchiectasis. IntJRespir. 2018;38(19):1460–1464.
47. Zhao W, Zhang ZP, Wang DY, et al. Study on the correlation between IL-18, hs-CRP, and TNF-α expression in patients with gastric cancer complicated by Helicobacter pylori infection. Chin J Nosocomiol. 2020;30(11):1651–1654.
48. Davarpanah E, Jafarzadeh A, Nemati M, et al. Circulating concentration of interleukin-37 in Helicobacter pylori-infected patients with peptic ulcer: its association with IL-37 related gene polymorphisms and bacterial virulence factor CagA. Cytokine. 2020;126:154928. doi:10.1016/j.cyto.2019.154928
49. He YK, Huang XL, Zhang XY, et al. Effect of vitamin D adjuvant therapy on serum levels of TNF-α, IL-6, and CRP in patients with non-alcoholic fatty liver disease. Hainan Med J. 2017;28(9):1481–1483.
50. Li X, Liu S, Luo J, et al. Helicobacter pylori induces IL-1β and IL-18 production in human monocytic cell line through activation of NLRP3 inflammasome via ROS signaling pathway. Pathog Dis. 2015;73(4):ftu024. doi:10.1093/femspd/ftu024
51. Liu Q, Meng X, Li Y, et al. Natural products for the prevention and management of Helicobacter pylori infection. Compr Rev Food Sci Food Saf. 2018;17(4):937–952. doi:10.1111/1541-4337.12355
52. Tarantino G, Balsano C, Santini SJ, et al. It is high time physicians thought of natural products for alleviating MASLD. is there sufficient evidence to use them? Int J Mol Sci. 2021;22(24):13424. doi:10.3390/ijms222413424
53. Gen R, Demir M, Ataseven H. Effect of Helicobacter pylori eradication on insulin resistance, serum lipids and low grade inflammation. South Med J. 2010;103(3):190–196. doi:10.1097/SMJ.ob0113e3181cf373f
54. Coronado MT, Pozzi AO, Punchard MA, González P, Fantidis P. Inflammation as a modulator of the HDL cholesterol induced inteleukin-10 production by human circulating mononuclear cells. Atherosclerosis. 2009;202(1):183–184. doi:10.1016/j.atherosclerosis.2008.03.015
55. Scharnagl H, Kist M, Grawitz AB, Koenig W, Wieland H, März W. Effect of Helicobacter pylori eradication on high density lipoprotein cholesterol. Am J Cardiol. 2004;93(2):219–220. doi:10.1016/j.amjcard.2003.09.045
56. Kanbay M, Gür G, Yücel M, Yilmaz U, Boyacioğlu S. Does eradication of Helicobacter pylori infection help normalize serum lipid and CRP levels? Dig Dis Sci. 2005;50(7):1228–1231. doi:10.1007/s10620-005-2764-9
57. Elizalde JI, Piqué JM, Moreno V, et al. Influence of Helicobacter pylori infection and eradication on blood lipids and fibrinogen. Aliment Pharmacol Ther. 2002;16(3):577–586. doi:10.1046/j.1365-2036.2002.01202.x
58. Zhang L, Gail MH, Wang YQ, et al. A randomized factorial study of the effects of long-term garlic and micronutrient supplementation and of 2-wk antibiotic treatment for Helicobacter pylori infection on serum cholesterol and lipoproteins. Am J Clin Nutr. 2006;84(4):912–919. doi:10.1093/ajcn/84.4.912
59. Wald NJ, Law MR, Morris JK, Bagnall AM. Helicobacter pylori infection and mortality from ischaemic heart disease: negative result from a large, prospective study. BMJ. 1997;315(7117):1199–1201. doi:10.1136/bmj.315.7117.1199
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
