Back to Journals » International Journal of General Medicine » Volume 16
Effect of Emergency Percutaneous Coronary Intervention Combined with Sacubitril and Valsartan on the Cardiac Prognosis in Patients with Acute Myocardial Infarction
Authors Fan H, Wang Y, Wang X, Dong X, Shao X, Yang F
Received 20 September 2022
Accepted for publication 29 November 2022
Published 7 February 2023 Volume 2023:16 Pages 499—505
DOI https://doi.org/10.2147/IJGM.S389216
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hai Fan,1 Yuesong Wang,1 Xuezhong Wang,1 Xuebin Dong,1 Xuwu Shao,1 Fei Yang2
1Department of Cardiovascular Medicine, People’s Hospital of Maanshan, Maanshan, Anhui, People’s Republic of China; 2Department of Laboratory, People’s Hospital of Maanshan, Maanshan, Anhui, People’s Republic of China
Correspondence: Hai Fan, Tel +86-18255552083, Email [email protected]
Purpose: This study aimed to investigate the effect of emergency percutaneous coronary intervention (PCI) combined with sacubitril-valsartan (Entresto) on the cardiac prognosis in patients with acute myocardial infarction (AMI).
Patients and Methods: A total of 78 AMI patients who were treated in our hospital between January 2020 and September 2021 were included and randomly divided into treatment group and control group (n=39 per group). In the control group, patients were treated with primary PCI combined with irbesartan; in the treatment group, patients were treated with primary PCI combined with Entresto; pharmacotherapy lasted for 3 months. The left ventricular remodeling indexes, serum N-terminal B-type natriuretic peptide precursor (NT-proBNP), serum homocysteine (HCY), cystatin C (CysC) and results of 6-minute walk test (6MWT) before and after treatment were compared between two groups. The incidence of major adverse cardiovascular events (MACE) was determined and compared between them.
Results: (1) Before treatment, there were no marked differences in the left ventricular end-systolic diameter (LVESD), left ventricular end-diastolic diameter (LVEDD), interventricular septum thickness (IVST), NT-proBNP, left ventricular ejection fraction (LVEF), HCY, CysC, and results of 6MWT between two groups (P> 0.05). After treatment, the LVEDS, LVEDD, NT-proBNP, HCY and CysC in the control group were significantly higher than in the treatment group (P< 0.05). The recovery of LVEF and 6MWT in the treatment group was significantly better than in the control group (P< 0.05). After treatment, there was no significant difference in the IVST between two groups (P> 0.05). (2) The incidence of MACE in the control group was significantly higher than in the treatment group (P< 0.05).
Conclusion: Compared with irbesartan, Entresto can further improve the cardiac function, prevent ventricular remodeling, and further optimize the clinical efficacy of PCI in AMI patients.
Keywords: percutaneous coronary intervention, sacubitril-valsartan, acute myocardial infarction, ventricular remodeling
Introduction
Acute myocardial infarction (AMI) is a common cardiovascular disease, especially in the middle-aged and elderly people. The clinically defined type I AMI refers to the large-area myocardial ischemia necrosis caused by thrombus induced arterial occlusion due to the rupture of atherosclerotic plaques of any cause in the presence of pre-existing atherosclerosis.1 Emergency percutaneous coronary intervention (PCI) has been widely employed for the emergency treatment of AMI and can help quickly recover the myocardial reperfusion, which thereafter reduces the infarct size and improves left ventricular function.2 However, after PCI, some patients will still develop heart failure, which is symptomatic. Sacubitril valsartan (Entresto) is a new type of drug for the treatment of heart failure with favorable efficacy.3 The PARADIGM-HF trial has proved that Entresto is more effective than traditional angiotensin converting enzyme inhibitor/angiotensin receptor antagonist (angiotensin converting enzyme inhibitor/angiotensin receptor antagonist, ACEI/ARB) in the treatment.4 Studies have confirmed that Entresto can improve the cardiac function and prognosis of patients with heart failure secondary to AMI. However, whether the Entresto is more effective than traditional ACEI/ARB in AMI patients without heart failure who underwent primary PCI is still poorly understood. In the present study, 78 AMI patients without heart failure who received primary PCI in our hospital were recruited, and the effects of Entresto on the cardiac function, ventricular remodeling, major adverse cardiovascular events (MACE), homocysteine (HCY) and cystatin C (CysC) were investigated. Our findings aimed to elucidate the advantages of Entresto over traditional ACEI/ARB in AMI patients without heart failure.
Materials and Methods
Patients
Inclusion criteria were as follows: (1) Patients were diagnosed with AMI according to the diagnostic criteria for AMI in the 2019 Guidelines for the Diagnosis and Treatment of Acute Myocardial Infarction”; (2) Patients were initially diagnosed with AMI; (3) Thrombolytic therapy was not administered before admission; (4) There was no history of other cerebrovascular diseases; (5) There were no contraindications to anti-platelet aggregation. Exclusion criteria were as follows: (1) EF was <40% on cardiac Doppler ultrasound; (2) patients had congenital coagulation dysfunction; (3) patients had severe injury to important organs (such as liver, kidney, heart); (4) patients were intolerant to irbesartan or Entresto.
Study Design
This study was approved by the Medical Ethics Committee of our hospital (No. 2019–003-002), and informed consent was obtained from patients or their relatives. And all procedures were complied with the criteria outlined in the Declaration of Helsinki (as revised in 2013). All the patients received PCI immediately after admission. In brief, aspirin at 300 mg and ticorrelor 180mg were administered orally before surgery. After local anesthesia with 2% lidocaine, the right radial artery was punctured and a 6F arterial sheath was placed. Then, 2000 U of unfractionated heparin and 200 μg of nitroglycerin were mixed in 10 mL of normal saline, followed by injection into the arterial sheath to avoid vascular spasm. Then, coronary angiography was performed after the catheter and guide wire were placed, and the detailed surgery protocol was personalized designed according to the results of the angiography. 78 patients were randomly divided into treatment group and control group. In the control group, patients received oral irbesartan (Huahai Pharmaceutical Co., Ltd. H20030016; Lot No. 0000017225) at 37.5–75 mg/d after PCI. The specific dose of irbesartan was dependent on the blood pressure control. When the blood pressure decreased and remained in the normal range, the dose of irbesartan was adjusted to 0.15 g/d. In the treatment group, Patients I received sacubitril valsartan (Novartis Pharmaceutical Co., Ltd. H20170363; Lot No. SDL680) at 25–100 mg once or twice daily. The dose was initiated at 25 mg and dependent on the blood pressure. When the patient was tolerant to the sacubitril valsartan, the dose could increase to 200 mg within 4 week twice daily. The pharmacotherapy lasted for a total of 3 months. The cardiac function, MACE, HCY and CysC were compared between two groups. Patients for the first time received 6MWT on the day of discharge, and the result was used as the score before pharmacotherapy. Three months later, the 6MWT was performed again and the result served as the score after pharmacotherapy.
Observations
Left Ventricular Remodeling
Three-dimensional echocardiography was used to examine the cardiac remodeling of patients with Philips intelligent echocardiography system (Q7C). The left ventricular end systolic diameter (LVESD), left ventricular end systolic diameter (LVESD), left ventricular end diastolic diameter (LVEDD) and interventricular septum thickness (IVST) were obtained through echocardiography. In addition, the serum levels of CysC and HCY were measured in the patients of two groups.
Cardiac Function
Before and after treatment, 5 mL of venous blood was collected from patients, and the serum was harvested after centrifugation at 3000 r/min. Serum NT-proBNP level was determined. The left ventricular ejection fraction (LVEF) was measured by three-dimensional echocardiography; The 6-minute walk test (6MWT) was performed and the results were recorded.
Prognosis
Patients received follow up for 3 months after discharge. All the patients completed the follow-up, and none was lost to follow-up. The incidence of major adverse cardiovascular events (MACE) was calculated in two groups. MACE includes rehospitalization due to heart failure, recurrent AMI, recurrent UA, malignant arrhythmia, repeat revascularization, and cardiac death.
Statistical Analysis
Statistical analysis was performed using SPSS version 25.0 software. Quantitative data are expressed as mean ± standard deviation (SD), and qualitative data expressed as percentage. The independent sample t-test was used for comparisons between two groups, and Chi square test was employed for comparison of qualitative data. A value of P<0.05 was considered statistically significant.
Results
General Characteristics
A total of 78 patients with AMI who were treated in our hospital between January 2020 and September 2021 were recruited into present study. Among the included patients, there were 33 patients diagnosed as non-ST elevation myocardial infarction (NSTEMI), and 45 as ST-elevation myocardial infarction (STEMI). All the patients received the primary PCI without delay or time-to-PCI. There were 45 males and 33 females with the mean age of 62.79 ± 6.49 years (range: 50–80 years). According to the treatments, the patients were divided into treatment group and control group (n=39 per group). There was no significant difference in the general characteristics of these patients (P>0.05) (Table 1).
 |
Table 1 General Characteristics of Patients in Two Groups |
Ventricular Remodeling and Cardiac Function in Two Groups Before and After Pharmacotherapy
Before pharmacotherapy, there were no marked differences in the LVESD, LVEDD, IVST, serum NT-proBNP level, LVEF and result of 6MWT between two groups. After pharmacotherapy, the LVESD, LVEDD and serum NT-proBNP level in the control group were significantly higher than in the treatment group (P<0.05). The IVST was comparable between two groups before and after pharmacotherapy (P>0.05) (Table 2 and Table 3).
 |
Table 2 Ventricular Remodeling of Patients in Two Groups Before and After Treatment |
 |
Table 3 Cardiac Function of Patients in Two Groups Before and After Treatment |
Serum Levels of HCY and CysC in Two Groups Before and After Pharmacotherapy
Before pharmacotherapy, there were no significant differences in the serum levels of HCY and CysC between two groups (P>0.05). After pharmacotherapy, the serum levels of HCY and CysC in the control group were markedly higher than in the treatment group (P<0.05) (Table 4).
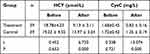 |
Table 4 Serum Levels of HCY and CysC of Patients in Two Groups Before and After Treatment |
Incidence of MACE in Two Groups
The incidence of MACE in the treatment group was significantly lower than in the control group (P<0.05) (Table 5).
 |
Table 5 MACE in Two Groups After 3-Month Follow-Up |
Discussion
In recent years, with the improvement of living standards, the incidence of cardiovascular diseases, especially myocardial infarction, has been increasing over year.5 Although the chest pain center has been promoted in China and the primary PCI can be routinely performed in the first-level tertiary hospitals in cities and counties, the mortality and disability of AMI are still at a high level, and the inflection point has not yet appeared.6 Currently, primary PCI for revascularization of affected vessels is still the optimal treatment for AMI.7–9 However, some patients will still experience heart failure, malignant arrhythmia, and even sudden death due to the myocardial necrosis and ventricular remodeling after AMI. Therefore, reducing myocardial necrosis, preventing ventricular remodeling, and improving cardiac function are crucial for reducing the mortality and disability of myocardial infarction.10 Although the routine treatments (such as Cardiotonic drugs, diuretics and vasodilators) may exert therapeutic effects on clinical symptoms to a certain extent, the improvement of cardiac prognosis and cardiac function are still limited. Thus, it is imperative to develop more effective drugs and therapeutic protocols to improve the cardiac function of AMI patients, therefore reducing their mortality and disability.
Irbesartan is a commonly used angiotensin II receptor antagonist in clinical practice. After orally administered, the drug can be hydrolyzed into active ingredients in the body, which then reduce the blood pressure and relieve the heart load to a certain extent. However, there is evidence showing that the traditional ACEI/ARB (such as irbesartan) fail to effectively block the excessive activation of the neuroendocrine system (a process related to heart failure), which greatly compromises the therapeutic effect on the heart failure.11 Entresto is a new type of anti-heart failure drug and the main components of Entresto are valsartan (an ARB) and AHU377 (a precursor of neprilysin inhibitor). It can effectively inhibit the type I angiotensin II receptor in AMI patients and target the sympathetic nerve endings to inhibit the secretion of norepinephrine and relieve the vascular and myocardial contractility in AMI patients.12 Moreover, Entresto can also effectively inhibit the proliferation of vascular endothelial cells, smooth muscle cells and cardiomyocytes and suppress the aldosterone secretion, therefore alleviating the ventricular remodeling in AMI patients.13–17
NT-proBNP is a long amino acid peptide chain secreted in case of heart failure, and it has been employed for the diagnosis of heart failure.18 The significant increase or decrease of serum NT-proBNP level also predicts the elevated risk of sudden death and hospitalization.19 6MWT is a common clinical examination for the systematic quantitative assessment of cardiac function and tolerance to activities in patients with myocardial infarction and heart failure, and it can also be used to predict the prognosis of patients with cardiovascular disease.20 HCY is an important risk factor for myocardial infarction, cerebral infarction, heart failure, hypertension and other diseases. Studies have shown that HCY mainly mediates oxidative stress by increasing the synthesis of oxygen free radicals in cells, causing damage to the heart, which further increases the incidence of heart failure after myocardial infarction.21 CysC is a marker of inflammation. It can activate the cysteine protease to cause damage to the cardiovascular endothelial cells, which not only aggravates coronary atherosclerosis and causes myocardial ischemia, but also lead to collagen deposition in the myocardial interstitium, therefore inducing ventricular remodeling and heart failure.22
This study investigated the effects of Entresto on the cardiac prognosis and ventricular remodeling of AMI patients after primary PCI. Our findings may provide evidence on the safe use of Entresto in clinical practice. Our results showed the LVEDS, LVEDD and serum NT-proBNP level in the control group were significantly higher than in the treatment group, the LVEF and increase in the distance on 6MWT were markedly lower than in the treatment group. These findings indicate that Entresto may further improve the cardiac function of AMI patients after primary PCI, and the ability of Entresto to prevent and reverse ventricular remodeling is superior to traditional ACEI/ARB (such as irbesartan). In addition, the new risk factors of cardiovascular diseases (serum HCY and CysC levels) were detected in these patients before and after pharmacotherapy. Our results further indicated that Entresto alleviated the oxidative stress and inflammation in AMI patients after primary PCI. In view of overall prognosis, the incidence of MACE in the control group was markedly higher than in the treatment group. This suggests that Entresto after primary PCI may improve the prognosis of AMI patients and other endpoint outcomes (such as death and recurrence).
Taken together, as compared to irbesartan, Entresto is more effective to improve the cardiac function and prevent/reverse ventricular remodeling in AMI patients, and further optimize the clinical efficacy of primary PCI.
Conclusion
Compared with irbesartan, Entresto can further improve the cardiac function, prevent ventricular remodeling, and further optimize the clinical efficacy of PCI in AMI patients.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology. 2019 Chinese society of cardiology (CSC) guidelines for the diagnosis and management of patients with ST segment elevation myocardial infarction. Chin J Cardiol. 2019;47(10):766–783. doi:10.3760/cma.j.issn.0253-3758.2019.10.003
2. Shen-Guo B. Comparison of Percutaneous Coronary Intervention (PCI) and intravenous thrombolytic therapy in patients with acute myocardial infarction. J Math Med. 2019;32(12):1762–1763.
3. Cun-fang C, Jia B, Shan J, et al. Clinical effect and prognosis of sacubitril-valsartan in treating heart failure patients with midrange ejection fraction. Chin J New Drugs Clin Remed. 2020;39(2):88–92.
4. Cannon JA, Shen L, Jhund PS, et al. Dementia-related adverse events in PARADIGM-HF and other trials in heart failure with reduced ejection fraction. Eur J Heart Fail. 2017;19(1):129. doi:10.1002/ejhf.687
5. Wachter R, Senni M, Senni M, et al. Initiation of sacubitril/valsartan in haemodynamically stabilised heart failure patients in hospital or early after discharge: primary results of the randomised TRANSI-TION study. Eur J Heart Fail. 2019;21(8):998–1007. doi:10.1002/ejhf.1498
6. Jie L, Yan Y, Hong-Yu S. Study on the effect of chest pain center construction on treatment efficiency and prognosis of acute myocardial infarction. J Clin Emerg. 2019;20(10):767–770.
7. Neumann FJ, SOUSA-UVA M, Ahlsson A, et al. 2018 ESC/ EACTS guidelines on myocardial revascularization. The task force on myocardial revascularization of the European society of cardiology (ESC) and European Association for cardio-thoracic surgery (EACTS). G Ital Cardio. 2019;20(7/8S1):1S–61. doi:10.1714/3203.31801
8. Qi D, Shu-Hong W, Ye-zi F, et al. Risk factors of slow / no reflow in patients with acute ST-segment elevation myocardial infarction during direct percutaneous coronary intervention. Chin J Evid-Bases Cardiovasc Med. 2020;12(3):364–369.
9. Li P, Ruan JW, Liu M, et al. Thrombus aspiration catheter improve the myocardial reperfusion of STEMI patients with high thrombus load during the emergency PCI operation. J Cardio-Thorac Surg. 2019;14(1):172.
10. Lee JM, Rhee TM, Hahn JY, et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J Am Coll Cardiol. 2018;71(8):844–856. doi:10.1016/j.jacc.2017.12.028
11. Nakano Y, Matoba T, Tokutome M, et al. Nanoparticle-mediated delivery of irbesartan induces cardioprotection from myocardial ischemia-reperfusion injury by antagonizing monocyte-mediated inflammation. Sci Rep. 2016;6:29601. doi:10.1038/srep29601
12. Qi-dong W, Mu-qiao L. Effect of sacubitril valsartan on cardiac function in patients with acute ST-segment elevation myocardial infarction of the anterior wall complicated with heart failure. Acad J Guangzhou Med Colle. 2019;47(1):92–95.
13. Qing G, Guo-qing L, Qiong G, et al. Recombinant human brain natriuretic peptide sacubitril/valsartan by sequential therapy improves acute heart failure. Pract Med. 2021;37(7):919–923.
14. Badae NM, Naggar AE, Sayed SE. Could cardioprotective effect of ACE2 activator “diminazene aceturate” is more potent than ACE inhibitor “Enalapril” on acute myocardial infarction in rats? Can J Physiol Pharmacol. 2019;96(8):1–12.
15. Chong D, Long-Long H, Kai Z, et al. Treatment comparison between actual dose of sacubitril-valsartan and target dose of ACEI in patients with heart failure with reduced ejection fraction: a real-world cohort study. Pract Med. 2020;36(22):3084–3093.
16. Wen H, Ji-huan Q, Lang H, et al. Clinical effect of sacubitril valsartan in treating heart failure patients with mid-range ejection fraction. Chin Heart J. 2020;32(2):135–139.
17. Wachter R, Fonseca AF, Balas B, et al. Real‐world treatment patterns of sacubitril/valsartan: a longitudinal cohort study in Germany. Eur J Heart Fail. 2019;21:1.
18. Lin-lin H, Bang-ning W, Jun F, et al. Correlation of preoperative plasma NT-proBNP level with slow / no blood flow and short-term prognosis after emergency PCI in patients with acute myocardial infarction. Guizhou Medl J. 2019;43(12):1939–1940.
19. Zhi-di L. Clinical observation of sakubattral and valsartan sodium tablets in the treatment of heart failure and its effect on cardiac function and serum BNP level. Chin J Primary Med Pharm. 2020;27(5):586–590.
20. Jin P, Bin-yue Z, Hui-yong D, et al. Clinical analysis of Sacubitril-Valsartan in patients with clinical diastolic heart failure. Pract Med. 2021;37(11):1461–1465.
21. Cohen E, Margalit I, Shochat T, et al. Gender differences in homocysteine concentrations, a population-based cross-sectional study. Nutr Metab Cardiovasc Dis. 2019;29(7):9–14. doi:10.1016/j.numecd.2018.09.003
22. Lin L, Jin L, Chuang H, et al. Clinical value of detection of high-sensitivity C-reactive protein and cystatin C in patients with ventricular remodeling after acute myocardial infarction. Hebei Med. 2019;25(12):2045–2049.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
