Back to Journals » International Journal of Women's Health » Volume 15
Effect of Elevated Progesterone Levels on hCG Trigger Day on Clinical Pregnancy Outcome in Short-Acting GnRHa Downregulated Cycles
Authors Jiang J, Kong N , Shi Q , Yan Y, Shen X, Mei J, Sun H, Huang C
Received 5 October 2023
Accepted for publication 14 December 2023
Published 21 December 2023 Volume 2023:15 Pages 1971—1979
DOI https://doi.org/10.2147/IJWH.S437794
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Jingwen Jiang,1– 3,* Na Kong,1– 3,* Qingqing Shi,1– 3,* Yuan Yan,1– 3 Xiaoyue Shen,1– 3 Jie Mei,1– 3 Haixiang Sun,1– 3 Chenyang Huang1– 3
1Center for Reproductive Medicine and Obstetrics and Gynecology, Drum Tower Clinic Medical College of Nanjing Medical University, Nanjing, 210008, People’s Republic of China; 2Reproductive Medicine Center, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, 210008, People’s Republic of China; 3Center for Molecular Reproductive Medicine, Nanjing University, Nanjing, 210008, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Haixiang Sun; Chenyang Huang, Center for Reproductive Medicine and Obstetrics and Gynecology, Drum Tower Clinic Medical College of Nanjing Medical University, Nanjing, 210008, People’s Republic of China, Tel +8625-8310-6666-70261, Fax +8625-8310-7188, Email [email protected]; [email protected]
Background: Previous studies suggested higher serum progesterone (P) levels were strongly associated with a lower clinical pregnancy rate (CPR) for in vitro fertilization-embryo transfer (IVF-ET). However, the effect of increased serum P levels on the day of human chorionic gonadotropin (hCG) administration on clinical outcomes in short-acting gonadotropin-releasing hormone agonist (GnRHa) downregulated IVF-ET cycles remains unclear.
Methods: We conducted a retrospective cohort study from January 2017 to December 2021, which included a total of 1664 patients receiving their first short-acting GnRHa IVF-ET cycles at our reproductive medicine centre of Nanjing Drum Tower Hospital. The smooth curve fitting and interaction analysis were employed to analyse the association between the CPR and the serum P levels with different embryo types (cleavage-stage embryo or blastocyst). In addition, total cycles were grouped according to different P levels on the trigger day of hCG administration for further analysis.
Results: The CPR of patients with increased serum P level (higher than 1.5 ng/mL) on the hCG day did not decrease. A smoothing curve fitting showed that the CPR did not change obviously with the increase in serum P levels. Subgroup analysis of different types of embryos transferred showed that no correlation was observed between the CPR and serum P levels on the day of hCG administration in cleavage-stage embryo transfer cycles. However, the CPR of patients receiving blastocyst transfer showed a downward trend with the increase in serum P levels. At the same time, an interaction analysis also confirmed that the CPR of blastocyst transfer was more likely to be affected by elevated serum P levels on the hCG day.
Conclusion: In the luteal phase short-acting GnRHa downregulated IVF-ET cycles, the elevated serum P levels on the hCG day did not affect the CPR of cleavage-stage embryo transfer but reduced the CPR of blastocyst transfer.
Keywords: short-acting GnRHa, elevated progesterone level, hCG trigger day, clinical pregnancy rate, blastocyst transfer
Background
Oestrogen and progesterone levels jointly regulate the synchronous development and receptivity of endometrium.1,2 Progesterone (P) is an important factor to promote the transformation of endometrium to secretory phase, while the early increase of the P level on the hCG trigger day in controlled ovarian hyperstimulation (COH) cycles will adversely affect the transformation of endometrium and endometrial receptivity and inhibit embryo implantation.3–8 Most previous studies suggested that elevated P levels would have a negative impact on the clinical outcome of in vitro fertilization/intracytoplasmic sperm injection and embryo transfer (IVF/ICSI-ET) cycles.7,9–12 However, there are also several studies suggesting that it has no adverse effect on the clinical outcome of IVF/ICSI cycles.13–15 Therefore, the influence of serum P levels on the hCG day on clinical outcome remains controversial.
Previous studies suggested that the increase in serum P level (>1.5 ng/mL) on the day of hCG administration was related to the significant decrease in the persistent pregnancy rate after the assisted reproductive technology (ART) cycle.16 The increase of serum P level on the hCG day occurred in about 6–30% COH cycles. Papanikolaou et al17 revealed that when the cleavage-stage embryos were transferred, the increased P (>1.5 ng/mL) had a significant negative impact on the pregnancy outcome. However, no negative effects on blastocyst transfer were observed, suggesting that the selection of blastocyst transfer may overcome the adverse effects of elevated P levels. On the contrary, in our recent study, we found that the increase in serum P levels on the hCG day in long-acting GnRHa downregulated IVF-ET cycles had adverse effects on blastocyst transfer. To explore whether the same phenomenon exists in patients who receive short-acting GnRHa downregulated IVF-ET cycles, we have conducted a retrospective study at our reproductive medicine centre from 2017 to 2021. We further explored whether the increase of P levels on the hCG day had different effects on the clinical outcomes of different types of embryos (cleavage-stage embryo or blastocyst) transfer.
Methods
Study Population
Our retrospective cohort study was focused on patients undergoing their first short-acting GnRHa IVF-ET cycles. All enrolled participants received the ART treatment from 2017 to 2021 at our reproductive medicine centre of Nanjing Drum Tower Hospital. Each couple was informed of the possibility of using their basic information and treatment data during the IVF cycle for subsequent study. The study approval was obtained from Nanjing Drum Tower Hospital ethics committee, and patients were provided written informed consent. The exclusion criteria were as follows: (1) over 45 years old; (2) intracytoplasmic sperm injection (ICSI) cycles; (3) combined hydrosalpinx or lesions of the uterine cavity, such as endometrial polyps and endometrial dysplasia; (4) adenomyosis or endometriosis. 1664 IVF-ET cycles were enrolled in this study.
Luteal Phase Short-Acting GnRHa Long Protocol for Controlled Ovarian Stimulation
A short-acting GnRHa (triptorelin acetate, decapeptyl, Ferring GmbH, 0.1 mg) was administered in 5 to 7 days after ovulation. The patients received GnRHa injection every day for 14 days (0.1 mg i.h. q.d. for 10 days and 0.05 mg i.h. q.d. for 4 days). The levels of sex hormone, such as oestradiol (E2), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and P, and the diameter and number of follicles were measured after GnRHa downregulation. After meeting the criteria of pituitary downregulation, recombinant FSH (rFSH, Gonal-F, Merck Sereno, 75–300 IU i.h.) was injected according to the female age, body mass index (BMI), basal FSH level, and antral follicle count (AFC). Recombinant LH (rLH, Luveris, Merck Sereno, 75–150 IU i.h.) or human menopausal gonadotropin (HMG, Menotropins for Injection, Livzon Pharm, 75–300 IU i.m.) was added or not. The dosage of gonadotropin (Gn) was adjusted based on follicular growth rate and serum hormone (FSH, LH, E2, P) levels. Recombinant hCG (rhCG, Merck Sereno, 250 μg, i.h.) or hCG (Chorionic Gonadotropin for Injection, Livzon Pharm, 10,000 IU, i.m.) was injected to trigger ovulation as 1–2 dominant follicles reached 18 mm. The oocytes were collected 36–38 hours after triggering. Mature oocytes (metaphase II, MII) were fertilization and cultured to different embryo stages (cleavage-stage embryos or blastocysts). The whole embryo freezing scheme was conducted for the increased serum P level (>2.5 ng/mL) on the trigger day.
Embryo Transfer and Pregnancy Detection
The abdominal ultrasound-guided fresh embryos transfer was conducted for patients without abnormal conditions. The cleavage-stage embryos were transferred on the 3rd day and blastocysts were transferred on the 5th day after oocyte retrieval. Serum β-human chorionic gonadotropin (β-hCG) levels were detected 12–14 days after embryo transfer to determine biochemical pregnancy. Ultrasound examination was performed 28–30 days after embryo transfer in patients with positive β-hCG results to confirm the clinical pregnancy, which was defined as the presence of a gestational sac. Luteal support was maintained for 55–60 days after embryo transfer of pregnant patients. The patients were continuously followed up to assess any abnormalities in pregnancy and until live birth. The patients were continuously followed up until the birth of the newborn to evaluate the abnormal conditions of persistent pregnancy and live birth.
Statistical Analysis
To analyse the association between serum P levels on the hCG day and the CPR in short-acting GnRHa downregulated IVF-ET cycles, a smooth curve fit analysis was conducted. According to the reported cut-off value of P levels (1.5 ng/mL), all cycles were divided into two groups (Group A: P ≤ 1.5 ng/mL; Group B: P > 1.5 ng/mL). Propensity score matching was conducted for the lower number of patients in Group B. According to different types of transferred embryos, further subgroup analysis was carried out, and then, an interaction analysis was taken to confirm the influence of embryo stages on the association between P levels and CPR. All variables are presented as the mean ± standard deviation (SD). P < 0.05 was considered statistically significant. Our analyses were performed with R software version 3.6.0 (http://www.R-project.org) and EmpowerStats software (www.empowerstats.com, X&Y solutions, Inc. Boston MA).
Results
Relationship Between Serum P Levels on the hCG Day and the CPR
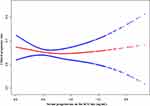
A smooth curve fitting revealed that the CPR did not change as the serum P level on the hCG day increased (Figure 1). All data were divided into two groups: Group A, P levels less than or equal to 1.5 ng/mL, and Group B, P levels greater than 1.5 ng/mL (Table 1). The female age, BMI, basal FSH levels, AFC, duration of infertility and Gn stimulation duration were similar in these two groups. But total dose of Gn was greater in Group A. The serum P level on the trigger day was significantly higher in Group B than that in Group A (1.78 ± 0.22 vs 0.60 ± 0.33 ng/mL). The number of oocytes retrieved was significantly higher in Group B, while the number of available embryos showed no difference in these two groups. There were no difference in the clinical outcomes (CPR, early miscarriage rate or live birth rate) between Group A and B. Because the number of patients in Group B was too small, the propensity score matching was employed to control confounding variables. Similarly, the CPR, early miscarriage rate and live birth rate were similar between the two groups after propensity score matching (Table S1).
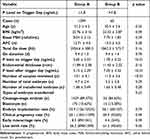 |
Table 1 Characteristics of Patients with Different Serum P Levels (1.5 ng/mL) on the hCG Day |
Effect of the Serum P Levels on the CPR for Different Types of Embryos Transfer
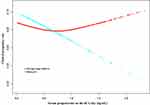
A smooth fitting curve was further constructed to investigate the association between serum P levels on the hCG day and the CPR for different types of embryos transfer. As shown in Figure 2, the red line, which represents patients receiving blastocyst transfer, showed a decline in the CPR with gradually increased serum P levels on the hCG day. In contrast, the CPR of cleavage-stage embryo transfer remained stable as the P level increasing. In addition, an interaction test between the types of embryos and the serum P levels on the CPR was statistically significant (Table 2, P = 0.04).
 |
Table 2 Effect Modification of P Levels on the hCG Day on CPR According to Different Types of Embryos Transferred |
Discussion
Our study explored the association between serum P levels on the hCG trigger day and the clinical outcomes of short-acting GnRHa IVF-ET cycles. The results showed that the increase in serum P level on the hCG day could significantly reduce the CPR of blastocyst transfer but had no significant effect on the CPR of patients receiving cleavage-stage embryo transfer.
Most previous studies suggested that the increased serum P level on the hCG day had an adverse impact on embryo implantation. A retrospective analysis showed that the pregnancy rate of patients with serum P level of 1.5 ng/mL or above was significantly lower and was not related to COH protocol.16 In addition, a meta-analysis included 63 studies with a total of more than 60,000 IVF/ICSI cycles, which showed that the increase in serum P levels in late follicular phase had a negative impact on the pregnancy rate of fresh embryo transfer.18 On the contrary, several studies suggested that the serum P level elevation on the trigger day showed no effect on clinical outcomes.19–21 To determine whether there is such phenomenon in the IVF cycles of our reproductive medicine centre, we first grouped all data according to different P levels on the hCG trigger day (cut-off value: 1.5 ng/mL). Our study, including 1664 IVF-ET cycles, showed that when the serum P level was greater than 1.5 ng/mL, the CPR of all patients was not significantly decreased. Compared with previous studies, our study only included patients received short-acting GnRHa for pituitary downregulation, and did not include the GnRH antagonist IVF cycles, in which patients usually received the whole embryo freezing strategy. Additionally, the clinical pregnancy rate reported in previous studies was fluctuating at 30–40%, lower than the conventional clinical pregnancy rate in our centre. This combined with the heterology of infertility patients from different areas might lead to these different conclusions. At present, with the continuous progress of ART technology, the cut-off value of serum P levels on the hCG day in fresh embryo transfer cycles needs to be constantly updated.
Previous studies believed that blastocyst transfer could better tolerate the problem of serum P levels elevation on the day of hCG trigger.17,22 Therefore, blastocyst transfer is considered as one of the solutions to improve the clinical outcomes of the increased serum P levels on the hCG day.17,22,23 In this regard, the recent study we published suggested that in the early follicular phase long-acting GnRHa downregulated IVF cycles, the CPR of patients receiving blastocyst transfer decreased with the increase of the P level on the hCG day, which showed that the blastocyst transfer could not conquer the negative effect of the elevated P level.24 In addition, the COH treatment used in our centre for fresh embryo transfer is mainly the long protocol with long-acting GnRHa or short-acting GnRHa for pituitary downregulation. Therefore, in this retrospective study, we also conducted a subgroup analysis on different types of transferred embryos. We observed a similar phenomenon in the short-acting GnRHa IVF-ET cycles: the adverse influence of elevated serum P levels on the day of hCG trigger on blastocyst transfer. At the same time, there are some previous studies supporting our view.23,25,26 These inconsistent conclusions remind us that we need to propose corresponding cut-off values of serum P levels for different types of transferred embryos. Therefore, we elementarily explored the potential serum P cut-off value to provide theoretical basis for clinical fresh embryo transfer strategies. When the serum P level is greater than 0.7 ng/mL, the red line (blastocyst transfer) is below the blue line (cleavage-stage embryo transfer) (Figure 2). We re-grouped the serum P levels on the day of hCG trigger (cut-off value: 0.7 ng/mL) and conducted the interaction analysis again for these two groups. The results suggested that when the serum P level >0.7ng/mL, blastocyst transfer is more vulnerable to the adverse effect of the elevated P level on the hCG day (Table S2), suggesting that cleavage-stage embryo transfer may be a better choice in this condition. However, this hypothesis of P cut-off value and embryo selection for transfer needs to be verified through further prospective studies. Why is blastocyst transfer more susceptible to the increased P levels than cleavage-stage embryo transfer? Studies suggested that increased P levels had adverse effects on the endometrial receptivity.4–6 The increased P level in advance makes the transformation of endometrium to secretory phase earlier,4 which leads to the time shift of implantation window and affects embryo implantation. We usually scheduled blastocyst transfer on the fifth day after egg retrieval. The early transformation of the endometrium may lead to the closure of the embryo implantation window at this time, thus causing the failure of blastocyst implantation. The time of embryo transfer at cleavage stage is the third day after egg retrieval, which is easier to match the implantation window of endometrium. In our two studies, we found that the predicted P cut-off value of the long-acting GnRHa IVF cycle is higher than that of the short-acting GnRHa IVF cycle. Previous studies suggested that the pre-treatment of long-acting GnRHa was conducive to the establishment of endometrial receptivity, and the endometrial receptivity of long-acting GnRHa IVF cycle is better than that of short-acting GnRHa IVF cycle.27,28 We speculate that this may be the possible reason for the different predicted P cut-off values of these two COH protocols. Cleavage-stage embryos transfer has certain advantages in short-acting GnRHa IVF-ET cycles.
The freeze-all policy is also considered as one of the strategies to address the elevated P levels on the hCG day.23 Some studies suggested that the clinical outcomes of freeze-thaw embryo transfer cycles were similar to or even exceed those of fresh cycle transfer.29–33 However, the potential risks of the FET cycle cannot be ignored. Studies suggested that there was an increased risk of complications in preeclampsia after the FET cycle,32 and FET protocols are linked to higher neonatal birth weight and lower risk of low birth weight than fresh embryo transfer.34,35 The effect of technique on children born from frozen embryos needs long-term follow-up, and more evidence is needed before larger-scale use of embryo freezing.
In addition to above two methods, nowadays there are many other potential strategies that help to achieve successful pregnancy. An increasing number of studies suggested that artificial intelligence (AI) might improve the diagnosis and treatment process of infertility and the clinical outcomes of ART. AI has the potential to be applied in many fields of reproductive medicine, such as follicle monitoring, endometrial receptivity assessment, embryo selection, and prediction of embryonic development after implantation.36 AI models based on patient clinical features have been trained to help make more effective clinical decisions.35 According to our studies, progesterone levels on the hCG day may serve as one of important parameters in predicting the outcome of ET, and further mining of AI functions may help find better prevention or solutions to this issue. It is worth noting that not only high quality embryos, proper implantation time and proper physical status are vital points in IVF procedure, psychological condition and many other aspects also counts a lot in a successful ART procedure.37
There are still some deficiencies in the current study. Previous studies showed that there were differences in the effect of the increased level of P concentration on the day of hCG trigger on clinical outcomes in women of different ovarian response,38,39 and the cut-off value of the P level was different.40 Only the COH protocol of short-acting GnRHa for pituitary down-regulation was included in our study. The ovarian response of these enrolled women is usually at a moderate or slightly low level in our centre. This conclusion is only applicable to the characteristic population. There is a significant difference in the number of patients receiving blastocyst transfer and cleavage-stage embryo transfer. In real life, these results are cautiously applicable. Retrospective design is the main limitation of this study. Further prospective studies are needed to clarify the impact of P level on the hCG day on clinical outcomes.
Conclusions
This retrospective study revealed that elevated serum P levels on the day of hCG trigger in the short-acting GnRHa pituitary downregulated IVF-ET cycle had an adverse effect on blastocyst transfer. When the serum P level was increased on the hCG day, cleavage-stage embryo transfer might be a more reasonable choice than blastocyst transfer, which needs to be confirmed by further prospective clinical studies.
Abbreviations
P, progesterone; COH, controlled ovarian hyperstimulation; CPR, clinical pregnancy rate; IVF-ET, in vitro fertilization-embryo transfer; hCG, human chorionic gonadotropin; GnRHa, gonadotropin-releasing hormone agonist; ICSI, intracytoplasmic sperm injection; ART, assisted reproductive technology; E2, oestradiol; FSH, follicle-stimulating hormone; LH, luteinizing hormone; BMI, body mass index; AFC, antral follicle count; HMG, human menopausal gonadotropin; Gn, gonadotropin; SD, standard deviation.
Data Sharing Statement
The datasets generated and analysed during the current study are not publicly available due to the special requirements of our hospital and our reproductive medicine center for the disclosure of patients’ clinical data but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This retrospective study received ethical approval from the ethics committee of Nanjing Drum Tower Hospital (No. 2023-067-01). All patient couples provided written informed consent. All methods were carried out in accordance with relevant guidelines and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Jingwen Jiang, Na Kong and Qingqing Shi should be regarded as joint First Authors.
Funding
This work was supported by the National Natural Science Foundation of China (81801530, 82071646), Reproductions Research Program of Young and Middle-aged Physicians and China Health Promotion Foundation (BJHPA-2022-SHZHYXZHQNYJ-LCH-002). There are no conflicts of interest.
Disclosure
The authors declare that they have no competing interests.
References
1. Ozturk S, Demir R. Particular functions of estrogen and progesterone in establishment of uterine receptivity and embryo implantation. Histol Histopathol. 2010;25(9):1215–1228. doi:10.14670/HH-25.1215
2. Cheng J, Sha Z, Li J, et al. Progress on the role of estrogen and progesterone signaling in mouse embryo implantation and decidualization. Reprod Sci. 2023;30(6):1746–1757. doi:10.1007/s43032-023-01169-0
3. Melo MA, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohi J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21(6):1503–1507. doi:10.1093/humrep/dei474
4. Li R, Qiao J, Wang L, Zhen X, Lu Y. Serum progesterone concentration on day of HCG administration and IVF outcome. Reprod Biomed Online. 2008;16(5):627–631. doi:10.1016/S1472-6483(10)60475-0
5. Nikas G, Makrigiannakis A. Endometrial pinopodes and uterine receptivity. Ann N Y Acad Sci. 2003;997(1):120–123. doi:10.1196/annals.1290.042
6. Labarta E, Martinez-Conejero JA, Alama P, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26(7):1813–1825. doi:10.1093/humrep/der126
7. Zhang J, Du M, Wu Y, Wei Z, Guan Y. Effect of serum progesterone levels on hCG trigger day on pregnancy outcomes in GnRH antagonist cycles. Front Endocrinol. 2022;13:982830. doi:10.3389/fendo.2022.982830
8. Kalakota NR, George LC, Morelli SS, Douglas NC, Babwah AV. Towards an improved understanding of the effects of elevated progesterone levels on human endometrial receptivity and oocyte/embryo quality during assisted reproductive technologies. Cells. 2022;11(9):1405. doi:10.3390/cells11091405
9. Papanikolaou EG, Pados G, Grimbizis G, et al. GnRH-agonist versus GnRH-antagonist IVF cycles: is the reproductive outcome affected by the incidence of progesterone elevation on the day of HCG triggering? A randomized prospective study. Hum Reprod. 2012;27(6):1822–1828. doi:10.1093/humrep/des066
10. Jiang W, Li D, Zhu L, et al. Elevated serum progesterone levels on the hCG trigger day have a negative impact on the live birth rate in the first fresh IVF-ET cycle. J Obstet Gynaecol. 2022;42(8):3503–3508. doi:10.1080/01443615.2022.2151345
11. Huang C, Shen X, Shi Q, et al. Adverse impact of elevated serum progesterone and luteinizing hormone levels on the hCG trigger day on clinical pregnancy outcomes of modified natural frozen-thawed embryo transfer cycles. Front Endocrinol. 2022;13:1000047. doi:10.3389/fendo.2022.1000047
12. Lepage J, Keromnes G, Epelboin S, Luton D, Yazbeck C. Premature progesterone rise on day of hCG negatively correlated with live birth rate in IVF cycles: an analysis of 1022 cycles. J Gynecol Obstet Hum. 2019;48(1):51–54. doi:10.1016/j.jogoh.2018.05.005
13. Martinez F, Coroleu B, Clua E, et al. Serum progesterone concentrations on the day of HCG administration cannot predict pregnancy in assisted reproduction cycles. Reprod Biomed Online. 2004;8(2):183–190. doi:10.1016/S1472-6483(10)60514-7
14. Doldi N, Marsiglio E, Destefani A, Gessi A, Merati G, Ferrari A. Elevated serum progesterone on the day of HCG administration in IVF is associated with a higher pregnancy rate in polycystic ovary syndrome. Hum Reprod. 1999;14(3):601–605. doi:10.1093/humrep/14.3.601
15. Wu Z, Dong Y, Ma Y, et al. Progesterone elevation on the day of hCG trigger has detrimental effect on live birth rate in low and intermediate ovarian responders, but not in high responders. Sci Rep. 2019;9(1):5127. doi:10.1038/s41598-019-41499-1
16. Bosch E, Labarta E, Crespo J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod. 2010;25(8):2092–2100. doi:10.1093/humrep/deq125
17. Papanikolaou EG, Kolibianakis EM, Pozzobon C, et al. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Sterility. 2009;91(3):949–952. doi:10.1016/j.fertnstert.2006.12.064
18. Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19(5):433–457. doi:10.1093/humupd/dmt014
19. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96(2):344–348. doi:10.1016/j.fertnstert.2011.05.050
20. Yding Andersen C, Bungum L, Nyboe Andersen A, Humaidan P. Preovulatory progesterone concentration associates significantly to follicle number and LH concentration but not to pregnancy rate. Reprod Biomed Online. 2011;23(2):187–195. doi:10.1016/j.rbmo.2011.04.003
21. Tanada MS, Yoshida IH, Santos M, et al. The impact of high progesterone levels on the day of HCG administration in assisted human reproduction treatments. JBRA Assist Reprod. 2018;22(2):99–101. doi:10.5935/1518-0557.20180020
22. Huang Y, Wang EY, Du QY, et al. Progesterone elevation on the day of human chorionic gonadotropin administration adversely affects the outcome of IVF with transferred embryos at different developmental stages. Reprod Biol Endocrinol. 2015;13:82. doi:10.1186/s12958-015-0075-3
23. Corti L, Papaleo E, Pagliardini L, et al. Fresh blastocyst transfer as a clinical approach to overcome the detrimental effect of progesterone elevation at hCG triggering: a strategy in the context of the Italian law. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):73–77. doi:10.1016/j.ejogrb.2013.08.017
24. Kong N, Liu J, Jiang Y, et al. Adverse impact of elevated progesterone levels on human chorionic gonadotropin trigger day on blastocyst transfer outcomes in gonadotropin-releasing hormone agonist cycles. Eur J Obstet Gynecol Reprod Biol. 2022;276:107–112. doi:10.1016/j.ejogrb.2022.07.007
25. Ochsenkuhn R, Arzberger A, von Schonfeldt V, et al. Subtle progesterone rise on the day of human chorionic gonadotropin administration is associated with lower live birth rates in women undergoing assisted reproductive technology: a retrospective study with 2555 fresh embryo transfers. Fertil Sterility. 2012;98(2):347–354.
26. Elgindy EA, Abou-Setta AM, Mostafa MI. Blastocyst-stage versus cleavage-stage embryo transfer in women with high oestradiol concentrations: randomized controlled trial. Reprod Biomed Online. 2011;23(6):789–798. doi:10.1016/j.rbmo.2011.08.011
27. Song J, Duan C, Cai W, Wu W, Lv H, Xu J. Comparison of GnRH-a prolonged protocol and short GnRH-a long protocol in patients with thin endometrium for assisted reproduction: a retrospective cohort study. Drug Des Devel Ther. 2020;14:3673–3682. doi:10.2147/DDDT.S270519
28. Liu Y, Ma L, Zhu M, Yin H, Yan H, Shi M. STROBE-GnRHa pretreatment in frozen-embryo transfer cycles improves clinical outcomes for patients with persistent thin endometrium: a case-control study. Medicine. 2022;101(31):e29928. doi:10.1097/MD.0000000000029928
29. Maheshwari A, Pandey S, Amalraj Raja E, Shetty A, Hamilton M, Bhattacharya S. Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Human Reproduction Update. 2018;24(1):35–58. doi:10.1093/humupd/dmx031
30. Sciorio R, Esteves SC. Clinical utility of freeze-all approach in ART treatment: a mini-review. Cryobiology. 2020;92:9–14. doi:10.1016/j.cryobiol.2019.11.041
31. Duarte-Filho OB, Podgaec S. Freeze-all policy for in vitro fertilization in women with normal response to ovarian stimulation. Einstein. 2021;19:eAO6290. doi:10.31744/einstein_journal/2021AO6290
32. Chen ZJ, Shi Y, Sun Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. New Engl J Med. 2016;375(6):523–533. doi:10.1056/NEJMoa1513873
33. Zhu Y, Zhang F, Chen H, Sun X, Jiang F. The use of frozen embryos and frozen sperm have complementary IVF outcomes: a retrospective analysis in couples experiencing IVF/Donor and IVF/Husband. BMC Pregnancy Childbirth. 2022;22(1):776. doi:10.1186/s12884-022-05088-x
34. Gullo G, Basile G, Cucinella G, et al. Fresh vs. frozen embryo transfer in assisted reproductive techniques: a single center retrospective cohort study and ethical-legal implications. Eur Rev Med Pharmacol Sci. 2023;27(14):6809–6823. doi:10.26355/eurrev_202307_33152
35. Gullo G, Scaglione M, Cucinella G, et al. Neonatal outcomes and long-term follow-up of children born from frozen embryo, a narrative review of latest research findings. Medicina. 2022;58(9):1218. doi:10.3390/medicina58091218
36. Medenica S, Zivanovic D, Batkoska L, et al. The future is coming: artificial intelligence in the treatment of infertility could improve assisted reproduction outcomes-the value of regulatory frameworks. Diagnostics. 2022;12(12):2979. doi:10.3390/diagnostics12122979
37. Burgio S, Polizzi C, Buzzaccarini G, et al. Psychological variables in medically assisted reproduction: a systematic review. Prz Menopauzalny. 2022;21(1):47–63. doi:10.5114/pm.2022.114404
38. Griesinger G, Mannaerts B, Andersen CY, Witjes H, Kolibianakis EM, Gordon K. Progesterone elevation does not compromise pregnancy rates in high responders: a pooled analysis of in vitro fertilization patients treated with recombinant follicle-stimulating hormone/gonadotropin-releasing hormone antagonist in six trials. Fertil Sterility. 2013;100(6):1622–1623. doi:10.1016/j.fertnstert.2013.08.045
39. Requena A, Cruz M, Bosch E, Meseguer M, Garcia-Velasco JA. High progesterone levels in women with high ovarian response do not affect clinical outcomes: a retrospective cohort study. Reprod Biol Endocrinol. 2014;12(1):69. doi:10.1186/1477-7827-12-69
40. Xu B, Li Z, Zhang H, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Sterility. 2012;97(6):1321–1324. doi:10.1016/j.fertnstert.2012.03.014
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.