Back to Journals » Journal of Pain Research » Volume 16
Effect of E-PR-01 on Activity-Induced Acute Knee Joint Discomfort in Healthy Individuals: A Randomized, Placebo-Controlled, Double-Blind, Cross-Over Study
Authors Srivastava S , Girandola RN
Received 7 April 2023
Accepted for publication 12 June 2023
Published 23 June 2023 Volume 2023:16 Pages 2141—2153
DOI https://doi.org/10.2147/JPR.S412018
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Shalini Srivastava,1 Robert N Girandola2
1Department of Clinical Development, Enovate Biolife, Wilmington, DE, 19801, USA; 2Department of Human Biology, University of South California, Los Angeles, CA, USA
Correspondence: Shalini Srivastava, Enovate Biolife, 913 N Market Street, Suite 200, Wilmington, DE, 19801, USA, Tel +91-9619477885, Email [email protected]
Purpose: A randomized, double-blind, placebo-controlled cross-over study was conducted to investigate the efficacy and safety of E-PR-01, a proprietary formula containing Vitex negundo and Zingiber officinale, on knee joint discomfort due to pain.
Patients and Methods: Forty adults aged 20– 60 years with self-reported pain score of ≤ 30 mm at rest and ≥ 60 mm post-exertion on a 100-mm visual analog scale (VAS) were randomized in a 1:1 ratio to receive either the E-PR-01 (200 mg twice daily) or placebo for 5 days. The primary outcome was time to achieve meaningful pain relief (MPR) (≥ 40% reduction in post-exertion pain VAS score from baseline) post-single dose of intervention on day 1 compared to placebo. The secondary outcomes were post-exertion pain intensity difference (PID) at 2-, 3- and 4-hours and time-weighted sum of pain intensity difference (SPID) over 4 hours post single dose on day 1; post-exertion VAS score at 4 hours’ post-intervention on day 5; percentage of responders on day 1; and physical efficiency as assessed by the total duration of exercise sessions completed after single dose of IP compared to placebo.
Results: The average time to achieve MPR was 3.38 hours, 32.50% of participants achieved it in the E-PR-01 group post single-dose administration on day 1 as opposed to the placebo where no participant achieved MPR. There were significant intergroup differences in PID (− 23.58 vs 2.45 mm) and SPID (− 67.48 vs − 0.08 mm) at 4 hours of E-PR-01 and placebo administration on day 1. 95% of participants in the IP group experienced some degree of pain relief within 2 hours compared to 37.5% in the placebo group.
Conclusion: A single dose of E-PR-01 provided a statistically significant as well as clinically meaningful reduction in exercise-induced knee joint discomfort within 4 hours of administration.
Keywords: Vitex negundo, Zingiber officinale, joint discomfort, pain VAS, meaningful pain relief, pain intensity difference
Introduction
Joint pain is traditionally considered as disease of old age however in recent times more young adults are said to suffer from such discomfort. The major reason for joint pain is obesity, repetitive movements and inflammatory conditions. In individuals with high physical activity levels, the chondrocytes gradually start declining reactivity to growth factors leading to altered structure and decreased functional ability in collagen to accommodate stress.1 Generally such individuals resort to fast-acting pain relief medications, which often have unpleasant side effects. Several safer alternatives, such as nutraceuticals, are available in the market to improve joint health, including collagen supplements, glucosamine hydrochloride, chondroitin sulfate, hyaluronic acid, methylsulfonylmethane, vitamin D, and likewise. These supplements help reduce joint discomfort by reducing inflammation or protecting the cartilage in the joints. However, their onset of action is slow, and the research into these supplements has produced mixed results in terms of effect size due to several methodological issues.2,3 Numerous clinical studies have supported the efficacy of herbal or plant-based ingredients in managing joint discomfort.4–6 However, most of them have been studied for their effect on chronic pain conditions, such as osteoarthritis, while very few, like Curcumin, Capsaicin, and Ginger, have been studied for their role in acute pain conditions.7 This situation has created a need for an evidence-based fast-acting alternative for managing joint discomfort and thereby improving physical activity. Enovate Biolife has formulated a proprietary blend containing extracts of Vitex negundo leaves and Zingiber officinale rhizome to fill the gap of a safe and fast-acting pain-relieving alternative that any group of individuals can use without fearing the side effects. It has been hypothesized that this blend will have potent pain relieving effect as compared to the individual ingredients as different phytochemical tend to provide synergistic effect.8
The choice of individual components has been based on the available literature and in-house screening. Vitex negundo has been widely used as a medicinal plant and food in South Asian countries.9,10 The presence of several bioactives like phenolic glycosides, lignans, diterpenoids, and triterpenoids makes it a potent anti-oxidant, anti-inflammatory, and analgesic effect, as proved in several preclinical studies.10,11 However, to date, no human trial has been conducted to evaluate the pain-relieving effect of V. negundo in a diseased or healthy population.
Zingiber officinale (Ginger) rhizome, is also a well-known Asian spice with centuries of history of culinary use.12 It has been explicitly used as a dietary supplement. Several clinical studies have been conducted to investigate the effect of Ginger extract or whole powder on exercise-induced joint pain, muscle soreness, and inflammation.13–16 A recent review of clinical trials of Ginger concluded that its use for pain-lowering effect is safe and promising.17 Ginger has been granted “generally regarded as safe (GRAS)” status by the US Food and Drug Administration and is considered safe at dosages of up to 4 grams daily.18 Also, both plants are considered safe for consumption due to their long history of use in traditional medicine.
Therefore, the primary objective of this clinical trial was to determine the effect of a single dose of E-PR-01, a proprietary blend containing extracts of V. negundo leaf and Z. officinale rhizome, on the time taken to achieve meaningful pain relief (MPR) in exercise-induced joint discomfort. The secondary objectives were post-exertion pain intensity difference (PID) at 2-, 3- and 4-hours, the time-weighted sum of pain intensity difference (SPID) over 4 hours, the percentage of responders, and physical efficiency as assessed by the total duration of exercise sessions after a single dose of investigational product (IP) administration on day 1 compared to the placebo. The study results indicated that the single 200 mg dose of E-PR-01 effectively reduced exercise-induced joint pain within 4 hours of its administration.
Materials and Methods
Study Design
This study was designed as a 5-day, prospective, randomized, double-blind, placebo-controlled, cross-over (AB/BA design) clinical trial. The study was conducted between September 2021 and February 2022 at a single site in Mumbai, Maharashtra, India under supervision of a qualified health professional. Participants were randomly assigned E-PR-01 in intervention period one, followed by placebo in intervention period two, or placebo in intervention period one, followed by E-PR-01 in intervention period two.
The study protocol was approved by ACEAS, Independent Ethics Committee, Ahmedabad, India (CDSCO Reg. No. ECR/281/Indt/GJ/2017/RR-21, date: 04/02/2021 and OHRP US DHHS Reg. No. IRB00011046) vide Letter No.: VED/P-21/31/JUL/2021; date: 31/7/2021. The study complies with the Declaration of Helsinki, ICH-GCP, and Ethical Guidelines for Biomedical Research on Human Participants, 2006, issued by the Indian Council of Medical Research, India.
It was registered on clinicaltrials.gov (ID: NCT05052112). The investigators explained the objectives, procedures, risks, and benefits involved in the study to all the participants. Only participants willing to give written informed consent were recruited for the study. The study results have been reported as per the Consolidated Standards of Reporting Trials (CONSORT) statement (Table S1).
Participants
This study was conducted on 40 healthy, physically active men and women aged 20–60 years selected from an internal database of healthy volunteers. The participants had no or minimal pain at rest (VAS score ≤30 mm);19 however, they had a history of knee joint pain on physical stress (walking, running, cycling, and so on). Participants self-reported joint pain of ≥60 on a 100 mm VAS scale after walking on a treadmill using modified Naughton’s protocol.20,21 Other inclusion criteria were body mass index (BMI) ≥20 and ≤29.9 kg/m2, and willingness to abstain from the analgesics, anti-inflammatory and disease modifying drugs and supplements before inclusion in the study and throughout the study.
Individuals with a history of any form of arthritis, including those suffering from osteoarthritis, as per the American College of Rheumatology (ACR) diagnostic criteria,22 were planned to be excluded from the study. Other exclusion criteria were medical history of lower limb injury in the past six months, insomnia, restless leg syndrome, uncontrolled hypertension (systolic blood pressure (SBP) >139 mmHg and diastolic blood pressure (DBP) > 89 mmHg), type II diabetes mellitus, hyperacidity with at least one episode/week, migraine, clinically significant renal, hepatic, endocrine, biliary, gastrointestinal, pancreatic, or neurological disorders; knee surgery, replacement, or any non-knee surgical procedures. Participants with a history of regular use of anti-hypertensives or any joint health supplement and intra-articular injections in the past 6 months were not allowed to participate in the study. Furthermore, pregnant or lactating females, and those on oral contraceptives, were not included in the study.
Intervention
The study products were manufactured in compliance with all regulations and guidelines associated with good manufacturing practices and were supplied by Enovate Biolife. Each E-PR-01 gelatin capsule contained 200 mg of a proprietary blend containing extracts of V. negundo and Z. officinale, while the placebo capsules contained the same amount of microcrystalline cellulose.
The computer-generated randomisation chart using random block sizes of 4 with a 1:1 allocation rate for the two cross-over sequences (E-PR-01 followed by Placebo and vice-versa) was prepared by an independent statistician. The randomization chart was secured, saved, and maintained in the electronic trial master file with access to only designated personnel. The participants, the research team, and the investigator were blinded to the sequence allocation.
All the participants were administered the assigned study product at a dose of one capsule orally after a baseline exercise session and 1 capsule before dinner on Day 1, followed by one capsule daily after breakfast and before dinner for next four days. After a washout period of 5 days, the participants were allocated to the alternative intervention. The IP and placebo capsules were identical in appearance and were packed in a high-density polyethylene (HDPE) bottle labeled with unique identifiers for each participant according to the randomization chart.
Study Procedures
During the screening visit, the study procedures were thoroughly explained to the research participants in a language well understood by them, following which he/ she duly signed and dated informed consent. Demographic and baseline characteristics, such as weight, height, BMI, vitals (pulse rate and blood pressure), exercise, sleep, and medical history with prior and concomitant medication were recorded. A urine pregnancy test was performed for the female participants. Participants were asked to self-administer a 100-mm VAS to indicate the intensity of knee joint pain they experienced at rest. Subsequently, the participants performed a treadmill-based submaximal exercise test using the modified Naughton Protocol.21 In this study, the modified Naughton protocol was followed up to stage 5. It has been used in numerous studies to induce physical stress, detect ischemic abnormalities, and in trials studying exercise-aggravated pain.23–26 Participants marked their baseline knee joint pain intensity using the VAS within 5–10 minutes of ending the exercise protocol (Figure 1).
 |
Figure 1 Study procedures. |
All the other pharmacological and non-pharmacological therapies used for alleviating pain were prohibited in this study. Participants were instructed not to undergo any form of intense physical activity 48 hours before any scheduled visit and to maintain their usual physical exercise regime with no abrupt changes during the study.
During the randomization visit, the participants were again assessed for their perceived knee joint pain intensity at rest and after performing the treadmill test using pain VAS. Participants who fulfilled the pre-define randomization criteria, ie, pain VAS score ≤30 mm at rest and ≥60 mm post-exertion, were randomized into the study. Randomized participants were then instructed to consume their first dose and perform the treadmill-based exercise test at 2-hour, 3-hour, and 4-hour of IP consumption. The participants self-reported their knee joint pain intensity on pain VAS after every exercise session. The duration of each exercise session was recorded. The resting time between two consecutive exercise sessions was provided to avoid reporting high VAS scores due to muscle fatigue. Finally, the participants were asked to report on day 5 for the end of the study assessment. On day 5, the exercise session was conducted at 4 hours post-IP administration. IP compliance was checked by counting the number of capsules in the bottle brought by the participant.
Outcomes
Time to Pain Relief
Meaningful Pain Relief (MPR) was defined as the clinically relevant reduction27 in pain VAS score by ≥40% of the baseline score. In acute pain, it seems reasonable to anchor clinical relevance to the participants’ experience; hence meaningful pain relief and perceptible pain relief derived from self-reported pain intensity served as valid criteria.28 The study also explored the perceptible pain relief, which was considered as the timepoint when the participant first began to feel any pain-relieving effect from the study product.29
Pain Intensity Difference
Pain intensity difference was calculated as the difference between the pain VAS score reported after each exercise session and the pre-exercise/baseline score.30–32
Time-Weighted Sum of Pain Intensity Difference
The time-weighted SPID is used to summarize the intervention response over a clinically relevant period.33 It was calculated as
where ti=specific time interval, n=number of intervals, and PIDi=pain intensity difference for the specific time interval. The SPID over 4 hours of IP consumption after single dose of the product was compared to the placebo group.
Responder Analysis
For the present study, responders were defined as the number of participants who reported MPR from baseline on day 1. The proportion of responders was assessed and compared between the IP and placebo groups.
Physical Efficiency
The physical efficiency of each participant was evaluated using the total time spent exercising on day 1 and compared between the two study groups.
Pain VAS Score on Day 5
The sustained effect of IP on pain reduction was determined by the change in pain VAS scores from the baseline to Day 5, with at least 9 doses of product intake.
Safety Variables
Blood pressure and pulse rate were monitored throughout the study. The site team also monitored participants for any adverse drug reaction.
Statistical Analysis
The sample size for the present study was calculated assuming a minimal difference of 15 points in the pain VAS between groups at 3rd hour with 80% power and an alpha level of 0.05. Allowing a 20% dropout total of 40 participants were required to be randomized and crossed over both the arms in pre-determined sequence with at least 32 participants completing the study. The efficacy and safety outcomes were analyzed using the per-protocol population as all the participants randomized in the study completed the study. The data were visually assessed for normality. All continuous variables have been summarized by presenting the number of participants, mean, standard deviation (SD), and 95% confidence interval (CI). Categorical variables have been presented as frequencies and percentages. The continuous outcome variables were analyzed for within the group and between group comparisons by calculating change from baseline to the post-exertion scores reported after each exercise session. For continuous data, paired t-tests or analysis of covariance (intervention as a factor and baseline as a covariate) were used where appropriate. Chi-square/Fisher’s exact test was used for categorical variables to compare the data between groups. All statistical tests were two-sided and were performed with a significant level of 0.05 using R/R Foundation for Statistical Computing, Vienna, Austria, and XLSTAT Statistical and Data Analysis Solution, New York, USA.
Quality Assurance
The study was planned and conducted in compliance with the ICH-GCP guidelines. Both the investigator and the research team were GCP certified. There was a pre-approved monitoring and audit plan to ensure data quality.
Results
Overall, 40 participants were randomized in the study, and all completed the intervention period with more than 99% compliance.
Demographic and Baseline Characteristics
The male and female participants had a mean age of 45 years and an average BMI of 26 kg/m2 with an average on-and-off pain history of 22.5 months. The demographics and other characteristics of the participants were in line with the inclusion-exclusion criteria defined for the study, as shown in Table 1. Fifty participants were screened, out of which 10 were excluded due to: screen failures (n=8), drop-out (n=1) and withdrawal (n=1). The reasons for screen failures were as follows: a) participants had high blood pressure (n=3), b) participants had a pain VAS score post exercise below 60 (n=4), and c) participant’s ACR score was 4 (n=1). Thus, 40 participants were randomized. Twenty participants each were randomized to either the E-PR-01 group or the placebo group. After a follow-up on day 5, the participants underwent a washout period of 5±2 days. Post which, the participants of the E-PR-01 group were crossed over to placebo and vice-versa. After 5 days, a follow-up visit was again scheduled. All the participants completed the study and none were excluded from the analysis. The details of participant disposition are illustrated in Figure 2.
 |
Table 1 Demographics and Other Characteristics at the Screening Visit |
 |
Figure 2 Participant disposition. |
Time to Pain Relief
The mean time to achieve MPR in the E-PR-01 group was 3.38 (0.77) hours with 95% CI values of 2.92–3.85 whereas, in the placebo group, no participant could achieve MPR till 4 hours. The number and percentage of participants achieving MPR in the E-PR-01 group was 13 (32.50%), while the placebo group had zero achievers. Thus, there is a significant difference in the number of participants achieving MPR in the two groups (p <0.001) (Figure 3). Also, 95% of participants in the E-PR-01 group experienced perceptible pain relief as compared to 37.5% in the placebo group at 2 hours after the first dose of IP administration.
 |
Figure 3 Number of participants achieving MPR. Abbreviations: MPR, meaningful pain relief; No., number. |
Pain Intensity Difference
The post-exertion mean pain intensity difference at 2-, 3- and 4-hour after single-dose administration of E-PR-01 was statistically significant compared to the placebo group (all p=<0.001) on day 1. In the E-PR-01 group, there was a continuous reduction in post-exertion pain VAS scores from 19% at 2 hours to 35% at 4 hours post-IP administration from the baseline values, while in the placebo group, the pain VAS scores increased at 4 hours post-IP administration (4%) after an initial reduction at 2-hour (2%) (Table 2 and Table 3, Figure 4).
 |
Table 2 Summary of Pain VAS Score |
 |
Table 3 Summary of PID and SPID |
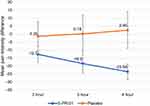 |
Figure 4 Mean pain intensity difference (mm) at day 1. |
Time-Weighted Sum of Pain Intensity Difference
The time-weighted sum of pain intensity difference was significantly more in the E-PR-01 group compared to the placebo group (p<0.0001) after single-dose administration (Table 3).
Responder Analysis
In the E-PR-01 group, the responders doubled with each passing hour on day 1 (post-exertion) 2 hours, 3 hours, 4 hours, and day 5 (post-exertion) (4 hours). However, in the placebo group, no responders were observed. After 4 hours post IP on day 1, there was a significant difference in the cumulative number of responders between both groups (p<0.0001). We also calculated responders on day 5 of the intervention period. A significant proportion of participants (70%) experienced meaningful pain relief after five days of IP consumption, while no one in the placebo group experienced meaningful pain relief (Table 4 and Figure 5).
 |
Table 4 Cumulative Number and Percentage of Responders on Days 1 and 5 |
 |
Figure 5 Percentage of responders on day 1 and day 5. |
Physical Efficiency
All the participants completed the exercise sessions till 4 hours post-IP on day 1 in both the study groups without any debilitating pain (defined as pain VAS score >90 mm). Additionally, on day 5, all the participants completed their exercise session without a problem.
Pain VAS Score on Day 5
Pain VAS scores were statistically comparable between the two groups at baseline (p>0.05). On day 5, a significant reduction (50%) in mean VAS scores from the baseline (0-hour post-exertion) scores was observed in the E-PR-01 group (p<0.001). In addition, this improvement in the pain scores in the E-PR-01 group was statistically significant (p<0.001) compared to the placebo group, where the baseline and day 5 scores almost remained the same, as shown in Table 5 and Figure 6.
 |
Table 5 Summary of Change in Pain VAS Scores from Day 1 to Day 5 |
Safety Outcomes
No adverse event was reported in the study groups during the entire study duration. This can be attributed to short study duration of the study.
Discussion
The present study successfully demonstrated the analgesic potential of E-PR-01, by reducing the exercise-induced knee joint pain up to a clinically meaningful magnitude compared to the placebo. The significant difference between the groups in the time to achieving MPR might be attributed to the temporal prostaglandin inhibiting property of V. negundo and Z. officinale extracts.12,34,35 It is worth noting that some of the participants in the E-PR-01 group could achieve MPR as early as 2-hours post single-dose administration. Also, perceptible pain relief was experienced in 95% of participants in the E-PR-01 group compared to 37.5% in the placebo group indicating lower number needed to treat (NNT). A lower NNT is generally associated with better outcome.36 A meta-analysis on 1512 participants concluded that approximately 60% of participants experienced at least 50% pain relief over 4 to 6 hours at any dose with diclofenac.37 In the current study, the perceptible pain relief in 95% participants can be considered important. E-PR-01 at a dose of 200 mg took a mean of 3.38 hours to achieve mean MPR as compared to a 4.46 hours taken by turmeric-boswellia formulation and 4.5 hours by acetaminophen in adults with acute musculoskeletal pain.38 A proprietary product, 5-Loxin containing a standardized extract of Boswellia serrata at a dose of 100 mg and 250 mg, exhibited a 10% and 12% reduction in pain VAS scores, respectively, after 7 days of administration.39 Another similar product Aflapin reduced the pain VAS scores by 12.8% after 7 days of administration.40 This shows that E-PR-01 can relieve joint discomfort faster than other herbal extracts.
Specific mechanisms that may be involved in the pain relieving E-PR-01 needs to be explored however [6]-Gingerol and [6]-shogaol have a high binding affinity for TRPV1 receptors thereby modulating release of Substance-P and subsequently providing analgesia.
The study did not have effect of placebo on post-exertion pain VAS scores over different time points probably owing to study’s cross-over design, which minimized the inter-individual variability and repeated measures in a shorter time period.41 However, further clinical studies are required to affirm these reasons and substantiate the efficacy claim of E-PR-01 on acute pain relief.
Conclusion
Overall, E-PR-01 significantly improved the exercise-induced acute knee joint pain at 2 hours which continued till 4 hours after a single dose of 200 mg. This pain relief was considered meaningful by the participants. It was found to be safer than the conventional treatments compared to the results obtained in similar studies.
Data Sharing Statement
The study data is available from the corresponding author upon reasonable request.
Acknowledgments
The authors are grateful to all the participants and the research team at Vedic Lifesciences for contributing to the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Enovate Biolife funded the study and provided the study products.
Disclosure
Shalini Srivastava is affiliated with Enovate Biolife. The other author reports no conflicts of interest in this work.
References
1. Ramasamy TS, Yee YM, Khan IM. Chondrocyte aging: the molecular determinants and therapeutic opportunities. Front Cell Dev Biol. 2021;9:625497. doi:10.3389/fcell.2021.625497
2. Colletti A, Cicero AFG. Nutraceutical approach to chronic osteoarthritis: from molecular research to clinical evidence. Int J Mol Sci. 2021;22(23):12920. doi:10.3390/ijms222312920
3. Miller LE, Fredericson M, Altman RD. Hyaluronic acid injections or oral nonsteroidal anti-inflammatory drugs for knee osteoarthritis: systematic review and meta-analysis of randomized trials. Orthop J Sports Med. 2020;8(1):2325967119897909. doi:10.1177/2325967119897909
4. Grando RL, Fierro IM. Medicinal plants used on arthritis treatment: an overview through patent analysis. J Pharmacogn Phytochem. 1999;6(6):1999–2003.
5. Yang L, Sibbritt D, Adams J. A critical review of complementary and alternative medicine use among people with arthritis: a focus upon prevalence, cost, user profiles, motivation, decision-making, perceived benefits and communication. Rheumatol Int. 2017;37(3):337–351. doi:10.1007/s00296-016-3616-y
6. Yatoo MI, Gopalakrishnan A, Saxena A, et al. Anti-inflammatory drugs and herbs with special emphasis on herbal medicines for countering inflammatory diseases and disorders - a review. Recent Pat Inflamm Allergy Drug Discov. 2018;12(1):39–58. doi:10.2174/1872213X1266618011515363
7. Jahromi B, Pirvulescu I, Candido KD, Knezevic NN. Herbal medicine for pain management: efficacy and drug interactions. Pharmaceutics. 2021;13(2):251. doi:10.3390/pharmaceutics13020251
8. Zhang L, Virgous C, Si H. Synergistic anti-inflammatory effects and mechanisms of combined phytochemicals. J Nutr Biochem. 2019;69:19–30. doi:10.1016/j.jnutbio.2019.03.009
9. Facciola S. Cornucopia: A Source Book of Edible Plants. Kampong publications; 1990.
10. Zheng CJ, Li HQ, Ren SC, et al. Phytochemical and pharmacological profile of Vitex negundo. Phytother Res. 2015;29(5):633–647. doi:10.1002/ptr.5303
11. Hu P, Li DH, Jia CC, et al. Bioactive constituents from Vitex negundo var. heterophylla and their anti-oxidant and α-glucosidase inhibitory activities. J Funct Foods. 2017;35:236–244. doi:10.1016/j.jff.2017.05.047
12. Wilson PB. Ginger (Zingiber officinale) as an analgesic and ergogenic aid in sport: a systemic review. J Strength Cond Res. 2015;29(10):2980–2995. doi:10.1519/JSC.0000000000001098
13. Matsumura MD, Zavorsky GS, Smoliga JM. The effects of pre-exercise ginger supplementation on muscle damage and delayed onset muscle soreness. Phytother Res. 2015;29(6):887–893. doi:10.1002/ptr.5328
14. Mashhadi NS, Ghiasvand R, Askari G, et al. Influence of ginger and cinnamon intake on inflammation and muscle soreness endued by exercise in Iranian female athletes. Int J Prev Med. 2013;4(Suppl 1):S11–S15.
15. Manimmanakorn N, Manimmanakorn A, Boobphachart D, Thuwakum W, Laupattarakasem W, Hamlin MJ. Effects of Zingiber cassumunar (Plai cream) in the treatment of delayed onset muscle soreness. J Integr Med. 2016;14(2):114–120. doi:10.1016/S2095-4964(16)60243-1
16. Black CD, Oconnor PJ. Acute effects of dietary ginger on quadriceps muscle pain during moderate-intensity cycling exercise. Int J Sport Nutr Exerc Metab. 2008;18(6):653–664. doi:10.1123/ijsnem.18.6.653
17. Rondanelli M, Fossari F, Vecchio V, et al. Clinical trials on pain lowering effect of ginger: a narrative review. Phytother Res. 2020;34(11):2843–2856. doi:10.1002/ptr.6730
18. Ryan JL, Morrow GR. Ginger. Oncol Nurs Edn. 2010;24(2):46.
19. Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1–2):95–97. doi:10.1016/s0304-3959(97)00005-5
20. Naughton J, Sevelius G, Balke B. Physiological responses of normal and pathological subjects to a modified work capacity test. J Sports Med Phys Fitness. 1963;3:201–207.
21. Mangione KK, Axen K, Haas F. Mechanical unweighting effects on treadmill exercise and pain in elderly people with osteoarthritis of the knee. Phys Ther. 1996;76(4):387–394. doi:10.1093/ptj/76.4.387
22. Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. doi:10.1002/art.1780290816
23. Girandola RN, Srivastava S, Loullis CC. A clinical trial comparing Lanconone® with ibuprofen for rapid relief in acute joint pain. Trials. 2016;17:189. doi:10.1186/s13063-016-1268-6
24. Aguiar J, Reis RP, Caria R, et al. Provas de esforço na terceira idade. Escolha do protocolo de esforço [Stress tests in old age. The choice of the stress protocol]. Acta Med Port. 1997;10(4):311–316. Portuguese.
25. Handler CE, Sowton E. A comparison of the Naughton and modified Bruce treadmill exercise protocols in their ability to detect ischaemic abnormalities six weeks after myocardial infarction. Eur Heart J. 1984;5(9):752–755. doi:10.1093/oxfordjournals.eurheartj.a061737
26. Starling MR, Crawford MH, O’Rourke RA. Superiority of selected treadmill exercise protocols predischarge and six weeks postinfarction for detecting ischemic abnormalities. Am Heart J. 1982;104(5 Pt 1):1054–1060. doi:10.1016/0002-8703(82)90440-9
27. Cepeda MS, Africano JM, Polo R, Alcala R, Carr DB. What decline in pain intensity is meaningful to patients with acute pain? Pain. 2003;105(1–2):151–157. doi:10.1016/s0304-3959(03)00176-3
28. Grilo RM, Treves R, Preux PM, Vergne-Salle P, Bertin P. Clinically relevant VAS pain score change in patients with acute rheumatic conditions. Joint Bone Spine. 2007;74(4):358–361. doi:10.1016/j.jbspin.2006.06.019
29. Daniels SE, Atkinson HC, Stanescu I, Frampton C. Analgesic efficacy of an Acetaminophen/Ibuprofen fixed-dose combination in moderate to severe postoperative dental pain: a randomized, double-blind, parallel-group, placebo-controlled trial. Clin Ther. 2018;40(10):1765–1776.e5. doi:10.1016/j.clinthera.2018.08.019
30. Moskowitz RW, Sunshine A, Hooper M, Olson NZ, Cawkwell GD. An analgesic model for assessment of acute pain response in osteoarthritis of the knee. Osteoarthritis Cartilage. 2006;14(11):1111–1118. doi:10.1016/j.joca.2006.05.004
31. Christensen S, Paluch E, Jayawardena S, Daniels S, Meeves S. Analgesic efficacy of a new immediate-release/extended-release formulation of ibuprofen: results from single- and multiple-dose postsurgical dental pain studies. Clin Pharmacol Drug Dev. 2017;6(3):302–312. doi:10.1002/cpdd.297
32. Boureau F, Schneid H, Zeghari N, Wall R, Bourgeois P. The IPSO study: ibuprofen, paracetamol study in osteoarthritis. A randomised comparative clinical study comparing the efficacy and safety of ibuprofen and paracetamol analgesic treatment of osteoarthritis of the knee or Hip. Ann Rheum Dis. 2004;63(9):1028–1034. doi:10.1136/ard.2003.011403
33. Farrar JT, Berlin JA, Strom BL. Clinically important changes in acute pain outcome measures: a validation study. J Pain Symptom Manag. 2003;25(5):406–411. doi:10.1016/s0885-3924(03)00162-3
34. Gill BS, Mehra R, Navgeet Kumar S, Kumar S. Vitex negundo and its medicinal value. Mol Biol Rep. 2018;45(6):2925–2934. doi:10.1007/s11033-018-4421-3
35. Dharmasiri MG, Jayakody JR, Galhena G, Liyanage SS, Ratnasooriya WD. Anti-inflammatory and analgesic activities of mature fresh leaves of Vitex negundo. J Ethnopharmacol. 2003;87(2–3):199–206. doi:10.1016/s0378-8741(03)00159-4
36. Andrade C. The numbers needed to treat and harm (NNT, NNH) statistics: what they tell us and what they do not. J Clin Psychiatry. 2015;76(3):e330–e333. doi:10.4088/JCP.15f09870
37. Derry P, Derry S, Moore RA, McQuay HJ. Single dose oral diclofenac for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(2):CD004768. doi:10.1002/14651858.CD004768.pub2
38. Rudrappa GH, Chakravarthi PT, Benny IR. Efficacy of high-dissolution turmeric-sesame formulation for pain relief in adult subjects with acute musculoskeletal pain compared to Acetaminophen: a randomized controlled study. Medicine. 2020;99(28):e20373. doi:10.1097/MD.0000000000020373
39. Sengupta K, Alluri KV, Satish AR, et al. A double blind, randomized, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Arthritis Res Ther. 2008;10(4):R85. doi:10.1186/ar2461
40. Sengupta K, Krishnaraju AV, Vishal AA, et al. Comparative efficacy and tolerability of 5-Loxin and AflapinAgainst osteoarthritis of the knee: a double blind, randomized, placebo controlled clinical study. Int J Med Sci. 2010;7(6):366–377. doi:10.7150/ijms.7.366
41. Vambheim SM, Daniali H, Flaten MA. Placebo effects on stress, but not on pain reports. A multi-experiment study. Front Psychol. 2021;12:639236. doi:10.3389/fpsyg.2021.639236
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


