Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Effect of Continuation-Maintenance Electroconvulsive Therapy on Hospitalization: A Retrospective Mirror-Image Study
Authors Sombatcharoen-non N, Yamnim T, Jullagate S, Ittasakul P
Received 5 April 2023
Accepted for publication 7 June 2023
Published 15 June 2023 Volume 2023:19 Pages 1427—1433
DOI https://doi.org/10.2147/NDT.S415878
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Nujaree Sombatcharoen-non, Thidarat Yamnim, Sudawan Jullagate, Pichai Ittasakul
Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Pichai Ittasakul, Tel +662-2011478, Fax +662-200-3277, Email [email protected]
Objective: To examine the effect of continuation-maintenance electroconvulsive therapy (ECT) on psychiatric hospitalization in Thai patients.
Methods: This retrospective mirror-image study reviewed medical records of Thai patients who received continuation-maintenance ECT at Ramathibodi Hospital, Bangkok, between September 2013 and December 2022. The initiation of continuation-maintenance ECT served as the index event, establishing pre-initiation and post-initiation periods. The primary outcome measured the differences in admissions and admission days before and after continuation-maintenance ECT.
Results: Forty-seven patients were included in the study, with diagnoses of schizophrenia (38.3%), schizoaffective disorder (21.3%), and bipolar disorder (19.1%) being the most common. The mean (standard deviation; SD) age was 44.6 (12.2) years. The total duration that patients received continuation-maintenance ECT was 53 ± 38.2 months. Following the initiation of ECT, there was a significant reduction in the median (interquartile range) number of hospitalizations for all patients (2 [2] versus 1 [2], p < 0.001), as well as for the psychotic disorder group (2 [2] versus 1 [2.75], p = 0.006) and the mood disorder group (2 [2] versus 1 [2], p = 0.02). Moreover, there was a significant reduction in the median (interquartile range) length of admission days for all patients after the initiation of continuation-maintenance ECT (66 [69] versus 20 [53], p < 0.001). Specifically, the psychotic disorder group (64.5 [74] versus 15.5 [62], p = 0.02) and mood disorder group (74 [57] versus 20 [54], p = 0.008) demonstrated statistically significant decreases in admission days.
Conclusion: Continuation-maintenance ECT may be an effective treatment option for reducing hospitalizations and admission days in patients with various psychiatric diagnoses. However, the study also highlights the need to carefully consider the potential adverse effects of ECT in clinical decision-making.
Keywords: continuation ECT, electroconvulsive therapy, hospitalization, maintenance ECT, Thai
Introduction
Electroconvulsive therapy (ECT) is a safe and effective treatment modality for mood and other psychiatric disorders. While a short-term course of ECT induces remission in psychiatric symptoms,1 but does not guarantee prevent a relapse. Therefore, maintenance therapy should always be considered after remission of psychiatric symptoms for relapse prevention.
Continuation ECT or maintenance ECT is sometimes used as a maintenance therapy in some patients. Continuation ECT refers to ECT sessions administered approximately six months following the initial index series,2 with treatments given once every 1–6 weeks.3 Maintenance ECT, on the other hand, involves infrequent ECT treatments administered over a long period after the index series and continuation ECT. Continuation-maintenance ECT treatments have been reported to be effective in preventing relapse.4–7 Indications for continuation-maintenance ECT treatments may include rapid relapse after initial ECT, severe symptoms, psychotic symptoms, and medication intolerance.8 In Thailand, the most common diagnoses among patients who received continuation-maintenance ECT were schizophrenia, followed by bipolar disorder, schizoaffective disorder, major depressive disorder, respectively.9
Previous studies demonstrated that continuation-maintenance ECT appears to be effective in reducing and shortening psychiatric admissions in people with severe affective illness. A recent study in the elderly with major depressive disorder revealed a 53% reduction in the number of admissions and a 79% reduction in admission duration in the two years after continuation-maintenance ECT treatment, compared to the previous two years.10 Similarly, a recent study from the Netherlands reported a 52% reduction in the duration of hospitalization during maintenance ECT, compared with pre-ECT, across all patients, with greater reductions observed for patients with mood disorders as opposed to those with schizophrenia.11 A previous study conducted in Thailand followed 58 patients who met remission criteria during the acute phase and were included in a single-blind, 6-month continuation treatment study. These patients were randomly assigned to three treatment groups: continuation ECT and flupenthixol combined, continuation ECT alone, and flupenthixol alone. After the 6-month continuation treatment, the relapse rate was found to be 40% for the group receiving the combination treatment, while it was 93% for both other monotherapy groups. These results suggest that the use of continued maintenance ECT in combination with an antipsychotic may be a valuable strategy in managing this patient population.12
To date, limited research has explored the effect of continuation-maintenance ECT in Thai patients. Therefore, the present study aims to examine the effect of continuation-maintenance ECT on psychiatric hospitalization in this population. We hypothesize that continuation-maintenance ECT will be beneficial in reducing admissions among psychiatric patients.
Materials and Methods
Study Design and Setting
The present research was conducted following approval by the Human Research Ethics Committee of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University (COA. No.: MURA2022/465), and written informed consent was obtained from patients or their family members. Research was conducted in accordance with the Declaration of Helsinki.
This was a retrospective mirror-image study that involved the review of medical records of all patients who received continuation-maintenance ECT at the Brain stimulation unit, Ramathibodi Hospital, Bangkok between September 2013 and December 2022. The initiation of continuation-maintenance ECT was considered as the index event, serving as the reference point to establish the pre-initiation and post-initiation periods. The observation duration before and after ECT was consistently maintained for each patient. This approach was implemented to mitigate potential confounding factors that may arise from variations in follow-up periods.
Definition of Continuation-Maintenance ECT
The continuation-maintenance ECT was defined as ECT that is started directly after the index course to prevent relapse, usually administered every 1–4 weeks. At our institution, continuation-maintenance ECT is predominantly delivered in an outpatient setting. Patients arrive at the Brian Stimulation Unit in the morning to complete the registration process and undergo pre-ECT evaluations.
Patient Assessment and ECT Procedure
Prior to administering ECT, all patients were evaluated by psychiatrists and anesthesiologists. Benzodiazepines were discontinued at least 15 hours before treatment. The ECT procedure was conducted in the post-anesthesia care unit and involved a team comprising a psychiatrist, in-training psychiatric residents, anesthetic staff, psychiatric nurses, and anesthetic nurses. ECT was administered after anesthesia with either thiopental (1.5–2.5 mg/kg intravenous [IV]) or propofol (1–2 mg/kg IV) and succinylcholine (0.5–1.5 mg/kg IV), a muscle relaxant. The procedure utilized a modified technique that incorporated a brief pulse wave generated by a Mecta Spectrum 5000Q (Mecta, Tualatin, OR, USA) or Thymatron System IV (Somatics, Northampton, MA, USA). The pulse width of ECT administered to all patients was 0.5–1.0 milliseconds.
Data Collection
We collected demographic data, clinical characteristics including the age at which continuation-maintenance ECT was initiated, age of onset, psychiatric diagnosis. The diagnoses of the patients had been determined by psychiatrists based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) criteria.13 We also collected hospitalization data, including number of admissions and length of stay before and after receiving continuation-maintenance ECT.
Statistical Analysis
Categorical variables were expressed as numbers and percentages, while continuous variables were reported as mean ± standard deviation or median and interquartile range, depending on the normality of the data distribution. The normality of variables was assessed using the Kolmogorov–Smirnov test. The Wilcoxon signed rank test was used to compare the differences in the number of admissions and admission days before and after continuation-maintenance ECT. The significance level was set at p < 0.05 for all analyses.
All statistical analyses were performed using IBM SPSS software (version 26.0 for Windows; IBM Corp., Armonk, NY, USA).
Results
Between September 2013 and December 2022, a total of 47 patients received continuation-maintenance ECT and were included in this study. The review period, encompassing both the pre- and post-initiation of continuation-maintenance electroconvulsive therapy (ECT), had a mean duration of 61.3 ± 36.8 months.
The demographic and clinical characteristics of all participants at the initiation of continuation-maintenance ECT are presented in Tables 1. The age of participants ranged from 19 to 96 years, with 5 (10%) patients being elderly (age ≥ 60 years of age). The most common diagnoses among patients were schizophrenia (18, 38.3%), schizoaffective disorder (10, 21.3%), bipolar disorder (9, 19.1%). Bilateral electrode placement was administered to 38 (80.9%) patients, while 9 (19.1%) patients received right unilateral electrode placement. The total duration of continuation-maintenance ECT treatment for all patients was 53 ± 38.2 months (range 5–190 months).
 |
Table 1 Demographic and Clinical Characteristics (n=47) |
Number of Hospitalization and Admission Days
The number of hospitalizations and total admission days for all 47 patients before and after the initiation of continuation-maintenance ECT are presented in Table 2.
 |
Table 2 Comparison of Hospitalizations and Admission Days Before and After Continuation-Maintenance ECT Initiation During the Observation Period |
To conduct a subgroup analysis, considering the limited patient numbers within each diagnostic group, we divided the patients into two distinct categories: the psychotic disorder group (n = 28), consisting of individuals diagnosed with schizophrenia and schizoaffective disorder, and the mood disorder group (n = 17), comprising patients diagnosed with major depressive disorder and bipolar disorder.
The median number of hospitalizations and total admission days showed a statistically significant reduction in both the psychotic disorder group and the mood disorder group following the initiation of continuation-maintenance ECT).
Adverse Effects
The study observed adverse effects in 43 (91.5%) of the 47 patients who underwent ECT. The most common adverse effects were headache, muscle ache and memory loss, retrospectively. (Table 3) These adverse effects were generally of mild intensity.
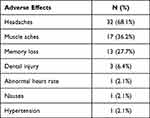 |
Table 3 The Observed Adverse Effects (N= 47) |
Discussion
In this retrospective mirror-image study, our objective was to investigate the effectiveness of continuation-maintenance ECT in reducing the number of hospitalizations and admission days in patients with various psychiatric diagnoses. The study included 47 patients who received continuation-maintenance ECT over a period of 53 ± 38.2 months, with the majority receiving bilateral electrode placement. The predominant diagnosis appears to be schizophrenia, comprising 38.3% of patients, followed by schizoaffective disorder at 21.3%, bipolar disorder at 19.1%, and major depressive disorder at 17%. These patterns closely mirror the broader trends observed in Asian countries.9,14 However, there are notable distinctions when compared to the United States, Australia, New Zealand, and several other Western nations, where mood disorders exhibit a higher prevalence.15–19
Our findings indicate that the number of hospitalizations and admission days were significantly reduced in all patients after the initiation of continuation-maintenance ECT. Specifically, individuals in both the psychotic disorder group, encompassing schizophrenia and schizoaffective disorder, as well as the mood disorders group, comprising major depressive disorder and bipolar disorder, exhibited a statistically significant reduction in the aforementioned parameters. These results are consistent with previous studies that have demonstrated the effectiveness of continuation-maintenance ECT in reducing the risk of relapse and readmission rates for patients with schizophrenia,20,21 bipolar disorder,22,23 and major depressive disorder,10,24 and schizoaffective disorder.23,25
The reduction in admission days and hospitalizations in patients undergoing continuation-maintenance ECT can be attributed to several factors. Firstly, it effectively manages psychiatric conditions by stabilizing mood, alleviating symptoms, and preventing relapses, thus reducing the severity of symptoms and the need for prolonged hospitalization. Secondly, it is particularly effective in preventing relapse in patients with severe and treatment-resistant psychiatric disorders, reducing the likelihood of relapses and subsequent hospitalizations. Thirdly, the consistent delivery of ECT over an extended period ensures treatment continuity and promotes adherence to the treatment plan, helping patients maintain stability in the community and minimizing the need for hospitalization due to exacerbations. Lastly, the individualized treatment approach of continuation-maintenance ECT, which tailors treatment parameters to each patient’s needs, response, and tolerance, optimizes outcomes by providing personalized therapeutic benefits and minimizing adverse effects.
In terms of adverse effects, our study found that 91.5% of patients who underwent ECT experienced at least one adverse effect. The most commonly reported adverse effects were headaches, muscle aches, memory loss, with dental injury. Nevertheless, it is worth noting that these adverse effects were generally mild and well-tolerated. These results are consistent with previous studies that have shown continuation-maintenance ECT is well-tolerated in psychiatric patients.10,26,27 In regards to the cognitive adverse effect, data from previous studies indicated that the continuation and maintenance ECT do not appear to have a harmful effect for global cognitive function.28,29
Strengths of this study was the inclusion of patients with various psychiatric diagnoses. The study also used objective measures of hospitalization and admission days before and after continuation-maintenance ECT, which adds to the validity of the findings. However, there are some limitations that need to be considered. First, the study was retrospective, which means that data collection was dependent on medical records and may have led to missing or incomplete information. Additionally, there was no control group, which limits the ability to draw firm conclusions about the effectiveness of continuation-maintenance ECT compared to other treatment options. Moreover, the study did not include a formal assessment of cognitive function, which is a potential adverse effect of ECT that could impact patient quality of life. Finally, the study did not provide information about the frequency and number of continuation-maintenance ECT sessions, which could have an impact on patient outcomes.
Conclusions
In summary, continuation-maintenance ECT may be an effective treatment option for reducing hospitalizations and admission days in patients with various psychiatric diagnoses. However, the study also highlights the need to carefully consider the potential adverse effects of ECT in clinical decision-making.
Data Sharing Statement
The data presented in this study are available upon request from the corresponding author.
Informed Consent Statement
All participants provided written informed consent.
Acknowledgments
The authors would like to express their gratitude to the personnel affiliated with the Brain Stimulation Unit of Ramathibodi Hospital for their invaluable assistance in facilitating the data collection process.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Disclosure
All authors received salary support from Mahidol University, Bangkok, Thailand. Pichai Ittasakul received lecture honoraria from Janssen, Pfizer, and Sumitomo Dainippon Pharma. The authors report no other conflicts of interest in this work.
References
1. Ittasakul P, Vora-Arporn S, Waleeprakhon P, Tor PC. Number of electroconvulsive therapy sessions required for Thai psychiatric patients: a retrospective study. Neuropsychiatr Dis Treat. 2020;16:673–679. doi:10.2147/NDT.S244031
2. Trevino K, McClintock SM, Husain MM. A review of continuation electroconvulsive therapy: application, safety, and efficacy. J ECT. 2010;26(3):186–195. doi:10.1097/YCT.0b013e3181efa1b2
3. van Waarde JA, Wielaard D, Wijkstra J, Verwey B, van der Mast RC. Retrospective study of continuation electroconvulsive therapy in 50 patients. J ECT. 2010;26(4):299–303. doi:10.1097/YCT.0b013e3181cf114c
4. Ward HB, Szabo ST, Rakesh G. Maintenance ECT in schizophrenia: a systematic review. Psychiatry Res. 2018;264:131–142. doi:10.1016/j.psychres.2018.03.033
5. Petrides G, Tobias KG, Kellner CH, Rudorfer MV. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64(3):129–140. doi:10.1159/000328943
6. Medda P, Toni C, Perugi G. The mood-stabilizing effects of electroconvulsive therapy. J ECT. 2014;30(4):275–282. doi:10.1097/YCT.0000000000000160
7. Luccarelli J, McCoy TH, Seiner SJ, Henry ME. Maintenance ECT is associated with sustained improvement in depression symptoms without adverse cognitive effects in a retrospective cohort of 100 patients each receiving 50 or more ECT treatments. J Affect Disord. 2020;271:109–114. doi:10.1016/j.jad.2020.03.152
8. Gill SP, Kellner CH. Clinical practice recommendations for continuation and maintenance electroconvulsive therapy for depression: outcomes from a review of the evidence and a consensus workshop held in Australia in may 2017. J ECT. 2019;35(1):14–20. doi:10.1097/YCT.0000000000000484
9. Kittayarak K, Ittasakul P. Electroconvulsive therapy practice in Thailand: a nationwide survey. Neuropsychiatr Dis Treat. 2022;18:2477–2484. doi:10.2147/NDT.S385598
10. O’Connor DW, Gardner B, Presnell I, Singh D, Tsanglis M, White E. The effectiveness of continuation-maintenance ECT in reducing depressed older patients’ hospital re-admissions. J Affect Disord. 2010;120(1–3):62–66. doi:10.1016/j.jad.2009.04.005
11. Stegmann B, Gale C, Glue P. Maintenance ECT treatment in New Zealand: local and national data. Australas Psychiatry. 2022;10398562221126589.
12. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15(3):178–192. doi:10.1097/00124509-199909000-00002
13. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-V. Am Psychiatric Assoc. 2013;1:546.
14. Chanpattana W, Kramer BA, Kunigiri G, Gangadhar BN, Kitphati R, Andrade C. A survey of the practice of electroconvulsive therapy in Asia. J Ect. 2010;26(1):5–10. doi:10.1097/YCT.0b013e3181a74368
15. Leiknes KA, Jarosh-von Schweder L, Høie B. Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav. 2012;2(3):283–344. doi:10.1002/brb3.37
16. Antosik-Wójcińska AZ, Dominiak M, Mierzejewski P, et al. Changes in the practice of electroconvulsive therapy in Poland: a nationwide survey comparing data between 2005 and 2020. Neuropsychiatr Dis Treat. 2021;17:605–612. doi:10.2147/NDT.S296210
17. Vera I, Sanz-Fuentenebro J, Urretavizcaya M, et al. Electroconvulsive therapy practice in Spain: a national survey. J Ect. 2016;32(1):55–61. doi:10.1097/YCT.0000000000000270
18. Chanpattana W. A questionnaire survey of ECT practice in Australia. J Ect. 2007;23(2):89–92. doi:10.1097/YCT.0b013e318031bc50
19. Sienaert P, Falconieri T, Obbels J, van den Ameele H, Bouckaert F. Improving Practice in Electroconvulsive Therapy: a Nationwide Survey in Belgium. J Ect. 2016;32(1):29–32. doi:10.1097/YCT.0000000000000260
20. Ali SA, Mathur N, Malhotra AK, Braga RJ. Electroconvulsive therapy and schizophrenia: a systematic review. Mol Neuropsychiatry. 2019;5(2):75–83. doi:10.1159/000497376
21. Shelef A, Mazeh D, Berger U, Baruch Y, Barak Y. Acute electroconvulsive therapy followed by maintenance electroconvulsive therapy decreases hospital re-admission rates of older patients with severe mental illness. J ECT. 2015;31(2):125–128. doi:10.1097/YCT.0000000000000197
22. Madero S, Anmella G, Sagué-Vilavella M, et al. Evaluating maintenance electroconvulsive therapy in Bipolar Disorders: 3-year mirror-image study. J Affect Disord. 2022;298(Pt A):58–64. doi:10.1016/j.jad.2021.10.052
23. Santos Pina L, Bouckaert F, Obbels J, et al. Maintenance electroconvulsive therapy in severe bipolar disorder: a retrospective chart review. J ECT. 2016;32(1):23–28. doi:10.1097/YCT.0000000000000253
24. Rapinesi C, Kotzalidis GD, Serata D, et al. Prevention of relapse with maintenance electroconvulsive therapy in elderly patients with major depressive episode. J ECT. 2013;29(1):61–64. doi:10.1097/YCT.0b013e31826d369a
25. Swoboda E, Conca A, König P, Waanders R, Hansen M. Maintenance electroconvulsive therapy in affective and schizoaffective disorder. Neuropsychobiology. 2001;43(1):23–28. doi:10.1159/000054861
26. van Schaik AM, Comijs HC, Sonnenberg CM, Beekman AT, Sienaert P, Stek ML. Efficacy and safety of continuation and maintenance electroconvulsive therapy in depressed elderly patients: a systematic review. Am J Geriatr Psychiatry. 2012;20(1):5–17. doi:10.1097/JGP.0b013e31820dcbf9
27. Abraham G, Milev R, Delva N, Zaheer J. Clinical outcome and memory function with maintenance electroconvulsive therapy: a retrospective study. J ECT. 2006;22(1):43–45. doi:10.1097/00124509-200603000-00009
28. Yoldi-Negrete M, Gill LN, Olivares S, Lauzière A, Désilets M, Tourjman SV. The effect of continuation and maintenance electroconvulsive therapy on cognition: a systematic review of the literature and meta-analysis. J Affect Disord. 2022;316:148–160. doi:10.1016/j.jad.2022.08.005
29. Rowland T, Mann R, Azeem S. The efficacy and tolerability of continuation and maintenance electroconvulsive therapy for depression: a systematic review of randomized and observational studies. J ECT. 2023. doi:10.1097/YCT.0000000000000914
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
