Back to Journals » Journal of Pain Research » Volume 17
Effect of Best Practice Alert (BPA) on Post-Discharge Opioid Prescribing After Minimally Invasive Hysterectomy: A Quality Improvement Study
Authors Jankulov A , As-Sanie S, Zimmerman C, Virzi J, Srinivasan S, Choe HM, Brummett CM
Received 26 July 2023
Accepted for publication 28 December 2023
Published 14 February 2024 Volume 2024:17 Pages 667—675
DOI https://doi.org/10.2147/JPR.S432262
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Alexandra Jankulov,1 Sawsan As-Sanie,2 Christopher Zimmerman,3 Jessica Virzi,4 Sudharsan Srinivasan,5 Hae Mi Choe,3 Chad M Brummett5,6
1Oakland University William Beaumont School of Medicine, Rochester Hills, MI, USA; 2Department of Obstetrics & Gynecology, University of Michigan Health System, Ann Arbor, MI, USA; 3Department of Health Information and Technology Services, University of Michigan Health System, Ann Arbor, MI, USA; 4Department of Precision Health, University of Michigan Health System, Ann Arbor, MI, USA; 5Department of Anesthesiology, University of Michigan Health System, Ann Arbor, MI, USA; 6Michigan Opioid Prescribing Engagement Network, Ann Arbor, MI, USA
Correspondence: Chad M Brummett, Department of Anesthesiology, University of Michigan, 325 E Eisenhower Pkwy Ste 100, Ann Arbor, MI, 48108, USA, Tel +1 734-998-0455, Fax +1 734-936-6585, Email [email protected]
Purpose: The aim of this study was to describe the effectiveness of an electronic health record best practice alert (BPA) in decreasing gynecologic post-discharge opioid prescribing following benign minimally invasive hysterectomy.
Patients and Methods: The BPA triggered for opioid orders > 15 tablets. Prescribers’ options included (1) decrease to 15 ≤ tablets; (2) remove the order/utilize a defaulted order set; or (3) override the alert.
Results: 332 patients were included. The BPA triggered 29 times. The following actions were taken among 16 patients for whom the BPA triggered: “override the alert” (n=13); “cancel the alert” (n=2); and ‘remove the opioid order set’ (n=1). 12/16 patients had discharge prescriptions: one patient received 20 tablets; two received 10 tablets; and nine received 15 tablets. Top reasons for over prescribing included concerns for pain control and lack of alternatives.
Conclusion: Implementing a post-discharge opioid prescribing BPA aligned opioid prescribing following benign minimally invasive hysterectomy with guideline recommendations.
Keywords: hysterectomy, opioid, prescribing, patient discharge, practice patterns
Introduction
Opioid-related morbidity and mortality continue to be a public health crisis in the United States,1–3 and post-surgical prescribing is an important contributor to this problem at large.4 For example, an estimated 72% of patients have excess opioids following common surgical procedures.5–8 Thus, excess prescribing in North America poses adverse outcomes including increased rates of new persistent opioid use9–12 and diversion, misuse, and abuse throughout the community, exacerbating the opioid epidemic.13 Hysterectomy is the most common non-obstetric surgical procedure in women,14,15 and approximately 82% of patients receive opioids following hysterectomy.16–18 Recent data also suggest that opioids are vastly overprescribed in this patient population.19
Among the potential approaches to address excess post-surgical prescribing in these patients is use of behavioral economics and nudge interventions to improve clinical compliance. Applications of these interventions in the medical field exist on a continuum, ranging from a subtle opportunity to provide information to clinicians to a more restrictive elimination of choice.20 In particular, best practice alerts (BPA) are clinical decision support tools accessible in the electronic health record (EHR) and prompt clinicians to bring additional attention to particular components of a patient’s care needs.21 BPAs are well described in the literature for supporting and improving clinical decisions and compliance measures. Favorably, recent evidence indicates that BPA interventions are effective in multiple clinical situations,21–26 particularly in decreasing opioid prescribing in inpatient and outpatient settings,25,26 decreasing antibiotic prescribing,27–29 and increasing naloxone prescribing.30–32 Together, these studies highlight that BPAs may be an effective platform for improving adherence to prescribing guidelines and reducing excess post-surgical opioid prescribing in US health-care systems in the future.
Although there is growing evidence in support of prescribing BPAs, a limited set of data exists regarding BPAs in the setting of opioid prescribing after surgery, including hysterectomy.33 The present quality improvement project was designed to assess the impact and provider perceptions of a BPA for post-discharge opioid prescribing after hysterectomy implemented in a large, tertiary care health system. The two aims of this QI project were to (1) evaluate this BPA’s effectiveness and feasibility in decreasing gynecologic post-discharge opioid prescribing following benign minimally invasive hysterectomy and (2) obtain qualitative clinician perspectives of prescribing BPA.
Methods
This QI project was approved by the University of Michigan Institutional Review Board (IRB HUM00201769). This quality improvement project was deemed as not regulated by the University of Michigan's institutional review board. No informed consent procedures were required.
Clinical Rationale
The Opioid Prescribing Engagement Network at the University of Michigan (OPEN, www.michigan-OPEN.org)—a statewide collaboration—aims to establishing evidence-based guidelines to tailor acute and postoperative care opioid prescribing in combat of the opioid epidemic in the state of Michigan. OPEN has developed opioid prescribing recommendations for multiple surgical specialties and has also worked to improve use of non-opioid analgesics, increase expectation setting for patients prior to surgery, and encourage safe storage and disposal of opioid prescriptions. In partnership with the Michigan Department of Health and Human Services, Blue Cross Blue Shield of Michigan (BCBSM) Value Partnerships, and the Institute for Healthcare Policy and Innovation (IHPI) at the University of Michigan, this program was initiated to promote awareness about and advance perioperative pain management while minimizing surgical opioid prescribing-related morbidity and mortality. Evidence-based opioid prescribing recommendations by OPEN have been recognized by the Leapfrog Group as meeting quality standards for post-surgical opioid prescribing, as well as the revised Centers for Disease Control and Prevention (CDC) Opioid Prescribing Guidelines.34
In 2017, OPEN released the first evidence-based prescribing guidelines for multiple surgical conditions and has continued to refine and update these guidelines. Per the guidelines, the appropriate quantity of oxycodone 5 mg tablets for abdominal hysterectomy was 0–20 tablets and for vaginal or laparoscopic/robotic hysterectomy was 0–15 tablets.35 In partnership with OPEN, the Precision Health Initiative Implementation Team at the University of Michigan36 developed an interruptive BPA in an attempt to ensure compliance with opioid prescribing guidelines after hysterectomy.
BPA Development
In Fall 2019, Michigan Medicine created a clinical decision support tool, in the form of an interruptive BPA (Epic Systems Inc., Verona, WI), for patients undergoing minimally invasive hysterectomy.
The BPA criteria were as follows:
- Prescribed oral opioids with a quantity greater than 15 tablets/pills
- Admission/discharge transfer system (ADT) Patient Class: hospital outpatient surgery, defined as non-admitted patients with 0 stays past midnight
- Primary Procedure performed: minimally invasive hysterectomy (defined as vaginal, laparoscopic, or robotic hysterectomy)
The BPA was triggered upon signing new opioid medications in the EHR Discharge Navigator Order Reconciliation (Supplemental Figure 1), if the above criteria were met. When triggered, the BPA presented a link to the OPEN guidelines, a custom-built gynecology postoperative discharge order set containing defaulted prescription order options for both oral non-opioid and opioid pain medications and additional medications including oral anti-emetics and laxatives. Prescribers had multiple prescribing options when interacting with the BPA tool: (1) cancel the alert and change the dispense quantity to less than or equal to 15 tablets/pills; (2) remove the opioid order in progress and open a gynecology order set with defaulted medication options; or (3) override the alert. Providers that chose to override the BPA recommendations were required to outline reasons for a prescription order of greater than 15 tablets/pills.
BPA Implementation
In October 2019, the BPA was integrated into the existing discharge workflow and configured to trigger once a postoperative discharge opioid-containing oral analgesic was prescribed exceeding a quantity greater than a 3-day supply as a proxy for the 15 tablet recommendations. Following a 3-month time period, the pilot BPA was adjusted in February 2020 to trigger once a discharge opioid prescription exceeded 15 tablets/pills, reflecting a more precise measurement of prescribing practices. All BPA data were collected for postoperative patients following a minimally invasive hysterectomy during the time period of October 2019 to February 2021.
Data Acquisition & Variables of Interest
A retrospective chart review was performed. Data were collected for patients who underwent minimally invasive hysterectomy for benign indications between October 2019 and February 2021.
The study team abstracted information regarding gender, age, race, ethnicity, surgeon, date of surgery, preoperative opioid use in the 30 days prior to surgery, American Society of Anesthesiologists physical status classification score, Charlson Comorbidity Index, opioid prescription at discharge (type of medication, dose, and number of pills), and prescribed non-opioid adjuncts. Once the data were collected, all identifiers were removed.
Provider Survey
During Summer 2021, resident physicians for whom the BPA fired during the time period of October 2019 to February 2021 were invited to complete a 5-min Qualtrics survey to discuss the BPA (Supplemental Information). The domain of interest included provider/user satisfaction with the BPA, as well as input from surgeons regarding BPA improvement. Categories addressed included resident perspectives of the BPA, BPA interface preferences, and QI barriers and facilitators. The survey was constructed to allow for the potential development of new categories.
Analysis
Patient characteristics were described through the utilization of descriptive statistics (eg percentages, means, and standard deviations). Differences between patients for whom the BPA triggered versus patients for whom the BPA did not trigger were assessed using the t-test and chi-square test. Sample size was selected based on the number of times the BPA triggered during this time period.
Results
Patient Population
This project initially had 344 patients (≥18 years) undergoing a benign minimally invasive outpatient hysterectomy—vaginal, laparoscopic, or robotic approach—between October 2019 and February 2021. We excluded seven patients who had an abdominal hysterectomy, four patients who had surgery at an outside hospital, and one patient who had a cancelled procedure. The final dataset included 332 patients (Figure 1). The mean age of the population was 50.5 (SD,12.65), and 71.4% of patients identified as white and non-Hispanic. Other descriptive data are displayed in Table 1.
 |
Table 1 Sample Preoperative Characteristics for Overall Sample and by Best Practice Alert (BPA) Group |
 |
Figure 1 Flow diagram displaying inclusion and exclusion criteria for studied patients. |
BPA Triggering
Between the months of October 2019 to February 2021, 332 patients in our cohort underwent benign minimally invasive hysterectomy, and the BPA triggered a total of 29 times; 4.82% of patients (n=16) had the BPA trigger and 95.18% of patients (n=316) did not have the BPA trigger. Seven patients had one BPA trigger; six patients had two BPA triggers; two patients had three BPA triggers; and one patient had four BPA triggers in their EHR account.
There were differences in demographics between those for whom a BPA was triggered. On average, BPA was more likely to trigger for younger patients (approximately 38.4 years), of white, non-Hispanic race/ethnicity (50% of patients) with an ASA score of 2 (62.5% of patients). The average Charlson comorbidity index score for patients for whom the BPA triggered and those the BPA did not trigger was 2.3 (SD of 3.94) and 4.1 (SD of 4.54), respectively. In the 30 days prior to surgery, a total of five patients had preoperative opioid prescriptions: one patient (SD 6.3) had a BPA trigger and four patients (SD 1.3) did not have BPA triggers (Table 1).
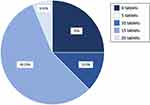
Final BPA Action
Among the 16 patients for whom the BPA triggered, 13 patients (81.25%) had “override the alert” as the final BPA action entered in the EHR by their provider. Two patients (12.50%) had “cancel the alert” as the final BPA action entered in the EHR. One patient (6.25%) had “remove the opioid order set in progress” as the final BPA action. Chart review data identified that among the 16 patients with a BPA trigger, 12 patients had a discharge prescription: one patient received 20 tablets (6.25% of patients); two patients received 10 tablets (12.50% of patients); and 9 patients received 15 tablets (56.25% of patients). 4/16 patients (25% of patients) did not have a discharge prescription (Figure 2).
Semi-Structured Qualtrics Survey
50% of resident providers (n=4) remembered the BPA trigger event and were aware of OPEN guidelines prior to writing their opioid prescriptions. When all providers were asked for intentions for prescribing over guideline recommendations, the following reasons were provided: “concerns for pain control” (37.5% of providers, n=3), “inability to use alternative treatments” (37.5% of providers, n=3), and “do not remember details” (25% of providers, n=2). Opinions regarding the BPA organization, structure, and utility were varied among providers.
For providers that recalled the BPA trigger, providers’ agreement (n=4) with the statement, “The BPA was clinically useful” was as follows: 25% slightly agreed, slightly disagreed, moderately disagreed, or were unsure, respectively. For the statement, “The BPA increased my awareness and knowledge of prescribing guidelines”, 50% were neutral, 25% slightly disagreed, and 25% strongly disagreed. Regarding, “The BPA made me consider my post-discharge prescribing habits”, 25% slightly agreed, 25% were neutral, and 50% moderately disagreed. For the statement, “The BPA would be beneficial for other procedure/surgery types in the future”, 50% moderately agreed, 25% slightly disagreed, and 25% strongly disagreed. For providers’ response to “What aspects of [the BPA’s] quality and/or interface would you change?”, 25% stated “get rid of the alert as it adds to alert fatigue” while 75% did not provide a response.
For providers that did not recall the BPA trigger, providers’ agreement (n=4) with the statement “The BPA would be clinically useful for post-discharge opioid prescribing after hysterectomy” was as follows: 50% strongly agreed, 25% moderately agreed, and 25% were neutral. For the statement “The BPA would increase my awareness and knowledge of the prescribing guidelines”, 50% slightly agreed, 25% were neutral, and 25% moderately disagreed. For the statement “The BPA would be beneficial for other procedure/surgery types in the future”, 25% strongly agreed, slightly agreed, were neutral, and moderately disagreed, respectively. Regarding the statement “The BPA would make me consider my own post-discharge opioid prescribing habits”, 25% moderately agreed, slightly agreed, slightly disagreed, and strongly disagreed, respectively. Supplemental Figure 2 and Box 1 describe the findings from the provider satisfaction survey.
 |
Box 1 Free Response of Provider Satisfaction for Whom the Best Practice Alert (BPA) Triggered |
Discussion
In this quality improvement study, we found that the implementation of a BPA for opioid prescribing after hysterectomy was associated with changes in the discharge opioid prescription that were aligned with prescribing recommendations. Specifically, the BPA triggered 29 times and was more likely to trigger for younger patients with lower comorbidities (lower ASA physical status and Charlson comorbidity scores), which could partly be due to pain being underreported or better tolerated by older patients. There is also a possibility older patients may have more realistic expectations regarding post-operative pain based on previous surgical experiences in contrast to younger patients who may not have a surgical history. Moreover, it is known that opioid consumption is higher in younger patients, so it may be that the providers were responding to a perceived need for more opioids. Post-operative opioid prescribing after minimally invasive hysterectomy aligned more closely with prescribing recommendations with the utilization of EHR post-discharge BPA. Only one patient received a tablet count above the recommended prescribing guidelines recommended by OPEN (0–15 tablets).35
While the use of BPAs for post-hysterectomy opioid prescribing has not been studied to our knowledge, studies highlighting the use of BPAs for opioid prescribing in general have noted a 34% decrease in the morphine milligram equivalents (MME) per opioid prescription per month following BPA implementation in inpatient and outpatient settings25 and a 19% increase in guideline-concordant opioid prescriptions following BPA implementation in ambulatory care.26 Similarly, BPA interventions have had considerable success in the arena of antibiotic stewardship and naloxone prescribing. Prior work across three groups highlighted that BPAs served as de-escalation tools for reducing antimicrobial prescriptions and broad-spectrum antibiotics specifically in patients hospitalized for ≥72 hours,27 sustainable interventions for implementing antibiotic management protocol in patients hospitalized with staph aureus bacteremia,28 and effective tools for minimizing discharge antibiotic prescribing when diagnostics supported viral respiratory infection.29 Yielding similar findings in naloxone prescribing, DeVries et al30 identified 13.8% of naloxone prescriptions being signed for patients with known substance abuse disorders or opioid overdose in response to BPA alerts; Eldred et al31 found an increase in naloxone prescribing from 2% prior to 57.6% following BPA implementation for ED patients with high risk for overdose; shortly after Funke et al32 introduced an evidence-based harm reduction BPA for 1426 patients with opioid use disorder in the ED, researchers saw naloxone prescriptions increase by 21.1%. The application of our novel BPA in the setting of post-gynecologic surgery has also yielded positive findings as described in these works.
While most providers selected to prescribe 15 tablets for discharge, a discrepancy existed between providers who remembered the BPA triggering versus those who did not remember the BPA altogether. Those providers that recalled the BPA triggering for patients were more likely to state that the BPA did not increase their awareness of prescribing guidelines or individual prescribing habits. However, 50% of these providers moderately agreed that the BPA would be successful for other procedure types. Meanwhile, providers that did not remember the BPA were more agreeable in terms of the alert’s clinical use, ability to increase awareness of prescribing guidelines, and benefit for future use in other procedure types. Perhaps, the interruption in workflow made providers that remembered the BPA less likely to find the alert useful, while those that did not remember were less likely to make negative associations with the idea of the BPA.
Alert fatigue has been identified as a potential issue in hospital settings, with approximately 50% or more of alerts being overridden or ignored by physicians.37,38 Similar sentiments were expressed by the findings in this pilot project. Potential methods to overcome these considerable figures include prioritizing alert triggers for at-risk patients, alert delays, customizing commercially available alerts, adding sophistication to existing alerts, and allowing providers to comment on the alert when interacting with interface.39,40 While our alert did utilize alert delays, customization, and opportunities for provider feedback, the physicians in this project did report alert fatigue as a concern for the BPA. We must further explore the mechanism with which providers engage with EHR alerts in order to determine other factors impacting their interaction with this particular BPA. For example, one must consider cognition and the distinctions between delaying a response by exiting an alert versus overriding an alert altogether. By examining the positive and negative cognitive processes at play when interacting with drug safety alerts, a more sustainable and effective choice architecture for BPA workflow will be achievable in the future—thus improving patient outcomes.
Strengths and Limitations
Although this pilot project contains a small sample, a major strength of the project is the emphasis on one of the most common non-obstetric surgical procedures in women (benign minimally invasive hysterectomy). In addition, this project utilized nationally recognized, data-driven opioid prescribing recommendations for abdominal and laparoscopic or vaginal hysterectomy from OPEN.35 Another strength of this project was early adjustment to focus on quantity of prescribed opioid tablets versus days supplied which may be interpreted in many ways. Furthermore, the BPA was designed to allow providers to close out and revisit the alert once a patient’s chart was accessed at a later time. Thus, more frequent alert appearances in the single patient’s chart nudged overall prescribing behaviors in favor of a reduced opioid tablet count.
This project has some limitations. The pilot BPA was initiated at a tertiary academic medical center in the Midwest, which can limit the generalizability to other locales (eg rural or urban settings). Additionally, an emphasis on multiple procedure types could have described a more robust result, pointing to surgery types in which BPAs could be most useful.33 Since clinicians at Michigan Medicine have exposure to best practices for opioid prescribing due to initiatives set by OPEN, it is possible that our limited BPA trigger data may reflect a more positive prescribing environment. Finally, the EHR alert architecture could not account for the initial discharge opioid order details entered by the provider: only the final prescription was captured. These missing data points present an incomplete picture of how the BPA affects clinicians’ thought processes.
Future Directions
Additional research will be necessary to capture the extent of overprescribing of opioids following hysterectomy at other hospital sites across the state of Michigan and its implications for further resident education and guideline establishment. Future renditions of a post-discharge prescribing BPA may include opioid alternatives for providers to select instead of prescribing opioids altogether. In addition, comparing pre- and post-BPA implementations of opioid prescribing and expanding future iterations of this BPA to the state-wide level and including additional procedure types may help to identify pockets of excessive opioid prescribing in other surgical specialties and hospital systems.
Conclusion
The use of a post-discharge opioid prescribing BPA was associated with changes in opioid prescribing following a benign minimally invasive hysterectomy that aligned with prescribing recommendations, in favor of a reduced opioid count.
Disclosure
Dr. Sawsan As-Sanie served as a consultant to Bayer Pharmaceuticals, Organon, Myovant-Sciences and Pfizer for research studies related to endometriosis, receives author royalties from UpToDate, and provided expert testimony, not relevant for any aspect of the submitted work. Dr. Brummett is a consultant for Alosa Health, Benter Foundation, Heron Therapeutics, Vertex Pharmaceuticals, and provides expert testimony, not relevant for any aspect of the submitted work. The authors report no other conflicts of interest in this work.
References
1. Bohnert S. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi:10.1001/jama.2011.370
2. Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314(17):1818–1831. doi:10.1001/jama.2015.13766
3. Overdose Death Rates. National Institute on Drug Abuse (NIDA). Available from: https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates.
4. Waljee JF, Li L, Brummett CM, Englesbe MJ. Iatrogenic opioid dependence in the United States. Ann Surg. 2017;265(4):728–730. doi:10.1097/SLA.0000000000001904
5. Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg. 2012;37(4):645–650. doi:10.1016/j.jhsa.2012.01.035
6. v HM, Mcmahon ML, Stucke RS, Barth RJ. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–714. doi:10.1097/SLA.0000000000001993
7. Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS One. 2016;11(1). doi:10.1371/journal.pone.0147972
8. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–1071. doi:10.1001/jamasurg.2017.0831
9. Brummett CM, Waljee JF, Goesling J, et al. New Persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6). doi:10.1001/JAMASURG.2017.0504
10. Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total Hip arthroplasty. Pain. 2016;157(6):1259–1265. doi:10.1097/J.PAIN.0000000000000516
11. Johnson SP, Chung KC, Zhong L, et al. Risk of prolonged opioid use among opioid-naïve patients following common hand surgery procedures. J Hand Surg Am. 2016;41(10):947–957.e3. doi:10.1016/J.JHSA.2016.07.113
12. Marcusa DP, Mann RA, Cron DC, et al. Prescription opioid use among opioid-naive women undergoing immediate breast reconstruction. Plast Reconstr Surg. 2017;140(6):1081–1090. doi:10.1097/PRS.0000000000003832
13. Brown CS, V. VJ, Howard RA, et al. Assessment of a quality improvement intervention to decrease opioid prescribing in a regional health system. BMJ Qual Saf. 2021;30(3):251–259. doi:10.1136/BMJQS-2020-011295
14. Center for Health Statistics N. Number of All-Listed Procedures for Discharges from Short-Stay Hospitals, by Procedure Category and Age. United States, 2010; 2010.
15. Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstetrics Gynecol. 2013;122(2 Pt 1):233–241. doi:10.1097/aog.0b013e318299a6cf
16. Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectomy: a nationwide questionnaire and database study. Anesthesiology. 2007;106(5):1003–1012. doi:10.1097/01.anes.0000265161.39932.e8
17. Darnall B, Li H. Hysterectomy and predictors for opioid prescription in a chronic pain clinic sample. Pain Med. 2011;12(2):196–203. doi:10.1111/j.1526-4637.2010.01038.x
18. Wen X, Kogut S, Aroke H, Taylor L, Matteson KA. Chronic opioid use in women following hysterectomy: patterns and predictors. Pharmacoepidemiol Drug Saf. 2020;29(4):493–503. doi:10.1002/pds.4972
19. As-Sanie S, Till SR, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstetrics Gynecol. 2017;130(6):1261–1268. doi:10.1097/AOG.0000000000002344
20. Wang SY, Groene O. The effectiveness of behavioral economics-informed interventions on physician behavioral change: a systematic literature review. PLoS One. 2020;15(6):e0234149. doi:10.1371/JOURNAL.PONE.0234149
21. Swedlund M, Norton D, Birstler J, Chen G, Cruz L, Hanrahan L. Effectiveness of a best practice alerts at improving hypertension control. Am J Hypertens. 2019;32(1):70–76. doi:10.1093/AJH/HPY155
22. Morgan JL, Baggari SR, Chung W, Ritch J, McIntire DD, Sheffield JS. Association of a best-practice alert and prenatal administration with tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccination rates. Obstetrics Gynecol. 2015;126(2):333–337. doi:10.1097/AOG.0000000000000975
23. Klatt TE, Hopp E. Effect of a best-practice alert on the rate of influenza vaccination of pregnant women. Obstetrics Gynecol. 2012;119(2 Pt 1):301–305. doi:10.1097/AOG.0B013E318242032A
24. Seetharaman S, Wilson C, Landrum M, et al. Does use of electronic alerts for Systemic Inflammatory Response Syndrome (SIRS) to identify patients with sepsis improve mortality? Am J Med. 2019;132(7):862–868. doi:10.1016/J.AMJMED.2019.01.032
25. Meisenberg BR, Grover J, Campbell C, Korpon D. Assessment of opioid prescribing practices before and after implementation of a health system intervention to reduce opioid overprescribing. JAMA Network Open. 2018;1(5):e182908–e182908. doi:10.1001/JAMANETWORKOPEN.2018.2908
26. Ancker JS, Gossey JT, Nosal S, et al. Effect of an electronic health record “nudge” on opioid prescribing and electronic health record keystrokes in ambulatory care. J Gen Intern Med. 2021;36(2):430–437. doi:10.1007/S11606-020-06276-1/TABLES/2
27. Schulz L, Osterby K, Fox B. The use of best practice alerts with the development of an antimicrobial stewardship navigator to promote antibiotic de-escalation in the electronic medical record. Infect Control Hosp Epidemiol. 2013;34(12):1259–1265. doi:10.1086/673977
28. Brotherton AL, Rab S, Kandiah S, Kriengkauykiat J, Wong JR. The impact of an automated antibiotic stewardship intervention for the management of Staphylococcus aureus bacteraemia utilizing the electronic health record. J Antimicrob Chemother. 2020;75(4):1054–1060. doi:10.1093/JAC/DKZ518
29. Moradi T, Bennett N, Shemanski S, Kennedy K, Schlachter A, Boyd S. Use of procalcitonin and a respiratory polymerase chain reaction panel to reduce antibiotic use via an electronic medical record alert. Clin Infect Dis. 2020;71(7):1684–1689. doi:10.1093/CID/CIZ1042
30. Devries J, Rafie S, Polston G. Implementing an overdose education and naloxone distribution program in a health system. J Am Pharm Assoc. 2017;57(2):S154–S160. doi:10.1016/J.JAPH.2017.01.002
31. Eldred S, Anstett T, Dietsche C, Wick A, Johnston C Combating the opioid epidemic through a naloxone best practice alert and other quality improvement interventions within an academic hospital. J Hosp Med. Available from: https://shmabstracts.org/abstract/combating-the-opioid-epidemic-through-A-naloxone-best-practice-alert-and-other-quality-improvement-interventions-within-an-academic-hospital/.
32. Funke M, Kaplan MC, Glover H, et al. Increasing naloxone prescribing in the emergency department through education and electronic medical record work-aids. Jt Comm J Qual Patient Saf. 2021;47(6):364–375. doi:10.1016/J.JCJQ.2021.03.002
33. Shenoy R, Wagner Z, Kirkegaard A, et al. Assessment of postoperative opioid prescriptions before and after implementation of a mandatory prescription drug monitoring program. JAMA Health Forum. 2021;2(10):e212924–e212924. doi:10.1001/JAMAHEALTHFORUM.2021.2924
34. About CDC’s Opioid Prescribing Guideline | opioids | CDC. Available from: https://www.cdc.gov/opioids/providers/prescribing/guideline.html.
35. Opioid Prescribing Recommendations. Michigan OPEN. Available from: https://michigan-open.org/prescribing-recommendations/.
36. University of michigan precision health. Available from: https://precisionhealth.umich.edu/.
37. Cash JJ. Alert fatigue. Am J Health Syst Pharm. 2009;66(23):2098–2101. doi:10.2146/AJHP090181
38. Griesbach S, Lustig A, Malsin L, Carley B, Westrich KD, Dubois RW. Best practices: an electronic drug alert program to improve safety in an accountable care environment. J Manag Care Spec Pharm. 2015;21(4):330–336. doi:10.18553/JMCP.2015.21.4.330
39. Kane-Gill SL, O’Connor MF, Rothschild JM, et al. Technologic distractions (Part 1): summary of approaches to manage alert quantity with intent to reduce alert fatigue and suggestions for alert fatigue metrics. Crit Care Med. 2017;45(9):1481–1488. doi:10.1097/CCM.0000000000002580
40. Winters BD, Cvach MM, Bonafide CP, et al. Technological distractions (Part 2): a summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit Care Med. 2018;46(1):130–137. doi:10.1097/CCM.0000000000002803
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.